Abstract
The Arab world is comprised of 22 countries with a combined population of ∼360 million. The region is still at the initial stages of the tobacco epidemic, where it is expected to witness an increase in smoking levels and mounting tobacco-related morbidity and mortality in the future. Still, the bleak outlook of the tobacco epidemic in the Arab world continues to be faced with complacency in the form of underutilization of surveillance systems to monitor the tobacco epidemic and prioritize action, and failure to implement and enforce effective policies to curb the tobacco epidemic. Understandably, the focus on the Arab world carries the risk of trying to generalize to such a diverse group of countries at different level of economic and political development. Yet, tobacco control in the Arab world faces some shared patterns and common challenges that need to be addressed to advance its cause in this region. In addition, forces that promote tobacco use, such as the tobacco industry, and trends in tobacco use, such as the emerging waterpipe epidemic tend to coalesce around some shared cultural and socio-political features of this region. Generally, available data from Arab countries point at three major trends in the tobacco epidemic: (1) high prevalence of cigarette smoking among Arab men compared with women; (2) the re-emergence of waterpipe (also known as hookah, narghile, shisha, arghile) smoking as a major tobacco use method, especially among youth and (3) the failure of policy to provide an adequate response to the tobacco epidemic. In this review, we will discuss these trends, factors contributing to them, and the way forward for tobacco control in this unstable region.
Keywords: Arab world, waterpipe, hookah, policy, tobacco industry
KEY MESSAGES.
The prevalence of cigarette smoking among Arab men is high compared with women and is increasing.
The Arab world is the hot-bed for the re-emerging of waterpipe smoking (also known as hookah, narghile, shisha, arghile), especially among youth.
Arab governments are still underutilizing population-based surveillance systems to monitor the tobacco epidemic and prioritize areas of concern and action.
Despite the adoption of the Framework Convention on Tobacco Control (FCTC) by most Arab countries, efforts of the tobacco industry and the presence of unaccountable governing systems in most of Arab countries have delayed serious policy responses to the tobacco epidemic.
Introduction
Annually, tobacco smoking causes ∼6 million deaths worldwide, and is projected to exceed 8 million by 2030 (WHO 2011). In industrialized nations, tobacco control policies (including price increases, advertising bans, clean indoor air legislation) have reduced but not eliminated tobacco use (WHO 2008a,b, 2011). This partial success prompted the tobacco industry to shift its focus to the developing world, where the combination of a weak public health sector and lack of political commitment provides a fertile ground for tobacco marketing efforts (Mackay and Crofton 1996). Consequently, most of today’s tobacco-caused morbidity and mortality occurs in the developing world, wreaking havoc on the livelihood of families and communities as it affects smokers during their most productive years (WHO 2011). The escalating tobacco epidemic is particularly apparent in the Arab world, a diverse group of countries at different levels of economic and political development (Jabbour et al. 2012). Reducing tobacco-caused death and disease in the Arab world requires an understanding of how these diverse countries share common challenges and root causes of the tobacco epidemic. Such understanding is instrumental for the development of an effective plan to respond to these challenges and garner public and political support for it.
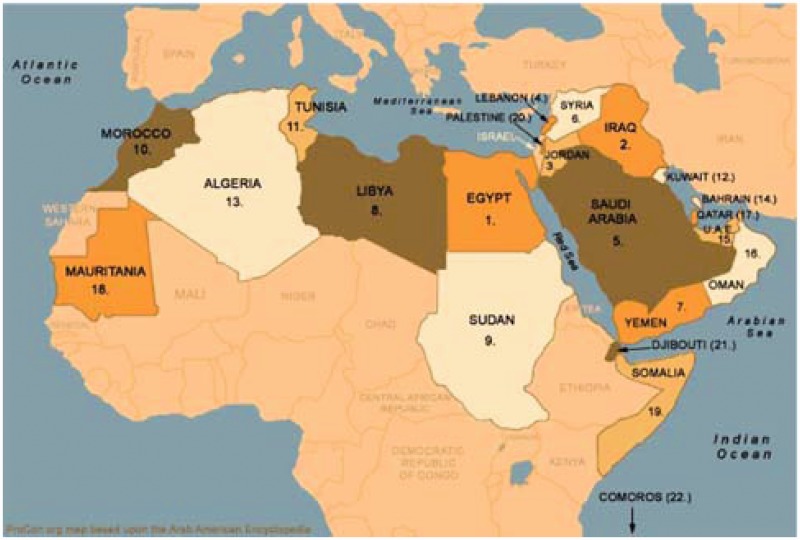
The Arab world is comprised of 22 member states of the Arab League with a combined population of ∼360 million (Figure 1) (Maziak 2009; Jabbour et al. 2012) The region remains in the initial stages of the tobacco epidemic, meaning that, in the coming years, it will continue to suffer increased tobacco use levels and mounting tobacco-caused morbidity and mortality. Yet, the escalating tobacco epidemic in Arab societies elicits minimal response at the public health and policy levels. Adding to this minimal response is the fact that national tobacco surveillance in the Arab world is poorly organized and available surveillance data are used ineffectively. For example, many Arab world countries are participants in the Global Tobacco Surveillance System (GTSS 2005), yet few use these data to plan and prioritize tobacco control initiatives. Generally, available data from Arab countries point at three major trends in the tobacco epidemic: (1) high prevalence of cigarette smoking among Arab men compared to women; (2) the re-emergence of waterpipe (also known as hookah, narghile, shisha, arghile) smoking as a major tobacco use method, especially among youth and (3) the failure of policy to provide an adequate response to the tobacco epidemic. In this review, we will discuss these trends, factors contributing to them, and the way forward for tobacco control in this unstable region.
Figure 1.
Map of the 22 member states of the Arab league in their order of joining (Maziak 2009).
Cigarette smoking: an epidemic among Arab men
In many Arab countries, about half of the male population smokes cigarettes (Ali et al. 2012), and smoking levels are dramatically higher than observed for women (Table 1) (WHO 2009c, 2011). Indeed, cigarette smoking among Arab men is increasing in several Arab countries, as is cigarette consumption at the societal level (Table 1) (WHO 2009c, 2011). Where reliable and detailed population data are available (e.g. Syria), they reveal a worrisome picture, where more than half of males are daily smokers, most of those are heavy smokers (i.e. average 20 cigarettes/day) (GTSS 2005; Ward et al. 2006). Heavy smoking challenges cessation efforts, because it produces and maintains high levels of tobacco/nicotine dependence. Cessation efforts in this region are further challenged by the scarcity of cessation services in most Arab countries. Moreover, in countries where cessation services are available, they tend to model treatment programmes from western societies with a different healthcare delivery and cultural contexts (Fiore et al. 2008). For example, the first randomized clinical trial comparing behavioural counselling vs counselling + nicotine replacement treatment (NRT) in an Arab country (Syria) showed no advantage for NRT over counselling alone, a result that suggests that cessation medications (like NRT) may not be useful if implemented in other cultures and healthcare settings (Ward et al. 2012).
Table 1.
Time trend in current cigarette smoking (age standardized) among adults for selected Arab countries, 2006–09
| Country | Year | Current cigarette use % (age standardized) |
|
|---|---|---|---|
| Male age standardized | Female age standardized | ||
| Bahrain | 2006 | 21 | 2 |
| 2009 | 29 | 7 | |
| Egypt | 2006 | 24 | 1 |
| 2009 | 33 | 0.5* | |
| Iraq | 2006 | 29 | 3 |
| 2009 | 26 | 3 | |
| Jordan | 2006 | 59 | 10 |
| 2009 | 42 | 3 | |
| Lebanon | 2006 | 31 | 7 |
| 2009 | 46 | 31 | |
| Morocco | 2006 | 27 | 0.2 |
| 2009 | 28 | 2 | |
| Saudi Arabia | 2006 | 22 | 3 |
| 2009 | 19 | 0.5* | |
| Syria | 2006 | 40 | – |
| 2009 | 35 | – | |
| Tunisia | 2006 | 53 | 6 |
| 2009 | 53 | 4 | |
| UAE | 2006 | 24 | 2 |
| 2009 | 15 | 0.5* | |
| Yemen | 2006 | 28 | 6 |
| 2009 | 30 | 10 | |
The escalating trend in cigarette smoking among men in the Arab world is contrasted by traditionally low levels of smoking among women (Figure 2), although under-reporting of this socially unacceptable behaviour by women cannot be ruled out. According to the latest Tobacco Atlas (2012), most Arab countries have a 10 to 1 gender-based ratio in cigarette smoking (Eriksen et al. 2012). This disparity is due mostly to the unacceptability of cigarette smoking by women within the prevailing culture of Arab societies. Evidence from youth supports this notion. For example, in a study of 2443 students (age ≈ 15 years) in Lebanon, girls who smoked cigarettes were less likely to be open with their parents about their practice compared to girls who smoked waterpipe, which is a more traditional form of smoking in Arab societies (Tamim et al. 2007). Lebanon provides another case in support of the culturally driven gender-divide in cigarette smoking. Being perhaps the most socially liberal Arab country, Lebanon has the least male/female disparity in cigarette smoking, and the highest level of women cigarette smoking in the region (Maziak 2009) (Figure 2). As we will see below, this relative immunity of Arab women to tobacco use is threatened by the more culturally acceptable waterpipe tobacco smoking.
Figure 2.
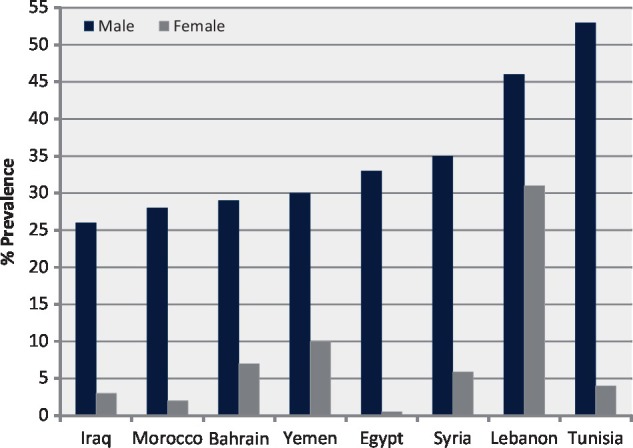
Age-standardized estimated prevalence of current cigarette smoking among men and women (15+ years) for selected Arab countries, 2009 (WHO 2009a).
Waterpipe tobacco smoking: a new epidemic?
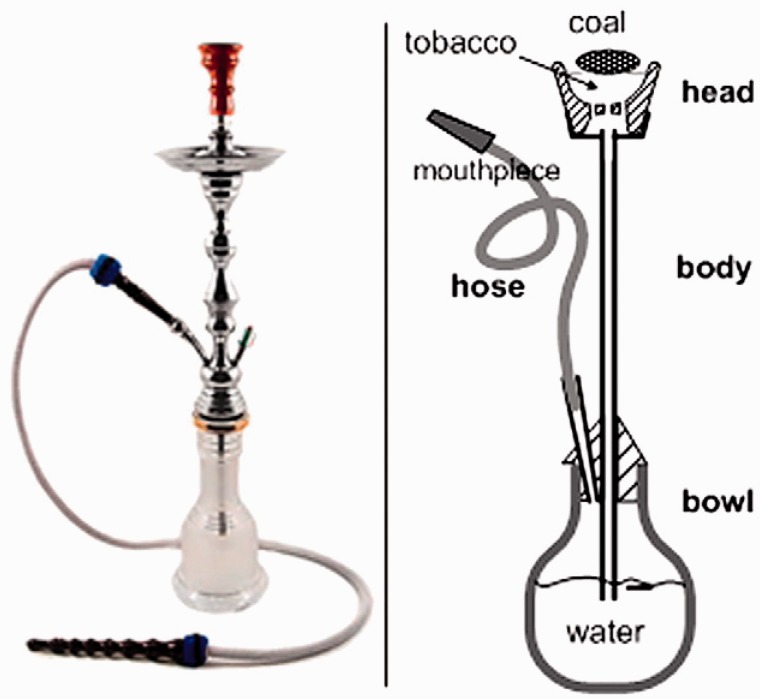
The recent rise of waterpipe smoking is putting several vulnerable groups in Arab societies such as women and youth in the path of tobacco addiction and harm. The waterpipe is a centuries-old tobacco use method that traditionally has been associated with Middle Eastern and South Asian societies (Maziak et al. 2004). In the waterpipe as it is commonly used nowadays (Figure 3), lit charcoal is placed atop perforated aluminum foil that separates the charcoal from a mass of flavoured tobacco (called Maassel). When the user inhales from the mouthpiece, charcoal-heated air is drawn through the tobacco and thus a combination of charcoal and tobacco smoke is generated and passes (bubbles) through the water on its way to the smoker (Figure 3). This last feature—the passage of smoke through water—underlies much of the widespread misperception about waterpipe’s ‘reduced’ addictiveness and harm (Maziak et al. 2004). In fact, available evidence reviewed below suggests that waterpipe smoking is associated with many of the diseases caused by cigarettes and also with tobacco/nicotine dependence (Ward et al. 2006; Fiore et al. 2008).
Figure 3.
Waterpipe picture (left) and schematic showing main parts (right) (Maziak 2011).
Waterpipe tobacco smoking started to become popular among youth in the Arab world in the 1990s, and now has spread across the globe (Akl et al. 2010; Maziak 2011). Many factors are thought to drive the re-emergence of waterpipe smoking including the introduction of manufactured flavoured waterpipe tobacco (also known as Maassel), misperception of reduced harm, the communication revolution brought about by the internet and the failure of policies to address this tobacco use method specifically (Rastam et al. 2004; Martinasek et al. 2011; Nakkash et al. 2011).
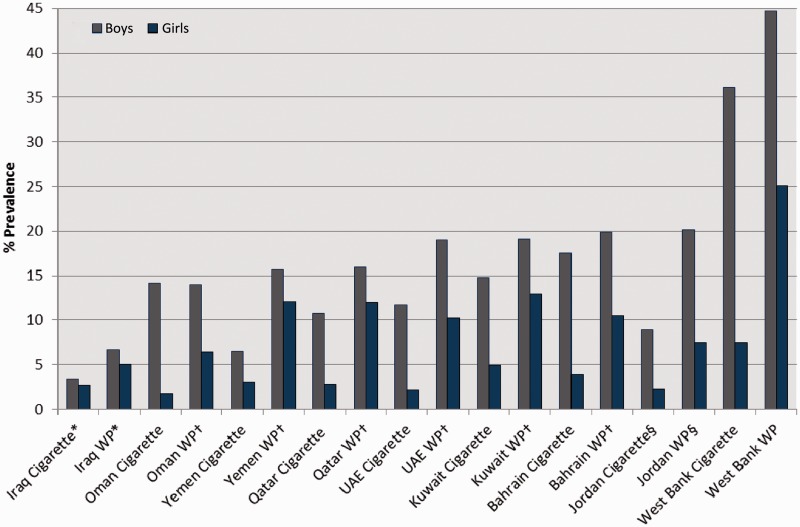
Among Arab youth in particular, numerous epidemiological surveys have documented the dramatic increase in waterpipe smoking (El-Awa et al. 2010; Akl et al. 2011) and it has now replaced cigarettes as the most common form of tobacco use in just a few years (Figure 4). For example, in the only longitudinal study of smoking behaviour among youth in the region (n = 1781, mean age at baseline 13 years, Jordan), waterpipe smoking prevalence was more than double that of cigarette at baseline (13.3 vs 5.3%) and increased by 40% within 2 years of follow-up (from 13.3 to 18.9%; P < 0.01) (Mzayek et al. 2012). In addition, a multi-country study involving a representative sample of 13- to 15-year-old school children in several Arab gulf countries (Bahrain, Oman, Qatar, United Arab Emirates [UAE], Kuwait, Yemen) showed a prevalence of waterpipe smoking ranging from 9 to 15%, and mostly surpassing that of cigarette (Figure 4) (Al-Mulla et al. 2008). Finally, in a region dominated by cigarette and waterpipe smoking with much less use of other forms of tobacco, the Global Youth Tobacco Survey (GYTS) involving more than 90 000 children (13–15 years) in the Arab region indicates the predominance of waterpipe smoking amongst youth, and its dramatic increase during the past decade or so (Warren et al. 2006; El-Awa et al. 2010).
Figure 4.
Current cigarette vs waterpipe smoking among 13–15 year olds in several Arab countries according to GYTS or surveys of comparable methods (Al-Mulla et al. 2008; Jasim et al. 2009; WHO 2010; Mzayek et al. 2012). *Based on a study in Baghdad city alone. †The estimates for ‘other’ tobacco were mainly for waterpipe. §Based on a study in Irbid city (Jordan).
The spread of waterpipe smoking among Arab youth might not be alarming if this form of tobacco use were not addictive and harmful. The first direct evidence that waterpipe smokers are exposed to the dependence-producing drug nicotine came from Macaron and colleagues in 1997: they showed increased levels of cotinine (a nicotine metabolite) in the urine of waterpipe smokers (Macaron et al. 1997). Our own work in waterpipe tobacco smokers demonstrates classic features of drug dependence including failed quit attempts, self-perception of being ‘hooked’, use escalation over time, behavioural adaptations to ensure access and abstinence-induced symptoms that are suppressed by subsequent waterpipe use (Maziak et al. 2004; Ward et al. 2005). Case histories from waterpipe smokers provide another line of evidence of its addictiveness; ‘I like to dominate everything, but the narghile has completely dominated me’ (Hammal et al. 2008). An especially concerning finding of our own research is that the waterpipe can potentiate failed quit attempts in cigarette smokers (Asfar et al. 2008; Hammal et al. 2008). While most of the described dependence features are known from the cigarette literature, studies in waterpipe smokers indicate dependence features and cues that are unique to the waterpipe such as the appeal of waterpipe smoke’s aromatic smell and smoothness, the bubbling sound of the water, and most importantly, the social and shared experience of this tobacco use habit (Maziak et al. 2005; Cobb et al. 2010; Maziak 2011; Martinasek et al. 2011; Nakkash et al. 2011). These unique features require novel approaches to waterpipe prevention and cessation based on evidence about the development and composition of dependence in waterpipe smokers and factors influencing it (Maziak 2011, 2013a).
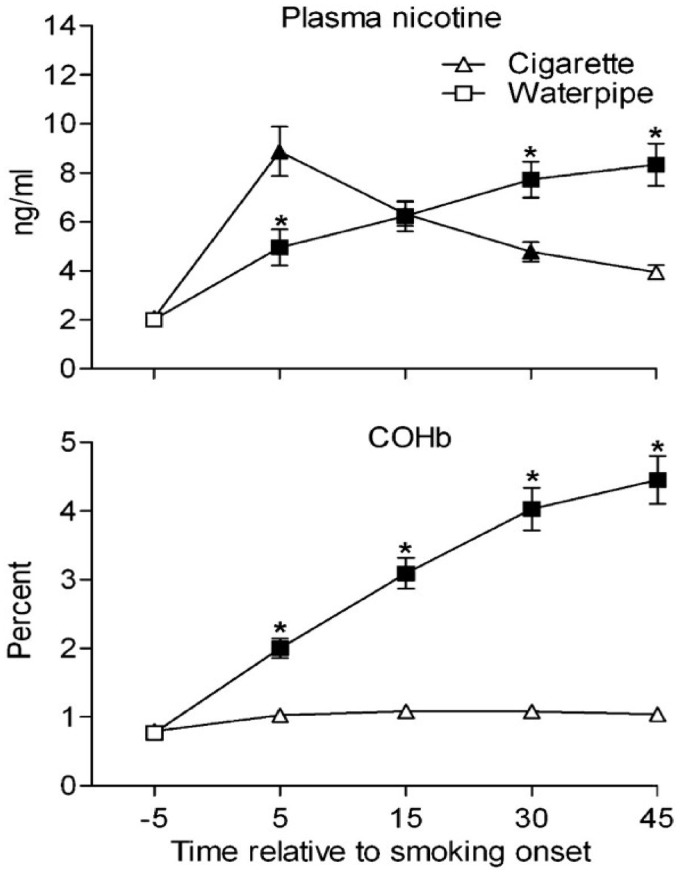
While quality studies of the long-term health effects of waterpipe smoking are scarce, available evidence suggest that it increases the risk for several serious health effects such as lung cancer, respiratory disease and low birth weight (Akl et al. 2010). These deleterious health effects are perhaps not surprising given that smoke from a waterpipe contains many of the same toxicants found in cigarette smoke, including nicotine that produces dependence, CO that causes cardiovascular disease, volatile aldehydes that cause pulmonary disease and polycyclic aromatic hydrocarbons (PAHs) that cause cancer (Table 2) (Maziak 2013b). In fact, due to the involvement of charcoal, some of the most deadly smoke toxicants (e.g. PAHs, CO), are produced at much greater levels in the waterpipe compared to cigarettes (Table 2) (Maziak 2013b). CO is a toxicant in cigarette smoke that has been implicated in cigarette-caused cardiovascular disease and the fact that a single waterpipe use episode exposes smokers to several times the CO compared to a single cigarette (and for extended periods) is particularly alarming. Reports of waterpipe-related emergency room admissions due to acute CO intoxication are beginning to accumulate, providing a cause for additional concerns (Cavus et al. 2010; Türkmen et al. 2011). A recent lab study comparing toxicant exposure between waterpipe and cigarette smoked by the same individual in a two-condition crossover design provides an elegant visualization of smoker CO and nicotine exposure in a single waterpipe use episode compared to a single cigarette (Figure 5) (Cobb et al. 2011) Particulate matter, another important toxicant for the cardiovascular system is also produced at higher levels during waterpipe smoking compared to cigarettes both in smoke and in the surrounding air (Monn et al. 2007; Maziak et al. 2008; Katurji et al. 2010; Schubert et al. 2011).
Table 2.
Comparison of smoke toxicants yield between waterpipe and cigarettea
| Waterpipe | Cigarette | Waterpipe/ cigarette | |
|---|---|---|---|
| ‘Tar’ (mg) | 802 | 15–29 | 8–53 |
| Nicotine (mg) | 3.09 | 1–3 | 1–3 |
| CO (mg) | 145 | 10–23 | 6–15 |
| PAH (ng) | |||
| Benzo(a)pyrene | 307 | 20–40 | 8–15 |
| Dibenz(a,h)anthracene | 147 | 4 | 37 |
| Indeno(1,2,3-cd)pyrene | 183 | 4–20 | 9–45 |
| Aldehydes (mg) | |||
| Formaldehyde | 630 | 70–100 | 6–9 |
| Acetaldehyde | 2520 | 500–1400 | 2–5 |
| Acrolein | 892 | 60–140 | 6–14 |
| Heavy metals (ng) | |||
| Arsenic | 165 | 40–120 | 1–4 |
| Chromium | 1340 | 4–70 | 19–335 |
| Lead | 6870 | 34–85 | 80–200 |
| Phenols (µg) | |||
| Phenol | 58.0 | 22.3 | 2.6 |
| o-Cresol | 4.41 | 5.79 | 0.8 |
| m-Cresol | 4.66 | 4.33 | 1.1 |
| p-Cresol | 5.38 | 10.1 | 0.5 |
| Catechol | 316 | 40.7 | 7.8 |
| Resorcinol | 1.69 | 0.79 | 2.1 |
| Hydroquinone | 111 | 34.6 | 3.2 |
aComparisons of machine-smoked waterpipe and cigarette using standard protocol for an average 1 h for waterpipe and 5 min for a cigarette [adapted from Maziak (2013b)].
Figure 5.
Mean (±SEM) for plasma nicotine and COHb. Filled symbols indicate a significant difference relative to the pre-smoking, and * indicate a significant difference between sessions (Cobb et al. 2011). SEM = Standard Error of Mean.
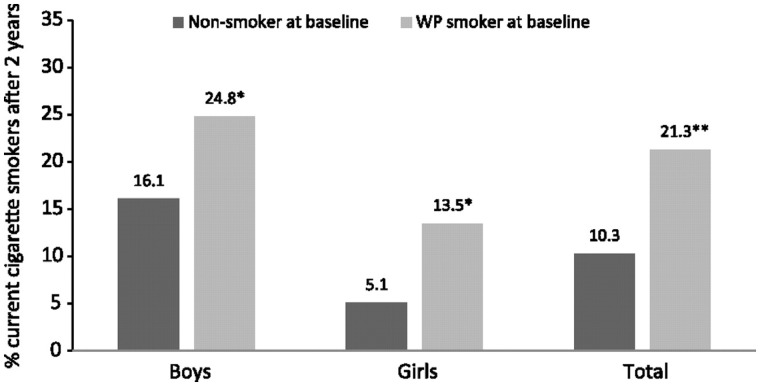
Increasingly among youth in the Arab world, waterpipe smoking initiation is occurring at a younger age than cigarettes (McKelvey et al. under review). This fact, combined with the addictive and generally non-portable nature of the waterpipe (i.e. remaining mobile while smoking a waterpipe is difficult) highlights the risk of waterpipe serving as a gateway to cigarettes. This hypothesis was tested recently in a longitudinal study by comparing cigarette smoking at two-year follow-up between children who were waterpipe smokers compared to those who were tobacco-naïve at baseline. Accordingly, waterpipe smokers at baseline were twice as likely to become current cigarette smokers at two-year follow-up (Figure 6) (Mzayek et al. 2012). Given the growing prevalence of waterpipe smoking, the potential of waterpipe to lead to cigarette smoking among Arab youth should be a catalyst for tobacco control in the region. If not, we predict a dramatic rise of cigarette smoking in the next 10 years, followed by increased rates of tobacco-caused death and disease in the next 20–30 years.
Figure 6.
Progression to current cigarette smoking among waterpipe smokers vs non-smokers at baseline. *P < 0.05, **P < 0.01 (Mzayek et al. 2012).
Tobacco control policy: an effective step towards eradication
The main drivers of the tobacco epidemic worldwide are well understood. Faced with increasing resistance in developed countries, the tobacco industry has shifted focus to developing countries, exploiting their less strong political, legal and civil society systems (Yach and Bettcher 2000). Industry efforts usually focus on economic activity (e.g. foreign investment and smuggling), promotion (e.g. targeting particular populations such as women), maintaining the social acceptability of tobacco (e.g. countering tobacco-control efforts), political activity (e.g. lobbying policy makers) and deception (e.g. manipulation of science) (WHO 2008a, b). The role of tobacco control advocates, therefore, involves a wide range of counter activities aimed at exposing industry tactics, building the evidence base about tobacco’s addictiveness and harm, testing potentially effective strategies and implementing policy.
The enormity and interconnectedness of the tobacco epidemic makes clear the need for a global policy approach. This approach is exemplified by the World Health Organization’s Framework Convention on Tobacco Control (FCTC), the first global health treaty. The FCTC aims at providing WHO member states with a co-ordinated roadmap towards the implementation of tobacco control policies with demonstrated effectiveness in diverse environments (Wipfli et al. 2004). These policies target both the demand and supply sides of the epidemic through price increases, bans on smoking in public places, packaging and labelling regulations, banning tobacco promotion and sponsorship, limiting minors’ access to tobacco, offering smoking cessation and fighting illicit tobacco trade (Nikogosian 2010). The two obvious caveats of a global approach are that (1) evidence created in one context may not translate to another and (2) policy based on cigarette control may not address effectively other tobacco use methods such as the waterpipe. In addition, we must understand that public policy works best in political systems that are accountable and responsive to their people, and that uphold the rule of law. All these issues are very relevant to tobacco control in the Arab world as discussed below.
The FCTC and the Arab world
Overall, 19 of 22 Arab countries have ratified the FCTC, yet few implement and even fewer enforce FCTC-mandated policies. For example, only seven Arab countries have enacted comprehensive smoking bans in public places, while the rest have partial or no bans, and enforcement remains low overall (WHO 2009a). A recent countrywide evaluation of smoking restrictions in recreational and public venues in Arab countries including Bahrain, Djibouti, Egypt, Iraq, Jordan, Lebanon, Oman, Sudan and Yemen indicated that of those evaluated only five showed complete compliance, whereas the rest had observed high smoking rates in public venues (WHO EMRO 2012). This low compliance rate suggests that many Arab countries allow an environment where populations of all ages are exposed to tobacco smoke in their everyday lives, and where the omnipresence of smoking contributes to the perception of smoking as a normative behaviour. Such perception is well known to influence a youth’s decision to try or initiate smoking, and discourages smokers from quitting and seeking cessation help (Alesci et al. 2003; Hamilton et al. 2008; Thrasher et al. 2009). Even fewer Arab countries commit to other policies mandated by the FCTC, such as large and pictorial warning labels, or banning tobacco advertisement and sponsorship. For example, few Arab countries (e.g. Jordan, Egypt, United Arab Emirates) require pictorial warning on tobacco packages, and even among those implementation is usually delayed. In Lebanon, legislation mandating larger textual and pictorial warnings has been in effect since 2011, but political commitment for enforcement still lags behind. Regarding taxation, the Eastern Mediterranean Region (EMR), where most of Arab countries are, has the lowest average consumer price and tax share of tobacco products compared to other WHO regions (WHO 2009b).
The political nuances for this policy paralysis can be different in different Arab countries, but their underlying roots can be found in a mixture of dysfunctional and corrupt political systems that are more sensitive to tobacco industry influence than the health needs of their people. In addition, the suppression of civic activity in undemocratic Arab world countries has deprived tobacco control in the region of one of its main allies. As a result, politicians are not open to public scrutiny, inquiry or litigation, leaving the pressure of vested interest on them unopposed.
A policy mismatch: the FCTC and waterpipe
The policies that are recommended were based mainly on evidence of controlling cigarette smoking. Accordingly, implementation of these policies for waterpipe faces shortfalls mainly due to the unique nature of this tobacco smoking method compared to cigarettes. So while a cigarette pack’s size and packaging modality is uniform all over the world and the cigarette tobacco industry is well defined, this is not the case for the waterpipe. Compared with cigarettes, the waterpipe is variable in shape and size, less portable, and is often shared. Those differences reflect on whether FCTC policies suite the waterpipe and how they need to be adapted for its nuances. For example, policies requiring detailed labelling for waterpipe tobacco and accessories are needed given what we know about its toxic contents. An evaluation of warning labelling practices on waterpipe tobacco products and related accessories in several Arab and non-Arab countries revealed that none of the waterpipe products purchased there were FCTC compliant. Moreover, misleading descriptors were common stating 0% nicotine, 0% tar on waterpipe tobacco packages (Nakkash and Khalil 2010). Since some of these countries (e.g. Canada, Germany) have strict labelling regulations for cigarettes, the paradoxical lax situation on waterpipe labelling indicates that some legislative and enforcement bodies are not considering FCTC labelling regulations applicable to the waterpipe. A related issue is that it is not sufficient to require health warnings on waterpipe tobacco packages only since there are many accessories associated with waterpipe smoking that need to be labelled as well. This is particularly relevant in light of the strong social dimension of waterpipe smoking. So in a coffee shop and restaurant setting waterpipe smokers are served the packed waterpipe and have no direct contact with the tobacco package.
The spread of waterpipe tobacco smoking also poses particular threat to proper enforcement of smoking bans in public places. Due to the high net profit margin gained from waterpipe sales in restaurants and cafés, indoor smoking bans are persistently challenged by waterpipe establishments. For example, despite the evidence of harmful ambient emissions associated with waterpipe smoking (Daher et al. 2010; Maziak et al. 2008), and laws banning all smoking indoors, enforcement is weak when it comes to the waterpipe in some Arab countries (e.g. Lebanon, Gulf states). Similar situations of waterpipe exemption from indoor air legislations have been noted even in countries with strong law enforcement. For example, a recent analysis of indoor smoking restrictions in major US cities found that most cities that disallow cigarette smoking in bars may permit waterpipe smoking via exemptions (Primack et al. 2012a).
With regard to advertising and promotion bans, waterpipe specificities can render them ineffective even if they are enforced. For example, a lot of waterpipe advertisement is done through the advertisement of accessories in a way that promotes the image of a healthier product. Advertisements of coal used in the waterpipe have touted new such products as ‘natural’ and made of ‘100% coconut shell’, smokeless, odourless and ‘free of chemicals’ (Khalil et al. 2009; Nakkash et al. 2011). Because of the visibility and social nature of waterpipe smoking moreover, much of its advertisement is done indirectly through the promotion of establishments serving the waterpipe. For example, many coffee shops display waterpipes on their windows as a decoration. The predominance of waterpipe smoking among the young and educated moreover, makes the internet an important venue for waterpipe promotion and sales, which is something to be considered to achieve the desired effect of tobacco advertisement bans for the waterpipe (Primack et al. 2012b).
The Arab world and waterpipe, therefore, provide an important case study for the mismatch between the FCTC and tobacco use methods other than cigarettes, and the need for FCTC articles to be adapted and tested to ensure effectiveness and sensitivity to such methods.
Tobacco industry efforts in the Arab world
The political atmosphere in many Arab world countries provides considerable opportunity for tobacco industry efforts to undermine tobacco control and to work tacitly with government officials to minimize the effect of policies on their markets and marketing activities. These efforts are revealed in industry internal documents and include circumventing the implementation of existing laws, and blocking passage of new ones (WHO 2002). With respect to the former, brand positioning market research that focuses on developing an in-depth understanding of young people has provided evidence that youth in the region have been a main target for the industry since the early 1970s. In Gulf countries such as the United Arab Emirates and Saudi Arabia, as well as in Lebanon, Syria and Jordan, tobacco industry research revealed a focus on age groups as young as 16 years (Nakkash and Lee 2009). Furthermore, the industry adopted strategies to circumvent and diffuse any tobacco control legislation in the region. Sponsorship of music and sports events served to evade advertising bans, and cross-border advertising techniques were used to reach ‘dark markets’ defined by the industry as countries with strict tobacco regulations. For example, the tobacco industry was able to bypass tobacco advertising bans in several Arab countries (e.g. Jordan, Syria) through satellite Lebanese TV stations and land border promotion (Hammond and White 2001a, b). The industry has also been complicit in smuggling activities. Smuggled products provide cheap alternatives for tobacco users, and allow the industry to reach otherwise closed or restricted markets. Evidence from the tobacco industry documents indicates how the industry took advantage of weak governance and the unstable security situation in Lebanon to access neighbouring countries’ markets, build market share and spread cheaper products (Nakkash and Lee 2008). Two main industry smuggling routes were through Lebanon and Cyprus to Iran and Iraq, both industry-attractive markets due to their market size (WHO EMRO 2003a,b). The internal tobacco industry documents suggest that smuggling was always happening with knowledge and complicity of the companies themselves (WHO 2002).
Working through either local surrogates of their own making or by lobbying members of ruling families or governments in Arab countries, the industry has aimed to disrupt tobacco control policy in the region. For example, one of the main players in industry interference in the Arab region has been members of the Middle East Tobacco Association (META) setup in the 1980s. Members of this association compiled information to lobby public officials and prominent figures from a number of countries (WHO EMRO 2003a,b). In addition, META developed a media strategy, which included sending letters to editors, and placing stories in top national and pan-Arab publications distorting science and promoting misinformation. In the early 1990s, META orchestrated the ‘voice of reason’ campaign that focused on building pro-industry opinion and targeted widely spread Arab press outlets (Hammond and White 2001a). More specifically in relation to advertisement bans that were under consideration by some countries of the Gulf Cooperation Council, META developed a media strategy paper that would be used to argue for marketing freedoms (Hammond and White 2001a).
The undemocratic and familial nature of many of Arab regimes provide an optimal entry point for the tobacco industry’s public relations efforts. Working with government officials the tobacco industry sought to delay and stall the discussion of any tobacco control related policy in the Arab Gulf Health Ministers conferences (Hammond and White 2001a, b). In Egypt, a leading member of parliament assured the industry that no advertising bans would pass parliament, though a law nevertheless was passed (WHO EMRO 2001). In response, the industry continued to lobby against the issuance of an executive order banning advertising (Hammond and White 2001a, b). In Lebanon, the industry succeeded in blocking a few attempts for marketing and advertising restrictions in the 1980s through 1990s (Nakkash and Lee 2008). In other countries (e.g. Bahrain, Kuwait, UAE, Oman) the tobacco industry employed a mixture of tactics based on cautioning against loss of revenue, promoting free markets and defending smokers’ rights to oppose the adoption of tobacco advertisement bans. These same tactics were used to circumvent other important tobacco control policies such as raising taxes on tobacco products (Hammond and White 2001a, b).
Many Arab countries officials continue to interact with tobacco industry representatives despite the clear conflict of interest this represents under their obligations to FCTC article 5.3. For example, the tobacco industry continues to engage with the staff of several ministries in the region under the auspices of providing anti-smuggling training. They at times choose to blatantly disregard advertising and sponsorship bans as in the case of Jordan, where they continued to post the same advertisement but without the name of the brand, or in Lebanon as they continued their distribution of tobacco products in nightclubs and pubs after such ban went into (Salloum et al. 2013). This documented meddling has greatly contributed towards the delayed tobacco control regulations in many Arab countries and current status quo.
Tobacco control in the Arab world: a growing movement
Despite the grim picture of the tobacco epidemic in the Arab world and the status of policy paralysis, tobacco control legislation and programmes in the region have had some success. Key factors in these successes were governmental and civil society involvement, and the engagement and leadership of academia. For example, the Palestinian ministry of health in partnership with the legislative council, academia and various health-related non-governmental organizations (NGOs) were able to sponsor a comprehensive tobacco control law in the Occupied Palestinian Territory in 2005. A similar story of multi-sector partnership to advance tobacco control policy took place in Lebanon, which ratified the FCTC in 2005, but did not meet its policy obligations under this treaty until 2011. Here, the American University of Beirut’s Tobacco Control Research Group joined efforts with civil society groups—IndyAct and Tobacco Free Initiative—in the push for the adoption of a comprehensive tobacco control law. Their strategy was to lead an intensive and sustained multimedia advocacy campaign targeting three main groups: policy makers (parliamentarians responsible for enacting the law), media and NGOs. This concerted and multi-sectorial effort culminated with the passage of a comprehensive and strong tobacco control law (law 174) on 17 August 2011, and the law came into effect a year later (R Nakkash, personal communication). In Jordan, despite the pioneer implementation of strong tobacco control policies (e.g. large health and pictorial warnings) there was a realization that smokers willing to quit were left without cessation support and help. To fill this gap the Jordanian Ministry of Health and King Hussein Cancer Center worked together to establish the first cessation clinics in the country. These clinics provided smoking cessation services based on best international practices and trained scores of smoking cessation counselors in and outside the country. In Syria, the Syrian Center for Tobacco Studies worked with NGOs and Ministry of Health officials to influence the passage of a law that bans smoking in public places, and included a clear clause about the waterpipe for the first time in the region (BBC NEWS 12 April 2010).
In addition to local initiatives to advance tobacco control policies, a remarkable contribution of tobacco control professionals in the Arab world has been to the creation of an evidence base regarding tobacco use and effects, especially in relation to waterpipe smoking. As the waterpipe epidemic is spreading to all corners of the globe, the work of Arab scientists in this field has paved the way for an evidence-based response to this new epidemic. Scientists and centres in the Arab world were the first to characterize the addictive properties of waterpipe, measure major toxicants in waterpipe’s smoke, demonstrate smokers’ exposure to these toxicants, conduct studies of the acute effects of waterpipe smoking and specify waterpipe toxic emissions that can harm non-smokers (e.g. Monzer et al. 2008; Sepetdjian et al. 2008; Daher et al. 2010; Maziak 2013b). Their work was truly collaborative in a region where collaboration is not the norm due to regional tensions and the scarcity of specialized research bases. Involving scientists and institutions in the USA and Europe has helped to advance these collaborations by allowing regional scientists better access to required expertise and funding opportunities. The success of this unique scientific collaboration is supported by an outstanding record of scientific reports, training initiatives and overall impact within and beyond the Arab region (e.g. Maziak et al. 2004; Hammal et al. 2008; Cobb et al. 2010; Mzayek et al. 2012).
The way forward
The tobacco epidemic in the Arab world is at a transitional stage, where cigarette smoking among men continues to be the main threat to the health and wellbeing of local communities, whereas waterpipe tobacco smoking is spreading among youth and women. The FCTC provides a promising path for tobacco control in the region, but the challenges associated with poor implementation of FCTC policies are formidable. These challenges are mostly due to the lack of true political commitment to tobacco control, tobacco industry tactics and weak civil society, which is usually instrumental in driving public health policies. In addition, the FCTC speaks primarily to cigarette smoking and suggests polices that are based on research completed in developed countries. Thus, while better implementation and enforcement of FCTC policies holds the promise of decreasing cigarette smoking in the Arab world, locally based evidence and policy must be generated to deal with the emerging waterpipe epidemic. An essential starting point for all these efforts lies in establishing reliable population-based surveillance for tobacco use in Arab countries, and the use of such data to inform tobacco control strategies and priorities.
On that grim backdrop, local tobacco control initiatives in the Arab world have been able to put tobacco control issues on the radar of local governments and achieve limited success. The main ingredients of these successes were the ability to build coalitions of civil society, academia and health professionals that provided an unrelenting and multi-channeled pressure on politicians and policy makers. The involvement of the local academia in contributing to the evidence base to inform such policies seems to be of paramount importance to energize and at times lead public health advocacy for tighter tobacco control.
The current instability and uncertainty engulfing the Arab world will surely influence tobacco control outlook in ways that are yet hard to predict. These events will likely move tobacco control backwards on Arab governments’ and people priorities, and can disrupt already weak regional tobacco control networks. Yet the emergence of political systems in the region that are more representative and accountable to their people can create environments more susceptible to public health advocacy. At the same time, the rise of civil society all over the region revealed the power of youth activism when equipped with new forms of communication and social media. All these dynamics can be exploited to build broad coalitions that can apply co-ordinated pressure for tobacco control nationally and region wide. But for this to happen, the tobacco control community need to be ahead of the curve and prepared for totally different political, economic and social realities in the Arab region. With this perspective in mind, focusing on the generation of local evidence, applying civil society pressure and better use of the media can acquire increasing importance for the future of tobacco control in this region. The economic hardship resulting from the recent dramatic changes in Arab countries can also provide an opening for an economic-based rational to advance tobacco control.
The grim perspective of the tobacco control situation in the Arab world despite mass FCTC ratification can still be turned around in a region undergoing major transformations. Readers may think that this statement sounds like ‘wishful thinking’. If so, remember that, if the recent uprisings are any indication, the Arab world still holds some surprises.
Funding
This work is partially supported by the National Institute on Drug Abuse (NIDA) grants R01 DA024876 and R01 DA035160.
Conflict of interest
None declared.
References
- Akl EA, Gaddam S, Gunukula SK, et al. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. International Journal of Epidemiology. 2010;39:834–57. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- Akl EA, Gunukula SK, Aleem S, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine. 2003;36:272–81. doi: 10.1016/s0091-7435(02)00029-4. [DOI] [PubMed] [Google Scholar]
- Ali AYM, Safwat T, Onyemelukwe G, et al. Smoking prevention and cessation in the Africa and Middle East region: a consensus draft guideline for healthcare providers—executive summary Respiration. International Review of Thoracic Diseases. 2012;83:423–32. doi: 10.1159/000337726. [DOI] [PubMed] [Google Scholar]
- Al-Mulla AM, Abdou Helmy S, Al-Lawati J, et al. Prevalence of tobacco use among students aged 13-15 years in Health Ministers’ Council/Gulf Cooperation Council Member States, 2001-2004. Journal of School Health. 2008;78:337–43. doi: 10.1111/j.1746-1561.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- Asfar T, Weg MV, Maziak W, et al. Outcomes and adherence in Syria’s first smoking cessation trial. American Journal of Health Behavior. 2008;32:146–56. doi: 10.5555/ajhb.2008.32.2.146. [DOI] [PubMed] [Google Scholar]
- BBC NEWS. “Syria smoking ban enters into force”. BBC.com. 21 April 2010. http://news.bbc.co.uk/2/hi/middle_east/8634411.stm, accessed 10 December 2012. [Google Scholar]
- Cavus UY, Rehber ZH, Ozeke O, Ilkay E. Carbon monoxide poisoning associated with narghile use. Emergency Medicine Journal. 2010;27:406. doi: 10.1136/emj.2009.077214. [DOI] [PubMed] [Google Scholar]
- Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. American Journal of Health Behavior. 2010;34:275. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine & Tobacco Research. 2011;13:78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daher N, Saleh R, Jaroudi E, et al. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmospheric Environmen, 2010;44:8–14. doi: 10.1016/j.atmosenv.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Awa F, Warren C, Jones N. Changes in tobacco use among 13–15-year-olds between 1999 and 2007: findings from the Eastern Mediterranean Region. Eastern Mediterranean Health Journal. 2010;16:266–73. [PubMed] [Google Scholar]
- Eriksen M, Mackay J, Ross H, editors. The Tobacco Atlas. 4th. Atlanta, GA: American Cancer Society; 2012. [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update—Clinical Practice Guidelines. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- Global Tobacco Surveillance System Collaborating Group. Global Tobacco Surveillance System (GTSS): purpose, production, and potential. Journal of School Health. 2005;75:15–24. doi: 10.1111/j.1746-1561.2005.tb00004.x. [DOI] [PubMed] [Google Scholar]
- Hamilton WL, Biener L, Brennen RT. Do local tobacco regulations influence perceived smoking norms? Evidence from adult and youth surveys in Massachusetts. Health Education Research. 2008;23:709–22. doi: 10.1093/her/cym054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammal F, Mock J, Ward K, Eissenberg T, Maziak W. A pleasure among friends: how narghile (waterpipe) smoking differs from cigarette smoking in Syria. Tobacco Control. 2008;17:e3. doi: 10.1136/tc.2007.020529. [DOI] [PubMed] [Google Scholar]
- Hammond R, White CM. Voices of Truth, Vol. 1: Multinational Tobacco Industry Activity in the Middle East: A Review of Internal Industry Documents. 2001a. Center for Tobacco Control Research and Education, UC San Francisco; World Health Organization Regional Office for the Eastern Mediterranean, Cairo, Egypt. http://www.emro.who.int/TFI/TFIonthemove-VoiceOfTruth.htm, accessed 8 March 2012. [Google Scholar]
- Hammond R, White C. Voices of Truth, Vol. 2: Multinational Tobacco Industry Activity in the Middle East: A Review of Internal Industry Documents. (No. qt1v6935q0) 2001b. Center for Tobacco Control Research and Education, UC San Francisco; World Health Organization Regional Office for the Eastern Mediterranean, Cairo, Egypt. http://www.emro.who.int/TFI/VoiceOfTruthVol2.pdf, accessed 12 March 2012. [Google Scholar]
- Jabbour S, Giacaman R, Khawaja M, Nuwayhid I, Yamout R, editors. Public Health in the Arab World. 1st. New York: Cambridge University Press; 2012. [Google Scholar]
- Jasim S, Kadhim L, El-Awa F, et al. Tobacco use among students aged 13-15 years-Baghdad, Iraq, 2008. Morbidity and Mortality Weekly Report. 2009;58:305–8. [PubMed] [Google Scholar]
- Katurji M, Daher N, Sheheitli H, Saleh R, Shihadeh A. Direct measurement of toxicants inhaled by water pipe users in the natural environment using a real-time in situ sampling technique. Inhalation Toxicology. 2010;22:1101–9. doi: 10.3109/08958378.2010.524265. [DOI] [PubMed] [Google Scholar]
- Khalil J, Heath RL, Nakkash RT, Afifi RA. The tobacco health nexus? Health messages in narghile advertisements. Tobacco Control. 2009;18:420–1. doi: 10.1136/tc.2009.030148. [DOI] [PubMed] [Google Scholar]
- Macaron C, Macaron Z, Maalouf MT, Macaron N, Moore A. Urinary cotinine in narguila or chichi tobacco smokers. Journal Medical Libanais. 1997;45:19–20. [PubMed] [Google Scholar]
- Mackay J, Crofton J. Tobacco and the developing world. British Medical Bulletin. 1996;52:206–21. doi: 10.1093/oxfordjournals.bmb.a011527. [DOI] [PubMed] [Google Scholar]
- Martinasek MP, Mcdermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Current Problems in Pediatric and Adolescent Health Care. 2011;41:34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Maziak W. The crisis of health in a crisis ridden region. International Journal of Public Health. 2009;54:349–55. doi: 10.1007/s00038-009-0061-7. [DOI] [PubMed] [Google Scholar]
- Maziak W. The global epidemic of waterpipe smoking. Addictive Behaviors. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. Am J Addict. 2013a. The waterpipe; a new way of hooking youth on tobacco. Jun 10. doi:10.1111/j.1521-0391.2013.12073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. The waterpipe: an emerging global risk for cancer. Cancer Epidemiology. 2013b;37:1–4. doi: 10.1016/j.canep.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Ward K. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacology Biochemistry and Behavior. 2005;80:173–9. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ibrahim I, Rastam S, Ward KD, Eissenberg T. Waterpipe-associated particulate matter emissions. Nicotine & Tobacco Research. 2008;10:519–23. doi: 10.1080/14622200801901989. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward K, Soweid RAA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tobacco Control. 2004;13:327–33. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mckelvey K, Wilcox M, Madhivanan P, et al. under review. Time-trends of cigarette and waterpipe smoking among a cohort of school children in Irbid, Jordan 2008-2011. Adolescent Health. doi: 10.1093/eurpub/ckt140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monn C, Kindler P, Meile A, Brändli O. Ultrafine particle emissions from waterpipes. Tobacco Control. 2007;16:390–3. doi: 10.1136/tc.2007.021097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food and Chemical Toxicology. 2008;46:2991–5. doi: 10.1016/j.fct.2008.05.031. [DOI] [PubMed] [Google Scholar]
- Mzayek F, Khader Y, Eissenberg T, et al. Patterns of water-pipe and cigarette smoking initiation in schoolchildren: Irbid Longitudinal Smoking Study. Nicotine & Tobacco Research. 2012;14:448–54. doi: 10.1093/ntr/ntr234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash R, Khalil J. Health warning labeling practices on narghile (shisha, hookah) waterpipe tobacco products and related accessories. Tobacco Control. 2010;19:235–9. doi: 10.1136/tc.2009.031773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash R, Lee K. Smuggling as the “key to a combined market”: British American Tobacco in Lebanon. Tobacco Control. 2008;17:324–31. doi: 10.1136/tc.2008.025254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash R, Lee K. The tobacco industry’s thwarting of marketing restrictions and health warnings in Lebanon. Tobacco Control. 2009;18:310–6. doi: 10.1136/tc.2008.029405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakkash RT, Khalil J, Afifi RA. The rise in narghile (shisha, hookah) waterpipe tobacco smoking: a qualitative study of perceptions of smokers and nonsmokers. BMC Public Health. 2011;11:315. doi: 10.1186/1471-2458-11-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikogosian H. WHO framework convention on tobacco control: a key milestone. Bulletin of the World Health Organization. 2010;88:83. doi: 10.2471/BLT.10.075895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Hopkins M, Hallett C, et al. US health policy related to hookah tobacco smoking. American Journal of Public Health. 2012a;102:e47–e51. doi: 10.2105/AJPH.2012.300838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Rice KR, Shensa A, et al. US hookah tobacco smoking establishments advertised on the internet. American Journal of Preventive Medicine. 2012b;42:150–6. doi: 10.1016/j.amepre.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastam S, Ward KD, Eissenberg T, Maziak W. Estimating the beginning of the waterpipe epidemic in Syria. BMC Public Health. 2004;4:32. doi: 10.1186/1471-2458-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloum RG, Nakkash RT, Myers AE, Woods KA, Ribisl KM. Point-of-sale tobacco advertising in Beirut, Lebanon following a national advertising ban. BMC Public Health. 2013;13:534. doi: 10.1186/1471-2458-13-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert J, Hahn J, Dettbarn G, et al. Mainstream smoke of the waterpipe: does this environmental matrix reveal as significant source of toxic compounds? Toxicology Letters. 2011;205:279–84. doi: 10.1016/j.toxlet.2011.06.017. [DOI] [PubMed] [Google Scholar]
- Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food and Chemical Toxicology. 2008;46:1582–90. doi: 10.1016/j.fct.2007.12.028. [DOI] [PubMed] [Google Scholar]
- Tamim H, Al-Sahab B, Akkary G, et al. Cigarette and nargileh smoking practices among school students in Beirut, Lebanon. American Journal of Health Behavior. 2007;31:56–63. doi: 10.5555/ajhb.2007.31.1.56. [DOI] [PubMed] [Google Scholar]
- Thrasher J, Boado M, Sebrie E, Bianco E. Smoke-free policies and the social acceptability of smoking in Uruguay and Mexico: findings from the International Tobacco Control Policy Evaluation Project. Nicotine & Tobacco Research. 2009;11:591–9. doi: 10.1093/ntr/ntp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Türkmen S, Eryigit U, Sahin A, Yeniocak S, Turedi S. Carbon monoxide poisoning associated with water pipe smoking. Clinical Toxicology. 2011;49:697–8. doi: 10.3109/15563650.2011.598160. [DOI] [PubMed] [Google Scholar]
- Ward KD, Asfar T, Al Ali R, et al. Randomized trial of the effectiveness of combined behavioral/pharmacological smoking cessation treatment in Syrian primary care clinics. Addiction. 2013;108:394–403. doi: 10.1111/j.1360-0443.2012.04048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KD, Hammal F, Vanderweg MW, et al. Are waterpipe users interested in quitting? Nicotine and Tobacco Research. 2005;7:149–56. doi: 10.1080/14622200412331328402. [DOI] [PubMed] [Google Scholar]
- Ward KD, Eissenberg T, Rastam S, et al. The tobacco epidemic in Syria. Tobacco Control. 2006;15(Suppl. 1):i24–9. doi: 10.1136/tc.2005.014860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren C, Jones N, Eriksen M, Asma S. Patterns of global tobacco use in young people and implications for future chronic disease burden in adults. The Lancet. 2006;367:749–53. doi: 10.1016/S0140-6736(06)68192-0. [DOI] [PubMed] [Google Scholar]
- WHO. The Tobacco Industry Documents: What They are, What They Tell Us, and How to Search Them. A Practical Manual. Geneva, Switzerland: World Health Organization; 2002. WHO-EM/TF1/005/E/G. [Google Scholar]
- WHO. Tobacco Industry Interference with Tobacco Control. Geneva, Switzerland: World Health Organization; 2008a. [Google Scholar]
- WHO. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. Geneva, Switzerland: World Health Organization; 2008b. http://whqlibdoc.who.int/publications/2008/9789241596282_eng.pdf, accessed 2 April 2012. [Google Scholar]
- WHO. Tobacco Free Initiative: Country Profile. Geneva, Switzerland: World Health Organization; 2009a. www.who.int/tobacco/surveillance/policy/country_profile/en/index.html, accessed 1 November 2012. [Google Scholar]
- WHO. Chapter II: Tobacco Tax Levels and Structure: A Theoretical and Empirical Overview. Geneva, Switzerland: World Health Organization; 2009b. http://www.who.int/tobacco/publications/en_tfi_tob_tax_chapter2.pdf, accessed 3 November 2012. [Google Scholar]
- WHO. WHO REPORT ON THE GLOBAL TOBACCO EPIDEMIC, 2009: Implementing Smoke-free Environments. Geneva, Switzerland: World Health Organization; 2009c. http://www.who.int/tobacco/mpower/2009/gtcr_download/en/index.html, accessed 17 April 2013. [Google Scholar]
- WHO. Global Youth Tobacco Survey, Country Fact Sheets: West Bank (Ages 13-15) Global Youth Tobacco Survey (GYTS) Fact Sheet, 2009. Geneva, Switzerland: World Health Organization; 2010. http://www.emro.who.int/images/stories/tfi/documents/GYTS_FS_WEST_BANK_R3.pdf, accessed 1 April 2013. [Google Scholar]
- WHO. WHO Report on the Global Tobacco Epidemic, 2011: Warning about the Dangers of Tobacco. Geneva, Switzerland: World Health Organization; 2011. http://www.who.int/tobacco/global_report/2011/appendix_vii/en/index.html, accessed 17 April 2013. [Google Scholar]
- WHO EMRO. Coveting Iran: The Infiltration and Exploitation of Iran by Global Cigarette Companies. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2001. [Google Scholar]
- WHO EMRO. The Cigarette “Transit” Road to the Islamic Republic of Iran and Iraq: Illicit Tobacco Trade in the Middle East. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2003a. WHO-EM/TFI/011/E/G/07.03/1000. http://www.emro.who.int/TFI/TFIiraniraq.pdf, accessed 13 June 2012. [Google Scholar]
- WHO EMRO. The Tobacco Industry’s Tactics and Plans to Undermine Control Efforts in Egypt and North Africa. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2003b. http://www.emro.who.int/TFI/tfiegypt.pdf, accessed 17 August 2012. [Google Scholar]
- WHO EMRO. Exposure to Second-hand Smoke in Selected Public Places in the WHO Eastern Mediterranean Region: Report of a Pilot Study. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2012. [Google Scholar]
- Wipfli H, Stillman F, Tamplin S, et al. Achieving the framework convention on tobacco control’s potential by investing in national capacity. Tobacco Control. 2004;13:433–7. doi: 10.1136/tc.2003.006106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yach D, Bettcher D. Globalization of tobacco industry influence and new global responses. Tobacco Control. 2000;9:206–16. doi: 10.1136/tc.9.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]