Abstract
Introduction Injuries are a significant cause of mortality and morbidity, of which more than 90% occur in low- and middle-income countries (LMICs). Given the extent of this burden being confronted by LMICs, there is need to place injury prevention at the forefront of public health initiatives and to understand the costs associated with injury. The aim of this article is to describe the extent to which injury-related costing studies have been conducted in LMICs.
Methods A review of literature was performed to explore costing data available for injury and/or trauma care in LMICs. Study quality was described using recommendations from the Community Guide’s quality assessment tool for economic evaluations.
Results The review identified 68 studies, of which 13 were full economic evaluations. Cost of injury varied widely with mean costs ranging from US$14 to US$17 400. In terms of injury-prevention interventions, cost per disability adjusted life year averted for injury-prevention interventions ranged from US$10.90 for speed bump installation to US$17 000 for drunk driving and breath testing campaigns in Africa. The studies varied in quality, ranging from very good to unsatisfactory.
Discussion There is a lack of injury-related economic evidence from LMICs. Current costing research has considerable variability in the costs and cost descriptions of injury and associated prevention interventions. The generalizability of these studies is limited. Yet the economic burden of injury is high, suggesting significant potential for cost savings through injury prevention. A standardized approach to economic evaluation of injury in LMICs is needed to further prioritize investing in injury prevention.
Keywords: Injury, trauma, economic evaluation, costs, developing countries
KEY MESSAGES.
The economic burden of injury and trauma care is high in LMICs, suggesting significant potential for cost savings through injury prevention.
A standardized approach to economic evaluation of injury in LMICs is needed to further prioritize investing in injury prevention.
Introduction
Injuries are a significant cause of mortality and morbidity, accounting for ∼5.8 million or 10% of global deaths per year (World Health Organization, 2008). The magnitude of the burden of injury is alarming when compared to other diseases: there are 32% more deaths from injuries than from AIDS, tuberculosis (TB) and malaria combined (World Health Organization, 2008). More than 90% of these injury-related deaths occur in low- and middle-income countries (LMICs).
Given the extent of this burden being confronted by LMICs, there is need to place injury prevention at the forefront of public health initiatives. Yet this is not happening. Efforts to promote injury prevention have not received the attention and prioritization of diseases such as HIV/AIDS, TB and malaria. If injury mortality and morbidity data have failed to convince policy-makers to invest in injury prevention, there is a need to explore alternative ways to advocate for injury prevention. One approach is to consider the costs associated with injury and the cost-effectiveness of injury-prevention interventions.
Nearly half of injury-related mortality occurs in individuals aged 15 to 44 years during their most economically productive years (Nilsen et al., 2006). This makes the financial burden of injuries far exceed the immediate medical costs associated with the injury. As such, more comprehensive injury-related cost studies that describe not only medical costs, but also those related to the consequences of injury to the individual, family and society, such as productivity losses, can be used to inform policies and interventions at the local and national levels.
In addition to describing the cost of injuries, there is also a need to describe the cost-effectiveness of injury-prevention initiatives. While a key first step in injury prevention requires obtaining evidence on the effectiveness of interventions, potential effectiveness is only part of a policy-maker’s decision to invest in a prevention programme (Zaza et al., 2005). With limited resources and competing health needs, the costs of an intervention in relation to the benefits must also be taken into account.
The increased use of cost calculations to implement injury-prevention efforts has been encouraged by the World Health Organization (WHO) and the Disease Control Priorities Project (DCPP) (World Health Organization, 2011a; Jamison et al., 2006). While systematic reviews have explored the cost-effectiveness of injury prevention in high income countries (HICs), this represents less than 10% of the global burden of injury and conclusions drawn from reviews from HICs may not be transferable to LMICs (Gyllensvard, 2010; Waters et al., 2004; Scuffham, 2008).
There is a need to review the literature in the context of LMICs; to the best of our knowledge, this has not previously been done. The aim of this article is thus to describe the extent to which injury-related costing studies have been conducted in LMICs. The specific objectives of this article are 3-fold: to summarize the body of economic evidence on injury in LMICs; to assess the quality of cost-effectiveness studies using standard methods to highlight the role of economic data as a tool for injury-prevention advocacy; and to provide recommendations regarding economic evaluations in LMICs.
Methods
We searched Medline/PubMed (National Library of Medicine, 2013), EconLit (American Economic Association, 2013), Econbase (Elsevier Inc., 2013a), Embase (Elsevier Inc., 2013b) the Cochrane Library (The Cochrane Collection, 2013) and the National Health Service Economic Evaluation Database (National Institute for Health Research, 2013) to identify articles published before February 2013 that pertained to costs associated with injury in LMICs using key words presented in the Appendix. Citations and reference lists were reviewed to identify any additional studies (Littell et al., 2008). Since this was a review of published literature only, the ‘grey’ literature was not searched.
We assessed each study for inclusion using three criteria. First, included studies had to use costing data from LMICs. We defined a LMIC according to the World Bank’s classification of a country with a gross national income per capita of less than US$12 195 in 2011 (World Bank, 2011). Second, studies had to describe either injuries, an injury classification (i.e. road traffic injures (RTIs), burns, falls, drowning and violence), or trauma care defined as pre-hospital and hospital-based trauma care services (World Health Organization, 2008). Third, studies had to use either a cost-related partial evaluation or full economic evaluation. We included cost-related partial evaluations in our review because they represent important initial work in LMICs to describe the economic burden of injury (Drummond et al., 2005). These partial economic evaluations were grouped into four categories: 1) ‘cost description’ which examined only costs without a comparison to alternative outcomes; 2) ‘cost analysis’ which compared alternatives in terms of costs only; 3) ‘cost-outcome description’ which examined both costs and outcomes, but did not compare alternatives; and 4) ‘outcome analysis’ which compared alternatives in terms of outcome only (Drummond et al., 2005). Full economic evaluations included cost-effectiveness analysis, cost-utility analysis and cost-benefit analysis (Drummond et al., 2005).
Review articles, commentaries and editorials were excluded. Studies that did not report the currency unit for the reported costs were excluded. To avoid double counting, duplicate data presented in multiple publications were excluded; in these instances, the earlier publication was included. For the purposes of this review, we excluded poisoning, occupational injuries and disaster-related injuries given that the underlying causes of these injury classifications and the associated costs were too broad for the scope of this review. Injuries that were defined according to an anatomical location were excluded. This included head (including traumatic brain injuries), spinal cord and orthopaedic-related injuries. Studies that looked at only one type of cost, such as the cost of a particular dressing or wound care, were excluded as these costs were too narrow for this review.
Information regarding the study design and findings in terms of costs and outcomes was extracted and tabulated. To maximize comparisons among studies, we standardized costs when applicable. All costs were converted to US dollars (US$) for 2010 using gross domestic product (GDP) deflators and purchasing power parities (Shemilt et al., 2009).
For partial evaluation studies, mean costs were reported in the units described by the individual study, such as the cost per hospitalization or the cost per injury. The cost per hospitalization differed from cost of injury depending on whether the study included costs that would be incurred outside of the injured patient’s hospital admission. To describe this, the types of costs presented by the partial evaluation studies were tabulated into three categories: direct medical costs, direct non-medical costs and indirect costs. Medical costs are those costs incurred during the hospital inpatient stays, out-patient stays, hospital stay, medicine, surgery, emergency department visits, prostheses and wound-care dressings, radiological, laboratory and specialist consultation costs. Direct non-medical costs included administration costs (which included the medico-legal costs, cost administration, costs of police activity and insurance administration, funeral costs, transportation, non-medical material costs, and food and accommodation of the patient and/or family members. Indirect costs include loss of income, cost of premature death, pain and suffering and the cost of restricted activity (Drummond et al., 2005).
We tabulated the median and range of reported mean costs for partial evaluation studies, describing this in terms of those studies that reported costs as (1) direct medical costs only, (2) direct medical and non-medical costs and (3) direct medical and non-medical costs and indirect costs. To further compare costs among partial economic studies, when applicable, costs were reported as a percentage of GDP per capita for 2010, as reported by the World Bank (World Bank, 2013).
For full economic studies, costs were reported in units of costs per disability-adjusted life year (DALY) averted, per death averted and per years of life gained, as defined by the individual study. We described the quality of these studies using recommendations from the Community Guide’s quality assessment tool for economic evaluations (Community Guide, 2010). Of note, because this tool is designed for full economic evaluations, we did not apply the Community Guide to the partial evaluations. Quality was systematically assessed across five categories: study design, cost data, outcome measure, effects and analysis. A quality score was assigned to each study using the Community Guide quality assessment criteria. For full economic evaluation studies that did not require expert opinion, the respective categories were labelled as not applicable and the quality assessment score was adjusted to account for this. The score was then converted into ratings of very good, good, satisfactory and unsatisfactory. Following the Community Guide’s recommendations that stipulate studies with an unsatisfactory score should be discarded, we assessed studies that achieved a score of satisfactory or higher to then determine if the intervention was cost-effective (Community Guide, 2010). For those studies that reported costs in terms of life year saved or DALY averted, the interventions were described as very cost-effective, cost-effective or not cost-effective using World Health Organization Choosing Interventions that are Cost Effective (WHO-CHOICE) guidelines. These guidelines define a ‘very cost-effective’ intervention as an intervention that produces a healthy year of life for less than the GDP per capita, a ‘cost-effective’ intervention as producing a health year of life for less than three times GDP per capita and a ‘non-cost-effective’ intervention as producing a health year of life for more than three times GDP per capita (World Health Organization, 2003).
Given the lack of generalizability among studies, we did not conduct a meta-analysis (Drummond and Pang, 2001). We used the results to summarize the strength of the body of the evidence regarding injury in LMICs and identify research gaps.
Results
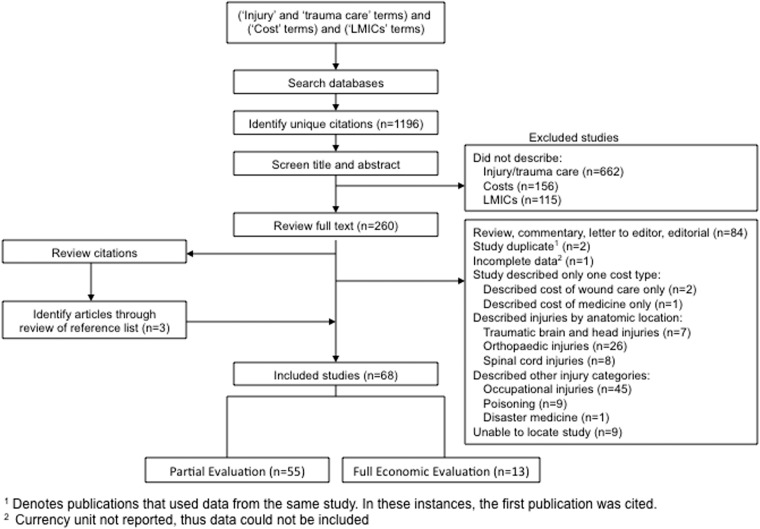
Sixty-eight of the initially identified 1196 unique citations met our inclusion criteria (Figure 1). Fifty-five studies were partial evaluations and 13 were full economic evaluations. Nearly half of partial evaluation studies were hospital based (n = 27/55; 49%), of which the majority were single-centre studies (n = 21/27; 78%). Fifteen studies described injuries in general; in terms of types of injury, the majority of studies described RTIs (n = 31/68; 46%), followed by burn injuries (n = 11/68; 16%). Six studies described trauma care, of which four described pre-hospital trauma care. While most studies were conducted in urban settings (n = 51), used national data (n = 6), or used data from both urban and rural areas (n = 8), three studies were exclusively set in rural areas.
Figure 1.
Literature review flowchart
Partial evaluation studies included 48 cost description studies, two cost-outcome description studies, three cost-analysis studies, and two outcome analysis studies that focused on RTIs, burns, violence and injuries (Table 1). Costs were presented in units of cost per hospitalization (n = 30 including one study of emergency room visits), cost per injury (n = 17), cost per fatality (n = 1), cost per safety intervention or device (n = 3), years of potential life lost (n = 1), years of lost productivity (n = 1) and total cost of injury (n = 2).
Table 1.
Partial evaluation studies of the costs of injuries, treatment and prevention in LMICs (n = 55)
| Author, year | Study location | Study setting | Study sample | Outcome | Cost (US$ 2010) | Unit (mean cost per) | Cost as a % of GDP/ capita | Direct medical costs | Direct non- medical costs | Indirect costs |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. RTIs (n = 25) | ||||||||||
| Cost description | ||||||||||
| Jadaan, 1989 | Jordan | Urban (one hospital) | N/A | N/A | $99 | Per hospitalization | 2% | X | ||
| Arokiasamy and Krishnan, 1994 | Malaysia | National | 2354 fatal RTIs | N/A | $129 000 | Per injury | 1484% | X | ||
| Al-Masaeid et al., 1999 | Jordan | Urban and Rural | 552 fatal RTIs | N/A | $4200 | Per fatality | 96% | X | X | X |
| Olukoga, 2004 | South Africa | Urban and Rural | N/A | N/A | Minor: $3970 | Per injury | 55% | X | X | X |
| Major: $14 800 | 200% | |||||||||
| Fatal: $64 700 | 890% | |||||||||
| Anh et al., 2005 | Vietnam | National | 26 925 RTIs | N/A | $8,770 | Per injury | 717% | X | X | X |
| De Leon, 2005 | Philippines | National | N/A | N/A | Minor: $1560 | Per injury | 73% | X | X | X |
| Major: $16 100 | 752% | |||||||||
| Fatal: $75 900 | 3546% | |||||||||
| Hassan et al., 2005 | Kenya | Urban (one hospital) | 136 RTIs | N/A | $140 | Per hospitalization | 18% | X | ||
| Jianping et al., 2006 | China | Urban | 420 RTIs | N/A | $720 | Per hospitalization | 16% | X | ||
| Yan-Hong et al., 2006 | China | National | N/A | N/A | $766 million | Total RTI costs | N/A | X | X | X |
| Hung et al., 2008 | Vietnam | Urban | 656 MCIs | N/A | $10 | Per motorcycle helmet | 1% | N/A | ||
| Riewpaiboon et al., 2008 | Thailand | Urban (one hospital) | 200 RTIs | N/A | $3000 | Per hospitalization | 65% | X | X | X |
| Reddy et al., 2009 | India | Urban (five hospitals) | 95 RTIs | N/A | $23 100 | Per hospitalization | 35% | X | X | |
| Juillard et al., 2010 | Nigeria | Urban | 127 RTIs | N/A | $28 | Per injury | 2% | X | X | |
| Mashreky et al., 2010 | Bangladesh | Urban and Rural (16 hospitals) | 7732 RTIs | N/A | $110 | Per hospitalization | 16% | X | X | |
| Perez-Nunez et al., 2010 | Belize | National | 964 RTIs | N/A | $10 300 | Per injury | 254% | X | X | X |
| Kudebong et al., 2011 | Ghana | Rural | 556 MCIs | N/A | $2220 | Per injury | 168% | X | X | X |
| Li et al., 2011 | China | Urban | 550 bicycle injuries | N/A | $4330 | Per injury | 98% | X | X | |
| Razzak et al., 2011 | Pakistan | Urban (five hospitals) | 341 RTIs | N/A | $355 | Per injury | 35% | X | X | X |
| Perez-Nunez et al., 2011 | Mexico | Urban (four hospitals) | 60 RTIs | N/A | $810 | Per hospitalization | 9% | X | X | X |
| Sangowawa et al., 2011 | Nigeria | Urban | 44 MCCs | N/A | $75 | Per injury | 5% | X | X | |
| Nguyen et al., 2012b | Vietnam | Urban (one hospital) | 477 RTIs | N/A | $363 | Per injury | 30% | X | X | X |
| Cost analysis | ||||||||||
| Bishai et al., 2003 | Uganda, Pakistan | National | N/A | N/A | Uganda: $0.12 | Per road safety | 0.02% | N/A | ||
| Pakistan: $0.09 | >0.01% | |||||||||
| Hendrie et al., 2004c | 8 LMICsa | Urban | Retail stores and internet vendors | N/A | Car seat: $100 | Per safety device | N/A | N/A | ||
| Booster seat: $219 | ||||||||||
| Bicycle helmet: $16 | ||||||||||
| Hijar et al., 2004 | Mexico | Urban (four hospitals) | 233 RTIs | N/A | Uninsured: <$25 | Per hospitalization | <0.3% | X | X | |
| Insured: >$123 | >1.3% | |||||||||
| Outcome analysis | ||||||||||
| Naci and Baker, 2008 | Turkey | Urban | N/A | N/A | $360,571 | Years of potential life lost | N/A | N/A | ||
| 2. Burn Injuries (n = 12) | ||||||||||
| Cost description | ||||||||||
| Nursal et al., 2003 | Turkey | Urban (one hospital) | 109 burns | N/A | $6310 | Per hospitalization | 601% | X | ||
| Mashreky et al., 2008 | Bangladesh | N/S (61 health facilities) | 791 burns | N/A | $267 | Per hospitalization | 675% | X | X | |
| Kai-Yang et al., 2009 | China | Urban (one hospital) | 178 paediatric burns | N/A | $1070 | Per hospitalization | 24% | X | ||
| Ogundipe et al., 2009 | Nigeria | Urban (one hospital) | 69 burns | N/A | $297 | Per hospitalization | 21% | X | ||
| Yin et al., 2010 | China | Urban (one hospital) | 201 elderly burns | N/A | $3860 | Per hospitalization | 87% | X | ||
| Ahachi et al., 2011 | Nigeria | Urban (one hospital) | 52 burns | N/A | $1390 | Per hospitalization | 96% | X | ||
| Allorto et al., 2011 | South Africa | Urban (one hospital) | 450 burns | N/A | $9800 | Per hospitalization | 135% | X | ||
| Sahin et al., 2011 | Turkey | Urban (one hospital) | 43 burns | N/A | $15 400 | Per hospitalization | 153% | X | X | |
| Alinia et al., 2013 | Iran | Urban (one hospital) | 723 firework burns | N/A | $227 | Per hospitalization | 2% | X | ||
| Cost analysis | ||||||||||
| Hendrie et al., 2004c | 8 LMICsa | Urban | Retail stores and internet vendors | N/A | Smoke alarm: $61.8 | Per safety device | N/A | N/A | ||
| Cost-outcome description | ||||||||||
| Zhou et al., 2003b | China | Urban (one hospital) | 40 burns treated with: | Plasma concentration | Per hospitalization | X | ||||
| 1. Glutamine | 1. 591 | 1. $9200 | 207% | |||||||
| 2. Control | 2. 399 | 2. $10 100 | 228% | |||||||
| Muangman et al., 2010 | Thailand | Urban | 70 burns treated with: | Time to wound closure: | Per hospitalization | X | X | |||
| 1. Siler sulfadiazine | 1. 13.7 days | 1. $94 | 2% | |||||||
| 2. Aqualcel Ag | 2. 10 days | 2. $53 | 1% | |||||||
| 3. Injuries from Violence (n = 4) | ||||||||||
| Cost description | ||||||||||
| Mansingh and Ramphal, 1993 | Jamaica | Urban (one hospital) | 640 violent injuries | N/A | $36 to $56 | Per hospitalization | 0.7–1.1% | X | ||
| Mendonca et al., 2002 | Brazil | Urban | 9220 violent injuries | N/A | $285 | Per hospitalization | 3% | X | ||
| Allard and Burch, 2005 | South Africa | Urban (one hospital) | 21 firearm injuries | N/A | $17,400 | Per hospitalization | 239% | X | ||
| Ward et al., 2009 | Jamaica | National | 8468 violent injuries | N/A | $59.2 million | Per injury | N/A | X | X | X |
| 4. Injury, not specified (n = 15) | ||||||||||
| Cost description | ||||||||||
| Kaya et al., 1999 | Turkey | Urban (one hospital) | 347 injuries | N/A | $2,190 | Per hospitalization | 209% | X | ||
| McDonald et al., 1999 | Jamaica | Urban (one hospital) | 22,311 injuries | N/A | $97 | Per hospitalization | 2% | X | ||
| Zhao et al., 2002 | China | Urban (eight hospitals) | 5876 injuries | N/A | $624 | Per hospitalization | 14% | X | ||
| Gurses et al., 2003 | Turkey | Urban (one hospital) | 91 paediatric injuries | N/A | $493 | Per hospitalization | 47% | X | ||
| Thanh et al., 2003 | Vietnam | Urban and rural | 1740 non-fatal unintentional injuries | N/A | $17 | Per injury | 1% | X | X | X |
| Mock et al., 2003 | Ghana | Urban and rural | 1609 injuries | N/A | Urban: $38 | Per injury | 3% | X | ||
| Rural: $14 | 1% | |||||||||
| Li et al., 2005 | China | Rural | 902 injuries | N/A | $1033 | Per injury | 23% | X | X | X |
| Melione and Mello-Jorge, 2008 | Brazil | Urban (one hospital) | 976 injuries | N/A | $188 | Per hospitalization | 2% | X | ||
| Joshi and Shrestha, 2009 | Nepal | Urban (six health centres) | 505 injuries | N/A | $128 | Per injury | 24% | X | ||
| Rodrigues et al., 2009 | Brazil | National | N/A | N/A | $868 million | Total cost of injury | N/A | X | X | X |
| Soyer et al., 2009 | Turkey | Urban (one hospital) | 146 paediatric injuries | N/A | $169 | Per emergency room visit | 16% | X | ||
| Bildik et al., 2010 | Turkey | Urban (one hospital) | 118 injuries | N/A | $78 | Per hospitalizaitonb | 1% | X | ||
| Plummer et al., 2010 | Jamaica | Urban | 715 injuries | N/A | $357 | Per hospitalization | 7% | X | ||
| Nguyen et al., 2012a | Vietnam | Urban (one hospital) | 892 injures | N/A | $366 | Per injury | 30% | X | X | X |
| Outcome analysis | ||||||||||
| Zhou et al., 2003a | China | National | N/A | N/A | $12.6 million | years of lost productivity | N/A | N/A | ||
RTI: road traffic injury; N/A: not applicable; N/S: not specified.
a Eight LMICs include: Albania, China, Philippines, Brazil, Thailand, Venezuela, Vietnam, and South Africa. As this study describes costs of both burn and RTI prevention, it is listed in both sections but counted once.
b Cost reported as median.
c Study listed twice under RTI and burn injury, respectively.
In terms of the breakdown of the costs of injury, of the applicable partial evaluation studies—excluding outcome analysis studies (n = 2) and studies that reported the costs of safety devices (n = 4)—all but one study (n = 48/49) reported direct costs. Twenty-one studies (42%) reported direct non-medical costs and 21 other studies (42%) reported indirect costs. Sixteen studies (32%) reported all three types of costs. As shown in Table 2, costs included within these categories varied widely. For example, while 21 studies included the cost of hospital stay, two studies defined in terms of direct medical costs only as hospital stay, while five studies defined direct medical costs as hospital stay, surgical services, laboratory investigations and medicine. Twenty-five studies (51%) did not specify how direct medical costs were defined. Twenty-one studies (42%) reported indirect costs, of which six defined indirect costs as income loss only.
Table 2.
Type of injury costs variables included in partial economic studies
| Cost Variables | Partial economic studies (n = 49)a |
|---|---|
| Direct medical cost (n = 48) | |
| Hospital stay | 21 |
| Pre-hospital care | 2 |
| Emergency department visit | 6 |
| Surgical services | 11 |
| Specialist consultation | 4 |
| Rehabilitation/physical therapy | 3 |
| Out-patient follow-up | 3 |
| Wound care/prostheses | 11 |
| Laboratory investigations | 8 |
| Radiological investigations | 9 |
| Blood and blood products | 2 |
| Medicine | 16 |
| Not specified | 25 |
| Direct non-medical costs (n = 21) | |
| Administrative | 6 |
| Transportation | 10 |
| Property damage | 6 |
| Food | 5 |
| Accommodation | 5 |
| Funeral cost | 3 |
| Not specified | 4 |
| Indirect costs (n = 21) | |
| Income loss | 15 |
| Cost of premature death | 8 |
| Pain and suffering | 3 |
| Restricted activity (not work related) | 2 |
| Not specified | 3 |
a Includes studies that reported unit cost as per injury, hospitalization and total injury.
The range of injury costs per hospitalization and per injury varied widely (Table 3). Of the 22 studies that reported only direct costs per hospitalization, the median cost was US$291, but costs ranged from US$14 to US$17 400. The median cost as a percentage of GDP was 15%. In terms of specific types of injuries, the highest reported median direct medical costs were for burn injuries. Six studies reported direct medical and non-medical costs, ranging from less than US$25 to US$15 400. Thirteen studies reported direct medical, direct non-medical and indirect costs; the median cost of these studies was US$4085 or 97% of GDP per capita.
Table 3.
Median and range of injury costs per hospitalization and per injury described by cost description studies (n = 41; US$ 2010)a
| Injury type | Direct medical costs per hospitalization |
Direct medical and non-medical costs per hospitalization |
Direct medical, direct non-medical, and indirect costs per injury |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Studies (n) | Median cost (range) | Median cost as % of GDP (range) | Studies (n) | Mean cost (range) | Median cost as % of GDP (range) | Studies (n) | Median cost (range) | Median cost as % of GDP (range) | |
| Injury (not specified) | 9 | $178.5 (14–2190) | 11% (1–209%) | 0 | – | – | 3 | $91 (17–366) | 16% (1–30%) |
| RTI | 3 | $140 (99–720) | 16% (2–18%) | 3 | $117 (<25–23 100) | 9% (<0.3–1680%) | 10 | $4200 (355–10 300) | 98% (9–717%) |
| Burn | 7 | $1390 (227–9800) | 87% (2–601%) | 3 | $181 (53–15 400) | 21% (1–153%) | 0 | – | – |
| Violence | 3 | $ 285 (36–17 400) | 3% (0.7–239%) | 0 | – | – | 0 | – | – |
| Total | 22 | $291 (14–17 400) | 15% (0.7–239%) | 6 | $125 (<25–15 400) | 9% (<0.3–1680%) | 13 | $4085 (17–10 300) | 97% (1–717%) |
a Excludes three studies that reported costs as a unit of total costs (Rodrigues et al., 2009; Ward et al., 2009; Yan-Hong et al., 2006), three studies that reported the costs of safety programmes or devices (Bishai et al., 2003; Hendrie et al., 2004; Hung et al., 2008), one study that reported only indirect costs (Arokiasamy and Krishnan, 1994) and two studies that reported only direct medical costs and indirect costs (Joshi and Shrestha, 2009; Juillard et al., 2010).
Three partial evaluation studies described the cost of safety interventions or devices, including road safety, car and booster seats, motorcycle and bicycle helmets, and smoke detectors, ranging from US$0.09 for a national road safety programme to US$219 for a booster seat.
Thirteen full economic evaluations explored costs associated with RTIs, drowning, and pre-hospital and hospital-based trauma care (Table 4). Some studies calculated cost per outcome using primary data (n = 6) and others applied secondary data from other published studies to epidemiological models (n = 7). Different units were used to describe effectiveness, including cost per death averted (n = 5), cost per DALY averted (n = 6), cost per life year saved (n = 1) and willingness to pay (n = 1). Costs per death averted ranged from US$30 for enhanced traffic enforcement to US$596 000 for a citywide pre-hospital system based on a North American emergency response model. The cost per DALY averted from injury-prevention interventions ranged from US$10.9 for speed bump installation to US$12 800 for legislation and enforcement of motorcycle helmets in the WHO's African (AFRO) region. In terms of hospital-based surgical care for trauma victims, costs ranged from US$30 to US$226 per DALY averted in Cambodia and Haiti, respectively.
Table 4.
Full economic evaluation studies of injuries and trauma care in low- and middle-income countries (n = 13)
| Author, year | Study location | Study setting | Study sample | Intervention | Cost (US$ 2010) | Unit (Cost per) | Cost-effectiveness |
|---|---|---|---|---|---|---|---|
| 1. Road traffic injuries (n = 6) | |||||||
| Harris, 2005 (Harris and Olukoga, 2005) | South Africa | Urban | Model using data from 7567 injured patients | Seat belt enforcement | $17 400 | Per death averted | N/A |
| Bishai, 2006 (Bishai and Hyder, 2006) | LMICs | Urban | Model using data from Bangladesh, Brazil, China, Ghana, and Philippines | 1. Traffic enforcement | $78.8 | Per DALY averted | Very cost-effective |
| 2. Speed bumps at locations that cause 25% of junction deaths | $10.9 | Per DALY averted | Very cost-effective | ||||
| 3. Motorcycle helmet legislation and enforcement | $575 | Per DALY averted | Very cost-effective | ||||
| Bishai, 2008 (Bishai et al., 2008) | Uganda | Urban | Model using data from 10 police stations | Enhanced traffic enforcement | $30 | Per life year saved | Very cost-effective |
| Pham, 2008 (Pham et al., 2008) | Vietnam | Urban | 414 households | Willingness to pay among 63% of respondents | $9.38 | Per motorcycle helmet | N/A |
| Chisholm, 2012 (Chisholm and Naci, 2012) | AFRO, SERO | Urban and rural | Model | 1. Speed cameras | AFRO: $4230; SERO: $5540 | Per DALY averted | AFRO and SERO: Very cost-effective |
| 2. Drink-driving and breath testing campaigns | AFRO: $5670; SERO: $9530 | Per DALY averted | AFRO and SERO: Cost-effective | ||||
| 3. Seatbelt usea | AFRO: $11600; SERO: $8730 | Per DALY averted | AFRO and SERO: Very cost-effective | ||||
| 4. Motorcycle helmetsa | AFRO: $17000; SERO: $5920 | Per DALY averted | AFRO: Cost-effective; SERO: Very cost-effective | ||||
| 5. Bicyclist helmetsa,b | AFRO: $3130; SERO: $12800 | Per DALY averted | AFRO: Very cost-effective; SERO: Cost-effective | ||||
| Ditsuwan, 2013 (Ditsuwan et al., 2013) | Thailand | Urban and rural | Model | 1. Selective breath testing | $367 | Per DALY averted | Very cost-effective |
| 2. Random breath testing | $403 | Per DALY averted | Very cost-effective | ||||
| 3. Mass media campaign | $291 | Per DALY averted | Very cost-effective | ||||
| 4. Selective breath testing with mass media | $353 | Per DALY averted | Very cost-effective | ||||
| 5. Random breath testing with mass media | $376 | Per DALY averted | Very cost-effective | ||||
| 2. Drowning (n = 1) | |||||||
| Rahman, 2012 (Rahman et al., 2012) | Bangladesh | Rural | 76918 children in 3 rural regions | Drowning prevention programme including a preschool education system and a child swim programme | 362 | Per DALY averted | Very cost-effective |
| 3. Pre-hospital trauma care (n = 4) | |||||||
| Hauswald, 1997 (Hauswald and Yeoh, 1997) | Malaysia | Urban | Model using data from 467 injury-related deaths | Development of pre-hospital system, based on a North American model | $596,000 | Per death averted | N/A |
| Arreola-Risa, 2004 (Arreola-Risa et al., 2004) | Mexico | Urban | 20 pre-hospital providers | PHTLS training | $1020 | Per death averted | N/A |
| Arreola-Risa, 2007 (Arreola-Risa et al., 2007) | Mexico | Urban | 35 pre-hospital providers | EMT training | $212 | Per death averted | N/A |
| Jayaraman, 2009 (Jayaraman et al., 2009) | Uganda | Urban | Model using estimates of 9000 lay first responders | Pre-hospital training | $1820 | Per death averted | N/A |
| 4. Hospital-based trauma care (n = 2) | |||||||
| Gosselin, 2008 (Gosselin and Heitto, 2008) | Cambodia | Urban (one hospital) | 957 injured patients | Surgical care for traumatic injuries | $30 | Per DALY averted | Very cost-effective |
| Gosselin, 2010 (Gosselin et al., 2010) | Nigeria and Haiti | Urban (two hospitals) | 6745 injured patients | 1. Surgical care in Nigeria | $174 | Per DALY averted | Very cost-effective |
| 2. Surgical care in Haiti | $226 | Per DALY averted | Very cost-effective | ||||
AFRO: World Health Organization African Region; DALY: Disability-adjusted life year; EMT: Emergency Medical Technician; LMICs: Low- and middle-income countries; PHTLS: PreHospital Trauma Life Support; SEARO: World Health Organization South-East Asia Region
a Legislation and enforcement
b In children less than 15 years old.
Based on the Community Guide’s criteria, two full economic evaluation studies were unsatisfactory in their methods to explore the costs associated with injuries (Table 5). Of the studies that achieved a rating of satisfactory or greater and reported costs per DALY averted, the level of cost-effectiveness was described (n = 7; Table 4). These studies show many interventions to be very cost-effective, such as legislation and enforcement of bicycle helmets in the AFRO region, speed bumps at junctions with 25% or more mortality, and surgical trauma care in Cambodia, Nigeria and Haiti.
Table 5.
Quality assessment of full economic studies on costs of injury in LMICsa
| Quality indicator | Full economic evaluation (n = 13) |
||
|---|---|---|---|
| Described | Not described | Not applicable | |
| Study design | |||
| Study population | 12 | 1 | – |
| Study question(s) | 13 | – | – |
| Alternative interventions | 7 | 6 | – |
| Study perspective specified | 6 (7 inferred) | – | – |
| Societal perspective specified | 4 (3 inferred) | 6 | – |
| Time frame defined | 12 | 1 | – |
| Analytic horizon defined | 3 | 10 | – |
| Costs | |||
| Data sources reported | 12 | 1 | – |
| Data sources appropriate | 10 | 3 | – |
| Quantities of resources reported | 13 | – | – |
| Programme costs included | 9 | 4 | – |
| Cost of illness included | 6 | 7 | – |
| Future costs discounted | 7 | 6 | – |
| Price base-year reported | 11 | 2 | – |
| Outcome measures | |||
| Outcome measures specified | 13 | – | – |
| Outcome measures consistent | 11 | 2 | – |
| Future outcomes discounted | 6 | 7 | – |
| Outcomes included other effects | 6 | 7 | – |
| Effects | |||
| Effect information provided | 13 | – | – |
| Criteria reported | 6 | 7 | – |
| Expert opinion appropriate | 1 | – | 12 |
| Analysis | |||
| Analytical model reported | 10 | 3 | – |
| Sensitivity analysis of discounted rate | 6 | 7 | – |
| Sensitivity analysis of effect size | 10 | 3 | – |
| Sensitivity analysis of any other parameter | 8 | 5 | – |
| Summary measure used correctly by study | 9 | 4 | – |
| Rating | |||
| Very good | 5 | ||
| Good | 1 | ||
| Satisfactory | 5 | ||
| Unsatisfactory | 2 | ||
a Based on the Community Guide Quality Assessment Criteria.
Discussion
Our study found that there are a relatively significant number of studies that have explored the cost of injury or the cost of hospitalizations from injury in LMICs. Yet only 13 studies performed full economic evaluations in 14 of 144 LMICs as classified by the World Bank. It is difficult to generalize the costs of injury at a regional or global level, as the currently available data are country and context-specific and heterogeneous in their definitions of costs.
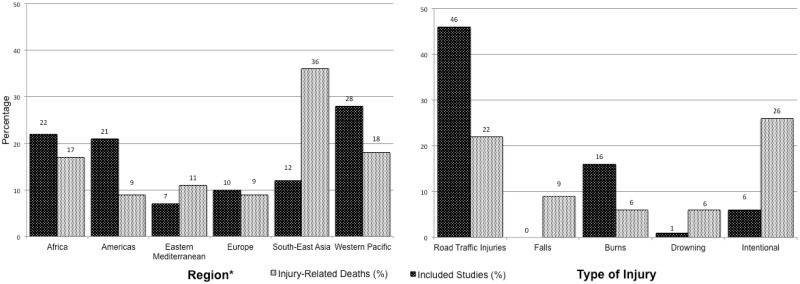
Our review showed LMIC injury-related costing research may not reflect the distribution of the burden of injury across regions and injury type. For example, only 12% of the studies included in our review were conducted in Southeast Asia, although the region accounts for 36% of injury-related deaths among LMICs (Figure 2) (World Health Organization, 2008). Conversely, 28% of studies were conducted in the Western Pacific Region although the region accounts for only 18% deaths from injury. In terms of injury type, only 4 of 68 studies examined the costs associated with intentional injuries, although they make up 26% of DALYs lost to injuries in LMICs (World Health Organization, 2008). In terms of demographics, only three studies used primary data collected from a rural setting, despite estimates that more than half of people in LMICs live in rural areas (The World Bank, 2012). Some studies set in urban referral hospitals may have captured injuries that occur in rural areas given the nature of referral hospitals, but this was not been specifically studied.
Figure 2.
Comparison between the number of papers published on costs of injury in LMICs (%) and injury-related deaths in LMICs by region and type of injury1
Source: WHO, Global Burden of Disease 2004 Update.
1As a percentage of total injuries
*Region defined using WHO classification
Unfortunately, a lack of representative data is not limited to these studies; even data from the WHO are limited. For example, estimates from the WHO on injuries per DALY for LMICs show that of the 144 LMICs, 74 countries (52%) lacked complete, country-specific data for these calculations, and therefore used modelled estimates (World Health Organization, 2011b).
In addition to gaps in data collection, our review found considerable variability in the costs and cost descriptions of injury. Costs and outcomes were often not reported nor measured in a systematic way. As there are no standard definitions for direct medical, direct non-medical and indirect costs, studies were left to their own discretion to decide which cost variables to include. Some studies did not even describe which cost variables were included in their estimates. This limits the ability to generalize costs across studies.
In addition to the limitations of the reported data, our review was limited in that we only searched published literature; additional costing studies may be available among the grey and unpublished literature. The study was further limited in that our search was conducted using English-language-based databases.
Despite these limitations, the economic burden of injury is indisputable. As shown in our review, the median cost of direct medical costs from injury was US$291 or 15% of GDP per capita. This estimate increased 14-fold to US$4085 or 97% of GDP per capita when studies included direct medical, direct non-medical and indirect costs. This shows not only the devastating financial impact of injury, but also the need to invest in injury prevention. Yet in a time of global budget constraints and competing social sector priorities, policy-makers and public health planners are increasingly faced with having to maximize available resources, and cost-effectiveness of interventions or programmes often comes into play.
Our review showed encouraging findings among the cost-effectiveness studies that achieved a quality-assessment rating of satisfactory or higher: many interventions could be cost-effective or very cost-effective in decreasing the burden of injury. These interventions include traffic enforcement, installation of speed bumps, motorcycle helmet legislation, breath testing campaigns and drowning prevention programmes. The provision of surgical care was also shown to be very cost-effective, suggesting a significant potential for cost savings through injury prevention and trauma care. Care, however, should be used when generalizing these interventions to national, regional and global contexts. This is also important as seven studies adopted a societal perspective and six used a provider perspective, highlighting heterogeneity among the costs included in each study. This concern is not unique to our review and prior literature has explored why results from economic studies may not be reproducible in different settings and times (Drummond and Pang, 2001; Sculpher et al., 2004).
Costs are often considered the ‘tie-breaker’ when decisions are made regarding how and where to prioritize health interventions. To make an impact in the future, we need to better understand the costs of injury and injury prevention in LMICs. Through multi-sectoral collaboration with Departments of Health, Transport and other stakeholders, injury prevention advocates in LMICs can generate economic data to advocate for greater investments in injury prevention. This may finally enable injury prevention to be placed on regional, national and district policy agendas.
Funding
H.K.H.W., A.B. and A.A.H. were funded by various grants to the Johns Hopkins International Injury Research Unit (www.jhsph.edu/IIRU), including the JHU Center for Global Health, Bloomberg Philanthropies, and Fogarty International Center of the US National Institutes of Health. N.M. and K.H. were funded by the Bill & Melinda Gates Foundation through the Disease Control Priorities Network (DCPN) Project though a subcontract to the Department of Global Health at the University of Washington, Seattle and by the Fogarty International Center at NIH. The study was undertaken under the auspices of PRICELESS SA (Priority Cost Effective Lessons for Systems Strengthening—South Africa) www.pricelesssa.ac.za.
Conflict of interest
None declared.
References
- Ahachi CN, Fadeyibi IO, Abikoye FO, Chira MK, Ugburo AO, Ademiluyi SA. The direct hospitalization cost of care for acute burns in Lagos, Nigeria: a one-year prospective study. Annals of Burns and Fire Disasters. 2011;24:94–101. [PMC free article] [PubMed] [Google Scholar]
- Al-Masaeid HR, Al-Mashakbeh AA, Qudah AM. Economic costs of traffic accidents in Jordan. Accident Analysis & Prevention. 1999;31:347–57. doi: 10.1016/s0001-4575(98)00068-2. [DOI] [PubMed] [Google Scholar]
- Alinia S, Rezaei S, Daroudi R, Hadadi M, Akbari Sari A. Extent, nature and hospital costs of fireworks-related injuries during the Wednesday Eve festival in Iran. Journal of Injury and Violence Research. 2013;5:11–16. doi: 10.5249/jivr.v5i1.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allard D, Burch VC. The cost of treating serious abdominal firearm-related injuries in South Africa. South African Medical Journal. 2005;95:591–94. [PubMed] [Google Scholar]
- Allorto NL, Clarke DL, Thomson SR. A cost model case comparison of current versus modern management of burns at a regional hospital in South Africa. Burns. 2011;37:1033–7. doi: 10.1016/j.burns.2011.04.004. [DOI] [PubMed] [Google Scholar]
- American Economic Association. EconLit [Online] 2013. http://www.aeaweb.org/econlit/index.php, accessed 24 March 2013.
- Anh TT, Anh TT, Dao NX. The cost of road traffic accident in Vietnam. Proceedings of the Eastern Asia Society for Transportation Studies. 2005;5:1923–33. [Google Scholar]
- Arokiasamy JT, Krishnan R. Some epidemiological aspects and economic costs of injuries in Malaysia. Asia-Pacific Journal of Public Health. 1994;7:16–20. doi: 10.1177/101053959400700103. [DOI] [PubMed] [Google Scholar]
- Arreola-Risa C, Mock C, Herrera-Escamilla AJ, Contreras I, Vargas J. Cost-effectiveness and benefit of alternatives to improve training for prehospital trauma care in Mexico. Prehospital and Disaster Medicine. 2004;19:318–25. doi: 10.1017/s1049023x00001953. [DOI] [PubMed] [Google Scholar]
- Arreola-Risa C, Vargas J, Contreras I, Mock C. Effect of emergency medical technician certification for all prehospital personnel in a Latin American city. Journal of Trauma. 2007;63:914–9. doi: 10.1097/TA.0b013e31806bf141. [DOI] [PubMed] [Google Scholar]
- Bildik F, Yardan T, Demircan A, Uckan MU, Ergin M, Hacioglu EG. The real victims of the Islamic feast of sacrifice: injuries related to the sacrifice. Ulus Travma Acil Cerrahi Derg. 2010;16:319–22. [PubMed] [Google Scholar]
- Bishai DM, Hyder AA. Modeling the cost effectiveness of injury interventions in lower and middle income countries: opportunities and challenges. Cost Effectiveness and Resource Allocation. 2006;4 doi: 10.1186/1478-7547-4-2. doi:10.1186/1478-7547-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishai D, Asiimwe B, Abbas S, Hyder AA, Bazeyo W. Cost-effectiveness of traffic enforcement: case study from Uganda. Injury Prevention. 2008;14:223–7. doi: 10.1136/ip.2008.018341. [DOI] [PubMed] [Google Scholar]
- Bishai D, Hyder AA, Ghaffar A, Morrow RH, Kobusingye O. Rates of public investment for road safety in developing countries: case studies of Uganda and Pakistan. Health Policy and Planning. 2003;18:232–5. doi: 10.1093/heapol/czg028. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Naci H, Hyder AA, Tran NT, Peden M. Cost effectiveness of strategies to combat road traffic injuries in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012:344. doi: 10.1136/bmj.e612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community Guide. Economic Evaluation Abstraction Form Version 4.0 [Online] 2010. http://www.thecommunityguide.org, accessed 16 March 2013.
- De Leon M, Cal P, Sigua R. Estimation of socio-economic cost of road accidents in metro Manila. Journal of the Eastern Asia Society for Transportation Studies. 2005;6:3183–98. [Google Scholar]
- Ditsuwan V, Lennert Veerman J, Bertram M, Vos T. Cost-effectiveness of interventions for reducing road traffic injuries related to driving under the influence of alcohol. Value in Health. 2013;16:23–30. doi: 10.1016/j.jval.2012.08.2209. [DOI] [PubMed] [Google Scholar]
- Drummond MF, Pang F. Transferability of economic evaluation results. In: Drummond MF, McGuire A, editors. Economic Evaluation in Health Care: Merging Theory with Practice. Oxford: Oxford University Press; 2001. [Google Scholar]
- Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddant GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005. [Google Scholar]
- Elsevier Inc. Econbase [Online] 2013a. Elsevier Inc. http://www.elsevier.com/homepage/sae/econworld/menu.htm, accessed 24 March 2013.
- Elsevier Inc. Embase [Online] 2013b. Elsevier Inc. http://www.embase.com/, accessed 20 March 2013.
- Gosselin RA, Heitto M. Cost-effectiveness of a district trauma hospital in Battambang, Cambodia. World J Surg. 2008;32:2450–3. doi: 10.1007/s00268-008-9708-4. [DOI] [PubMed] [Google Scholar]
- Gosselin RA, Maldonado A, Elder G. Comparative cost-effectiveness analysis of two MSF surgical trauma centers. World J Surg. 2010;34:415–9. doi: 10.1007/s00268-009-0230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurses D, Sarioglu-Buke A, Baskan M, Kilic I. Cost factors in pediatric trauma. Canadian Journal of Surgery. 2003;46:441–5. [PMC free article] [PubMed] [Google Scholar]
- Gyllensvard H. Cost-effectiveness of injury prevention – a systematic review of municipality based interventions. Cost Effectiveness and Resource Allocation. 2010;8:17. doi: 10.1186/1478-7547-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris G T, Olukoga I A. A cost benefit analysis of an enhanced seat belt enforcement program in South Africa. Injury Prevention. 2005;11:102–105. doi: 10.1136/ip.2004.007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan S, Macharia W, Atinga J. Self reported alcohol use in an urban traffic trauma population in Kenya. East Afr Med. 2005;82:144–7. doi: 10.4314/eamj.v82i3.9271. [DOI] [PubMed] [Google Scholar]
- Hauswald M, Yeoh E. Designing a prehospital system for a developing country: estimated cost and benefits. The American Journal of Emergency Medicine. 1997;15:600–603. doi: 10.1016/s0735-6757(97)90167-4. [DOI] [PubMed] [Google Scholar]
- Hendrie D, Miller TR, Orlando M, Spicer RS, Taft C, Consunji R, Zaloshnja E. Child and family safety device affordability by country income level: an 18 country comparison. Injury Prevention. 2004;10:338–43. doi: 10.1136/ip.2004.005652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijar M, Arredondo A, Carrillo C, Solorzano L. Road traffic injuries in an urban area in Mexico: an epidemiological and cost analysis. Accident Analysis & Prevention. 2004;36:37–42. doi: 10.1016/s0001-4575(02)00112-4. [DOI] [PubMed] [Google Scholar]
- Hung DV, Stevenson MR, Ivers RQ. Motorcycle helmets in Vietnam: ownership, quality, purchase price, and affordability. Traffic Injury Prevention. 2008;9:135–43. doi: 10.1080/15389580701882607. [DOI] [PubMed] [Google Scholar]
- Jadaan KS. Road accidents costs in Jordan. Journal of the Royal Society of Health. 1989;109:144–6. doi: 10.1177/146642408910900412. [DOI] [PubMed] [Google Scholar]
- Jamison DT, Breman JG, Measham AR, et al. Disease Control Priorities in Developing Countries. 2nd. Washington, DC: The World Bank and Oxford University Press; 2006. [PubMed] [Google Scholar]
- Jayaraman S, Mabweijano JR, Lipnick MS, et al. First things first: effectiveness and scalability of a basic prehospital trauma care program for lay first-responders in Kampala, Uganda. PLoS One. 2009;4:e6955. doi: 10.1371/journal.pone.0006955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jianping Z, Chongsuvivatwong V, Geater A. Clinical severity and financial burden among road traffic injury patients in Kunming, China. The Southeast Asian Journal of Tropical Medicine and Public Health. 2006;37:1034–9. [PubMed] [Google Scholar]
- Joshi SK, Shrestha S. Economic and social burden due to injuries and violence in Nepal: a cross-sectional study. Kathmandu Univ Med J. 2009;7:344–50. doi: 10.3126/kumj.v7i4.2752. [DOI] [PubMed] [Google Scholar]
- Juillard C, Labinjo M, Kobusingye O, Hyder AA. Socioeconomic impact of road traffic injuries in West Africa: exploratory data from Nigeria. Injury Prevention. 2010;16:389–92. doi: 10.1136/ip.2009.025825. [DOI] [PubMed] [Google Scholar]
- Kai-Yang L, Shi-Hui Z, Hong-Tai T, et al. The direct hospitalisation costs of paediatric scalds: 2-year results of a prospective case series. Burns. 2009;35:738–45. doi: 10.1016/j.burns.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Kaya E, Ozguc H, Tokyay R, Yunuk O. Financial burden of trauma care on a university hospital in a developing country. The Journal of trauma. 1999;47:572–5. doi: 10.1097/00005373-199909000-00027. [DOI] [PubMed] [Google Scholar]
- Kudebong M, Wurapa F, Nonvignon J, Norman I, Awoonor-Williams JK, Aikins M. Economic burden of motorcycle accidents in Northern Ghana. Ghana Medical Journal. 2011;45:135–42. [PMC free article] [PubMed] [Google Scholar]
- Li YH, Rahim Y, Zhou DD. A study on bicycle-related injuries and their costs in Shanghai, China. Journal of Environmental Health. 2011;73:22–28. [PubMed] [Google Scholar]
- Li ZH, Zhao ZT, Guo YX, Liu X. The burden caused by injury in countryside residents in Dongying, Shandong Province. Chinese Journal of Preventive Medicine. 2005;39:273–6. [PubMed] [Google Scholar]
- Littell JH, Corcoran J, Pillai VK. Systematic Reviews and Meta-Analysis. New York: Oxford University Press; 2008. [Google Scholar]
- Mansingh A, Ramphal P. The nature of interpersonal violence in Jamaica and its strain on the national health system. The West Indian Medical Journal. 1993;42:53–6. [PubMed] [Google Scholar]
- Mashreky SR, Rahman A, Chowdhury SM, et al. Burn injury: economic and social impact on a family. Public Health. 2008;122:1418–24. doi: 10.1016/j.puhe.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Mashreky SR, Rahman A, Khan TF, Faruque M, Svanstrom L, Rahman F. Hospital burden of road traffic injury: major concern in primary and secondary level hospitals in Bangladesh. Public Health. 2010;124:185–9. doi: 10.1016/j.puhe.2010.01.004. [DOI] [PubMed] [Google Scholar]
- McDonald A, Duncan ND, Mitchell DI, Fletcher PR. Trauma aetiology and cost in the Accident and Emergency Unit of the University Hospital of the West Indies. The West Indian Medical Journal. 1999;48:141–2. [PubMed] [Google Scholar]
- Melione LP, Mello-Jorge MH. Unified National Health System costs in Sao Jose dos Campos, Sao Paulo State, Brazil, for hospital admissions due to external causes. Cadernos de Saude Publica. 2008;24:1814–24. doi: 10.1590/s0102-311x2008000800010. [DOI] [PubMed] [Google Scholar]
- Mendonca RN, Alves JG, Filho JE. Hospital costs due to violence against children and adolescents in Pernambuco State, Brazil, during 1999. Cad Saude Publica. 2002;18:1577–81. doi: 10.1590/s0102-311x2002000600011. [DOI] [PubMed] [Google Scholar]
- Mock CN, Gloyd S, Adjei S, Acheampong F, Gish O. Economic consequences of injury and resulting family coping strategies in Ghana. Accident Analysis & Prevention. 2003;35:81–90. doi: 10.1016/s0001-4575(01)00092-6. [DOI] [PubMed] [Google Scholar]
- Muangman P, Pundee C, Opasanon S, Muangman S. A prospective, randomized trial of silver containing hydrofiber dressing versus 1% silver sulfadiazine for the treatment of partial thickness burns. International Wound Journal. 2010;7:271–6. doi: 10.1111/j.1742-481X.2010.00690.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naci H, Baker TD. Productivity losses from road traffic deaths in Turkey. International Journal of Injury Control and Safety Promotion. 2008;15:19–24. doi: 10.1080/17457300701847648. [DOI] [PubMed] [Google Scholar]
- National Institute for Health Research. National Health Service Economic Evaluation [Online] 2013. National Institute for Health Research, University of York. http://www.crd.york.ac.uk/crdweb/, accessed 24 March 2013.
- National Library of Medicine. Medline/PubMed [Online] 2013. National Library of Medicine. http://www.ncbi.nlm.nih.gov/pubmed/, accessed 26 March 2013.
- Nguyen H, Ivers R, Jan S, Martiniuk A, Pham C. Catastrophic household costs due to injury in Vietnam. Injury. 2012a doi: 10.1016/j.injury.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Nguyen H, Ivers RQ, Jan S, Martiniuk AL, Li Q, Pham C. The economic burden of road traffic injuries: evidence from a provincial general hospital in Vietnam. Injury Prevention. 2012b doi: 10.1136/injuryprev-2011-040293. [DOI] [PubMed] [Google Scholar]
- Nilsen P, Hudson D, Lindqvist K. Economic analysis of injury prevention – applying results and methodologies from cost-of-injury studies. International Journal of Injury Control and Safety Promotion. 2006;13:7–13. doi: 10.1080/17457300500167651. [DOI] [PubMed] [Google Scholar]
- Nursal TZ, Yildirim S, Tarim A, Caliskan K, Ezer A, Noyan T. Burns in southern Turkey: electrical burns remain a major problem. The Journal of Burn Care and Rehabilitation. 2003;24:309–14. doi: 10.1097/01.BCR.0000085876.28504.EE. [DOI] [PubMed] [Google Scholar]
- Ogundipe KO, Adigun IA, Solagberu BA. Economic burden of drug use in patients with acute burns: experience in a developing country. Journal of Tropical Medicine. 2009;2009:734712. doi: 10.1155/2009/734712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olukoga A. Cost analysis of road traffic crashes in South Africa. Injury Control and Safety Promotion. 2004;11:59–62. doi: 10.1076/icsp.11.1.59.26304. [DOI] [PubMed] [Google Scholar]
- Perez-Nunez R, Avila-Burgos L, Hijar-Medina M, et al. Economic impact of fatal and non-fatal road traffic injuries in Guadalajara Metropolitan Area and Jalisco, Mexico. Injury Prevention. 2011;17:297–303. doi: 10.1136/ip.2010.027995. [DOI] [PubMed] [Google Scholar]
- Perez-Nunez R, Hijar-Medina M, Heredia-Pi I, Jones S, Silveira-Rodrigues EM. Economic impact of fatal and nonfatal road traffic injuries in Belize in 2007. Pan American Journal of Public Health. 2010;28:326–36. [PubMed] [Google Scholar]
- Pham KH, Le Thi QX, Petrie DJ, Adams J, Doran CM. Households’ willingness to pay for a motorcycle helmet in Hanoi, Vietnam. Applied Health Economics and Health Policy. 2008;6:137–44. doi: 10.1007/BF03256128. [DOI] [PubMed] [Google Scholar]
- Plummer JM, Brown H, Jones K, Fearon-Boothe D, Meeks-Aitken N, Mcdonald AH. Trauma: the burden of a preventable problem. The West Indian Medical Journal. 2010;59:26–8. [PubMed] [Google Scholar]
- Rahman F, Bose S, Linnan M, et al. Cost-effectiveness of an injury and drowning prevention program in Bangladesh. Pediatrics. 2012;130:e1621–8. doi: 10.1542/peds.2012-0757. [DOI] [PubMed] [Google Scholar]
- Razzak JA, Bhatti JA, Ali M, Khan UR, Jooma R. Average out-of-pocket healthcare and work-loss costs of traffic injuries in Karachi, Pakistan. International Journal of Injury Control and Safety Promotion. 2011;18:199–204. doi: 10.1080/17457300.2011.551942. [DOI] [PubMed] [Google Scholar]
- Reddy GM, Negandhi H, Singh D, Singh AJ. Extent and determinants of cost of road traffic injuries in an Indian city. Indian Journal of Medical Sciences. 2009;63:549–56. [PubMed] [Google Scholar]
- Riewpaiboon A, Piyauthakit P, Chaikledkaew U. Economic burden of road traffic injuries: a micro-costing approach. The Southeast Asian Journal of Tropical Medicine and Public Health. 2008;39:1139–49. [PubMed] [Google Scholar]
- Rodrigues RI, Cerqueira DR, Lobao WJ, Carvalho AX. The cost of violence for the public health system in Brazil: available data and possibilities for estimation. Cadernos de Saude Publica. 2009;25:29–36. doi: 10.1590/s0102-311x2009000100003. [DOI] [PubMed] [Google Scholar]
- Sahin I, Ozturk S, Alhan D, Acikel C, Isik S. Cost analysis of acute burn patients treated in a burn centre: the Gulhane experience. Annals of Burns and Fire Disasters. 2011;24:9–13. [PMC free article] [PubMed] [Google Scholar]
- Sangowawa AO, Owoaje ET, Ekanem SE, Faseru B, Adekunle BJ. Economic costs of motorcycle injury among crash-involved commercial motorcyclists in Oyo State, Nigeria. African Journal of Medicine and Medical Sciences. 2011;40:385–91. [PubMed] [Google Scholar]
- Scuffham PA. Cost-effectiveness analyses for injury prevention initiatives in low- and middle-income countries. Injury Prevention. 2008;14:217–19. doi: 10.1136/ip.2008.019315. [DOI] [PubMed] [Google Scholar]
- Sculpher MJ, Pang FS, Manca A, et al. Generalisability in economic evaluation studies in healthcare: a review and case studies. Health Technology Assessment. 2004;8:1–4. doi: 10.3310/hta8490. [DOI] [PubMed] [Google Scholar]
- Shemilt I, Mugford M, Byford S, et al. Incorporating economics evidence. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. Cambridge: The Cochrane Collaboration; 2009. [Google Scholar]
- Soyer T, Deniz T, Akman H, et al. The impact of Pediatric Trauma Score on burden of trauma in emergency room care. The Turkish Journal of Pediatrics. 2009;51:367–70. [PubMed] [Google Scholar]
- Thanh NX, Hang HM, Chuc NT, Lindholm L. The economic burden of unintentional injuries: a community-based cost analysis in Bavi, Vietnam. Scandinavian Journal of Public Health. 2003;62:45–51. doi: 10.1080/14034950310015103. [DOI] [PubMed] [Google Scholar]
- The Cochrane Collection. The Cochrane Library [Online] 2013. John Wiley & Sons, Inc. http://www.cochrane.org/, accessed 24 March 2013.
- The World Bank. World Bank Data Urban Population. Washington, DC: The World Bank; 2012. [Google Scholar]
- Ward E, Mccartney T, Brown DW, et al. Results of an exercise to estimate the costs of interpersonal violence in Jamaica. The West Indian Medical Journal. 2009;58:446–51. [PubMed] [Google Scholar]
- Waters HR, Hyder AA, Phillips TL. Economic evaluation of interventions to reduce road traffic injuries – a review of the literature with applications to low and middle-income countries. Asia-Pacific Journal of Public Health. 2004;16:23–31. doi: 10.1177/101053950401600105. [DOI] [PubMed] [Google Scholar]
- World Bank. Data: How We Classify Countries [Online] Washington, DC: The World Bank; 2011. http://data.worldbank.org/about/country-classifications, accessed 16 April 2012. [Google Scholar]
- World Bank. GDP per Capita (USD$) for 2010. Washington, DC: World Bank; 2013. [Google Scholar]
- World Health Organization. Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- World Health Organization. Choosing Interventions that are Cost Effective (WHO-CHOICE) [Online] Geneva, Switzerland: World Health Organizaiton; 2011a. http://www.who.int/choice/en/, accessed 20 March 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Estimated DALYs per 100,000 population by cause, and Member State, 2004 [Online] 2011b World Health Organization. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html, accessed 18 March 2013. [Google Scholar]
- Yan-Hong L, Rahim Y, Wei L, et al. Pattern of traffic injuries in Shanghai: implications for control. International Journal of Injury Control and Safety Promotion. 2006;13:217–25. doi: 10.1080/17457300600580779. [DOI] [PubMed] [Google Scholar]
- Yin Z, Qin Z, Xin W, Gomez M, Zhenjiang L. The characteristics of elderly burns in Shanghai. Burns. 2010;36:430–5. doi: 10.1016/j.burns.2009.06.204. [DOI] [PubMed] [Google Scholar]
- Zaza S, Briss PA, Harris KW, Services TF OC P . The Guide To Community Preventive Services: What Works To Promote Health? Oxford: Oxford University Press; 2005. [Google Scholar]
- Zhao J, Huang C, Liu M, Li X, Yan L, Yuan X. The analysis of medical-related cost for in-patients with injuries in Ningxia region. Chinese Journal of Preventive Medicine. 2002;36:374–7. [PubMed] [Google Scholar]
- Zhou Y, Baker TD, Rao K, Li G. Productivity losses from injury in China. Injury Prevention. 2003a;9:124–7. doi: 10.1136/ip.9.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou YP, Jiang ZM, Sun YH, Wang XR, Ma EL, Wilmore D. The effect of supplemental enteral glutamine on plasma levels, gut function, and outcome in severe burns: a randomized, double-blind, controlled clinical trial. Journal of Parenteral and Enteral Nutrition. 2003b;27:241–5. doi: 10.1177/0148607103027004241. [DOI] [PubMed] [Google Scholar]