Introduction
Asthma is one of the most common chronic conditions in the United States, and prevalence is currently at historically high levels. The most recent figures from the Centers for Disease Control and Prevention (CDC) reveal that approximately 13% of adults have ever been told they have asthma, and 8% still have asthma.1 Asthma is marked by significant health disparities, with certain population subgroups exhibiting increased prevalence and worse health outcomes. One such group is older asthmatic women, in whom the highest asthma mortality rate is seen.
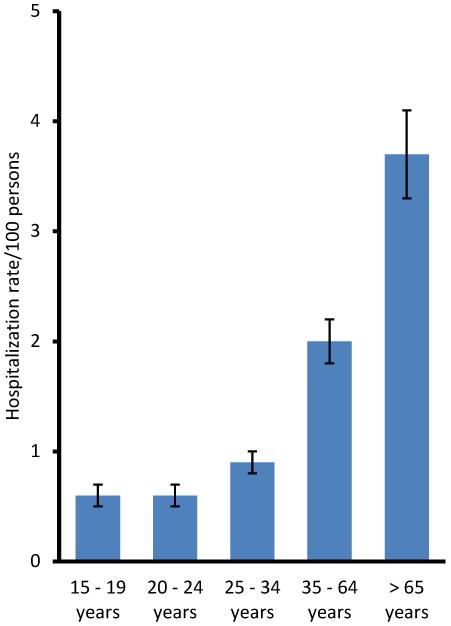
While the prevalence of asthma in the elderly is no different than the general population, the morbidity and mortality figures are strikingly worse. For example, the death rate among those above 65 is by far the highest, nearly four times higher than the overall average.2 Moreover, physician office visits per 100 persons with asthma are highest in those over 65.3 Although the rate of emergency department visits is no higher than other age groups, hospitalizations are again disproportionately higher among older adults (Figure 1). This suggests that older adults with asthma who visit the emergency room are more likely to require hospitalization, and are more likely to have a fatal asthma event, than other age groups.
Figure 1.
Asthma hospitalization rates by detailed age group: United States, average annual rate 2007 – 2009. Data presented as mean +/− SE mean. Vital Health Stat 3(35). 2012.
Gender discrepancies in asthma prevalence and outcomes are evident. Among all adults, women are significantly more likely to report asthma than men (9.9 vs. 6.2%). In those over 65, 9.1% of older women and 5.7% of older men noted current asthma in 2011.4 Among the elderly, it is women who suffer most from asthma. From 2007 – 2009, the asthma mortality rate was by far the highest in women over age 65, and this rate was 30% higher than men over age 65.2 The asthma death rate among older women is approximately four times higher than the overall total. Women over age 65 are also nearly twice as likely as men over age 65 to visit the emergency department for asthma. When considering asthma hospitalization rates by age and gender, older women had the highest rate of any sub-group.3 Therefore, understanding and improving asthma outcomes for older women is desperately needed in order to decrease health care costs, improve outcomes, and reduce health disparities.
Until recently, little research has focused on the unique asthma challenges of women or the elderly. The purpose of this paper is to examine factors that may contribute to the unequal burden of asthma among older women, and to present practical solutions to improve care in this population.
Menopause and hormone replacement therapy
Several studies have documented the effects of hormones such as estrogen and progesterone on airway caliber and asthma exacerbations. During the perimenopausal period, significant fluctuations in estrogen levels are observed; after menopause the gap between estrogen and progesterone levels is pronounced due to a higher estrogen:progesterone ratio, though levels of both hormones decrease.5 While the relative risk of new-onset asthma is not affected by menopause, this is not true for menopausal women on hormone replacement therapy (HRT). A recent meta-analysis found that post-menopausal women on HRT had an increased risk of asthma compared to premenopausal women.6 Other work has found that the use of postmenopausal HRT was associated with a 2.24 fold increase in newly diagnosed asthma, but not COPD.7
Conversely, in women with pre-existing asthma, HRT is often associated with improvement in respiratory symptoms and decreased asthma exacerbations.8 Menopause tends to increase the number of asthma exacerbations.5,9 In fact, the peak age for asthma exacerbations in women occurs at 50,10 which is also the mean age of menopause in the United States. This may indicate that sex hormones have a protective effect in asthma, or that fluctuations in estrogen levels can be particularly detrimental. A large study of 1200 asthmatic women found that significant respiratory symptoms were nearly twice as common during the perimenopausal period, and FEV1 decreased by approximately 150 mL.11 Asthma in women that begins after menopause can be quite problematic. This phenotype of asthma is frequently severe, nonatopic, and often requires oral corticosteroids for control.12 The risks and benefits of HRT must be considered, and the asthma specialist is in a unique position to offer specific information to assist in making decisions about HRT.
Side effects of medications
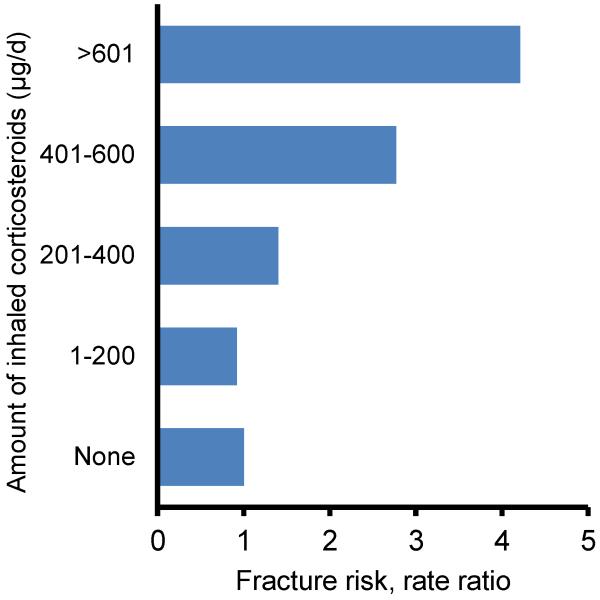
Elderly women may be particularly at risk from adverse effects of inhaled corticosteroids (ICS). Post-menopausal women (but not premenopausal women) treated with an ICS showed significantly lower bone mineral density than age-matched controls.13 A large study of over 1600 elderly individuals with either asthma or COPD (mean age 81 years) who denied any historical use of oral corticosteroids found a dose-dependent positive association for fracture risk with the use of inhaled corticosteroids, with those on high dose ICS having a 4.5 fold increased risk compared to those never exposed (Figure 2).14 As post-menopausal women make up the great majority of those with osteoporosis, special attention must be given to the screening, prevention, and treatment of this disorder for those on an ICS. Other systemic effects of ICS, such as glaucoma, cataracts, and adrenal suppression, are also more common in the elderly,15,16 and should be evaluated in older asthmatic women. Given the tremendous morbidity associated with adverse effects from an ICS, all older women with asthma who require inhaled corticosteroids should have periodic bone mineral density screenings and an ophthalmological examination. It is important to acknowledge that ICS use is currently the cornerstone of chronic asthma management, and therefore the benefits may outweigh the risks.
Figure 2.
Relation between inhaled corticosteroids and fracture incidence in model adjusted for gender, age, oral corticosteroid use, short-acting β-agonist use, nebulizer use, use of theophyllines, and a diagnosis of asthma and/or COPD. Chest. Oct 2006; 130(4):1082
Treatment of comorbidities can also be problematic for older adults with asthma. Beta-blockers, aspirin, and NSAIDS may all be used for a variety of conditions, and each may also worsen asthma. Dysrhythmias are far more common in the elderly with β-agonists use, especially in those who have previously suffered a myocardial infarction.17 The elderly are more likely to suffer tremor and nausea with β-agonists use.18 Therefore, a comprehensive history and careful investigation for medication side effects is critical when caring for the older woman with asthma.
Perception of breathlessness
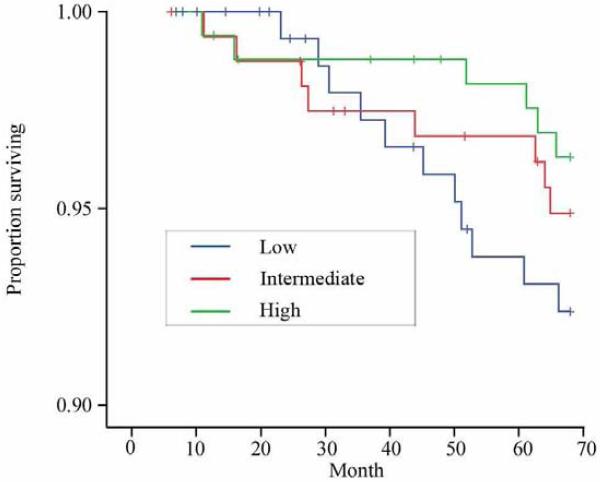
An important mechanism to prevent the progression of an asthma exacerbation is early intervention and treatment.19 Unfortunately, the elderly have a decreased perception of airflow obstruction.20,21 Altered perception of airflow limitation has also been demonstrated in women as compared to men, although the mechanisms that explain these differences are unclear and may be multifactorial.22,23 A recent study of elderly individuals (64% female) found that those with a decreased perception of airflow obstruction had greater medication costs, hospitalizations, and mortality compared to elderly individuals with a better perception of dyspnea (Figure 3).24
Figure 3.
Kaplan-Meier curves for survival of subjects according to the perception of dyspnea. Frontiers in physiology. 2012;3:238
One tool that may help to overcome the decreased perception of breathlessness in older women is self-monitoring with a peak flow meter (PFM). The current National Institute of Health (NIH) asthma guidelines recommend self-monitoring as an important component of asthma self-management, and considers this an ‘Evidence Level A’ recommendation.19 The guidelines go on to state that a PFM should strongly be considered for certain subgroups of asthma patients, including those who have a poor perception of airflow obstruction. Therefore, we advocate for the use of a PFM for older women with asthma.
Comorbidities
Among adults with asthma, more than half report one or more coexisting health conditions, with higher rates among women.25 As people age, it is not surprising that the number of medical conditions and medications to manage these conditions increases. In the United States, a staggering 40% of those above the age of 65 use 5 or more prescription medications on a daily basis.26 Patients with multiple chronic medical problems have several challenges to ensure optimal management of each of their conditions. There can be interactions between conditions, difficulties in determining which medical problem is primarily active when the symptoms are similar, decreased adherence with multiple medications, and conflicting recommendations in self-care management.27 One study of older adults with asthma (in which women comprised 85% of the cohort) found that some patients with coexisting cardiac disease and asthma had been instructed by their physician to try medications for both conditions simultaneously and/or sequentially during episodes of dyspnea.28 Medication and self-management costs can increase exponentially in elderly patients with multiple comorbidities, and therefore certain conditions may receive suboptimal care due to a lower prioritization by the individual.29
Recent data have shown that women with multiple comorbidities often feel that asthma is not their primary health problem. In a qualitative study of 25 African American asthmatic women (mean age 52) with an average of 5.7 chronic conditions in addition to asthma, fewer than half named asthma as a top priority, either alone or in combination with another condition such as heart disease, diabetes, or arthritis.30 These women admitted that asthma takes a “backseat” to other conditions, especially during asymptomatic periods; however, they also noted that asthma interferes with recommended physical activity for management of comorbidities.
To improve care of the older asthmatic woman, clinicians should consider discussing the importance of chronic disease management with multiple comorbidities. For example, highlighting that suboptimal asthma control can make exercise and weight loss problematic can impress upon the patient the importance of regular asthma care. Control of asthma may make it possible for the older woman to reduce the burden of other conditions including cardiac disease, diabetes and arthritis.
Depression
A comorbidity that deserves special attention for older women is depression. Multiple studies have demonstrated that asthma is associated with depression, and that more severe asthma is associated with a greater risk and severity of depression.31,32 This relationship is especially pronounced in elderly women. A study of 317 inner-city older asthma patients (83% female) found that depressive symptoms were associated with worse asthma control and lower quality of life, along with lower rates of adherence to controller medications.33 Similarly, a study of 77 older adult patients (77% female) found that when comparing multiple demographic, psychological and physiological characteristics (including asthma severity, previous asthma exacerbations, FEV1, exhaled nitric oxide levels, and medical comorbidities), depression was most strongly associated with lower asthma quality of life and control.34
Persistent asthma is a disease that requires daily medications (often inhaled corticosteroids) even if an individual does not have symptoms. Unfortunately, both adherence and outcomes can be significantly worse in those with asthma who also have depression, anxiety, or other mental health disorders. Depression and depressive syndromes have an extremely high prevalence among the elderly female population, with rates ranging from 15 to 35%.35,36 Studies consistently show that the rate is higher among older women than older men.35,37 Treatment of depression among asthma patients of varying age groups has shown an improvement in asthma outcomes.38,39 To optimize care, asthma providers of older women should consider screening patients for depression (for example, with the Geriatric Depression Scale),40 and treat or refer as appropriate.
Obesity
Obesity is on the rise globally, and in the United States it has taken on epidemic proportions. The elderly have the highest prevalence of obesity of any age group – and once again it is women who are most affected. The current overall prevalence of obesity among U.S. adults is 35.7%, yet for women above age 60 it is 42.3%.41 There are also racial/ethnic disparities in the obesity rate among women aged 65 - 74, with 54% of Non-Hispanic black women compared to 39% of Non-Hispanic white women being classified as obese.42
An increased prevalence of asthma has been reported among obese individuals, and this relationship is evident among all racial/ethnic groups.43,44 While the mechanisms through which obesity influences the development and severity of asthma are beyond the scope of this paper, they are thought to involve mechanical, inflammatory, and common etiologic factors.45 Importantly, obesity has more consistently been associated with asthma in women than men.44,46 This may suggest an interactive effect between estrogen/progesterone and obesity. In the obese women with asthma, even modest weight loss is associated with a significant improvement of asthma outcomes.47,48 The asthma specialist should therefore work in partnership with the patient and primary care physician to encourage weight loss for the overweight or obese older woman.
Primary caregivers
As adults grow older, women are often enlisted to serve as the primary caregiver for a spouse, friend or family member with a chronic, serious illness. This has been seen in heart disease, mental illness, and cancer, and COPD.49-51 Such studies consistently highlight that the overwhelming number of caregivers are older women. Unfortunately, these studies also detail a troubling trend – caregivers frequently suffer from stress, depression, anxiety, decreased quality of life, and decreased self-efficacy. To improve outcomes in older women with asthma, physicians should ascertain caregiver duties the patient may have. If identified, additional screening for depression or stress should be considered. Connecting the patient with appropriate resources, including mental health providers, social work services, and community advocacy groups, are activities that the clinician can pursue as appropriate.
Limited income/poverty
Among older adults, poverty is common. A recent report from the U.S. Census Bureau found that approximately 10% of older adults lived below the poverty line.52 Unfortunately, this number has been increasing over the past 10 years due to a variety of factors such as increased medical costs, loss of pension or retirement benefits, spending down assets to qualify for Medicaid and state-sponsored supplemental insurance coverage, and economic recessions requiring spending of retirement savings.53 According to the US Census Bureau, women in the United States enjoy a longer life expectancy than men (81 vs. 76 years), with approximately 60% of those over age 75 being female, and this discrepancy increases with age. However, after adjusting for the increased total number of female compared to male elderly, the rate of poverty in older women is much higher – in fact, elderly women are twice as likely to be living in poverty compared to elderly men.52
Asthma care is often expensive (medication costs, routine office visits, hospitalizations, etc.), and lack of access to care due to poverty is a known risk factor for poor asthma outcomes. Elderly adults who also struggle with poverty are less likely to receive appropriate care for COPD, cancer, and cardiac disease.54 While similar studies have not been conducted among older adults with asthma, it would be expected that a similar pattern exists. Further, women report foregoing care due to cost, or managing asthma through the emergency department as a result of coping with financial burdens.55 Therefore, the asthma provider should assess the financial abilities of older women to comply with recommended therapies. If barriers are encountered, a social worker may be instrumental in helping the patient access government-sponsored programs, health insurance, or pharmaceutical options.
Phenotypes of asthma
In recent years, it has been hypothesized that asthma is a number of distinct syndromes or phenotypes rather than a uniform disease. One of the largest studies examining asthma phenotypes in adults was conducted by the NIH Severe Asthma Research Program (SARP).56 Using cluster analysis, 5 distinct phenotypes were identified based on characteristics such as age of asthma onset, lung function tests, eosinophilia, and health care utilization. One phenotype identified was comprised primarily of women who demonstrated particularly poor lung function and high emergency department/hospitalization rates.
Important differences were observed for this phenotype as compared to the others. The group was overwhelmingly female (71%), obese (mean BMI = 33), less responsive to bronchodilator reversal with albuterol, and had late-onset asthma at a mean age of 42 years. Importantly, this group had the highest incidence of sinus disease and gastroesophageal reflux disease (GERD) of any phenotype, and were the least atopic as determined by skin prick testing and total IgE levels.56
While differences in treatment response are not yet known, the care of older women with asthma may be improved by obtaining information such as age of onset, perceived benefit with albuterol, and a careful review for sinusitis or GERD. For example, in women with late onset asthma who appear nonatopic, medications such as anticholinergic therapy may be more appropriate, though this hypothesis has yet to be formally investigated and merits further exploration. Further, treatment for sinus disease and GERD may be most beneficial for such patients, though again further research is needed in this area.
Asthma care of the elderly
While beyond the scope of this paper, certain features of asthma care of the older adult patient (not specifically women) have been discussed in detail elsewhere, and deserve careful consideration by the clinician. These include difficulties with inhaler use (due to arthritis, impaired inspiratory effort or visual deficiencies), high use of complementary/alternative medicine, increased rates of aspirin exacerbated respiratory disease (AERD), decreased responsiveness to short acting β-agonists, and lower rates of asthma education. The reader is encouraged to read some of the well-written review articles pertaining to these and other issues for care of older adults with asthma.57-60
Conclusion
Older women with asthma represent a specific demographic population who suffer an unequal amount of morbidity and mortality related to the disease. While the reasons behind these disparities continue to be an active area of investigations, there are considerations and treatment strategies that the asthma specialist can currently employ to improve care (Table 1). Better care of this vulnerable population is a goal that researchers and clinicians should strive to achieve.
Table 1. Strategies to improve the care of older women with asthma.
|
Acknowledgments
Financial Support: Supported by the National Institute of Aging/NIH grant 1 R01 AG043401-01A1
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 10. 2012 Jan;(252):1–207. [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Bailey C, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS data brief. 2012 May;(94):1–8. [PubMed] [Google Scholar]
- 3.Moorman JE, Akinbami LJ, Bailey CM, et al. National Surveillance of Asthma: United States, 2001-2010. Vital Health Stat. 3. 2012 Nov;(35):1–67. [PubMed] [Google Scholar]
- 4.Adams PF, Kirzinger WK, Martinez ME, National Center for Health Statistics Summary health statistics for the U.S. population: National Health Interview Survey, 2011. Vital Health Stat. 2012;10(255):1–110. [PubMed] [Google Scholar]
- 5.Balzano G, Fuschillo S, Melillo G, Bonini S. Asthma and sex hormones. Allergy. 2001 Jan;56(1):13–20. doi: 10.1034/j.1398-9995.2001.00128.x. [DOI] [PubMed] [Google Scholar]
- 6.Zemp E, Schikowski T, Dratva J, Schindler C, Probst-Hensch N. Asthma and the menopause: a systematic review and meta-analysis. Maturitas. 2012 Nov;73(3):212–217. doi: 10.1016/j.maturitas.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Barr RG, Wentowski CC, Grodstein F, et al. Prospective study of postmenopausal hormone use and newly diagnosed asthma and chronic obstructive pulmonary disease. Arch. Intern. Med. 2004 Feb 23;164(4):379–386. doi: 10.1001/archinte.164.4.379. [DOI] [PubMed] [Google Scholar]
- 8.Kos-Kudla B, Ostrowska Z, Marek B, Ciesielska-Kopacz N, Kajdaniuk D, Kudla M. Effects of hormone replacement therapy on endocrine and spirometric parameters in asthmatic postmenopausal women. Gynecol. Endocrinol. 2001 Aug;15(4):304–311. [PubMed] [Google Scholar]
- 9.Townsend EA, Miller VM, Prakash YS. Sex differences and sex steroids in lung health and disease. Endocr. Rev. 2012 Feb;33(1):1–47. doi: 10.1210/er.2010-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skobeloff EM, Spivey WH, St Clair SS, Schoffstall JM. The influence of age and sex on asthma admissions. JAMA. 1992 Dec 23-30;268(24):3437–3440. [PubMed] [Google Scholar]
- 11.Real FG, Svanes C, Omenaas ER, et al. Lung function, respiratory symptoms, and the menopausal transition. J. Allergy Clin. Immunol. 2008 Jan;121(1):72–80. e73. doi: 10.1016/j.jaci.2007.08.057. [DOI] [PubMed] [Google Scholar]
- 12.Balzano G, Fuschillo S, De Angelis E, Gaudiosi C, Mancini A, Caputi M. Persistent airway inflammation and high exacerbation rate in asthma that starts at menopause. Monaldi Arch. Chest Dis. 2007 Sep;67(3):135–141. doi: 10.4081/monaldi.2007.484. [DOI] [PubMed] [Google Scholar]
- 13.Fujita K, Kasayama S, Hashimoto J, et al. Inhaled corticosteroids reduce bone mineral density in early postmenopausal but not premenopausal asthmatic women. J. Bone Miner. Res. 2001 Apr;16(4):782–787. doi: 10.1359/jbmr.2001.16.4.782. [DOI] [PubMed] [Google Scholar]
- 14.Hubbard R, Tattersfield A, Smith C, West J, Smeeth L, Fletcher A. Use of inhaled corticosteroids and the risk of fracture. Chest. 2006 Oct;130(4):1082–1088. doi: 10.1378/chest.130.4.1082. [DOI] [PubMed] [Google Scholar]
- 15.Wlodarczyk JH, Gibson PG, Caeser M. Impact of inhaled corticosteroids on cortisol suppression in adults with asthma: a quantitative review. Ann. Allergy. Asthma. Immunol. 2008 Jan;100(1):23–30. doi: 10.1016/S1081-1206(10)60400-0. [DOI] [PubMed] [Google Scholar]
- 16.Cumming RG, Mitchell P, Leeder SR. Use of inhaled corticosteroids and the risk of cataracts. N. Engl. J. Med. 1997 Jul 3;337(1):8–14. doi: 10.1056/NEJM199707033370102. [DOI] [PubMed] [Google Scholar]
- 17.Newnham DM. Asthma medications and their potential adverse effects in the elderly: recommendations for prescribing. Drug Saf. 2001;24(14):1065–1080. doi: 10.2165/00002018-200124140-00005. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigo G, Rodrigo C. Effect of age on bronchodilator response in acute severe asthma treatment. Chest. 1997 Jul;112(1):19–23. doi: 10.1378/chest.112.1.19. [DOI] [PubMed] [Google Scholar]
- 19.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J. Allergy Clin. Immunol. 2007 Nov;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 20.Parameswaran K, Hildreth AJ, Chadha D, Keaney NP, Taylor IK, Bansal SK. Asthma in the elderly: underperceived, underdiagnosed and undertreated; a community survey. Respir. Med. 1998 Mar;92(3):573–577. doi: 10.1016/s0954-6111(98)90311-0. [DOI] [PubMed] [Google Scholar]
- 21.Connolly MJ, Crowley JJ, Charan NB, Nielson CP, Vestal RE. Reduced subjective awareness of bronchoconstriction provoked by methacholine in elderly asthmatic and normal subjects as measured on a simple awareness scale. Thorax. 1992 Jun;47(6):410–413. doi: 10.1136/thx.47.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wijnhoven HA, Kriegsman DM, Snoek FJ, Hesselink AE, de Haan M. Gender differences in health-related quality of life among asthma patients. J. Asthma. 2003 Apr;40(2):189–199. doi: 10.1081/jas-120017990. [DOI] [PubMed] [Google Scholar]
- 23.Osborne ML, Vollmer WM, Linton KL, Buist AS. Characteristics of patients with asthma within a large HMO: a comparison by age and gender. Am. J. Respir. Crit. Care Med. 1998 Jan;157(1):123–128. doi: 10.1164/ajrccm.157.1.9612063. [DOI] [PubMed] [Google Scholar]
- 24.Ebihara S, Niu K, Ebihara T, et al. Impact of blunted perception of dyspnea on medical care use and expenditure, and mortality in elderly people. Frontiers in physiology. 2012;3:238. doi: 10.3389/fphys.2012.00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel MR, Janevic MR, Heeringa SG, Baptist AP, Clark NM. An examination of adverse asthma outcomes in U.S. Adults with multiple morbidities. Annals of the American Thoracic Society. 2013 Oct;10(5):426–431. doi: 10.1513/AnnalsATS.201302-032OC. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics . Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2013. Library of Congress Catalog Number 76-641496. [PubMed] [Google Scholar]
- 27.Bayliss EA, Steiner JF, Fernald DH, Crane LA, Main DS. Descriptions of barriers to self-care by persons with comorbid chronic diseases. Annals of family medicine. 2003 May-Jun;1(1):15–21. doi: 10.1370/afm.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baptist AP, Deol BB, Reddy RC, Nelson B, Clark NM. Age-specific factors influencing asthma management by older adults. Qual. Health Res. 2010 Jan;20(1):117–124. doi: 10.1177/1049732309355288. [DOI] [PubMed] [Google Scholar]
- 29.Schoenberg NE, Leach C, Edwards W. “It’s a toss up between my hearing, my heart, and my hip”: prioritizing and accommodating multiple morbidities by vulnerable older adults. J. Health Care Poor Underserved. 2009 Feb;20(1):134–151. doi: 10.1353/hpu.0.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Janevic MR, Ellis KR, Sanders GM, Nelson BW, Clark NM. Self-management of multiple chronic conditions among African American women with asthma: a qualitative study. J. Asthma. 2013 Nov 22; doi: 10.3109/02770903.2013.860166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong KO, Hunter Rowe B, Douwes J, Senthilselvan A. Asthma and wheezing are associated with depression and anxiety in adults: an analysis from 54 countries. Pulmonary medicine. 2013;2013:929028. doi: 10.1155/2013/929028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yonas MA, Marsland AL, Emeremni CA, Moore CG, Holguin F, Wenzel S. Depressive symptomatology, quality of life and disease control among individuals with well-characterized severe asthma. J. Asthma. 2013 Oct;50(8):884–890. doi: 10.3109/02770903.2013.810750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krauskopf KA, Sofianou A, Goel MS, et al. Depressive symptoms, low adherence, and poor asthma outcomes in the elderly. J. Asthma. 2013 Apr;50(3):260–266. doi: 10.3109/02770903.2012.757779. [DOI] [PubMed] [Google Scholar]
- 34.Ross JA, Yang Y, Song PX, Clark NM, Baptist AP. Quality of life, health care utilization, and control in older adults with asthma. Journal of Allergy and Clinical Immunology: In Practice. 2013;(1):157–162. doi: 10.1016/j.jaip.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 35.Barry LC, Allore HG, Guo Z, Bruce ML, Gill TM. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch. Gen. Psychiatry. 2008 Feb;65(2):172–178. doi: 10.1001/archgenpsychiatry.2007.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br. J. Psychiatry. 1999 Apr;174:307–311. doi: 10.1192/bjp.174.4.307. [DOI] [PubMed] [Google Scholar]
- 37.Weissman MM, Olfson M. Depression in women: implications for health care research. Science. 1995 Aug 11;269(5225):799–801. doi: 10.1126/science.7638596. [DOI] [PubMed] [Google Scholar]
- 38.Brown ES, Vornik LA, Khan DA, Rush AJ. Bupropion in the treatment of outpatients with asthma and major depressive disorder. Int. J. Psychiatry Med. 2007;37(1):23–28. doi: 10.2190/D235-2285-2121-6724. [DOI] [PubMed] [Google Scholar]
- 39.Brown ES, Howard C, Khan DA, Carmody TJ. Escitalopram for severe asthma and major depressive disorder: a randomized, double-blind, placebo-controlled proof-of-concept study. Psychosomatics. 2012 Jan-Feb;53(1):75–80. doi: 10.1016/j.psym.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J. Psychiatr. Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 41.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS data brief. 2012 Jan;(82):1–8. [PubMed] [Google Scholar]
- 42.Fakhouri TH, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007-2010. NCHS data brief. 2012 Sep;(106):1–8. [PubMed] [Google Scholar]
- 43.Ford ES. The epidemiology of obesity and asthma. J. Allergy Clin. Immunol. 2005 May;115(5):897–909. doi: 10.1016/j.jaci.2004.11.050. quiz 910. [DOI] [PubMed] [Google Scholar]
- 44.Camargo CA, Jr., Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch. Intern. Med. 1999 Nov 22;159(21):2582–2588. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 45.Boulet LP. Asthma and obesity. Clin. Exp. Allergy. 2013 Jan;43(1):8–21. doi: 10.1111/j.1365-2222.2012.04040.x. [DOI] [PubMed] [Google Scholar]
- 46.Kim S, Camargo CA., Jr. Sex-race differences in the relationship between obesity and asthma: the behavioral risk factor surveillance system, 2000. Ann. Epidemiol. 2003 Nov;13(10):666–673. doi: 10.1016/s1047-2797(03)00054-1. [DOI] [PubMed] [Google Scholar]
- 47.Aaron SD, Fergusson D, Dent R, Chen Y, Vandemheen KL, Dales RE. Effect of weight reduction on respiratory function and airway reactivity in obese women. Chest. 2004 Jun;125(6):2046–2052. doi: 10.1378/chest.125.6.2046. [DOI] [PubMed] [Google Scholar]
- 48.Hakala K, Stenius-Aarniala B, Sovijarvi A. Effects of weight loss on peak flow variability, airways obstruction, and lung volumes in obese patients with asthma. Chest. 2000 Nov;118(5):1315–1321. doi: 10.1378/chest.118.5.1315. [DOI] [PubMed] [Google Scholar]
- 49.Barnes S, Gott M, Payne S, et al. Characteristics and views of family carers of older people with heart failure. International journal of palliative nursing. 2006 Aug;12(8):380–389. doi: 10.12968/ijpn.2006.12.8.380. [DOI] [PubMed] [Google Scholar]
- 50.Barber FD. Effects of social support on physical activity, self-efficacy, and quality of life in adult cancer survivors and their caregivers. Oncol. Nurs. Forum. 2013 Sep;40(5):481–489. doi: 10.1188/13.ONF.481-489. [DOI] [PubMed] [Google Scholar]
- 51.Nordtug B, Krokstad S, Sletvold O, Holen A. Differences in social support of caregivers living with partners suffering from COPD or dementia. International journal of older people nursing. 2013 May;8(2):93–103. doi: 10.1111/j.1748-3743.2011.00302.x. [DOI] [PubMed] [Google Scholar]
- 52.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2012. U.S. Census Bureau. U.S. Government Printing Office; 2013. pp. 60–245. [Google Scholar]
- 53.Banerjee S. Time Trends in Poverty for Older Americans Between 2001-2009. Vol. 33. Employee Benefit Research Institute; 2012. [Google Scholar]
- 54.Rathore SS, Berger AK, Weinfurt KP, et al. Race, sex, poverty, and the medical treatment of acute myocardial infarction in the elderly. Circulation. 2000 Aug 8;102(6):642–648. doi: 10.1161/01.cir.102.6.642. [DOI] [PubMed] [Google Scholar]
- 55.Patel MR, Caldwell CH, Id-Deen E, Clark NM. Experiences addressing health-related financial challenges with disease management among African American women with asthma. J. Asthma. 2014 Jan 28; doi: 10.3109/02770903.2014.885040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am. J. Respir. Crit. Care Med. 2010 Feb 15;181(4):315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gibson PG, McDonald VM, Marks GB. Asthma in older adults. Lancet. 2010 Sep 4;376(9743):803–813. doi: 10.1016/S0140-6736(10)61087-2. [DOI] [PubMed] [Google Scholar]
- 58.Mathur SK. Allergy and asthma in the elderly. Seminars in respiratory and critical care medicine. 2010 Oct;31(5):587–595. doi: 10.1055/s-0030-1265899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jones SC, Iverson D, Burns P, Evers U, Caputi P, Morgan S. Asthma and ageing: an end user’s perspective--the perception and problems with the management of asthma in the elderly. Clin. Exp. Allergy. 2011 Apr;41(4):471–481. doi: 10.1111/j.1365-2222.2011.03718.x. [DOI] [PubMed] [Google Scholar]
- 60.Melani AS. Management of asthma in the elderly patient. Clinical interventions in aging. 2013;8:913–922. doi: 10.2147/CIA.S33609. [DOI] [PMC free article] [PubMed] [Google Scholar]