Abstract
Acculturation has been implicated to be associated with physical activity (PA) behaviors in adults; little is known, however, with respect to the pediatric population. The purpose of this study was to determine whether cardiorespiratory fitness (VO2max) and/or PA were associated with acculturation status in overweight Hispanic children. In a sample of 144 children 8–13 years old, acculturation status was determined by place of birth: foreign born (n = 17), 1st generation (n = 101), or 2nd/3rd generation (n = 26), and by questionnaire: less assimilated (n = 76) or more assimilated (n = 34). VO2max was measured using a treadmill protocol, PA was assessed by questionnaire, and body composition by DEXA. ANOVA and ANCOVA were used to determine unadjusted and adjusted group differences, respectively. After adjusting for covariates, the 2nd/3rd generation group had significantly higher VO2max compared with the 1st generation group: 2.26 ± 0.20 L/min vs. 2.15 ± 0.19 L/min, p = .03. No differences were noted for PA, however. Acculturation to the U.S. is associated with higher VO2max in overweight Hispanic children. Longitudinal analyses are needed to determine whether these fitness differences confer protective health effects in this at-risk population.
Acculturation is defined as “when people from differing backgrounds come into contact with one another and interchange cultural attitudes and behaviors” (2). These interchanges often result in the adaptation and assimilation of traits from the dominant culture, which lead to changes in behaviors. Recent increases in immigration to the U.S. have created a large population of first- and second-generation children and adolescents who experience cultural influences from both the U.S. and the country of their ancestral origin (22). Such is the case for Hispanic children born in the U.S., who are now estimated to account for more than 50% of all births in California (10). It is therefore of great interest to investigate how this intermix of cultural influences might affect the health status and health behaviors of this population.
The association between acculturating to the U.S. and lifestyle behaviors and risk for chronic disease has been investigated almost exclusively in adults. Evidence from these studies suggests that the acculturation process is negatively associated with health and health behaviors. For example, one study reported that among Mexican Americans living in the U.S., English speakers had a diet higher in fat compared with Spanish-Speakers (32). Similarly, another study found that among U.S. residents (NHANES III; 5), Mexican Americans born in the U.S. adopted a high-fat, low-fiber diet compared with those born in Mexico, regardless of language spoken (5). Others have reported that diabetes was more common among highly acculturated individuals (31) and that U.S. born Spanish speaking women and men had the largest adjusted waist circumference, and the women were more likely to have at least one risk factor for cardiovascular disease (25). Despite methodological limitations concerning the use of birthplace and language spoken as measures of acculturation, these studies together provide evidence for the possible negative effects that acculturating to the U.S. has on the health and health behaviors of Mexican immigrants.
Studies in U.S. pediatric populations have indicated that acculturation is also a risk factor for unhealthy behaviors among adolescents including smoking (29) and disordered eating (9). Epidemiologic evidence revealed that Asian and Hispanic adolescents born in the U.S. are more than twice as likely to be obese compared with adolescents of the same ethnicity who are born outside the U.S. (21). Similarly, Gordon-Larsen et al. (8) reported that rapid acculturation to overweight-related behaviors such as diet, smoking, and inactivity was evident in U.S.-born versus foreign-born adolescent immigrants. Although evidence is limited compared with the adult literature, these studies also suggest that acculturation is associated with poorer health and health behaviors in U.S.-born children.
The epidemics of obesity and Type 2 diabetes in Hispanic children likely stem from a complexity of social and cultural factors that might involve physical activity (PA) and cardiorespiratory fitness (VO2max) (14, 16). Culturally driven health behaviors related to obesity such as the nature and type of physical activity a child engages in might partially explain the association between obesity and acculturation. Furthermore, such culturally bound physical activity behaviors can also be associated with differing levels of VO2max among acculturation groups. It is critical to develop a better understanding of how the degree of acculturation to the U.S. might influence such factors in order to determine appropriate lifestyle interventions for these populations. Furthermore, better uses of appropriate and validated measures of acculturation are necessary to support the current literature. Therefore, the purpose of this study was to determine whether VO2max and PA were associated with degree of acculturation in overweight Hispanic children. We hypothesized that both VO2max and PA would be lower in the more acculturated groups.
Methods
Sample
The current sample included 78 boys and 66 girls (N = 144) who were enrolled in the University of Southern California (USC) Study of Latino Adolescents at Risk for Type 2 Diabetes project (SOLAR). Participants were recruited from the greater Los Angeles area through medical referrals, advertisements, and word of mouth. Inclusion criteria for enrollment in this study were: a) ages 8–13 years; b) Hispanic descent (all four grandparents of Hispanic descent); c) age- and gender-specific BMI ≥ 85th percentile; d) a family history of Type 2 diabetes (sibling, parent, or grandparent); and e) absence of diabetes mellitus before enrollment as determined by an oral glucose tolerance test at the USC General Clinic Research Center (GCRC). Exclusion criteria were: a) taking medications known to influence body composition, insulin action, or insulin secretion; b) diagnosed with a syndrome or disease that could influence insulin action or secretion or body composition; and c) previously diagnosed with any major illness since birth. The primary analysis included participants who completed both outpatient and inpatient visits and had complete data on body composition and VO2max. Participants with extremely high self-reported physical activity values (i.e. implausible values such as 89 hours/week) were excluded (n = 4). The secondary analysis was a subset of the primary sample (n= 110). Participants with missing or incomplete data on an acculturation questionnaire were excluded (n = 20), as well as those with a cultural assimilation score equal to 4 (n = 14; this will be further explained in the acculturation section). Parents provided informed consent and children provided informed assent before the beginning of the research procedures. The USC Health Sciences Campus Institutional Review Board (IRB) approved this study.
Outpatient Visit
Participants arrived at the USC GCRC at approximately 8:00 a.m. after an overnight 12-hour fast. Height and weight were measured (to the nearest 0.1 cm and 0.1 kg, respectively) using a wall-mounted stadiometer and a balance beam scale with participants wearing light clothing and no shoes. A pediatrician administered a medical history and physical (H&P) examination and determined physical maturation based on breast development in girls and pubic hair growth in boys (17,18).
Inpatient Visit
Participants returned to the USC GCRC at least 7 days after their outpatient visit at approximately 1:00 pm. Height, weight, and a brief H&P were performed as described for the outpatient visit.
Body Composition
Body composition was estimated using a Hologic QDR 4500W (Bedford, MA) dual-energy X-ray absorptiometry (DEXA) scan of the total body (fat mass, lean tissue mass, and bone mineral content). Intra-abdominal adipose tissue (IAAT) and subcutaneous abdominal adipose tissue (SAAT) were measured by magnetic resonance imaging (MRI) of a single-slice axial TR 400/16 view of the abdomen at the umbilicus using a General Electric 1.5 Signa LX-Echospeed with a General Electric 1.5-Tesla magnet (Waukesha, WI).
VO2max
VO2max was assessed by an all-out, progressive, continuous treadmill protocol (27). Respiratory gases were collected and measured using open circuit spirometry and analyzed on a MedGraphics CardioO2/CP Combined Exercise System (St. Paul, MN). Heart rate was continuously measured using a Polar Vantage XL heart rate monitor (Port Washington, NY). Participants achieved VO2max if they satisfied two of the following three criteria: a) respiratory exchange ratio (RER) > 1.0; b) heart rate ≥ 195; and c) plateau of VO2 defined as < 2 ml · kg−1 · min−1 increase in VO2 with a concomitant increase in workload. Participants were familiarized with exercise procedures and equipment before the beginning of the exercise test. A warm-up period of 4 min at 0% grade and 4km/hr was followed by an increase in grade to 10%. Workload was increased by elevating the treadmill grade 2.5% at 2-min stages. Treadmill speed remained constant until 22.5% grade was reached, at which time the speed was increased by 0.6 km/hr until the participant was no longer able to continue.
Questionnaires
Questionaires were used to estimate past-year and past-week leisure and occupational physical activity (15). These instruments have been validated in minority populations (Native Americans) ages 10–59 years through comparisons with physical activity monitors, which demonstrated significant rank-order correlations between 0.62 and 0.96. These instruments were translated into Spanish to be used in our sample. Participants were asked to recall and estimate time spent at various types of activities (e.g. walking, running, playing sports, etc.,) for the previous 12 months. The average number of hours of recreational PA per week was calculated to represent the activity level of each child. Other PA questions included: estimation of the number of sports that the child participated in that were of moderate-to-vigorous intensity outside and inside school in the past year; number of days per week that the child attended physical education (PE) class; and duration of sports activities in PE class. Social economic status (SES) was estimated by the Hollingshead Index of Social Position (ISP) formula: SES = (Occupation score × 7) + (Education score × 4) (11). The highest parental occupation and education were assigned a score from occupation and education scales ranging from 1 to 7 (where 1 equaled the highest possible score and 7 equaled the lowest possible score for both occupation and education). These scores were inserted into the ISP formula to calculate SES. SES scores ranged from 11 to 77 (high SES to low SES, respectively).
Acculturation
Acculturation status for the primary analysis was determined by categorizing participants into three distinct groups on the basis of birthplace for both the child and the parents (such methods have been used in other studies; (21,25). The three acculturation categories were: a) 2nd/3rd generation—both child and one or both parents born in the U.S.; b) 1st generation—child born in U.S. and both parents born outside U.S.; and c) foreign born—child and both parents born outside the U.S. For the secondary analysis, the Acculturation, Habits, and Interests Multicultural Scale for Adolescents (AHIMSA) acculturation scale was used as a secondary method for measuring acculturation (28). This instrument contains easy to read and understand questions that can be used for younger participants.
Briefly, the AHIMSA scale consisted of eight questions related to the child’s cultural preference of friends, music, TV shows, and foods. Each question had four possible answers that correspond to one of four acculturation orientations (e.g., the U.S., the country my family is from, both, or neither). The AHIMSA scale generates four scores based on the four orientations: assimilation, separation, integration, and marginalization. For this study, assimilation scores were used as a measure of acculturation because this construct determines the level of adaptation to U.S. culture (i.e., more assimilated = more acculturated). Assimilation scores range between 0 and 8, and participants were categorized into 2 groups: Participants with an assimilation score ≥ 5 were considered more assimilated (n = 34), and those with an assimilation score ≤ 3 were considered less assimilated (n = 76). We aimed to establish discrete and well-defined categories of acculturation, thus participants with an assimilation score of 4 were excluded from the analysis because they represented a relatively small group and because their acculturation status was not well defined.
Statistical Analysis
Dependent variables were tested for normality and log transformed if determined to be not normally distributed. The following variables were log transformed: weight, BMI, BMI percentile, total fat mass, total lean tissue mass, IAAT, SAAT, total hours of PA per week, and all other PA variables. Analyses of variance (ANOVA) and covariance (ANCOVA) were used to determine unadjusted and adjusted differences between acculturation groups, respectively. Subsequently, the Tukey post-hoc analysis with Bonferroni adjustments was used to determine differences among acculturation groups when the F test was statistically significant. Independent sample t tests and ANCOVA were also used to examine unadjusted and adjusted assimilation group differences, respectively. Nonparametric tests such as the Kruskal-Wallis test and the Wilcoxon Rank sum test were used for group comparisons of dependent variables that remained nonnormally distributed after log transformation. The chi-square test was used to test the proportion of assimilation among the three generational acculturation categories. Log transformed data were untransformed after analysis and are presented as geometric means and standard deviations. All statistical tests were performed using SPSS®/PC statistical program (version 11.0 for Windows®; SPSS, Inc., Chicago, IL). The level of significance was predetermined at α < .05.
Results
Primary Analysis by Generation Status
Unadjusted analyses showed that there were no significant differences in age, Tanner stage, height, weight, BMI, BMI percentile, % fat, total lean tissue mass, total fat mass, SES, IAAT, and SAAT among acculturation groups (Table 1). Similarly, there were no unadjusted group differences noted in absolute or relative VO2max, max HR, max RER or PA (Table 2).
Table 1.
Unadjusted Subject Characteristics for Demographics, Anthropometrics, and Body Composition by Acculturation Groups (Mean ± SD)
| Foreign born (n = 17) | 1st generation (n = 101) | 2nd/3rd generation (n = 26) | Total (N = 144) | |
|---|---|---|---|---|
| Boys (n; %) | (9; 52.9) | (57; 56.4) | (12; 46.2) | (78; 54.2) |
| Girls (n; %) | (8; 47.1) | (44; 43.6) | (14; 53.8) | (66; 45.8) |
| Age (years) | 11.9 ± 1.7 | 11.1 ± 1.7 | 10.9 ± 1.7 | 11.2 ± 1.70 |
| Tanner stage | 2.8 ± 1.5 | 2.2 ± 1.4 | 2.1 ± 1.2 | 2.3 ± 1.4 |
| Height (cm) | 153.1 ± 11.4 | 149.2 ± 10.5 | 151.1 ± 12.2 | 150.0 ± 11.00 |
| Weight (kg) * | 66.7 ± 18.8 | 61.4 ± 17.2 | 61.8 ± 23.7 | 62.1 ± 17.60 |
| BMI (kg/m2) * | 28.6 ± 4.7 | 27.7 ± 4.8 | 27.3 ± 5.1 | 27.7 ± 4.80 |
| BMI percentile* | 97.5 ± 2.3 | 97.2 ± 2.8 | 96.5 ± 4.0 | 97.1 ± 3.00 |
| Total% fat (%) | 39.3 ± 5.7 | 38.7 ± 5.7 | 37.3 ± 8.0 | 38.5 ± 6.20 |
| Total fat mass (kg) * | 25.6 ± 9.2 | 23.1 ± 8.6 | 22.0 ± 10.4 | 23.2 ± 9.10 |
| Total lean mass (kg) * | 38.3 ± 10.2 | 35.5 ± 9.0 | 36.4 ± 10.4 | 36.0 ± 9.30 |
| Total BMC (kg) | 16.99 ± 4.2 | 15.37 ± 3.9 | 15.73 ± 4.7 | 15.62 ± 4.100 |
| Total BMD (g/cm2) | 0.96 ± 0.1 | 0.92 ± 0.1 | 0.93 ± 0.1 | 0.92 ± 0.10 |
|
| ||||
| (n = 17) | (n = 100) | (n = 26) | (N = 143) | |
|
| ||||
| SES index | 58.4 ± 10.1 | 56.9 ± 10.2 | 54.8 ± 12.4 | 56.7 ± 10.6 |
|
| ||||
| (n = 14) | (n = 86) | (n = 21) | (N = 121) | |
|
| ||||
| IAAT (cm2) * | 48.5 ± 17.2 | 42.6 ± 20.4 | 41.6 ± 23.1 | 43.1 ± 2000 |
| SAAT (cm2) * | 317.8 ± 106.7 | 309.7 ± 118.4 | 283.0 ± 151.2 | 305.8 ± 124.1 |
Note. SES = socioeconomic status; IAAT = intra-abdominal adipose tissue; SAAT = subcutaneous abdominal adipose tissue.
Values are the geometric means and standard deviations.
Table 2.
Unadjusted Participant Characteristics for VO2max and Physical Activity by Acculturation Groups (Mean ± SD)
| Foreign born | 1st generation | 2nd/3rd generation | Total | |
|---|---|---|---|---|
| (n = 17) | (n = 101) | (n = 26) | (N = 144) | |
|
| ||||
| VO2max (L/min) | 2.24 ± 0.55 | 2.12 ± 0.51 | 2.30 ± 0.64 | 2.17 ± 0.54 |
| VO2max (ml·kg−1·min−1) | 33.14 ± 6.7 | 34.10 ± 6.0 | 36.64 ± 8.2 | 34.45 ± 6.60 |
|
| ||||
| (n = 20) | (n = 112) | (n = 28) | (N = 160) | |
|
| ||||
| Max heart rate (beats/min) | 199.3 ± 8.4 | 200.5 ± 8.0 | 202.8 ± 8.1 | 200.8 ± 8.10 |
| Max RER | 1.14 ± 0.80 | 1.11 ± 0.07 | 1.12 ± 0.08 | 1.12 ± 0.07 |
|
| ||||
| (n = 14) | (n = 81) | (n = 24) | (N = 119) | |
|
| ||||
| Total PA (hrs/wk) * | 6.6 ± 7.9 | 7.1 ± 8.5 | 6.4 ± 7.4 | 6.9 ± 8.1 |
|
| ||||
| (n = 15) | (n = 73) | (n = 21) | (N = 109) | |
|
| ||||
| MVPA outside PE (days/week) * | 3.4 ± 2.6 | 3.2 ± 2.1 | 3.1 ± 1.9 | 3.2 ± 2.1 |
|
| ||||
| (n = 16) | (n = 93) | (n = 21) | (N = 130) | |
|
| ||||
| Days of PE per wk* | 3.4 ± 2.3 | 3.0 ± 2.1 | 3.3 ± 2.2 | 3.1 ± 2.1 |
|
| ||||
| (n = 15) | (n = 90) | (n = 22) | (N = 127) | |
|
| ||||
| MVPA during PE (days/week) * | 3.2 ± 2.2 | 2.8 ± 1.9 | 3.5 ± 2.4 | 3.0 ± 2.0 |
|
| ||||
| (n = 17) | (n = 98) | (n = 26) | (N = 141) | |
|
| ||||
| PA in PE duration index* | 4.3 ± 1.9 | 3.9 ± 1.7 | 3.5 ± 2.1 | 3.9 ± 1.8 |
|
| ||||
| (n = 5) | (n = 32) | (n = 7) | (N = 44) | |
|
| ||||
| Number of sports in school per year* | 2.2 ± 2.0 | 1.8 ± 1.2 | 1.8 ± 1.4 | 1.9 ± 1.3 |
|
| ||||
| (n = 4) | (n = 29) | (n = 8) | (N = 41) | |
|
| ||||
| Number of sports outside school per year* | 1.7 ± 1.9 | 1.5 ± 1.1 | 1.5 ± 1.2 | 1.5 ± 1.1 |
Note PA = physical activity; MVPA = moderate-to-vigorous physical activity; RER = Respiratory exchange ratio; PE = physical education class.
Values are the geometric means and standard deviations.
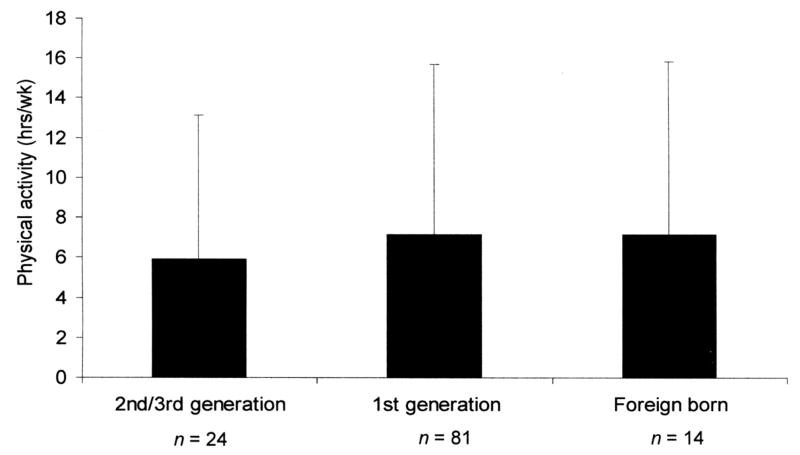
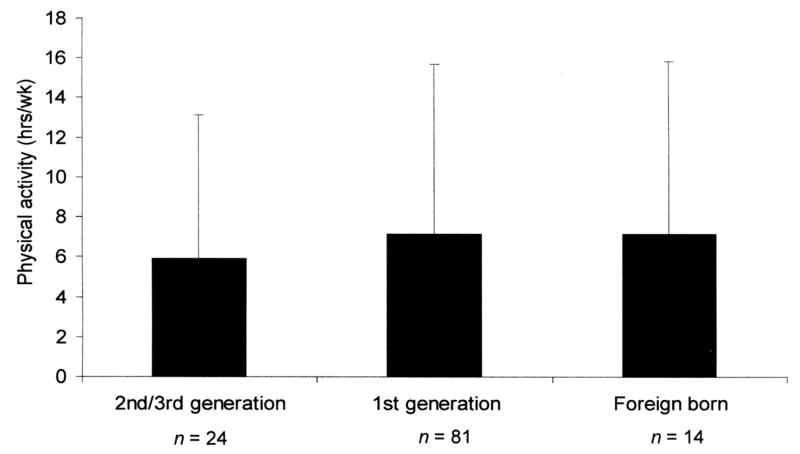
After adjusting for age, gender, total fat mass, total lean tissue mass, and SES, mean VO2max differed significantly among acculturation groups (F = 3.70, p = .027). More specifically, the 2nd/3rd-generation group had significantly higher VO2max compared with the 1st-generation group (p = .031), but not compared with the foreign-born group (p = 0.10) as shown in Figure 1. No other adjusted acculturation group differences were found with respect to anthropometric measures, body composition, total PA (see Figure 2), and type or duration of PA.
Figure 1.
Adjusted VO2max differences between acculturation groups (mean ± SD).
Note. Data adjusted for age, gender, total fat mass, total lean tissue mass, and socioeconomic status.
*Significantly different from 1st generation: p = .03.
Figure 2.
Adjusted total physical activity differences between acculturation groups.
Note. Data adjusted for age, gender, total fat mass, total lean tissue mass, and socioeconomic status; values are geometric means and standard deviations.
Secondary Analysis by Assimilation Status
Comparison of the proportion of assimilated participants among the three acculturation groups showed that assimilation was different across acculturation categories (p = .01). This was done to confirm the “generational assimilation” of categories. Specifically, 57.1% of participants classified as more assimilated were in the 2nd/3rd-generation group, whereas 73.7% and 84.6% of participants classified as less assimilated were in the 1st-generation or foreign-born groups, respectively.
There were no unadjusted group differences in age, Tanner stage, height, weight, BMI, % fat, total lean tissue mass, total fat mass, IAAT, SAAT, SES, VO2max, total PA, and type or duration of PA among the more assimilated and less assimilated groups (data not shown). After adjusting for age, gender, total fat mass, total lean tissue mass, and SES, however, the more assimilated group had significantly higher VO2max (2.25 ± 0.20 L/min) compared with the less assimilated group (2.16 ± 0.20 L/min; F = 4.25, p = .04), whereas no other differences were noted in any PA variable (data not shown).
Discussion
The purpose of this study was to determine whether VO2max and PA were associated with degree of acculturation in overweight Hispanic children. The main findings of this study were that VO2max was higher in the more acculturated groups, whereas PA was not different. Comparisons among acculturation groups revealed that there were no differences in any anthropometric measures or body composition. These results confer the homogeneity of our sample as a result of the inclusion criteria of the study.
VO2max
To our knowledge, there are few studies that have specifically investigated the associations between acculturation and VO2max. Rode & Shephard (23) reported that fitness appeared to deteriorate as individuals acculturated, and Weitz (30) reported that those least acculturated showed the highest fitness levels, reflecting strenuous work patterns. Although the findings of this study for VO2max differ from these previous studies and our hypothesized outcome, we can offer some possible explanations. First, the previous studies might not accurately reflect Hispanic pediatric populations. Second, VO2max and PA might not be as strongly related in children (6) as in adults (19), which might explain in part why acculturation was associated with VO2max and not with PA, suggesting that these findings are independent of each other. In fact, we also found that VO2max was not related to total hours of PA (r = .05, p = .59). More importantly, however, it is well established that children who engage in vigorous physical activity can achieve substantial improvements in VO2max (20,24). Therefore, although total PA did not differ among the groups, it is possible that physical activity intensity did. Furthermore, cultural differences in competitiveness, described by Kaga and Romero (13), might support the notion that more acculturated children practice a greater amount of vigorous PA. Lastly, the more acculturated children might be more affluent and comfortable in the dominant culture and might therefore experience fewer barriers to accessing fitness facilities, safe recreation areas, and better quality of health care (3). In fact, the more acculturated group tended to have a more favorable SES, which strengthens this postulation. Our PA instrument, however, was not able to assess differences in PA intensity or location, limiting our ability to confirm these explanations.
We are confident the observed fitness differences were not the result of misclassification or bias. Our outcomes were similar for both acculturation classification methods used, and the “assimilation by generation” analysis showed that both methods captured most of the same children in the groups expected. Our lab technicians were fluent in English and Spanish, and fitness-test procedures were conveyed to the children consistently in the preferred language. Any errors associated with understanding the fitness testing protocol were likely random. Moreover, although the VO2max test is effort dependent, we have no reason to believe that children giving more or less effort explain fitness differences. The same level of explanation and encouragement was provided to all children, and the physiological markers of effort (HRmax and RERmax) did not differ among groups. Last of all, analysis of data from participants excluded for not meeting the VO2max criteria (n = 64) demonstrated identical outcomes for VO2peak with those reported. Therefore, those children who were excluded did not seem to bias our results.
When expressed in absolute terms, these participants rated very good to excellent for VO2max according to U.S. population age- and gender-matched norms (24). When divided by body weight (expressed as ml·kg−1·min−1), however, this sample fell between the very poor and poor category (mean 34.3 ± 6.5 ml·kg−1·min−1). Moreover, although the relative fitness differences between the groups were small, they have implications for health in these children. Previous findings from our work in this population have shown that lower VO2max predicts greater fat accumulation (12), which might increase health risks over time. In addition, adult studies have confirmed that VO2max positively affects health and is a reflection of PA patterns (16). Most important, Church et al. (4) has shown a gradation of VO2max among obese individuals associated with reduced risk of death. When our data were expressed in similar units (METs), we found that our differences corresponded with different fitness quartiles described by Church et al. (4). Given this evidence, positive associations between acculturation and fitness could result in the more acculturated individuals having better overall health status than those less acculturated as a result of higher fitness levels.
Physical Activity
The PA findings did not support our hypothesis that PA would be lower in the more acculturated groups. These findings might be explained by several factors. Much of the evidence for the relationship between acculturation and health status in adults has focused on diseases such as diabetes (7), obesity (25), and cardiovascular disease (26). Only a few studies have investigated the association of acculturation with PA (8), and these studies have yielded inconclusive results. Our PA instrument might have missed the types of culturally specific PAs that the least acculturated children would engage in, such as their leisure time and home PA. Another explanation could be the inherently limited ability of children for recollection concerning moderate-to- vigorous PA. Although these questionnaires included questions concerning the intensity of PA (i.e., breathing heavy etc.), we might have needed a more appropriate instrument to measure these aspects of PA. Also, as a result of equivocal evidence on the relationship between VO2max and PA in children (1,6), total hours of PA per week or other specific measures of PA might not differ by acculturation status in the same manner as VO2max. Finally, total PA data as measured by questionnaire vary to a great extent by nature and are less precise compared with other more objective measures (i.e., pedometers or accelerometers). Because PA is often over- or underestimated, resulting in a wide range of values, it is possible that the sample size was too small and lacked statistical power to detect significant differences. We attempted to maximize the accuracy of PA data by administering the questionnaires in the language that the child preferred, which supports that these results are not the result of bias, but rather to random misclassification.
Conclusions
This study found that the more acculturated children had higher VO2max levels compared with less acculturated children in a sample of overweight Hispanic children; demographic, anthropometrics, body composition, and PA did not differ. It has yet to be determined whether these positive relationships would remain through adulthood and whether health outcomes such as diabetes and/or cardiovascular disease will be related to these fitness differences over time. Longitudinal analyses are needed to determine whether these fitness differences confer protective health effects in this at-risk population. In such a case, health professionals might need to develop interventions that focus on culturally appropriate PA behavior modifications that target the needs of these high-risk populations.
Acknowledgments
This study was supported by NIH Grant R01 DK 59211 and by GCRC National Center for Research Resources Grant M01 RR 00043. Crespo was supported by the National Institute of Diabetes and Digestive and Kidney Disease Grant 5R01 DK059211-01. Ball and Cruz were supported by the American Diabetes Association Mentor-Based Postdoctoral Fellowship Grant. We thank Quintilia Avila (project coordinator) and all of the children, families, and support staff at the USC-GCRC for making this study possible.
Contributor Information
Noé C. Crespo, Department of Preventive Medicine, University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
Geoff D.C. Ball, Department of Preventive Medicine, University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
Gabriel Q. Shaibi, Department of Biokinesiology and Physical Therapy, University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
Martha L. Cruz, Department of Preventive Medicine, University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
Marc J. Weigensberg, Department of Pediatrics, and University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
Michael I. Goran, Department of Physiology and Biophysics at the University of Southern California, Health Science Campus, Los Angeles, CA, 1540 Alcazar Street, Room 208, Los Angeles, CA, 90033
References
- 1.Atomi Y, Iwaoka K, Hatta H, Miyashita M, Yamamoto Y. Daily physical activity levels in preadolescent boys related to VO2max and lactate threshold. Eur J Appl Physiol. 1986;55:156–161. doi: 10.1007/BF00714998. [DOI] [PubMed] [Google Scholar]
- 2.Berry JW. Acculturation as varieties of adaptation. In: Padilla A, editor. Acculturation: Theory, Models and New Findings. Boulder, CO: Westview; 1980. pp. 9–25. [Google Scholar]
- 3.Cantero PJ, Richardson JL, Baezconde-Garbanati L, Marks G. The association between acculturation and health practices among middle-aged and elderly Latinas. Ethn Dis. 1999;9:166–180. [PubMed] [Google Scholar]
- 4.Church TS, Cheng YJ, Earnest CP, Barlow CE, Gibbons LW, Priest EL, Blair SN. Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care. 2004;27:83–88. doi: 10.2337/diacare.27.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Dixon LB, Sundquist J, Winkleby M. Differences in energy, nutrient, and food intakes in a US sample of Mexican-American women and men: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2000;152:548–557. doi: 10.1093/aje/152.6.548. [DOI] [PubMed] [Google Scholar]
- 6.Fenster JR, Freedson PS, Washburn RA, Ellison RC. The relationship between peak oxygen uptake and physical activity in 6- to 8-year-old children. Pediatr Exerc Sci. 1989;1:127–136. doi: 10.1123/pes.1.2.127. [DOI] [PubMed] [Google Scholar]
- 7.Franco LJ. Diabetes in Japanese-Brazilians—influence of the acculturation process. Diabetes Res Clin Pract. 1996;34(Suppl):S51–57. [PubMed] [Google Scholar]
- 8.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the U.S.: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 9.Gowen LK, Hayward C, Killen JD, Robinson TN, Taylor CB. Acculturation and eating disorder symptoms in adolescent girls. J Res Adolesc. 1999;9:67–83. [Google Scholar]
- 10.Hayes-Bautista DE, Hsu P, Perez A, Kahramanian MI. The Latino Majority Has Emerged: Latinos Comprise More Than 50% of all Births in California. Los Angeles: Center for the Study of Latino Health and Culture: Division of General Internal Medicine and Health Services Research, UCLA; 2003. pp. 1–3. [Google Scholar]
- 11.Hollingshead AB. Four Factor Index of Social Status. New Haven (Connecticut): Department of Sociology, Yale University; 1975. [Google Scholar]
- 12.Johnson MS, Figueroa-Colon R, Herd SL, Fields DA, Sun M, Hunter GR, Goran MI. Aerobic fitness, not energy expenditure, influences subsequent increase in adiposity in black and white children. Pediatrics. 2000;106:E50. doi: 10.1542/peds.106.4.e50. [DOI] [PubMed] [Google Scholar]
- 13.Kagan S, Romero C. Non-adaptive assertiveness of Anglo-American and Mexican American children of two ages. Rev Interamer Psychol. 1977;11:27–32. [Google Scholar]
- 14.Kelley DE, Goodpaster BH. Effects of physical activity on insulin action and glucose tolerance in obesity. Med Sci Sports Exerc. 1999;31:S619–623. doi: 10.1097/00005768-199911001-00021. [DOI] [PubMed] [Google Scholar]
- 15.Kriska AM, Knowler WC, LaPorte RE. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13:401–411. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 16.Lynch J, Helmrich SP, Lakka TA, Kaplan GA, Cohen RD, Salonen R, Salonen JT. Moderately intense physical activity and high levels of cardiorespiratory fitness reduce the risk of non-insulin-dependent diabetes mellitus in middle-aged men. Arch Intern Med. 1996;156:1307–1314. [PubMed] [Google Scholar]
- 17.Marshall W, Tanner J. Variations in the pattern of pubertal change in boys. Arch Dis Child. 1970;45:13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshall W, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAuley KA, Williams SM, Mann JI, et al. Intensive lifestyle changes are necessary to improve insulin sensitivity: A randomized controlled trial. Diabetes Care. 2002;25:445–452. doi: 10.2337/diacare.25.3.445. [DOI] [PubMed] [Google Scholar]
- 20.Pate RR, Ward DS. Endurance exercise trainability in children and youth. In: Grana WA, Lombardo JA, Sharkey BJ, Stone JA, editors. Advances in Sports Medicine and Fitness. Chicago: Year Book Medical; 1990. pp. 37–55. [Google Scholar]
- 21.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. J Nutr. 1998;128:701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 22.Portes A, Rumbaut RG. Legacies: The Story of the Immigrant Second Generation. Berkeley: University of California Press; 2001. [Google Scholar]
- 23.Rode A, Shephard RJ. Physiological consequences of acculturation: a 20-year study of fitness in an Inuit community. Eur J Appl Physiol Occup Physiol. 1994;69:516–524. doi: 10.1007/BF00239869. [DOI] [PubMed] [Google Scholar]
- 24.Shvartz E, Reibold RC. Aerobic fitness norms for males and females aged 6–75: a review. Aviat Space Env Med. 1990;61:3–11. [PubMed] [Google Scholar]
- 25.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29:470–477. [PubMed] [Google Scholar]
- 26.Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988–1994. Am J Public Health. 1999;89:723–730. doi: 10.2105/ajph.89.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trowbridge CA, Gower BA, Nagy TR, Hunter GR, Treuth MS, Goran MI. Maximal aerobic capacity in African-American and Caucasian prepubertal children. Am J Physiol. 1997;273:E809–814. doi: 10.1152/ajpendo.1997.273.4.E809. [DOI] [PubMed] [Google Scholar]
- 28.Unger JB, Gallaher P, Shakib S, Ritt-Olson A, Palmer PH, Johnson CA. The AHIMSA acculturation scale: A new measure of acculturation for adolescents in a multicultural society. J Early Adolesc. 2002;22:225–251. [Google Scholar]
- 29.Unger JB, Palmer PH, Dent CW, Rohrbach LA, Johnson CA. Ethnic differences in adolescent smoking prevalence in California: Are multi-ethnic youth at higher risk? Tob Control. 2000;9:ii9–ii14. doi: 10.1136/tc.9.suppl_2.ii9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weitz CA. Effects of acculturation and age on the exercise capacities of Solomon Islanders. Am J Phys Anthropol. 1990;81:513–525. doi: 10.1002/ajpa.1330810407. [DOI] [PubMed] [Google Scholar]
- 31.West SK, Munoz B, Klein R, Broman AT, Sanchez R, Rodriguez J, Snyder R. Risk factors for Type II diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Am J Ophthalmol. 2002;134:390–398. doi: 10.1016/s0002-9394(02)01595-7. [DOI] [PubMed] [Google Scholar]
- 32.Winkleby MA, Albright CL, Howard-Pitney B, Lin J, Fortmann SP. Hispanic/white differences in dietary fat intake among low educated adults and children. Prev Med. 1994;23:465–473. doi: 10.1006/pmed.1994.1064. [DOI] [PubMed] [Google Scholar]