Abstract
Objective
Examine the association between multiple psychological factors (depressive symptoms, trait anxiety, perceived stress) and subclinical atherosclerosis in older age.
Method
This cross-sectional study included 1,101 adults ages 65-84 from the Chicago Healthy Aging Study (CHAS—2007-2010). Previously validated self-report instruments were used to assess psychological factors. Noninvasive methods were used to assess subclinical atherosclerosis in two regions of the body, i.e., ankle-brachial blood pressure index (ABI) and coronary artery calcification (CAC). Multivariate logistic regression was used to examine the association between each psychological measure and subclinical atherosclerosis, after adjustment for socio-demographic factors, sleep quality, young adulthood/early middle age and late life CVD risk status, and psychological ill-being as appropriate.
Results
The burden of major cardiovascular disease risk factors did not significantly differ across tertiles of psychological factors. In multivariate adjusted models, trait anxiety was associated with calcification: those in the second tertile were significantly more likely to have CAC>0 compared to those in the lowest anxiety tertile [OR=1.68; 95%CI=1.09-2.58], but no significant difference was observed for Tertile III of trait anxiety [OR=1.31; 95%CI=0.75-2.27]. No association was seen between psychological measures and ABI.
Conclusion
Of several psychological factors, only trait anxiety was significantly associated with CAC.
Keywords: ankle brachial index, cardiovascular risk, coronary artery calcification, older adults, population study, psychological factors, subclinical atherosclerosis
INTRODUCTION
Depression, anxiety, and stress, have been linked to onset of cardiovascular disease (CVD) in adults without a previous history of cardiac conditions, and to increased risk of CVD morbidity and mortality among patients with diagnosed CVD (Everson et al., 1997; Iso et al., 2002; Kawachi et al., 1994; Richardson et al., 2012; Roest et al., 2010; Rugulies, 2002; Van der Kooy et al., 2007; Williams et al., 2000). These findings are independent of major CVD risk factors (e.g., hypercholesterolemia, hypertension, diabetes). Mechanisms whereby psychological factors may influence CVD-related outcomes remain uncertain, although biologic and behavioral models have been proposed, including adverse impact on engagement in healthy behaviors and stimulation of physiological dysregulation (Carney et al., 2002; Lett et al., 2004).
Previous studies examining the association between psychological factors and subclinical atherosclerosis, a marker for early asymptomatic disease, have reported inconsistent findings. Several have reported a positive association between subclinical atherosclerosis and the psychological attributes of depression (Agatisa et al., 2005; Janssen et al., 2011; Lewis et al., 2009; Tiemeier et al., 2004), anxiety (Paterniti et al., 2001; Seldenrijk et al., 2010), and stress (Troxel et al., 2003), while others document null findings (Low et al., 2011; Low et al., 2009; Matthews et al., 1998; O’Malley et al., 2000a; Ohira et al., 2012; Roux et al., 2006; Rozanski et al., 2011; Seldenrijk et al., 2011; Stewart et al., 2007; Yu et al., 2010). Select evidence indicates up to a three-fold higher risk for atherosclerosis among those with psychological ill-being (e.g., major depression) (Agatisa et al., 2005; Paterniti et al., 2001). Few studies have involved older adult populations, and none have had the ability to adjust for the confounding effect of CVD risk profiles in young adulthood/early middle age (Faramawi et al., 2007; Tiemeier et al., 2004). The current study examined cross-sectional associations between multiple psychological attributes (depressive symptoms, trait anxiety, and perceived stress) and subclinical atherosclerosis measured in the coronary arteries and peripheral vascular beds, using data from the Chicago Healthy Aging Study (CHAS). It was hypothesized that older persons with higher depression, anxiety, and stress scores are more likely to have prevalent subclinical atherosclerosis independent of CVD risk factor levels in young adulthood/early middle age and late-life.
MATERIALS AND METHODS
Study population and data source
CHAS is a longitudinal cohort study to determine impact of early-middle age low CVD risk status, i.e., favorable levels of all major CVD risk factors, on objectively measured health-related older age outcomes (Pirzada et al., 2013). The CHAS cohort is a subsample selected from a pool of 39,522 participants from the Chicago Heart Association Detection Project in Industry (CHA) Study. CHA participants underwent clinical examination in 1967-73 (baseline) which included objective measurement of major CVD risk factors. Details of the CHA study have been published (Greenland et al., 2003; Stamler et al., 1975). In 2007-2010, the CHAS study conducted follow-up re-examinations of 1,395 original CHA participants ages 65-84 at follow-up (72% men; 421 low risk (LR), i.e., with favorable levels of all major CVD risk factors, and 974 not-LR) (Pirzada et al., 2013). The Institutional Review Board (IRB) at Northwestern University approved the CHAS study.
Current analyses involved 1,101 participants, after exclusion of those with missing data on any of the main variables of interest, i.e., subclinical atherosclerosis (CAC=252 and ABI=19), psychological variables (n=17), and major CVD risk factors (n=6). Exclusion of 294 observations resulted in a full dataset with no missing values across factors of interest.
Study measures
Subclinical Atherosclerosis
Subclinical atherosclerosis was quantified as coronary artery calcification (CAC) (Arad et al., 2000; Greenland et al., 2004; O’Malley et al., 2000b) and ankle-brachial blood pressure index (ABI) (Fowkes et al., 2008; Ouriel and Zarins, 1982) at the follow-up examination (2007-2010). Both these measures have been associated with major CVD risk factors, clinical CVD, and CVD-related mortality (Arad et al., 1996; Criqui et al., 2010; Detrano et al., 1997; Doobay and Anand, 2005; Enoch and Ijeoma, 2008; Fowkes et al., 2008; Hoff et al., 2003; Leng et al., 1996; McDermott et al., 2009; McDermott et al., 2005; Newman et al., 1999; Pletcher et al., 2004; Price et al., 2007; Regensteiner et al., 2008). CAC was measured using a multidetector row helical computer tomography (CT) scanner, and quantified using Agatston’s method (Bild et al., 2002; Friedman et al., 1988). At 1-2 minute intervals, two separate readings were obtained across four major arteries, i.e., left main, left circumflex, left anterior descending, and right coronary. CAC was calculated by summing Agatston scores within and across these four arteries. Agatston scores >0 indicated extant calcification. Participants reporting CT scans or radiation therapy within the last year and those weighing over 350 pounds were ineligible for CT scan.
To assess peripheral arterial obstruction, ABI was calculated using systolic blood pressure (BP) readings of the brachial, dorsalis pedis, and posterior tibial arteries. Two readings were taken at each location using a Doppler probe with participants in a supine position (McDermott et al., 2009). Right and left extremity ABI scores were computed using the highest systolic BP reading for each leg and the average of the four brachial readings. Presence of peripheral artery disease was defined as ABI scores ≤0.90, per clinical guidelines (Rooke et al., 2011).
Psychological Factors
Validated questionnaires were used to collect self-reported psychological measures including depressive symptoms, trait anxiety and perceived stress at follow-up (2007-2010). With adequate validity and test-retest reliability reported across multiple community samples, the 20-item Center for Epidemiologic Studies Depression Scale (CES-D) is an effective screening tool for depression (Radloff, 1977). The CES-D uses a 4-point Likert scale (0—Rarely to 3—Most or all of the time) to probe the extent to which an individual has been troubled by depressive symptoms within the last seven days; scores range from 0-60. The trait anxiety scale of the Spielberger State-Trait Anxiety Inventory (STAI) is a validated instrument used to assess an individual’s long-standing predisposition to react to demanding situations with increased anxiety levels (Spielberger et al., 1970). The Perceived Stress Scale (PSS) assesses perceived levels of stress over the previous month. Psychometric testing has evidenced adequate criterion validity, internal consistency (Cronbach’s alpha=0.88), and test-retest reliability (Cohen et al., 1983). For all psychological measures, higher scores represent lower psychological well-being, i.e., greater levels of depressive symptoms, anxiety, and perceived stress.
Covariates
Covariates included baseline information on CVD risk status in young adulthood/early middle age and follow-up data on socio-demographic characteristics (age, sex, race/ethnicity, and education), late-life CVD risk factors, and sleep quality. The protocol and examination methods for assessing CVD risk factors at baseline (1967-1973) in the CHA study have been described (Greenland et al., 2003; Stamler et al., 1975). Low risk (LR) in young adulthood/early middle age (i.e., ages 25-45) was defined as: (1) blood pressure ≤120/≤80 mmHg and no reported use of antihypertensive medication, (2) serum cholesterol <200 mg/dL and no reported use of lipid-lowering medication, (3) BMI <25.0 kg/m2, (4) no diabetes, and (5) no current smoking. Participants not meeting these criteria were categorized as not low risk.
At the follow-up examination, health interviewers recorded date of birth, sex, and race/ethnicity. Self-reported education status was collected via mailed personal history questionnaire; educational attainment was categorized into 3 groups (≤12, 13-15, and ≥16 years of education). Three systolic and diastolic BP readings were taken with participants in the seated position; the second and third readings were averaged here (Friedman et al., 1988). After a 12-hour fast, blood was drawn to assess total serum cholesterol level. Measurements of height (in meters) and weight (in kilograms) were used to calculate body mass index (BMI). Presence of diabetes was defined as self-reported previous history, or treatment with antihyperglycemic medication. Dichotomized smoking status was determined from self-report. Late-life sleep quality was assessed using a single self-reported item from the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989); participants were asked to rate their overall sleep quality using a 4-point Likert response scale ranging from ‘very good’ to ‘very bad.’
Statistical analyses
Continuous scores for each psychological measure—depressive symptoms, trait anxiety, and perceived stress—were used to create tertiles across the full range of observations for each of these variables. Descriptive characteristics for the total sample are provided by tertiles of each psychological variable. Group differences in participant characteristics across tertile scores were examined using F-tests or χ2-tests as appropriate. Age-, sex-, and race-adjusted prevalence of CAC>0 and ABI ≤0.9 were computed across tertiles of each psychological factor and p-values for pair-wise comparisons were obtained from logistic regression models with the lowest tertile (indicative of best psychological health) serving as the reference group.
The association between each psychological measure and subclinical atherosclerosis was examined using multivariate logistic regression. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated for the prevalence of subclinical atherosclerosis, i.e., CAC>0 and ABI≥0.90 across tertiles of each psychological trait. The lowest tertile of each psychological measure served as the reference category. Four separate models were constructed. Model 1 was unadjusted. Model 2 was adjusted for age, gender, race/ethnicity, education, sleep quality, BP, use of antihypertensive medication, serum cholesterol, use of lipid-lowering medication, BMI, diabetes mellitus, and smoking status, all measured in later life. Model 3 was adjusted for all variables in model 2, with addition of CVD risk status as measured in 1967-1973 when participants were ages 22-44 years. Finally, Model 4 additionally adjusted for other psychological factors as appropriate, e.g., adjustment for trait anxiety and perceived stress when modeling the influence of depressive symptoms. In sensitivity analyses, multivariate-adjusted odds of atherosclerosis were re-examined with exclusion of participants with a self-reported history of cardiovascular disease, i.e., heart attack, angina, congestive heart failure, heart disease, stroke, and arteriosclerosis, at follow-up.
Data analyses conducted using statistical software (SAS 9.1 for Windows; SAS, Inc, Cary, North Carolina).
RESULTS
Characteristics of the study sample by tertile of each psychological attribute
Table 1 provides participant characteristics by tertile of each psychological factor. In general, sex, race/ethnicity, and sleep quality differed across tertiles of psychological variables. Women (depressive symptoms, P=0.03; and perceived stress, P=0.003) and African Americans (depressive symptoms, P=0.02; trait anxiety, P=0.02; and perceived stress, P=0.002) were more likely to be in the highest tertiles (i.e., greater burden of psychological symptoms). Correspondingly, sleep quality tended to be lowest for participants in the highest tertile of depressive symptoms (P<0.001), trait anxiety (P<0.001), and perceived stress (P<0.001). Differences by educational status were observed only for depressive symptoms; a higher proportion of participants with the highest educational attainment were in the lowest CES-D tertile (P=0.02). The burden of major CVD risk factors in late-life did not significantly differ across tertiles of psychological traits.
Table 1. Characteristics of Study Sample by Tertile of Psychological Variable: Chicago Healthy Aging Study (CHAS—2007-2010).
| N=1,101 | Depressive Symptoms
|
p ‡ | Trait Anxiety
|
p‡ | Perceived Stress
|
p‡ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lowest I (n=348) |
II (n=347) |
Highest III (n=406) |
Lowest I (n=299) |
II (n=437) |
Highest III (n=365) |
Lowest I (n=296) |
II (n=430) |
Highest III (n=375) |
||||
| Age, M (SD) | 70.7 (4.6) | 71.2 (4.5) | 71.4(4.7) | 0.12 | 71.1 (4.8) | 71.3 (4.5) | 70.9 (4.6) | 0.49 | 71.0 (4.6) | 71.6(4.69) | 70.7(4.50) | 0.02 |
| Gender, % | ||||||||||||
| Men | 74.7 | 72.9 | 66.3 | 0.02 | 75.3 | 71.5 | 67.1 | 0.07 | 75.3 | 73.8 | 64.5 | <0.01 |
| Women | 25.3 | 27.1 | 33.7 | 0.02 | 24.8 | 28.5 | 32.9 | 0.07 | 24.7 | 26.2 | 35.5 | <0.01 |
| Race/ethnicity, % | ||||||||||||
| White | 90.8 | 89.6 | 85.2 | 0.04 | 92.3 | 89.0 | 84.4 | <0.01 | 91.2 | 90.5 | 83.7 | <0.01 |
| African American | 6.6 | 8.4 | 12.3 | 0.02 | 6.0 | 8.9 | 12.3 | 0.02 | 6.4 | 7.4 | 13.6 | <0.01 |
| Education Level, % | ||||||||||||
| ≤ 12 years | 11.8 | 10.7 | 14.8 | 0.01 | 12.0 | 11.4 | 14.3 | 0.34 | 13.2 | 9.7 | 15.2 | 0.12 |
| 13-15 years | 23.3 | 29.1 | 32.0 | 24.8 | 29.9 | 29.3 | 26.4 | 28.3 | 29.9 | |||
| ≥ 16 years | 64.9 | 60.2 | 53.2 | 63.2 | 58.7 | 56.4 | 60.5 | 62.0 | 54.9 | |||
| Sleep Quality | ||||||||||||
| Very/Fairly good | 96.3 | 86.7 | 74.6 | <0.01 | 94.3 | 87.7 | 75.1 | <0.01 | 91.2 | 87.9 | 77.6 | <0.01 |
| Fairly/Very bad | 3.7 | 13.3 | 25.4 | 5.7 | 12.3 | 24.9 | 8.8 | 12.1 | 22.4 | |||
| Body mass index, kg/m2, M (SD) | 28.2 (4.7) | 28.3 (4.5) | 28.6 (5.3) | 0.51 | 28.6 (4.7) | 28.2 (4.6) | 28.3 (5.3) | 0.62 | 28.5 (4.8) | 28.3 (4.4) | 28.4 (5.4) | 0.90 |
| Blood Pressure, M (SD) | ||||||||||||
| Systolic | 127.2 (16.5) | 125.7 (14.7) | 126.4 (16.5) | 0.50 | 126.6 (16.5) | 127.4 (15.4) | 125.2 (16.1) | 0.14 | 127.0 (15.4) | 126.5 (16.1) | 125.9 (16.2) | 0.65 |
| Diastolic | 72.3 (9.9) | 71.5 (8.9) | 71.4 (9.9) | 0.40 | 71.9 (10.3) | 72.1 (9.1) | 71.0 (9.6) | 0.23 | 72.0 (9.9) | 71.8 (9.5) | 71.3 (9.5) | 0.66 |
| Hypertension,a % | 63.8 | 59.4 | 62.8 | 0.45 | 61.9 | 63.6 | 60.3 | 0.62 | 63.9 | 61.6 | 61.1 | 0.74 |
| Serum cholesterol, mg/dL,M (SD) | 185.2 (34.9) | 186.5 (39.1) | 186.9 (37.7) | 0.81 | 183.8 (37.0) | 186.6 (38.1) | 187.9 (36.5) | 0.36 | 185.2 (38.7) | 185.0 (37.5) | 188.4 (35.8) | 0.37 |
| Dyslipidemia,b % | 57.5 | 56.5 | 60.6 | 0.49 | 56.5 | 57.4 | 60.8 | 0.48 | 57.1 | 60.9 | 56.3 | 0.36 |
| Diabetes mellitus,c % | 10.9 | 10.4 | 12.3 | 0.68 | 10.4 | 11.0 | 12.3 | 0.71 | 11.5 | 11.6 | 10.7 | 0.90 |
| Current smoking, % | 1.4 | 3.5 | 3.0 | 0.22 | 2.7 | 2.5 | 2.7 | 0.98 | 2.7 | 3.0 | 2.1 | 0.73 |
The ranges corresponding to these tertiles are: depression, 0 to 1, 2 to 5, and 6 to 46, trait anxiety, 19 to 24, 24 to 31, and 32 to 70, and perceived stress, 0 to 4, 5 to 10, and 11 to 33, respectively.
Systolic blood pressure of 140 mm Hg or higher, diastolic blood pressure of 90 mm Hg or higher, and/or use of antihypertensive medication.
Dyslipidemia was defined as total cholesterol ≥240 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, low-density lipoprotein cholesterol ≥ 160 mg/dL, or receiving treatment.
Self-reported history of diabetes or use of antihyperglycemic medication.
P-value for differences across tertiles; χ2 or F test as appropriate.
Bivariate analysis revealed no statistically significant difference on measures of psychological ill-being (depressive symptoms, p=0.11; anxiety, p=0.08; stress, p=0.22) when comparing those excluded and included from final analyses, i.e., 294 vs. 1,101. However, older adults excluded from analysis displayed more favorable CVD risk profiles when considering hypertension (79.9% vs. 62.0%, p<0.001), dyslipidemia (81.0% vs. 58.3%, p<0.001), and diabetes mellitus (23.5% vs. 11.3%, p<0.001); the opposite was true for diastolic blood pressure (69.3 vs. 71.7, p<0.001) and serum cholesterol (165.5 vs. 186.2, p<0.001), with more favorable profiles evident for those included in the final analysis.
Association of psychological attributes with subclinical atherosclerosis
Prevalence of subclinical atherosclerosis, adjusted for age, sex, and race/ethnicity, is presented in Figures 1 and 2. In adjusted pair-wise comparisons, prevalence of atherosclerosis, i.e., CAC >0 or ABI ≤0.9, did not vary significantly across strata of psychological factors.
Figure 1. Prevalence of CAC > 0 in Later Life: Chicago Healthy Aging Study (CHAS—2007-2010).
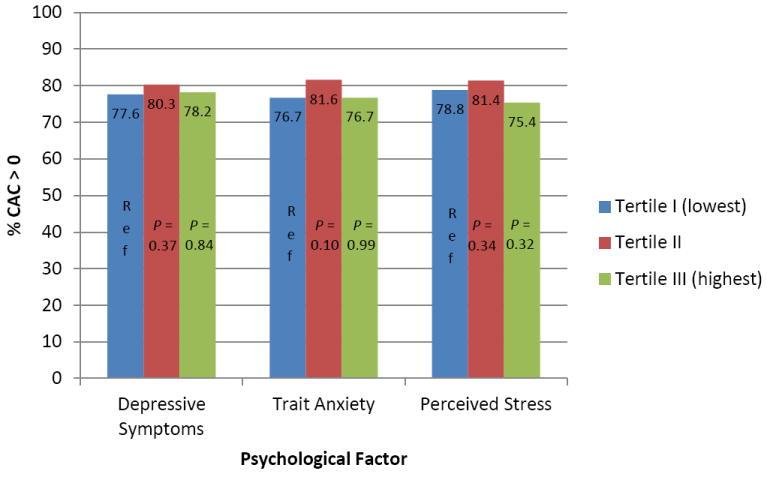
Age-, sex-, race/ethnicity-adjusted prevalence of CAC>0 in later life by tertile categories of the psychological factors. P-values were estimated for pair-wise comparisons within tertile categories with the lowest symptomatology tertile serving as the reference group; P-values are non-significant (p ≥ 0.05).
Figure 2. Prevalence of ABI ≤ 0.9 in Later Life: Chicago Healthy Aging Study (CHAS—2007-2010).
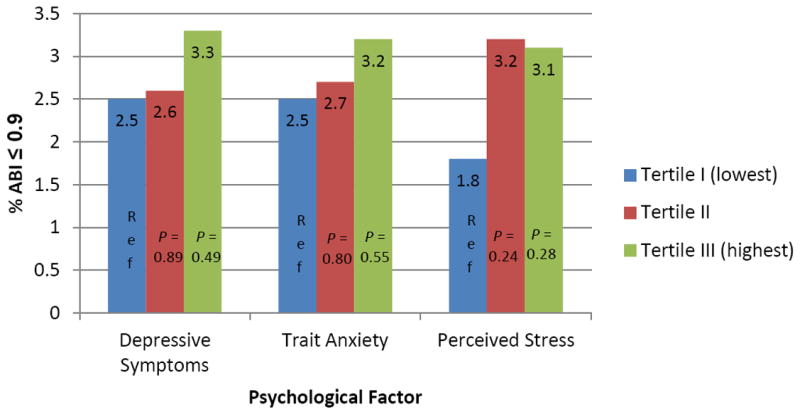
Age-, sex-, race/ethnicity-adjusted prevalence of ABI ≤ 0.9 in later life by tertile categories of the psychological factors. P-values were estimated for pair-wise comparisons within tertile categories with the lowest symptomatology tertile serving as the reference group; P-values are non-significant (p ≥ 0.05).
Table 2 shows odds ratios for having CAC>0 according to tertiles of each psychological factor. In the unadjusted Model 1, only perceived stress was inversely associated with calcification. Compared to those in the lowest tertile for perceived stress, those in the highest tertile had 33% lower odds of having CAC>0 [OR = 0.67; 95% CI=0.46-0.96]. Late-life cardiovascular risk factor levels explained much of this association which was attenuated to nonsignificance in models 2-4. In contrast, no significant association was observed between trait anxiety and CAC in unadjusted models. However, after adjustment for late-life socio-demographic factors, CVD risk status profiles in young adulthood, CVD risk factors in old age, and other psychological ill-being, i.e., depressive symptoms and perceived stress in older age (model 4), those in the second tertile had 68% higher odds of having CAC>0 compared to those in the lowest anxiety tertile [OR = 1.68; 95% CI=1.09-2.58]. There was a non-significant trend toward increased odds in the third tertile of trait anxiety [OR = 1.31; 95% CI=0.75-2.27]. There was no significant association between ABI and depressive symptoms, anxiety, or stress (Table 3). Analyses were not stratified by gender or socio-economic status as interactions with measures of psychological ill-being (i.e., effect modification), when considering atherosclerosis, were not evident.
Table 2. Association (Odds Ratios) Between Psychological Measures and Coronary Artery Calcification: Chicago Healthy Aging Study (CHAS—2007-2010).
| Psychological Measure | CAC > 0 (n=866)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1* | Model 2** | Model 3† | Model 4‡ | |||||
|
| ||||||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Depressive Symptoms | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.17 | (0.81-1.69) | 1.27 | (0.84-1.91) | 1.35 | (0.89-2.05) | 1.42 | (0.93-2.18) |
| Tertile III (highest) | 0.91 | (0.65-1.29) | 1.06 | (0.71-1.58) | 1.13 | (0.75-1.70) | 1.35 | (0.81-2.26) |
| Trait Anxiety | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.26 | (0.87-1.82) | 1.50 | (1.00-2.25) | 1.57 | (1.04-2.38) | 1.68 | (1.09-2.58) |
| Tertile III (highest) | 0.84 | (0.58-1.20) | 1.08 | (0.71-1.65) | 1.13 | (0.73-1.73) | 1.31 | (0.75-2.27) |
| Perceived Stress | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.20 | (0.82-1.75) | 1.27 | (0.84-1.92) | 1.26 | (0.82-1.92) | 1.28 | (0.83-1.97) |
| Tertile III (highest) | 0.67 | (0.46-0.96) | 0.88 | (0.58-1.33) | 0.94 | (0.62-1.43) | 0.98 | (0.58-1.63) |
Model 1 is unadjusted.
Model 2 is adjusted for age, gender, race/ethnicity, education, sleep quality, blood pressure, use of antihypertensive medication, serum cholesterol, use of lipid-lowering medication, body mass index, diabetes mellitus, and smoking status.
Model 3 adds baseline risk status, i.e., as measured in 1967-1973.
Model 4 is adjusted for all variables in model 3 and psychological measures
Table 3. Association (Odds Ratio) Between Psychological Measures and Ankle-brachial Index: Chicago Healthy Aging Study (CHAS—2007-2010).
| Psychological Measure | ABI ≤ 0.9 (n=31) | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1* | Model 2** | Model 3† | Model 4‡ | |||||
|
| ||||||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Depressive Symptoms | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.13 | (0.43-2.97) | 1.09 | (0.39-3.05) | 1.12 | (0.40-3.19) | 0.92 | (0.32-2.66) |
| Tertile III (highest) | 1.52 | (0.63-3.66) | 1.13 | (0.43-3.02) | 1.24 | (0.46-3.31) | 0.68 | (0.20-2.28) |
| Trait Anxiety | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.18 | (0.46-3.03) | 1.03 | (0.38-2.82) | 1.14 | (0.41-3.15) | 0.82 | (0.29-2.34) |
| Tertile III (highest) | 1.42 | (0.55-3.65) | 1.09 | (0.38-3.12) | 1.19 | (0.41-3.46) | 0.41 | (0.11-1.60) |
| Perceived Stress | ||||||||
| Tertile I (lowest) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Tertile II | 1.96 | (0.70-5.50) | 1.99 | (0.67-5.91) | 2.19 | (0.72-6.62) | 2.08 | (0.66-6.51) |
| Tertile III (highest) | 1.92 | (0.67-5.52) | 1.75 | (0.56-5.49) | 2.05 | (0.64-6.56) | 1.53 | (0.37-6.32) |
Model 1 is unadjusted.
Model 2 is adjusted for age, gender, race/ethnicity, education, sleep quality, blood pressure, use of antihypertensive medication, serum cholesterol, use of lipid-lowering medication, body mass index, diabetes mellitus, and smoking status.
Model 3 adds baseline risk status, i.e., as measured in 1967-1973.
Model 4 is adjusted for all variables in model 3 and psychological measures.
DISCUSSION
There were no significant consistent cross-sectional associations between psychological factors and the atherosclerotic measures of CAC or ABI. Only trait anxiety was positively associated with subclinical atherosclerosis as measured by CAC. Compared to those in the lowest tertile of trait anxiety, those in the mid-tertile (i.e., Tertile II) had higher odds of having any CAC (CAC >0). This association remained significant with adjustment for baseline CVD risk status, follow-up socio-demographic characteristics (i.e., age, sex race/ethnicity, and education), late-life CVD risk factors, depressive symptoms, and perceived stress. However, while there was a trend, the odds for presence of any CAC were not significantly elevated for participants in Tertile III of trait anxiety. None of the psychological factors were associated with ABI.
The few studies examining associations between negative affect, i.e., depressive symptoms or disorders and subclinical atherosclerosis among community-dwelling older adults have yielded inconsistent findings (Chen et al., 2006; Faramawi et al., 2007; Ohira et al., 2012; Roux et al., 2006; Stewart et al., 2007; Tiemeier et al., 2004). Longitudinal studies indicate an association between presence of depressive symptoms, as measured using self-reported screening tools, and development or progression of abnormal values of common carotid artery intima-media thickness (CCA-IMT) (Faramawi et al., 2007; Stewart et al., 2007). In contrast, cross-sectional studies have not demonstrated an association between depressive symptoms and atherosclerosis (Ohira et al., 2012; Roux et al., 2006; Tiemeier et al., 2004). The current study extends these cross-sectional findings to a population of older adults using the atherosclerotic measures of CAC and ABI. In contrast to studies of depressive symptoms, cross-sectional studies of clinically-diagnosed major depression have generally found an association with atherosclerosis (Chen et al., 2006; Tiemeier et al., 2004). Inconsistent associations between negative affect and atherosclerosis may be a consequence of differences in study design (e.g., longitudinal vs. cross-sectional) and assessment methods for depression (i.e., clinically diagnosed depressive disorder vs. self-reported symptomatology). It is plausible that longitudinal studies and those considering clinically diagnosed depression are capturing effects of long-term exposure to and severity of negative affect, respectively, which are less likely to be captured in cross-sectional studies or those examining depressive symptoms. Studies are needed to more accurately quantify effects of negative affect, and to assess whether a mechanistic threshold is plausible based on severity and length of exposure to depressive symptoms.
Both cross-sectional and longitudinal studies have yielded inconsistent findings on the association of trait anxiety with subclinical atherosclerosis among older adults (Narita et al., 2008; Ohira et al., 2012; Paterniti et al., 2001; Roux et al., 2006; Yu et al., 2010). Most studies have found no association between single measures of trait anxiety and either presence or development of subclinical atherosclerosis. A study examining anxiety levels over multiple points in time reported that consistently elevated symptoms of anxiety over a 2-year period were associated with greater progression of CCA-IMT (Paterniti et al., 2001). In the current study, higher odds of CAC >0 were found among participants in the second tertile of trait anxiety, with no such findings for those in the highest tertile (i.e., Tertile III). While the reason for this finding remains unclear, it is possible that persons with highest anxiety levels experience positive cardiovascular health because they seek medical attention even for minor health problems as a consequence of anxiety-causing hyper vigilance.
To our knowledge, only two studies have examined the association of stress—examining perceived stress in the past month and chronic burden of stress, respectively—and atherosclerosis in older adults; both have resulted in non-significant findings (Roux et al., 2006; Yu et al., 2010). The findings in the CHAS cohort are consistent with these previous studies despite the use of a different measure of stress.
Study limitations and strengths
The present study has multiple strengths. It included a large sample of older adults (n = 1,101), with standardized data on multiple psychological factors. Information from young adulthood/early middle age allowed for inclusion of baseline CVD risk status as a covariate. Limitations include the cross-sectional nature of analyses, which does not allow causal inferences. Although psychological measures were assessed using previously validated instruments, findings may differ if more clinical diagnostic guidelines were used. Use of pharmacotherapy was not considered. Generalizability of the findings to all community-dwelling older adult populations is limited as the CHAS cohort was relatively healthy, e.g., with a low prevalence of depressive symptoms (6.9% with CES-D scores ≥16). Previous reports of prevalence of depressive symptoms in community-dwelling older adults have ranged from 9.9%-40.3%.
It is relevant to note that in unadjusted analyses the prevalence of adverse CVD risk factors in older age was not associated with any of the psychological factors. In other words, those in the highest tertiles, i.e., increased psychological ill-being, did not display worse CVD risk factor levels in older age. This could explain the lack of association between psychological factors and atherosclerosis in this older adult cohort. Survival bias due to inability/unwillingness to participate because of ill-health or death may be responsible for these findings. For example, those excluded from final analysis as a result of missing data displayed more favorable CVD risk factor profiles when considering hypertension, dyslipidemia, and diabetes mellitus. If this limited variability of physical health profiles of those included in the final analysis, true associations with psychological ill-being may have been obscured.
Conclusions
The current study did not find a consistent or graded association between any of the psychological factors (depressive symptoms, anxiety, stress) and atherosclerosis, suggesting that among a relatively healthy cohort of older American individuals, current psychological health may not be independently associated with subclinical atherosclerosis. Future studies will need to consider cumulative, short- and long-term exposure to psychological ill-being, at varying intensities (e.g., mild depressive symptoms vs. major depressive disorder). In addition, it may be important to quantify the age at onset of psychological ill-being, as current study results suggest that pathology in late-life may not be associated with cardiovascular risk.
Highlights.
Association between psychological factors and atherosclerosis in older age.
1,101 adults ages 65-84 from the Chicago Healthy Aging Study.
Only trait anxiety was significantly associated with coronary artery calcification
Acknowledgments
Rosalba Hernandez is a T32 Post-Doctoral Fellow on NHLBI T32 HL 069771-10 (Daviglus, PI). CHAS is supported by contract R01 HLO89695 and R01 HL090873 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff, and the participants of the CHAS study for their valuable contributions.
Footnotes
Conflict of interest statement
Phyllis C. Zee reports the following—
2011-2012
Consultant: Sanofi-Aventis, UCB, Johnson and Johnson, Merck and Co, Takeda, Purdue, Philips
Research Grant Gift to Northwestern University Sleep Program: Respironics
2012-2013
Consultant: UCB, Purdue, Merck, Jazz, Vanda, Ferring, Takeda
Stock ownership: Teva
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agatisa PIK, Matthews KA, Bromberger JT, Edmundowicz D, Chang YF, Sutton-Tyrrell K. Coronary and aortic calcification in women with a history of major depression. Arch Intern Med. 2005;165:1229–36. doi: 10.1001/archinte.165.11.1229. [DOI] [PubMed] [Google Scholar]
- Arad Y, Spadaro LA, Goodman K, LledoPerez A, Sherman S, Lerner C, Guerci AD. Predictive value of electron beam computed tomography of the coronary arteries - 19-month follow-up of 1173 asymptomatic subjects. Circulation. 1996;93:1951–53. doi: 10.1161/01.cir.93.11.1951. [DOI] [PubMed] [Google Scholar]
- Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–60. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index - a New Instrument for Psychiatric Practice and Research. Psychiat Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity - A review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- Chen CS, Chen CC, Kuo YT, Chiang IC, Ko CH, Lin HF. Carotid intima-media thickness in late-onset major depressive disorder. Int J Geriatr Psych. 2006;21:36–42. doi: 10.1002/gps.1420. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- Criqui MH, McClelland RL, McDermott MM, Allison MA, Blumenthal RS, Aboyans V, Ix JH, Burke GL, Liu K, et al. The Ankle-Brachial Index and Incident Cardiovascular Events in the MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;56:1506–12. doi: 10.1016/j.jacc.2010.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detrano RC, Wong ND, Doherty TM, Shavelle R. Prognostic significance of coronary calcific deposits in asymptomatic high-risk subjects. Am J Med. 1997;102:344–49. doi: 10.1016/s0002-9343(97)00085-5. [DOI] [PubMed] [Google Scholar]
- Doobay AV, Anand SS. Sensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes - A systematic review. Arterioscl Throm Vas. 2005;25:1463–69. doi: 10.1161/01.ATV.0000168911.78624.b7. [DOI] [PubMed] [Google Scholar]
- Enoch A, Ijeoma A. The Role of Anlde-Brachial Index as a Screening Test for Coronary Artery Disease in the Hispanic Population. South Med J. 2008;101:1117–20. doi: 10.1097/SMJ.0b013e318189aabc. [DOI] [PubMed] [Google Scholar]
- Everson SA, Kauhanen J, Kaplan GA, Goldberg DE, Julkunen J, Tuomilehto J, Salonen JT. Hostility and increased risk of mortality and acute myocardial infarction: The mediating role of behavioral risk factors. Am J Epidemiol. 1997;146:142–52. doi: 10.1093/oxfordjournals.aje.a009245. [DOI] [PubMed] [Google Scholar]
- Faramawi MF, Gustat J, Wildman RP, Rice J, Johnson E, Sherwin R. Relation between depressive symptoms and common carotid artery atherosclerosis in American persons >= 65 years of age. Am J Cardiol. 2007;99:1610–13. doi: 10.1016/j.amjcard.2006.12.090. [DOI] [PubMed] [Google Scholar]
- Fowkes FGR, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, et al. Ankle brachial index combined with Framingham risk score to predict cardiovascular events and mortality - A meta-analysis. Jama-J Am Med Assoc. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–16. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB, Wilson PW. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. Jama-J Am Med Assoc. 2003;290:891–97. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. Jama-J Am Med Assoc. 2004;291:210–15. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- Hoff JA, Daviglus ML, Chomka EV, Krainik AJ, Sevrukov A, Kondos GT. Conventional coronary artery disease risk factors and coronary artery calcium detected by electron beam tomography in 30,908 healthy individuals. Ann Epidemiol. 2003;13:163–69. doi: 10.1016/s1047-2797(02)00277-6. [DOI] [PubMed] [Google Scholar]
- Iso H, Date C, Yamamoto A, Toyoshima H, Tanabe N, Kikuchi S, Kondo T, Watanabe Y, Wada Y, et al. Perceived mental stress and mortality from cardiovascular disease among Japanese men and women - The Japan Collaborative Cohort Study for Evaluation of Cancer Risk Sponsored by Monbusho (JACC Study) Circulation. 2002;106:1229–36. doi: 10.1161/01.cir.0000028145.58654.41. [DOI] [PubMed] [Google Scholar]
- Janssen I, Powell LH, Matthews KA, Cursio JF, Hollenberg SM, Sutton-Tyrrell K, Bromberger JT, Everson-Rosee SA. Depressive symptoms are related to progression of coronary calcium in midlife women: The Study of Women’s Health Across the Nation (SWAN) Heart Study. Am Heart J. 2011;161:1186–U600. doi: 10.1016/j.ahj.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E, Stampfer MJ, Willett WC. Prospective-Study of Phobic Anxiety and Risk of Coronary Heart-Disease in Men. Circulation. 1994;89:1992–97. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- Leng GC, Fowkes FGR, Lee AJ, Dunbar J, Housley E, Ruckley CV. Use of ankle brachial pressure index to predict cardiovascular events and death: A cohort study. Brit Med J. 1996;313:1440–44. doi: 10.1136/bmj.313.7070.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: Evidence, mechanisms, and treatment. Psychosom Med. 2004;66:305–15. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Colvin A, Matthews K, Bromberger JT, Sutton-Tyrrell K. Interactive Effects of Race and Depressive Symptoms on Calcification in African American and White Women. Psychosom Med. 2009;71:163–70. doi: 10.1097/PSY.0b013e31819080e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low CA, Matthews KA, Kuller LH, Edmundowicz D. Psychosocial Predictors of Coronary Artery Calcification Progression in Postmenopausal Women. Psychosom Med. 2011;73:789–94. doi: 10.1097/PSY.0b013e318236b68a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low CA, Salomon K, Matthews KA. Chronic Life Stress, Cardiovascular Reactivity, and Subclinical Cardiovascular Disease in Adolescents. Psychosom Med. 2009;71:927–31. doi: 10.1097/PSY.0b013e3181ba18ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Owens JF, Kuller LH, Sutton-Tyrrell K, Jansen-McWilliams L. Are hostility and anxiety associated with carotid atherosclerosis in healthy postmenopausal women? Psychosom Med. 1998;60:633–38. doi: 10.1097/00006842-199809000-00021. [DOI] [PubMed] [Google Scholar]
- McDermott MM, Guralnik JM, Tian L, Liu K, Ferrucci L, Liao Y, Sharma L, Criqui MH. Associations of borderline and low normal ankle-brachial index values with functional decline at 5-year follow-up: the WALCS (Walking and Leg Circulation Study) J Am Coll Cardiol. 2009;53:1056–62. doi: 10.1016/j.jacc.2008.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott MM, Liu K, Criqu MH, Ruth K, Goff D, Saad MF, Wu CL, Homma S, Sharrett AR. Ankle-brachial index and subclinical cardiac and carotid disease - The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2005;162:33–41. doi: 10.1093/aje/kwi167. [DOI] [PubMed] [Google Scholar]
- Narita K, Murata T, Hamada T, Kosaka H, Sudo S, Mizukami K, Yoshida H, Wada Y. Associations between trait anxiety, insulin resistance, and atherosclerosis in the elderly: A pilot cross-sectional study. Psychoneuroendocrino. 2008;33:305–12. doi: 10.1016/j.psyneuen.2007.11.013. [DOI] [PubMed] [Google Scholar]
- Newman AB, Shemanski L, Manolio TA, Cushman M, Mittelmark M, Polak JF, Powe NR, Siscovick D, Grp CHCR. Ankle-arm index as a predictor of cardiovascular disease and mortality in the cardiovascular health study. Arterioscl Throm Vas. 1999;19:538–45. doi: 10.1161/01.atv.19.3.538. [DOI] [PubMed] [Google Scholar]
- O’Malley PG, Jones DL, Feuerstein IM, Taylor AJ. Lack of correlation between psychological factors and subclinical coronary artery disease. New Engl J Med. 2000a;343:1298–304. doi: 10.1056/NEJM200011023431803. [DOI] [PubMed] [Google Scholar]
- O’Malley PG, Taylor AJ, Jackson JL, Doherty TM, Detrano RC. Prognostic value of coronary electron-beam computed tomography for coronary heart disease events in asymptomatic populations. Am J Cardiol. 2000b;85:945–48. doi: 10.1016/s0002-9149(99)00906-6. [DOI] [PubMed] [Google Scholar]
- Ohira T, Diez Roux AV, Polak JF, Homma S, Iso H, Wasserman BA. Associations of anger, anxiety, and depressive symptoms with carotid arterial wall thickness: the multi-ethnic study of atherosclerosis. Psychosom Med. 2012;74:517–25. doi: 10.1097/PSY.0b013e31824f6267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouriel K, Zarins CK. Doppler Ankle Pressure - an Evaluation of 3 Methods of Expression. Arch Surg-Chicago. 1982;117:1297–300. doi: 10.1001/archsurg.1982.01380340031008. [DOI] [PubMed] [Google Scholar]
- Paterniti S, Zureik M, Ducimetiere P, Touboul PJ, Feve JM, Alperovitch A. Sustained anxiety and 4-year progression of carotid atherosclerosis. Arterioscl Throm Vas. 2001;21:136–41. doi: 10.1161/01.atv.21.1.136. [DOI] [PubMed] [Google Scholar]
- Pirzada A, Reid K, Kim D, Garside DB, Lu B, Vu TH, Lloyd-Jones DM, Zee P, Liu K, et al. Chicago Healthy Aging Study: Objectives and Design. Am J Epidemiol. 2013 doi: 10.1093/aje/kwt020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events - A systematic review and meta-analysis. Arch Intern Med. 2004;164:1285–92. doi: 10.1001/archinte.164.12.1285. [DOI] [PubMed] [Google Scholar]
- Price JF, Tzoulaki I, Lee AJ, Fowkes FGR. Ankle brachial index and intima media thickness predict cardiovascular events similarly and increased prediction when combined. J Clin Epidemiol. 2007;60:1067–75. doi: 10.1016/j.jclinepi.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1:385–401. [Google Scholar]
- Regensteiner JG, Hiatt WR, Coll JR, Criqui MH, Treat-Jacobson D, McDermott MM, Hirsch AT. The impact of peripheral arterial disease on health-related quality of life in the Peripheral Arterial Disease Awareness, Risk, and Treatment: New Resources For Survival (PARTNERS) Program. Vasc Med. 2008;13:15–24. doi: 10.1177/1358863X07084911. [DOI] [PubMed] [Google Scholar]
- Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-Analysis of Perceived Stress and Its Association With Incident Coronary Heart Disease. Am J Cardiol. 2012;110:1711–16. doi: 10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and Risk of Incident Coronary Heart Disease A Meta-Analysis. J Am Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, Golzarian J, Gornik HL, Halperin JL, et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (Updating the 2005 Guideline) A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58:2020–45. doi: 10.1016/j.jacc.2011.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux AVD, Ranjit N, Powell L, Jackson S, Lewis TT, Shea S, Wu C. Psychosocial factors and coronary calcium in adults without clinical cardiovascular disease. Ann Intern Med. 2006;144:822–31. doi: 10.7326/0003-4819-144-11-200606060-00008. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Gransar H, Kubzansky LD, Wong N, Shaw L, Miranda-Peats R, Thomson LE, Hayes SW, Friedman JD, et al. Do Psychological Risk Factors Predict the Presence of Coronary Atherosclerosis? Psychosom Med. 2011;73:7–15. doi: 10.1097/PSY.0b013e3181fd94f5. [DOI] [PubMed] [Google Scholar]
- Rugulies R. Depression as a predictor for coronary heart disease - A review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- Seldenrijk A, Van Hout HPJ, van Marwijk HWJ, de Groot E, Gort J, Rustemeijer C, Diamant M, Penninx BWJH. Carotid atherosclerosis in depression and anxiety: Associations for age of depression onset. World J Biol Psychia. 2011;12:549–58. doi: 10.3109/15622975.2011.583942. [DOI] [PubMed] [Google Scholar]
- Seldenrijk A, Vogelzangs N, van Hout HPJ, van Marwijk HWJ, Diamant M, Penninx BWJH. Depressive and anxiety disorders and risk of subclinical atherosclerosis Findings from the Netherlands Study of Depression and Anxiety (NESDA) J Psychosom Res. 2010;69:203–10. doi: 10.1016/j.jpsychores.2010.01.005. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory 1970 [Google Scholar]
- Stamler J, Rhomberg P, Schoenberger JA, Shekelle RB, Dyer A, Shekelle S, Stamler R, Wannamaker J. Multivariate analysis of the relationship of seven variables to blood pressure: findings of the Chicago Heart Association Detection Project in Industry, 1967-1972. Journal of chronic diseases. 1975;28:527–48. doi: 10.1016/0021-9681(75)90060-0. [DOI] [PubMed] [Google Scholar]
- Stewart JC, Janicki DL, Muldoon MF, Sutton-Tyrrell K, Kamarck TW. Negative emotions and 3-year progression of subclinical atherosclerosis. Arch Gen Psychiat. 2007;64:225–33. doi: 10.1001/archpsyc.64.2.225. [DOI] [PubMed] [Google Scholar]
- Tiemeier H, van Dijck W, Hofman A, Witteman JCM, Stijnen T, Breteler MMB. Relationship between atherosclerosis and late-life depression - The Rotterdam study. Arch Gen Psychiat. 2004;61:369–76. doi: 10.1001/archpsyc.61.4.369. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22:300–09. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22:613–26. doi: 10.1002/gps.1723. [DOI] [PubMed] [Google Scholar]
- Williams JE, Paton CC, Siegler IC, Eigenbrodt ML, Nieto FJ, Tyroler HA. Anger proneness predicts coronary heart disease risk - Prospective analysis from the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2000;101:2034–39. doi: 10.1161/01.cir.101.17.2034. [DOI] [PubMed] [Google Scholar]
- Yu RH, Ho SC, Lam CW, Woo JL, Ho SS. Psychological factors and subclinical atherosclerosis in postmenopausal Chinese women in Hong Kong. Maturitas. 2010;67:186–91. doi: 10.1016/j.maturitas.2010.06.014. [DOI] [PubMed] [Google Scholar]


