Abstract
Objective
To measure the cost of non-attendance (“no-shows”) and benefit of overbooking and interventions to reduce no-shows for an outpatient endoscopy suite.
Methods
We used a discrete event simulation model to determine improved overbooking scheduling policies and examine the effect of no-shows on procedure utilization and expected net gain, defined as the difference in expected revenue based on CMS reimbursement rates and variable costs based on the sum of patient waiting time and provider and staff overtime. No-show rates were estimated from historical attendance (18% on average, with a sensitivity range of 12 to 24%). We then evaluated the effectiveness of scheduling additional patients and the effect of no-show reduction interventions on the expected net gain.
Results
The base schedule booked 24 patients per day. The daily expected net gain with perfect attendance is $4,433.32. The daily loss attributed to the base case no-show rate of 18% is $725.42 (16.36% of net gain), ranging from $472.14 to $1,019.29 (10.7% to 23.0% of net gain). Implementing no-show interventions reduced net loss by $166.61 to $463.09 (3.8% to 10.5% of net gain). The overbooking policy of 9 additional patients per day resulted in no loss in expected net gain when compared to the reference scenario.
Conclusions
No-shows can significantly decrease the expected net gain of outpatient procedure centers. Overbooking can help mitigate the impact of no-shows on a suite’s expected net gain and has a lower expected cost of implementation to the provider than intervention strategies.
INTRODUCTION
Endoscopy suites employ expensive human and physical resources that have high fixed costs. As a result, providers must carefully consider the number of cases scheduled per day. Unfortunately, patient attendance is uncertain. Patients may fail to attend their appointments (no-show) without prior notice, resulting in wasted capacity and a lost provider revenue opportunity. No-shows also include patients that cancel appointments on short notice (e.g., <24 hours). This equates to a no-show since a minimum time threshold is required for patients to prepare for the procedure yielding short notice rescheduling impractical. No-shows are prevalent in outpatient endoscopy suites, causing underutilization of expensive personnel and equipment, and decreased revenue. As a result, the occurrence of no-shows effectively increases the endoscopy cost, which may create a patient access barrier.
Endoscopy suite no-show rates have been reported to range from 12%–24% (1–5), and occur for a variety of reasons such as illness on the day of the procedure (1,2,4,6), procedure anxiety (1,2,4), improved symptoms (1,2), and forgetting the appointment (2,4,6). Patients are also more likely to no-show when they have to wait longer from the time the appointment is scheduled until the time the procedure occurs (2,4,7).
Several interventions offer providers the ability to lower no-show rates. These include telephone reminders, SMS (Short Message Service), and pre-assessment appointments. These no-show intervention strategies have been reported to produce relative reductions in the no-show rate of 75%, 39%, and 35%, respectively (1,5,7). In a review of 29 studies reporting intervention results for telephone reminders, SMS, and automated phone calls, the weighted (adjusting for study quality) mean relative reduction in the no-show rate was 34% (8). In addition, new interventions such as interactive voice response systems are continually being evaluated (9). While such methods show decreases in no-show rates, they can be costly to implement, and are not completely effective; thus, uncertainty in patient attendance often persists.
In addition to changing patient no-show behavior directly, endoscopy suites can also mitigate the no-show effects by scheduling additional patients, i.e., overbooking. Similar methods have been employed by hotels, car rental agencies, and airlines (10,11). However, those service industries are quite different because they have established recourse options for situations in which too many customers arrive for service. For example, they may reward customers who opt-out of service, or outsource business to another competitor. Overbooking methods have also been examined in outpatient clinic settings (12–14). However, for outpatient procedure centers, such as endoscopy suites, applying overbooking methods is problematic due to longer process durations, multiple stages of duration uncertainty (intake, procedure, recovery), and the coordination of many expensive resources (procedure rooms, endoscopists, recovery beds). Iit is neither feasible nor appropriate to deny service for a patient that has prepared for a procedure as a result of overbooking. Further, it is important to include patient waiting time costs because waiting or rescheduling can cause significant patient dissatisfaction. Therefore, the benefit of seeing more patients must be weighed against the risk of increased patient waiting time and staff overtime.
We used a discrete event simulation model to evaluate alternatives for mitigating the effect of no-shows. Simulation models have been applied to many problems related to health care delivery including endoscopy suites (15), surgical suites (16–20), primary care clinics (21,22), a pediatric emergency department (23), and other settings (24). Simulation models provide a means to test hypothetical policy changes or scenarios and limits experimentation in the practice setting, which can be time consuming and expensive. Comparisons of different scenarios can then be made based on performance measures that are important in measuring efficiency.
METHODS
Our discrete event simulation model is based on an outpatient endoscopy suite affiliated with a large academic medical center. The cost of no-shows was quantified by analyzing the difference in net gain due to the presence of no-shows compared to a perfect attendance reference scenario. We define net gain as the difference between the revenue gain from seeing each patient and the costs associated with managing the endoscopy suite. The effects of no-show interventions as well as overbooking are evaluated using this net gain definition.
Model
Our simulation model was designed by a group of systems engineers working in conjunction with several content experts from UNC School of Medicine and UNC Health Care System, Chapel Hill, NC. The group developed a conceptual model of process flow through on-site visits, meetings, e-mail, and weekly conference calls. Periodic review of the model was performed throughout the model development as part of the validation process.
Patient Flow
In a typical day, the off campus facility uses four procedure rooms, two gastroenterologists, four intake bays, four recovery bays, one intake nurse, four procedure nurses, two float nurses, one recovery nurse, and four endoscopy technicians. The model was based on three major process areas: an intake process involving the patient changing and preperation for the endoscopy, a procedure process involving sedation and procedure, and a recovery process:
Intake
Patients check-in and wait in a lobby until called back by the intake nurse or an endoscopy technician. The patient changes in one of three changing rooms and goes to one of four intake bays. Once in the intake bay, the intake nurse reviews the patient’s medical history and checks vital signs. There is one nurse designated for intake, and two float nurses who may help with intake.
Procedure
Once intake is complete, the patient is transferred to a procedure room. The patient’s procedure is reviewed, and sedation medication is administered. Each procedure requires one procedure room, one endoscopy technician, one registered nurse, and one provider to perform the endoscopy. Once the procedure is complete the patient is transferred to recovery and room turnover begins.
Recovery
One recovery nurse is designated to cover four patients. Once the patient is awake and recovered, the physician reviews the case with the patient. The patient is then discharged.
A scheduling process defines the time of patient arrivals throughout the day. This process reflects the probabilistic no-show patient behavior. Each scheduled patient passes through this decision process and has a probability of failing to attend the appointment. If a patient fails to attend, they are tallied as a no-show and exit the model; otherwise, the patient will continue to pass through the endoscopy process of the model.
The number of patients scheduled was increased iteratively, starting with one, to determine the number that maximized the net gain for the perfect attendance reference scenario. The iterative process was terminated when the expected net gain began to decrease, with respect to the previous iteration.
Overbooking
Overbooking involves booking additional patients relative to the base case schedule currently in use at the observed facility. The existing policy is as follows: two patients arrive at 8:00am. Following the initial arrival, two patients arrive at a time with interarrival times alternating between 30 and 40 minutes. The last two arrivals of the day occur at 2:20pm.
Four overbooking scheduling scenarios were compared. These scenarios were generated based on previous research and heuristics found in the outpatient appointment scheduling literature (25). The four scenarios presented were chosen to represent a wide variety of overbooking schedules. The first scheduled all overbooked patients at 8:00am. The second equally spreads overbooked patients between 8:00am and 10:00am. The third equally spreads overbooked patients between 8:00am and 12:00pm. The fourth schedule equally spreads overbooked patients between 8:00am and 2:00pm. As arbitrary examples, Table 1 illustrates the cases of overbooking four and five patients for the four scenarios.
Table 1.
Patient arrival schedules for overbooking 4 and 5 patients.
| Number Overbooked | All at 8 am | Early Morning | Morning | All Day |
|---|---|---|---|---|
| 4 | 8:00, 8:00, 8:00, 8:00 | 8:00, 8:40, 9:20, 10:00 | 8:00, 9:20, 10:40, 12:00 | 8:00, 10:00, 12:00, 2:00 |
| 5 | 8:00, 8:00, 8:00, 8:00, 8:00 | 8:00, 8:30, 9:00, 9:30, 10:00 | 8:00, 9:00, 10:00, 11:00, 12:00 | 8:00, 9:30, 11:00, 12:30, 2:00 |
Data
Historical time data was collected from July 1, 2009 to September 11, 2009, resulting in 1,184 observations. The data was extracted from ProVation RN, a third party software package, which recorded times for major steps during the colonoscopy process. In addition, a time study was performed on two separate days to determine turnover times for both intake and procedure rooms. Historical data was used to evaluate the facility no-show rate. Nurses collected 84 samples of the daily no-show rate from July-November 2009. The average daily no-show rate during this period was 18%.
Simulation Model
The discrete event simulation model was built using Arena 12.0 (26). The model consisted of intake, procedure room, and recovery modules; each having a first-come-first-serve queue discipline. Resources included intake bays, procedure rooms, recovery bays, endoscopists, nurses, and endoscopy technicians. A schematic of the processes included in the simulation model are illustrated in Figure 1. The probability distributions for intake, procedure review, sedation, procedure, recovery, and room turnover were fit using Arena 12.0 Input Analyzer. Samples for activity times were based on differences between time stamp data entries for patients that were collected using ProVation RN. Room turnover time, which was not collected in ProVation RN, was measured as the time the patient left the procedure room until the room was ready for the next procedure. Probability distributions were fit using visual fit and square error terms. Descriptive statistics and distribution information is provided in Table 2.
Figure 1.
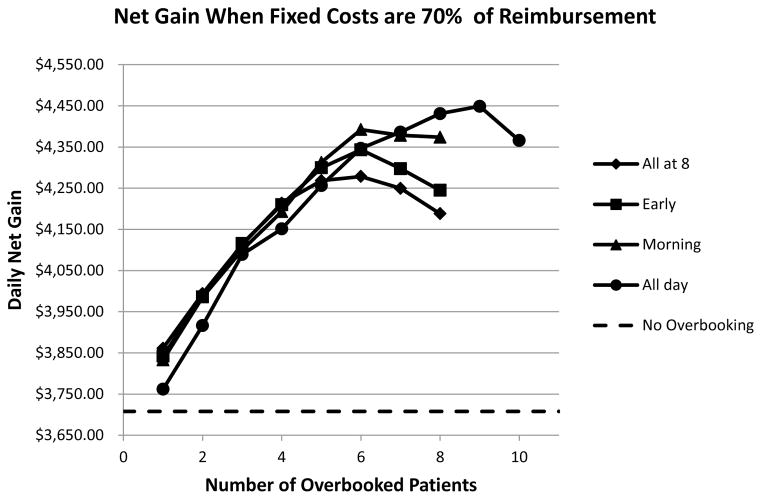
The expected net gain is presented for the baseline scenario (18% no-show rate) where fixed costs are assumed to consume 70% of reimbursements.
Table 2.
Process duration means, standard deviations, and distributions in the model fit using Arena 12.0 Input Analyzer. The distributions included shifted lognormal (LOGN), uniform (UNIF), shifted beta (BETA), shifted gamma (GAMM), and a truncated normal (NORM).
| Model Process | Duration Mean (minutes) | Standard Deviation (minutes) | Probability Distribution |
|---|---|---|---|
| Prep | 17.12 | 5.39 | 6.5 + LOGN(11.5, 9.4) |
| Procedure Review | 23.07 | 8.63 | 8 + BETA(1.14, 1.28) |
| Sedation | 12.49 | 4.26 | 5 + GAMM(3.12, 2.41) |
| Procedure | 21.80 | 10.26 | 8 + LOGN(14.1, 11.5) |
| Recovery | 50.47 | 14.55 | 22 + LOGN(29, 17.4) |
| Room Turnover | 2.41 | 1.28 | NORM(2.42, 1.28) |
To simplify the analysis, it was assumed the only procedures performed were colonoscopies. The simulation model also assumes that two endoscopists shared the four procedure rooms. This is consistent with the current practice and also reported to be an efficient configuration (15). Finally, certain processes such as scope cleaning and endoscopist dictation were not included in the simulation model since neither was a bottleneck in the system (procedures never waited for clean scope and room turnover was always longer than endoscopist dictation).
Net Gain
Three major costs were used to define the net gain from the colonoscopy procedures: operating costs, overtime costs, and patient waiting time costs. Consistent with a previous study, fixed operating costs were assumed to be 70% of the colonoscopy reimbursement (27). Fixed operating costs include capital investment, equipment costs, and staffing costs. These are fixed costs that are not affected by appointment scheduling decisions and are therefore not included in evaluating the overbooking strategy performance. The variable costs associated with the overbooking and scheduling decisions, however, are included in the overbooking strategy evaluation. The cost for patient waiting time was $18.62 per hour, based on the 2005 national average wage rate (28). Patient waiting time costs are included since we considered the societal perspective of the overbooking decisions. The waiting cost was multiplied by two in order to account for the companion that must accompany the patient due to the sedation used in the procedure. Reimbursement for a colonoscopy was obtained from CMS published rates and is estimated at $671.52(27). Overtime costs for the facility are assumed to be $12.37 per minute based on expert opinion estimate for a surgery practice (29). Overtime was measured relative to an 8.5 hour work day. Net gain is defined as expected reimbursements minus each of the costs where n is the number of patients screened during the day:
Validation
The simulation model was validated in multiple ways. First, the model was validated through code review by multiple authors, each with extensive familiarity with the modeling software. Second, results were reviewed with experts at a departmental meeting including the nurse administrator, nurses, and gastroenterologists. The consensus was that the results were reasonable and consistent with past experience and expectations. Third, total time in the endoscopy suite, estimated using the model, was compared to observed times recorded in ProVation RN. Intake times in ProVation RN that were less than ten minutes were eliminated and regarded as data entry errors because experts indicated a minimum time of ten minutes for intake. Other data was examined and unreasonable times, indicating likely data entry error, were not found. The mean (95% C.I.) expected time in system for colonoscopy patients according to ProVation RN was 138.8 (135.5, 142.1) minutes. The mean time estimated using the simulation model was 136.5 (135.6, 137.4) minutes.
Finally, simulation results were examined for extreme scenarios. For example, results were obtained for evaluating the system when only a single patient is scheduled. This resulted in an expected system time of 126.33 (124.24, 128.42) minutes with 0 patient waiting time, which is consistent with the sum of the individual process means, 124.95 minutes. Other scenarios evaluated include varying the time for recovery and evaluating the resulting system and waiting times; all behaved as expected.
RESULTS
Table 3 illustrates that net gain peaks with 24 patients scheduled under the perfect attendance scenario. All estimates were based on 500 samples (days), which provides sufficient precision for an expected net gain point estimate error of approximately less than 1%.
Table 3.
The expected net gains are displayed for scheduling 23, 24, and 25 patients where a 0% no-show rate is assumed as a reference scenario.
| Number Scheduled | Expected Net Gain | 95% CI |
|---|---|---|
|
| ||
| 23 | $ 4,364.44 | ($4,340.28, $4,388.59) |
| 24 | $ 4,433.32 | ($4,406.33, $4,460.31) |
| 25 | $ 4,339.27 | ($4,308.09, $4,370.44) |
The baseline scenario assumed a no-show rate of 18%. The difference in the expected net gain between the reference and baseline scenarios was $725.42, corresponding to a 16.36% reduction in net revenue. The net gain as well as overtime and wait time can be found for both scenarios in Table 4.
Table 4.
The sensitivity of the no-show rate on expected net gain is illustrated with 24 patients scheduled in each scenario. The reference scenario (0% no-show rate) and the baseline scenario (18% no-show rate) are included.
| No-show Rate (%) | Expected Number of Patients Attending | Expected Net Gain | Expected Overtime (hours) | Expected Patient Wait Time (min) | Expected Daily Loss |
|---|---|---|---|---|---|
|
| |||||
| 0 | 24 | $4,433.32 | 0.41 | 6.66 | - |
| 12 | 21.07 | $3,961.18 | 0.32 | 3.65 | $472.14 (10.7%) |
| 18 | 19.57 | $3,707.90 | 0.27 | 2.90 | $725.42 (16.4%) |
| 24 | 18.08 | $3,414.03 | 0.27 | 2.45 | $1,019.29 (23.0%) |
Sensitivity Analysis
Sensitivity Analysis was performed on the no-show rate. Expected net gain was calculated to reflect the range of no-show rates for endoscopy suites found in the literature ranging from 12% to 24%. The expected daily loss increases as the no-show rate increases. However, the percent loss is not equal to the no-show rate. This is in part attributed to the manner in which overtime is incurred. For example, while the loss in expected revenue corresponds to the no-show rate (since it is proportional to the decrease in the expected number of patients attending), Table 4 shows that the expected overtime and patient waiting time for the no-show rates of 12% and 24% are very close to those of a no-show rate of 18% in Table 4. Thus, the change in expected costs differs from the change in expected revenue with respect to varying no-show rates.
Overbooking
Overbooking patients throughout the day increases the expected net gain by as much as $741.04 (19.99%) over the baseline scenario (18% no-show rate). Figure 1 shows the effect that overbooking has on expected net gain when 70% of reimbursements are consumed by fixed costs, as previously described. Of the four candidate schedules, the overbooking schedule that worked best for the baseline scenario is the “All Day” schedule that equally spreads 9 overbooked patients throughout the day. While the four candidate schedules are not exhaustive in their representation, they are intended to represent a diverse range of potential overbooking schedules.
When the estimate for fixed costs as a percentage of the reimbursements increases to 80% and 90%, the number of patients by which to overbook decreases, as shown in Table 5. Further, the best performing overbooking schedule also changes when fixed costs estimates increase. The schedules that overbook patients earlier in the day (Early and Morning) result in the highest expected net gains.
Table 5.
Sensitivity analysis is presented on the estimate of the endoscopy suite’s fixed costs relative to reimbursements. For each estimate, the best number of patients to schedule, the overbooking schedule to use, and the expected net gain are presented.
| % Fixed Costs | Best Number of Patients to Schedule | Best Overbooking Schedule | Expected Net Gain |
|---|---|---|---|
| 70 | 9 | All Day | $ 4,448.94 |
| 80 | 6 | Morning | $ 2,737.74 |
| 90 | 3 | Early | $ 1,158.13 |
The best number of patients to overbook differed based on how overbooked patients are scheduled to arrive during the day. For example, if overbooked patients were only scheduled during the morning, then it is best to overbook six patients. However, if overbooked patients were scheduled throughout the entire day, overbooking by nine patients resulted in the highest expected net gain. This can be explained in part by the early part of the day becoming saturated with arrivals and patient waiting time quickly accumulating. If overbooked patients are spread throughout the day, lower expected patient wait times are incurred.
As illustrated in Table 6, the expected net gain from overbooking nine patients scheduled throughout the day is not different than the expected net gain in the reference scenario with no overbooked patients. In other words, the best performing overbooking policy for a no-show rate of 18% is no different in expected net gain than having a no-show rate of 0% with no overbooking.
Table 6.
The reference scenario (0% no-show rate) is compared to overbooking 9 patients with a no-show rate of 18%.
| No-show Rate (%) | Number Over-booked | Expected Number of Patients Attending | Expected Net Gain (95% CI) | Expected Overtime (hours) | Expected Patient Wait Time (min) |
|---|---|---|---|---|---|
|
| |||||
| 0 | 0 | 24 | $4,433.32 (4,406.33, 4,460.31) | 0.32 | 6.66 |
| 18 | 9 | 26.976 | $4,448.94 (4,408.59, 4,489.29) | 0.83 | 21.23 |
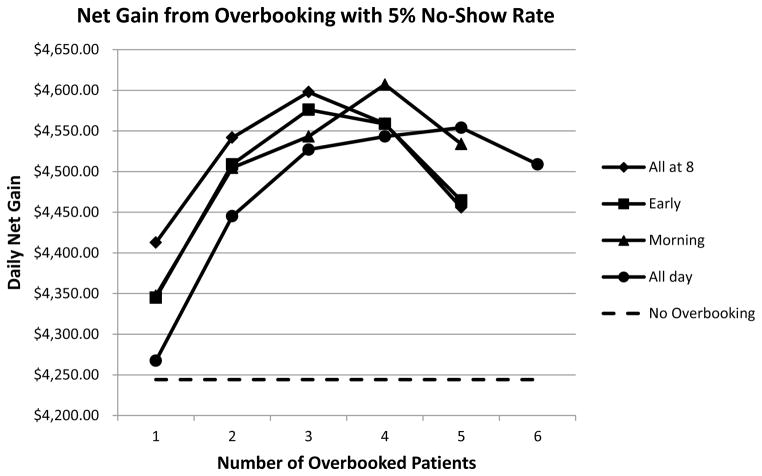
When overbooking is used when the no-show rate is low, similar results show that the number of patients by which to overbook depends on how the overbooked patients are scheduled to arrive. Figure 2 illustrates this result with the number of patients to overbook being based on the scheduling policy providing the highest expected net gain. With a 5% no-show rate, overbooking by four patients and scheduling them to arrive throughout the morning results in the highest expected net gain.
Figure 2.
The expected net gain is presented for where the no-show rate is 5%.
It is important to note that the studied endoscopy suite had two procedure rooms for each endoscopist. Thus, based on the low turnover times it is unlikely that room turnover or scope cleaning would be a bottleneck in the system. However, in other practices it may be the case that turnover times are much higher or there is only a single procedure room for each endoscopist. The implications of the procedure room turnover being a bottleneck are a lower number of patients by which to overbook. For example, when the mean room turnover times were increased by factors of five and ten, the resulting number of patients by which to overbook is five and three, respectively, when the overbooked patients are spread throughout the day. In other words, the number of patients by which to overbook is sensitive to the room turnover time and decreases as the turnover time increases. Each procedure requires additional procedure room time, and as a result, additional procedures scheduled later in the day are completed using overtime.
Intervention Strategies
Various no-show intervention strategies have been reported to reduce no-shows with varying success rates including telephone reminders, SMS (Short Message Service), and pre-assessment appointments. The lower and upper bounds of the intervention relative no-show reductions were 34.5% and 75.5% based on reductions reported in the literature for endoscopy settings (1,5). In the context of the practice we studied, such reductions would translate to no-show rates of 11.79% and 4.41%, respectively. The results of those no-show rates presented in Table 7 are based on scheduling 24 patients using the baseline arrival schedule.
Table 7.
The expected net gain is displayed over the range of no-show rates resulting from implementing no-show intervention strategies in the baseline scenario (18% no-show rate).
| No-show Rate (%) | Expected Number of Patients Attending | Expected Net Gain (95% CI) | Expected Overtime (hours) | Expected Patient Wait Time (min) | Expected Daily Loss |
|---|---|---|---|---|---|
|
| |||||
| 4.41 | 22.94 | $4,265.94 (4,237.44, 4,294.44) | 0.37 | 5.37 | $167.38 (3.8%) |
| 11.79 | 21.15 | $3,969.05 (3,936.46, 4,001.64) | 0.33 | 3.75 | $464.27 (10.5%) |
DISCUSSION
The net loss due to no-shows at the modeled facility was 16.4% per day. No-show intervention strategies were evaluated and were found to reduce the loss attributed to no-shows to between 3.8% and 10.5%. In other words, the expected net gains resulting from intervention strategies recoup between 36.0% and 76.9% of the loss attributed to no-shows. The overbooking policy with nine overbooked patients resulted in a minimal difference in expected net gain when compared to the reference scenario (0% no-show rate). However, the number of patients to overbook decreases as fixed costs increase. Further, with higher estimates of fixed costs relative to reimbursements, the results show that overbooking earlier in the day is better. These estimates can be used to help justify implementing an intervention method(s) that will drive down no-show rates. Further, the findings indicate that overbooking is a very effective measure for increasing performance at an endoscopy suite.
No-show behavior is a challenging problem with a negative chain reaction. The financial loss due to no-shows can be significant to practices such as the endoscopy suite we studied. As a result, no-shows increase the cost of each procedure performed. Through improved scheduling methods resulting in better efficiency, there are opportunities to mitigate such financial losses. As a result, overbooking methods and no-show intervention strategies have potential to reduce costs and the price of endoscopies and thus improve access. However, in the current system, any improvement in efficiency is likely to be realized in increased profits for the practice.
Overbooking methods have been examined in previous research in the scheduling literature (12–14). LaGanga and Lawrence (2007) proposed a utility model and used discrete event simulation to show that overbooking can be an appropriate method in certain cases such as high patient throughput, high no-show rates, and low service duration variability. Muthuraman and Lawley (2008) used queueing methods in their overbooking model with patient attendance uncertainty where appointment decisions are made dynamically as patient requests occur. Their work was extended by Zeng et al. (2010) to include heterogeneous no-show probabilities that vary based on patient attributes. While important insights about overbooking in outpatient clinics were developed in these works, they also include assumptions that are restrictive to a general outpatient procedure setting such as endoscopy suites including deterministic service times, single server systems, or exponentially distributed service times. Overbooking has also been considered within the context of endoscopy suites (6). In contrast with the previous analysis by Sonnenberg (2009), our study concludes that overbooking policies can achieve the same expected net gain that would be realized if all patients attended their appointments. In his research, Sonnenberg uses the binomial distribution to analyze no-show rates and states that the benefit gained from overbooking will increase as no-show rates increase and as the number of endoscopy slots available increases. In addition he finds that the relative loss associated with overbooking increases as no-show rates increase and as the number of available endoscopy slots decreases. However, he concludes that overbooking is not able to completely recoup the loss attributed to no-shows.
Our study differs in the following ways. First, we used a validated discrete event simulation model to evaluate the effects of no-shows on the endoscopy suite. This allowed us to include multiple stages (intake, procedure, recovery) and multiple resources (providers, procedure rooms, nurses) in our model as opposed to analyzing a single provider alone without considering the impact of patient flow in stages both up and down stream. Since uncertainty is inherent in many aspects of the system, this modeling approach provided a method to accurately include the complexity of the endoscopy suite in our model. Second, Sonnenberg measured the costs of overbooking as a ratio of the endoscopy suite’s benefit. In contrast, we modeled expected revenue from reimbursements and expected costs using estimates for fixed facility costs, patient wait time, and overtime. Finally, we model the uncertainty in process durations using historical data. This allowed us to include patient waiting and overtime directly in our cost estimates as compared to using the number of appointment slots and cost/benefit ratio estimates.
Thus, by avoiding closed form analyses based on a single provider, our simulation model allowed us to more explicitly model the effects of no-shows on the endoscopy suite we studied with a greater level of fidelity. While we conclude that overbooking can achieve more significant gains than has been previously reported for endoscopy suites, we affirm that overbooking can be a low cost and easily implemented strategy for mitigating the effects of no-shows.
The relative no-show rate reductions reported for various intervention strategies were evaluated and were found to recoup some of the loss attributed to no-shows. For example, the expected daily loss attributed to no-shows was reduced from 16.4% to a range of 3.8–10.5% through intervention strategy implementation. However, based on our results no intervention strategy was found to completely mitigate the loss in net gain. Further, depending on a practice’s infrastructure, such strategies may be costly. Overbooking policies, on the other hand, were demonstrated to completely recoup the financial loss attributed to no-shows. The performance of an overbooking policy, however, is sensitive to how overbooked patients are scheduled to arrive throughout the day. Thus, while implementing an overbooking schedule in addition to a no-show intervention is a possible course of action, overbooking alone can provide the same expected net gain results.
Impact on Indirect Waiting
Implementing overbooking schedules will also result in decreased indirect waiting time, or the time a patient waits between when an appointment is requested and when the procedure is actually scheduled. In order to evaluate overbooking’s effect on indirect waiting, we introduce a simple queueing model. In queueing theory, Little’s Law can be used to describe the relationship between the average number of customers waiting for service, L, the average time spent waiting for service, W, and the average service rate, λ(30). Little’s Law states that L= λW. Under the current scheduling practice where 24 patients are scheduled per day, patients typically wait 8 weeks for a requested appointment. Thus, L= λW=24 patients/day × 40 days = 960 patients waiting for their appointment at any given time. However, if λ′=33 based on the best overbooking scheduling rule and the same number of patients continue to request appointments, then W′=L/λ=960/33=29.09 days. Thus, through overbooking, the indirect waiting time can be reduced by over 25%. Therefore, the potential effects of overbooking can be extended to settings with no-shows where patient access is a challenge due to high demand and low resource levels.
Limitations
Study limitations include using a single endoscopy unit, and cost structure assumptions, as the basis for our model. The effectiveness of no-show mitigation strategies will certainly depend on the structure of a particular practice. Along with this modeling limitation is the use of a small time study along with expert opinion for estimates where data could not be abstracted from electronic sources, such as procedure turnover times. Regarding the cost structure, we further assume that resource levels are fixed at their present state. However, incorporating planning decisions about resource levels over time, and their impact on overbooking decisions, are important future research directions. Second, this study does not consider certain non-monetary costs such as dissatisfaction associated with overtime. For example, while employees may tolerate a small amount of overtime in return for higher compensation, their tolerance will likely decrease as overtime continues to accrue. This would suggest that a non-linear overtime cost estimate, where the overtime hourly wage increases for higher overtime hours, may be more appropriate and should be considered as a direction for future work. Third, we did not discuss the low probability case where all of the patients attend when overbooking. While the probability of this scenario is certainly low (1 in 1000 days when 33 patients are scheduled), provider fatigue is a challenge that should be considered. Fourth, our analysis assumed a homogeneous case mix of colonoscopy procedures. Since different procedures have different duration distributions, the case mix would likely impact the overbooking decision. Defining the optimal case mix remains an open question. Fifth, overbooking in endoscopy suites is likely to differ from other outpatient settings, such as primary care, in that patient visit frequency is comparatively low (every 3 to 10 years). Thus, patients are unlikely to modify their arrival habits based on their understanding of the booking practice being used. While this may not necessarily be a valid assumption in other outpatient settings, it is an interesting direction for future research. Finally, overbooking serves as a helpful tool for the provider and management to increase practice efficiency. However, overbooking does not help individual patients who do not receive requisite care because of non-attendance. For the purpose of providing care to the patients likely to no-show, other intervention strategies should be continually evaluated.
Conclusions
In this paper, we used a discrete event simulation model based on an outpatient endoscopy suite to measure the cost of no-shows and evaluate the effects of mitigation strategies as well as overbooking policies. In summary, the financial loss attributed to no-shows can be very high based on reported no-show rates for the practice we studied and those in the literature and can significantly decrease the expected net gain of outpatient procedure centers. No-show interventions reduce the no-show rate; but can be costly, challenging to implement, and do not resolve the problem entirely. Overbooking can help mitigate the impact of no-shows on a suite’s expected net gain and has a lower expected cost of implementation to the provider.
Acknowledgments
Grants: This research was funded in part by the National Science Foundation under grant CMMI-0844511.
This material is based in part upon work supported by the National Science Foundation under Grant Number CMMI 0844511. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation.
Footnotes
Meetings: This work was presented as an oral presentation at the Annual Meeting of the Society for Medical Decision Making in Chicago, IL in October, 2011.
References
- 1.Tibble JA, Forgacs I, Bjarnason I, Przemioslo R. The effects of a preassessment clinic on nonattendance rates for day-case colonoscopy. Endoscopy. 2000;32(12):963–965. doi: 10.1055/s-2000-9629. [DOI] [PubMed] [Google Scholar]
- 2.Sola-vera J, Sáez J, Laveda R, Girona E, Fegarcía-sepulcre M, Cuesta A, et al. Factors associated with non-attendance at outpatient endoscopy. Scand J Gastroenterol. 2008;43(2):202–206. doi: 10.1080/00365520701562056. [DOI] [PubMed] [Google Scholar]
- 3.Hardy KJ, O’Brien SV, Furlong NJ. Information given to patients before appointments and its effect on non-attendance rate. BMJ. 2001;323(7324):1298–1300. doi: 10.1136/bmj.323.7324.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adams L, Pawlik J, Forbes G. Nonattendance at outpatient endoscopy. Endoscopy. 2004;36(5):402–404. doi: 10.1055/s-2004-814329. [DOI] [PubMed] [Google Scholar]
- 5.Lee CS, McCormick PA. Telephone reminders to reduce non-attendance rate for endoscopy. J R Soc Med. 2003;96(11):547–548. doi: 10.1258/jrsm.96.11.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sonnenberg A. How to overbook procedures in the endoscopy unit. Gastrointest Endosc. 2009;69(3):710–715. doi: 10.1016/j.gie.2008.09.052. [DOI] [PubMed] [Google Scholar]
- 7.Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust. 2005;183(7):366–368. doi: 10.5694/j.1326-5377.2005.tb07085.x. [DOI] [PubMed] [Google Scholar]
- 8.Hasvold PE, Wooton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare. 2011;17(7):358–364. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Griffin JM, Hulbert EM, Vernon SW, Nelson D, Hagel EM, Nugent S, Simon AB, Bangerter A, van Ryn M. Improving Endoscopy Completion: Effectiveness of an Interactive Voice Response System. Am J Manag Care. 2011;17(3):199–208. [PubMed] [Google Scholar]
- 10.Weatherford LR, Bodily SE. A taxonomy and research overview of perishable-asset revenue management: yield management, overbooking, and pricing. Oper Res. 1992;40(5):831–844. [Google Scholar]
- 11.Rothstein M. OR and the airline overbooking problem. Oper Res. 1985;33(2):237–248. [Google Scholar]
- 12.LaGanga LR, Lawrence SR. Clinic Overbooking to Improve Patient Access and Increase Provider Productivity*. Decision Sciences. 2007;38(2):251–276. [Google Scholar]
- 13.Muthuraman K, Lawley M. A stochastic overbooking model for outpatient clinical scheduling with no-shows. IIE Transactions. 2008;40(9):820–837. [Google Scholar]
- 14.Zeng B, Turkcan A, Lin J, Lawley M. Clinic scheduling models with overbooking for patients with heterogeneous no-show probabilities. Annals of Operations Research. 2010;178(1):1–24. [Google Scholar]
- 15.Berg B, Denton B, Nelson H, Balasubramanian H, Rahman A, Bailey A, et al. A discrete event simulation model to evaluate operational performance of a colonoscopy suite. Medical Decision Making. 2010;30(3):380–387. doi: 10.1177/0272989X09345890. [DOI] [PubMed] [Google Scholar]
- 16.Dexter F, Macario A, Traub RD, Hopwood M, Lubarsky DA. An operating room scheduling strategy to maximize the use of operating room block time: computer simulation of patient scheduling and survey of patients’ preferences for surgical waiting time. Anesthesia & Analgesia. 1999;89(1):7–20. doi: 10.1097/00000539-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Marcon E, Dexter F. Impact of surgical sequencing on post anesthesia care unit staffing. Health Care Manag Sci. 2006;9(1):87–98. doi: 10.1007/s10729-006-6282-x. [DOI] [PubMed] [Google Scholar]
- 18.Marcon E, Kharraja S, Smolski N, Luquet B, Viale JP. Determining the number of beds in the postanesthesia care unit: a computer simulation flow approach. Anesthesia & Analgesia. 2003;96(5):1415–1423. doi: 10.1213/01.ANE.0000056701.08350.B9. [DOI] [PubMed] [Google Scholar]
- 19.Tyler DC, Pasquariello CA, Chen CH. Determining optimum operating room utilization. Anesthesia & Analgesia. 2003;96(4):1114–1121. doi: 10.1213/01.ANE.0000050561.41552.A6. [DOI] [PubMed] [Google Scholar]
- 20.Van Houdenhoven M, Van Oostrum JM, Hans EW, Wullink G, Kazemier G. Improving operating room efficiency by applying bin-packing and portfolio techniques to surgical case scheduling. Anesthesia & Analgesia. 2007;105(3):707–714. doi: 10.1213/01.ane.0000277492.90805.0f. [DOI] [PubMed] [Google Scholar]
- 21.Klassen KJ, Rohleder TR. Scheduling outpatient appointments in a dynamic environment. J Oper Manage. 1996;14(2):83–101. [Google Scholar]
- 22.Stahl JE, Roberts MS, Gazelle S. Optimizing management and financial performance of the teaching ambulatory care clinic. Journal of general internal medicine. 2003;18(4):266–274. doi: 10.1046/j.1525-1497.2003.20726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hung GR, Whitehouse SR, O’Neill C, Gray AP, Kissoon N. Computer modeling of patient flow in a pediatric emergency department using discrete event simulation. Pediatr Emerg Care. 2007;23(1):5–10. doi: 10.1097/PEC.0b013e31802c611e. [DOI] [PubMed] [Google Scholar]
- 24.Jun JB, Jacobson SH, Swisher JR. Application of discrete-event simulation in health care clinics: A survey. J Oper Res Soc. 1999;50(2):109–123. [Google Scholar]
- 25.Ho CJ, Lau HS. Minimizing total cost in scheduling outpatient appointments. Management Science. 1992;38(12):1750–1764. [Google Scholar]
- 26.Kelton W, Sadowski R, Sadowski D. Simulation with Arena. New York. NY: McGraw-Hill; 2007. [Google Scholar]
- 27.Vargo JJ, Bramley T, Meyer K, Nightengale B. Practice efficiency and economics: the case for rapid recovery sedation agents for colonoscopy in a screening population. J Clin Gastroenterol. 2007;41(6):591–598. doi: 10.1097/01.mcg.0000225634.52780.0e. [DOI] [PubMed] [Google Scholar]
- 28.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Value of patient time invested in the colonoscopy screening process: time requirements for colonoscopy study. Medical Decision Making. 2008;28(1):56–65. doi: 10.1177/0272989X07309643. [DOI] [PubMed] [Google Scholar]
- 29.Batun S, Denton BT, Huschka TR, Schaefer AJ. The benefit of pooling operating rooms and parallel surgery processing under uncertainty. Informs Journal on Computing. 2011;23(2):220–237. [Google Scholar]
- 30.Little JDC. A Proof for the Queuing Formula: L=λW. Operations Research. 1961;9(3):383–387. [Google Scholar]