Abstract
Background: Glenoid bone damages consisting of anterior rim erosion and bony avulsion are very important in decision making for treatment of recurrent dislocation in shoulder joint. This study was aimed to determine the prevalence of these damages in patients with anterior recurrent shoulder dislocation.
Methods: The study was a cross-sectional study evaluating patients with unstable shoulder joint. Glenoid bone damage was assessed using three dimensional (CT) scan implementing either glenoid width index or by Pico method.
Result: Ninety two patients were assessed by glenoid width index and 19 by PICO. Among the first group, 6 patients (6%) had intact shoulder joint and 86 patients (93%) had glenoid lesion including 56 (60.9%) erosions and 30 (32.6%) with bony Bankart. In this group, 60 (65%) patients had Hill-Sachs lesion. Using Pico evaluation, 8 (42%) had bony Bankart, 9 (47%) erosion and 2 (10%) no lesion, and 8 (42%) Hill-Sachs.
Conclusion: There was no significant correlation between severities of glenoid bone loss with patients'frequency of dislocations. Patients with convulsion-induced shoulder dislocation had the most severe bone loss. The CT scan should be done early in recurrent dislocation because severe bony damage could occur even after few dislocations. The overall prevalence of glenoid bone damage including bony Bankart and erosion are high in recurrent anterior dislocation. This is particularly emphasized in patients with seizure.
Keywords: Glenoid lesions, Recurrent shoulder dislocation, 3 dimensional CT scan, Pico
Introduction
Glenohumeral joint dislocation is the most common dislocation seen in human body and accounts for about 50% of all joint dislocations (1, 2). Anterior shoulder dislocation constitutes 95% of all shoulder dislocations. Young men with high energy contacts are at the highest risk. Shoulder instability is a complication of joint dislocation in 95% of patients younger than 20 years and 15% older than 40 (1). The important factors associated with shoulder instability after first dislocation are young age, ligament laxity, glenoid and humeral head bony lesions (3-5). Patient's age is considered as the most important predictor of recurrent dislocation (6, 7). Family history has been also reported by some studies as other risk factor (8).
The pathology of recurrent shoulder dislocation has been evaluated for long time. In 1938, a British surgeon named Bankart described a lesion which is now called Bankart Lesion. This damage is due to compression on the anterior-inferior articular surface of glenoid by humeral head in the abduction and external rotation position which leads to head dislocation and soft tissue detachment. Bankart lesion was reported as the most prevalent lesion after shoulder dislocation and has been seen in majority of patients with shoulder instability (1). However, sometimes this lesion presents as bony avulsion or rim erosion instead of soft tissue detachment (9). Theorically, anterior rim erosion can contribute itself to anterior instability due to loss of anterior buttress. Therefore, knowing the presence as well as its size is very important in making decision for surgical treatment. Bone loss due to compression fracture of the posterolateral side of the humeral head is called Hill-Sachs deformity (9). Although Hill-Sachs lesions are usually small and do not have effect on instability (6), but in the presence of wider than 30% joint surface involvement, dislocation would happen if humeral head engaged with anterior glenoid in the external rotation position.
This study was aimed to determine the prevalence of glenoid erosion and bony Bankart lesion in anterior shoulder dislocation using either 3-D CT scan or a new method, PICO. The correlation between the number of dislocations and severity of bone loss was also evaluated.
Methods
Patients
This was a cross sectional study evaluating 111 patients with recurrent anterior shoulder dislocation referred to orthopedic clinic of Imam Khomeini Hospital. Patients were enrolled consecutively from 2008 to 2011. The inclusion criteria were history of anterior shoulder dislocation for more than 2 times or patients with history of seizure and one dislocation. All patients were given informed consensus after detailed explanation.
Evaluation
The patients were divided in two groups. First with, the glenoid index method, both shoulders were evaluated with three-dimensional CT (spiral CT scan, 2-mm slice thickness, three-dimensional-edit mode). The head of humerus was eliminated and the ultimate image showed acromioclavicular joint to just below the glenoid bone. The images were reconstructed as multi planar reconstruction based on oblique, sagittal and axial view of glenoid surface to construct en face view of glenoid joint surface. The length of the horizontal axis of the glenoid was measured through the widest part of the mid portion of the inferior glenoid and the axis of the damaged shoulder was compared to healthy shoulder. The size of the damage was measured as the ratio of width of damaged shoulder to healthy shoulder (Figure 1).
Fig. 1 .
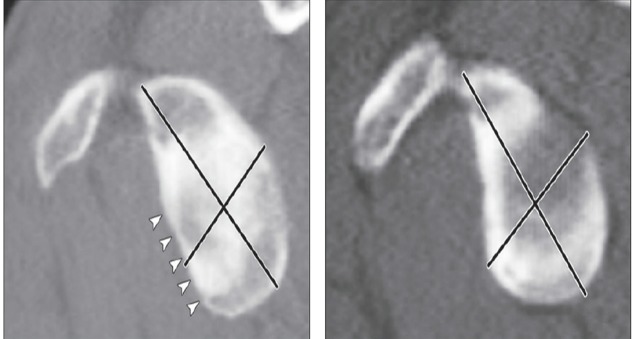
Evaluation of glenoid bone lesion using glenoid index method. Arrow head shows the erosion direction and lesion area.
In the second group a new method was implemented. This method, proposed by Sugaya, is based on the observation that the inferior portion of healthy glenoid contour fit the shape of true circle so that the surface could be calculated meticulously (10). Huijsman used the circle method proposed by Sugaya on 14 cadaver shoulders to validate 3D CT scans for quantification of the glenoid bone defect (11). The method coined later as “Pico “in memorial of Italian renaissance philosopher , Giovanni Pico della Mirandola, showed a very good intra-observer and interobserver reliability . “The pico method “ has been implemented by obtaining a circle base on the diameter from 3 o’clock to 9 o’clock ,on the en face images, thereafter the size of the lesion was calculated as a ratio of the surface of the damaged portion of glenoid to the area of outer fitting circle (12) (Figure 2).
Fig. 2 .
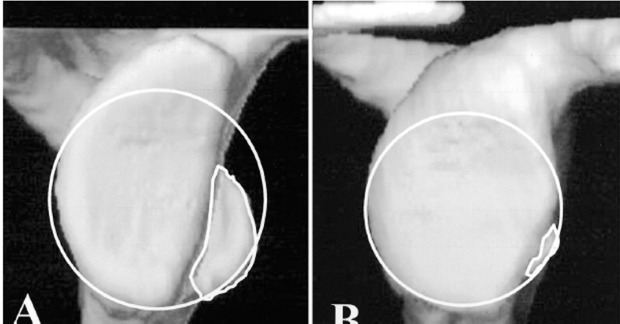
Evaluation of glenoid bone loss using Pico method.
Statistical analysis
Quantitative data were reported as mean and standard deviation (SD) and the categorical data as frequency and percent. The correlation between the number of dislocations with severity of glenoid bone loss was evaluated using Pearson’s correlation test. The Probability value (P value) less than 0.05 was considered significant. All analyses were done using SPSS vs. 16 version.
Results
111 patients with recurrent anterior shoulder dislocation enrolled in the present study. Of these patients, 92 were evaluated by glenoid width index and 19 by Pico method.
Glenoid index evaluation
There were 2 women (2.2%) and 90 (97.8%) men with the mean age of 25.8±4.1 years (16 to 37 years). Using glenoid index evaluation by 3 dimensional CT scan, 86 patients (93.4%) had glenoid bony damage and the others (6.5%) did not have any lesion. 30 patients (32.6%) had bony Bankart lesion and 56 (60.9%) bone erosions (Table1), and sixty (65.2%) Hill-Sachs damage.
Table 1. Glenoid lesions evaluated by glenoid index and Pico, number (%).
| Method | Glenoid Index | Pico |
| Glenoid lesion | 86 (93.4%) | 17 (89%) |
| Erosion | 56 (60.9%) | 9 (47%) |
| bony Bankart | 30 (32.6%) | 8 (42%) |
| Hill-Sachs | 60 (65.2%) | 8 (42%) |
Excluding seizure cases, patients with anterior glenoid bone loss had an average of 10% (ranging 0% to 18%) bone loss. In patients with seizure, average glenoid bone loss was 40% (ranging 30% to 50%).With large and deep hill-sachs leisions (Fig. 3).
Fig. 3 .
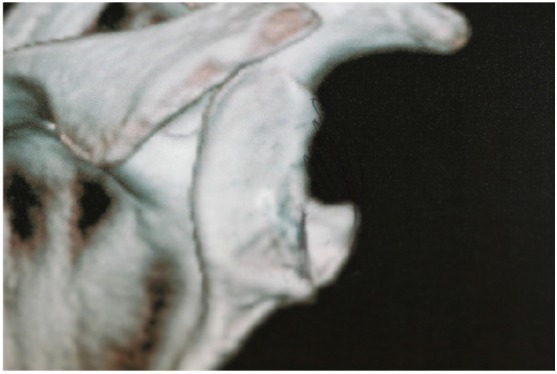
Severe damage is found after seizure-induced shoulder dislocation
Pico evaluation
19 patients in this group were all men with the mean age of 32.7±6.3 (23 to 41 years), In which 17 (89%) had glenoid lesion; 8 (42%) bony Bankart lesion while 9 patients (47%) counted to have erosion without bone fragment, and 8 (42%) had Hill-Sachs lesion (Table 1).
Apart from cases with history of seizure related dislocation, we did not find any case with glenoid bone loss of more than 20%
Severity of glenoid bone loss did not have significant correlation with number of shoulder dislocation (r=0.136, p>0.05, figure 4).
Fig. 4 .
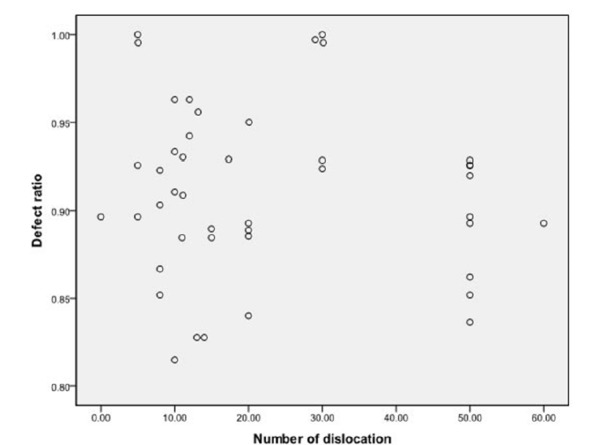
correlation between number of dislocations and severity of bone loss (r=0.136, p value> 0.05).
Discussion
The results of the present study showed that the majority of cases with recurrent anterior shoulder dislocation have anterior glenoid bone lesion leading to reduction of anterior-posterior diameter (93% of patients). The lesion can be either bony Bankart or more commonly glenoid erosion. From all patients with glenoid lesion, 65% had Hill-Sacks lesion. Excluding seizure induced shoulder dislocation, and none of our patients had more than 20% glenoid bone loss, which usually considered as significant loss in the literature (13).
There are many studies in regard to the value of three dimensional CT scan in diagnosis of glenoid lesions. The study achieved by james F. Griffith reveals that glenoid bone loss was common, since it was evident in 41% of single and 86% of recurrent dislocated shoulders (9). Sugaya et al applied a best-fit circle to the inferior glenoid on 3D reconstructed CT scan images. Glenoid lesion was present in 90% of recurrent dislocated shoulders, comprising a fracture in 50% and an erosion in 40% of the cases (10).
In a study by Calandra et. al in 1989, of 47% had Hill-Sachs lesion with an acute dislocation which was less than the result obtained in the present investigation (14).
On the basis of the findings of the present study, the correlation between damage severity and number of dislocations was not significant.
Mentioning as a limit in this study, patients with ligament laxity and trauma induced dislocation were not evaluated separately in the present study and should be investigated in further studies. There may be considrable correlation between number of dislocations and severity of bone loss in patients with trauma induced dislocation. It is highly suggested to confirm the findings of the imaging studies using arthroscopy which could be assumed as a gold standard for post-dislocation complications diagnosis.
Damage severity was almost similar in both evaluation methods (Pico vs. glenoid index) however Pico seems to be as accurate and using less x-ray exposure because only the affected shoulder is evaluated.
Conclusion
Bone damages are common in recurrent anterior shoulder dislocation including erosion and/or bony Bankart lesions. These lesions should be presumed inevitable and severe damage that could occur after numbers of dislocations. Thus, damage severity should be evaluated soon after dislocations.
Pico method is suggested for assessing the bone loss severity, because this method does not need to scan both shoulders therefore the patient receives less radiation.
Dislocations after seizure can cause more severe damage to glenoid joint and patients are at higher risk for severe bone loss than others. Severity of complications is dependent on various factors and not exclusively the number of dislocation.
Hill-Sachs lesion is common within these patients and physicians should not limit the evaluations on the glenoid and ignoring head of humerus.
Cite this article as: Guity M. R, Akhlaghpour Sh, Yousefian R. Determination of prevalence of Glenoid bony lesions after recurrent anterior shoulder dislocation using the 3-D CT scan. Med J Islam Repub Iran 2014 (3 Mar). Vol. 28:20.
References
- 1.Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009;91:2–7. doi: 10.1308/003588409X359123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phillips BB. Recurrent dislocations in: Canale ST,editor Campbell’s operative orthopaedics, 9 edn. Philadelphia: Mosby. 2003:2377–448. [Google Scholar]
- 3.Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am. 1982;64:494–505. [PubMed] [Google Scholar]
- 4.Bigliani LU, Newton PM, Steinmann SP, Connor PM, McLlveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26:41–5. doi: 10.1177/03635465980260012301. [DOI] [PubMed] [Google Scholar]
- 5.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patientsA ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–84. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Robinson CM, Dobson RJ. Anterior instability of the shoulder after trauma. J Bone Joint Surg Br. 2004;86:469–79. doi: 10.1302/0301-620x.86b4. [DOI] [PubMed] [Google Scholar]
- 7.Kralinger FS, Golser K, Wischatta R, Wambacher M, Sperner G. Predicting recurrence after primary anterior shoulder dislocation. Am J Sports Med. 2002;30:116–20. doi: 10.1177/03635465020300010501. [DOI] [PubMed] [Google Scholar]
- 8.O'Driscoll SW, Evans DC. Contralateral shoulder instability following anterior repairAn epidemiological investigation. J Bone Joint Surg Br. 1991;73:941–6. doi: 10.1302/0301-620X.73B6.1955441. [DOI] [PubMed] [Google Scholar]
- 9.Griffith JF, Antonio GE, Yung PS, Wong EM, Yu AB, Ahuja AT. et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008;190:1247–54. doi: 10.2214/AJR.07.3009. [DOI] [PubMed] [Google Scholar]
- 10.Sugaya H, Moiishi j, Dohi M, Kon Y. Glenoid rim morphology in recurrent anterior glenohumeral instability. j Bone joint Surg Am. 2003;85:878–84. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Huijsmans PE, Haen ps, Kidd M, Dhert WJ, van der Hulst VP. Quantification of a glenoid defect with three dimensional computed tomography and magnetic resonance imaging: a cadaveric study. J shoulder Elbow Surg. 2007;16 doi: 10.1016/j.jse.2007.02.115. [DOI] [PubMed] [Google Scholar]
- 12. Intra-observer and interobserver reliability of the "Pico" computed tomography method for quantification of glenoid defect in anterior shoulder instability. [DOI] [PubMed]
- 13.CHen AL, Hurt SA, Hawking RJ. et al. management of bone loss assosiated with recurrent glenohumeral instability. Am J Sports Med. 2005;33:912. doi: 10.1177/0363546505277074. [DOI] [PubMed] [Google Scholar]
- 14.Calandra JJ, Baker CL, Uribe J. et al. The incidence of Hill–Sachs lesions in initial anterior shoulder dislocations. Arthroscopy. 1989;5(4) doi: 10.1016/0749-8063(89)90138-2. [DOI] [PubMed] [Google Scholar]


