Abstract
Background and study aims
Demand for endoscopic procedures worldwide has increased while the number of physicians trained to perform endoscopy has remained relatively constant. The objective of this study was to characterize lower and upper endoscopic procedures performed by non-physicians.
Patients and methods
Bibliographical searches were conducted in Medline, EMBASE, and Cochrane library databases. Studies were included if patients underwent flexible sigmoidoscopy, colonoscopy or upper endoscopy by a non-physician (nurse, nurse practitioner, physician assistant) and had outcome measures reported (polyps, adenomas and/or cancer detected, adverse events). Pooled rates were calculated for specific outcomes and rate ratios were determined for selected comparison groups.
Results
The majority of studies included nurses who performed flexible sigmoidoscopies for colorectal cancer screening. Nurses and nurse practitioners/physician assistants who performed flexible sigmoidoscopies had a pooled polyp detection rate of 9.9% and 23.7%, adenoma detection rate of 2.9% and 7.2%, colorectal cancer detection rate of 1.3% and 1.2% and an adverse event rate of 0.3 and 0 per 1,000 sigmoidoscopies, respectively. There was no significant difference between polyp and adenoma detection rates in studies comparing nurses or nurse practitioners/physician assistants with physicians performing sigmoidoscopy. Among studies of non-physicians performing colonoscopies (n=3), the pooled adenoma detection rate was 26.4%, cecal intubation rate of 93.5% and an adverse event rate of 2.2/1,000 colonoscopies. Of the few studies examining upper endoscopies 99.4% of upper endoscopy procedures performed by nurses were successful with no reported adverse events.
Conclusion
Available studies in the literature suggest that non-physicians perform endoscopic procedures, especially lower endoscopies, with outcomes and adverse events in line with physicians.
Keywords: endoscopy, colonoscopy, flexible sigmoidoscopy, upper endoscopy, non-physician, quality, mid-level providers
INTRODUCTION
The demand for endoscopic procedures has dramatically increased over the last three decades in the U.S. and around the world and will continue to grow in upcoming years[1]. During the same period the number of physicians trained to perform endoscopy has remained constant while the number of years required for gastrointestinal training has increased[2], a trend mirrored in many other countries worldwide. Such a disconnect between demand and supply can result in increased patient wait times for endoscopic procedures, impaired patient access to endoscopy and decreased patient satisfaction[3]. Consequently, innovative solutions are needed to face this growing challenge.
One proposed innovative model is incorporation of non-physicians, such as nurses, nurse practitioners and physician assistants, into the endoscopy practice and to expand their scope of practice beyond traditional roles. For example, there is some evidence to support non-physicians performing simple endoscopic procedures (e.g. flexible sigmoidoscopy, screening colonoscopy), but such data is limited. Among the scarce literature, non-physicians performing endoscopy has largely focused on flexible sigmoidoscopy for colorectal cancer screening. It is suggested that screening sigmoidoscopies performed by nurses have comparable adverse events and adenoma detection rates to physicians performing the same procedure[4–7]. In contrast, there is significantly less evidence with respect to the performance of colonoscopy and upper endoscopy by non-physicians. This lack of data has resulted in the American Society of Gastrointestinal Endoscopy concluding there was insufficient data to support non-physician endoscopists performing colonoscopy and upper endoscopy[8]. A better knowledge of this practice, including gaps in the literature, will inform areas for future research and inform decision makers on the adoption of such practices.
To this end, our primary study aim was to perform a meta-analysis comparing non-physicians to physicians in the performance of lower endoscopic procedures, including flexible sigmoidoscopy and colonoscopy, with respect to a number of established quality metrics reported for these procedures. A similar secondary aim was to compare non-physicians to physicians in the performance of other endoscopic procedures, namely upper endoscopy.
PATIENTS/MATERIALS AND METHODS
Study population
We performed a systematic review of computerized bibliographic databases on patients who underwent an endoscopic procedure (defined as flexible sigmoidoscopy, colonoscopy or upper endoscopy) that was performed by a non-physician (defined as a nurse, nurse practitioner, or physician assistant) and had selected endoscopic outcome measures reported.
Literature search
We searched computerized bibliography databases including Medline (1950-August 1, 2013), EMBASE (1980- August 1, 2013), and Cochrane Review Library (October 1992 - August 1, 2013). A combination of the following MeSH subject headings and text-words was employed: “nurse,” “nurse practitioner,” “non-physician,” “physician assistant,” “colonoscopy,” “sigmoidoscopy,” “EGD,” “upper endoscopy,” “esophagogastroduodenoscopy,” and “flexible sigmoidoscopy.” The references of all retrieved articles were reviewed in order to identify additional studies. Lastly, a manual search of abstracts submitted to Digestive Disease Week and the American College of Gastroenterology Annual Conference (2001–2013) was performed. Two independent reviewers (L.W.D and D.S.) independently performed the literature search according to above strategy.
Selection criteria
Studies were included if a non-physician performed at least one of the following endoscopic procedures: 1) flexible sigmoidoscopy, 2) colonoscopy, or 3) upper endoscopy and at least one endoscopic quality outcomecould be abstracted. For flexible sigmoidoscopy and colonoscopy these outcomes included 1) polyp detection rate, 2) adenoma detection rate, 3) colorectal cancer detection rate and 4) adverse events. For upper endoscopy outcomes included: 1) esophageal and gastric pyloric intubation rate and 2) adverse events. Articles were limited to randomized controlled trials and cohort studies with no restriction based on language.
Quality assessment of articles
The methodological quality of each included study was assessed by two authors (L.W.D. and D.S.). Observational studies were scored using the Newcastle-Ottawa scale across three categories: selection (maximum 4 points) and comparability (maximum 2 points) of study groups and ascertainment of the outcome of interest (maximum 3 points). Studies with a cumulative score > 7 were considered high quality[9]. The methodological quality of randomized controlled trials was assessed using the Jadad scale which is based on randomization strategy (maximum 2 points), blinding (maximum of 2 points) and withdrawal and dropouts (maximum of 1 point)[10]. If there was a discrepancy between the two reviewers then M.S. reviewed the article and a consensus was then reached among all three authors.
Data abstraction
Data abstraction was divided by procedure type: flexible sigmoidoscopy, colonoscopy and upper endoscopy. Primary data and outcomes collected were determined a priori. For flexible sigmoidoscopy/colonoscopy the following information was abstracted from the full articles for non-physicians and physicians (if available): 1) number of procedures performed, 2) procedure indication, 3) number of polyps detected, 4) number of adenomas detected, 5) number of advanced adenomas detected, 6) detection of colorectal cancer, and 6) number and type of adverse events. For upper endoscopies the following information was abstracted from the full articles for non-physicians and physicians (if available): 1) number of procedures performed, 2) procedure indication, 3) successful intubation of the esophagus and gastric pylorus, 4) detection of ulcer, 5) detection of esophageal or gastric cancer and 6) number and type of adverse events. Detection and number of polyps and ulcers were self-reported by the endoscopists performing the procedure. Adenomas, advanced adenomas, colorectal cancer, and esophageal/gastric cancer had to be confirmed by a pathologist. Adverse events were self-reported and included major adverse events of perforation, post-polypectomy bleeding, cardiopulmonary, post-polypectomy syndrome, and mortality. Secondary data abstracted included flexible sigmoidoscopy depth of insertion, number of successful cecal intubations for colonoscopy, withdrawal time for flexible sigmoidoscopy and colonoscopy, procedure time for flexible sigmoidoscopy, colonoscopy and upper endoscopy, missed adenomas/cancer/ulcer by providers, and willingness of the patient to have a repeat procedure with the same provider. Two authors (L.W.D. and D.S.) independently screened and reviewed all titles, abstracts and full articles for eligibility and abstracted the data. If there was a discrepancy between the two reviewers then M.S. reviewed the article and a consensus was then reached among all three authors.
Statistical analysis
A meta-analysis was performed to compare physicians to non-physicians (which was further stratified to nurses and mid-level providers (nurse practitioners and/or physician assistants)) with respect to several outcomes across procedure type. The first analysis examined non-physicians and physicians performing lower endoscopic procedures. For flexible sigmoidoscopies the following outcomes were compared: 1) polyp detection rate, 2) adenoma detection rate, 3) colorectal cancer detection rate, 4) cumulative adverse event rate, 5) depth of insertion, and 6) procedure time. For colonoscopy the following outcomes were compared: 1) polyp detection rate, 2) adenoma detection rate, 3) colorectal cancer detection rate, 4) cecal intubation rate and 5) cumulative adverse event rate. Additionally, a sensitivity analysis was performed examining the effect of procedure indication (screening versus diagnostic), provider type (nurse versus midlevel provider), and study design (observational versus randomized controlled trial) on outcome measures for flexible sigmoidoscopy. Such a sensitivity analysis was not performed for studies involving colonoscopy given that there were too few studies available (N=3). There were no studies available in the literature that directly compared nurses to mid-level providers in either the performing of flexible sigmoidoscopy or colonoscopy and thus this analysis could not be performed. The second analysis compared non-physicians to physicians in the performing of upper endoscopy. For upper endoscopies the following outcomes were compared: 1) successful esophageal and gastric pyloric intubation rate, 2) cumulative adverse event rate and 3) procedure duration. Also, a similar sensitivity analysis was attempted for studies on upper endoscopies examining the impact of procedure indication, provider type, and study design on outcomes. However, all studies on non-physicians performing upper endoscopies were for diagnostic reasons, performed by nurses and there were too few studies (N=3) stratified by study design in which comparisons could be made. Thus, sensitivity analyses could not be performed on nonphysicians performing upper endoscopy. The primary analyses were performed using the random effects model. Rate ratios (RR) with 95% confidence intervals were calculated for each analysis if sufficient data existed. Of note, not all studies utilized for the rate calculations were included in the meta-analysis given that some studies did not have a physician group with which to make a comparison[5, 11–24].
Heterogeneity was calculated using χ2 with n-1 degrees of freedom, where n represented the number of studies included with a p<0.10 representing significant heterogeneity. Kendall’s Tau was determined and a funnel plot constructed to test for publication bias.
Second, using all studies that satisfied our selection criteria, pooled data for selected outcomes was used to calculate 1) polyp detection rate (percentage of polyps detected per procedure), 2) adenoma detection rate (percentage of adenomas detected per procedure), 3) colorectal cancer detection rate (percentage of colorectal cancers detected per procedure), 4) esophageal/gastric pyloric intubation rate (percentage of successful esophageal and gastric pyloric intubations on upper endoscopies), and cumulative adverse event rate (per 1,000 respective procedures). Calculations were stratified by provider type (nurse and mid-level (defined as nurse practitioner and/or physician assistant)), procedure type, procedure indication, and study design if an appropriate number of studies existed by the stratification method used. The rates and the 95% confidence intervals were calculated using the binomial distribution.
All statistical analyses were calculated using Stata 11.0 (Stata Corp®, College Station, Texas).
RESULTS
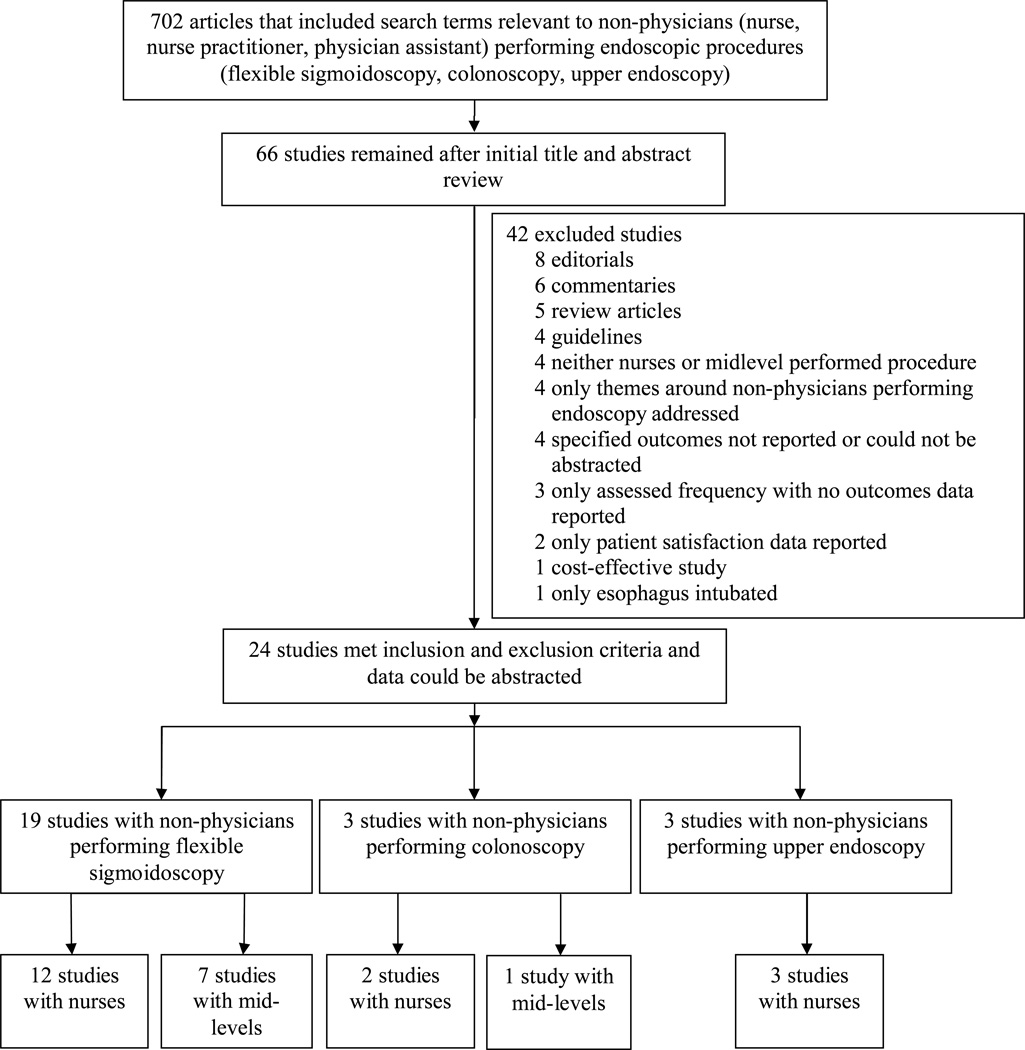
There were 702 studies included in our search with 66 studies selected for initial review. Of this group only 24 studies met our inclusion criteria (Table 1). The most frequent reason for excluding studies was that articles did not report data on non-physicians performing endoscopy, but rather offered a review of the literature or a commentary/editorial on the subject (Figure 1).
Table 1.
Studies included examining patients undergoing flexible sigmoidoscopies, colonoscopies, and upper endoscopies by non-physicians (nurses or mid-level providers). Note: Midlevel includes nurse practitioners and/or physician assistants.
| Study | Year | Design | Setting | Procedure indication (Screening vs. Diagnostic)a |
Provider(s) performing endoscopic procedure(s) |
Endoscopic procedure(s) performed |
Study Qualityb | ||
|---|---|---|---|---|---|---|---|---|---|
| Observational studies | Selection | Comparability | Outcome/Exposure | ||||||
| Spencer | 1977 | Prospective cohort | U.S. | Diagnostic | Nurse | Flexible sigmoidoscopy | ** | *** | |
| Roosevelt | 1984 | Prospective cohort | U.S. | Screening | Mid-level | Flexible sigmoidoscopy | *** | *** | |
| Schroy | 1988 | Prospective cohort | U.S. | Screening | Mid-level | Flexible sigmoidoscopy | *** | *** | |
| Gruber | 1996 | Prospective cohort | U.S. | Screening | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Duthie | 1998 | Prospective cohort | U.K. | Diagnostic | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Schoenfeld, Cash | 1999 | Prospective cohort | U.S. | Screening | Nurse, M.D. | Flexible sigmoidoscopy | **** | ** | *** |
| Wallace | 1999 | Prospective cohort | U.S. | Screening | Mid-level, M.D. | Flexible sigmoidoscopy | **** | ** | *** |
| Arumugam | 2000 | Prospective cohort | U.K. | Diagnostic | Mid-level, M.D. | Flexible sigmoidoscopy | **** | ** | ** |
| Goodfellow | 2003 | Prospective cohort | U.K. | Diagnostic | Mid-level | Flexible sigmoidoscopy | *** | *** | |
| Wu | 2003 | Prospective cohort | U.S. | Screening | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Smale | 2003 | Prospective cohort | U.K. | Diagnostic | Nurse, M.D. | Upper endoscopy | **** | ** | *** |
| Morcom | 2004 | Prospective cohort | Australia | Screening | Mid-level | Flexible sigmoidoscopy | *** | *** | |
| Maruthachalam | 2006 | Prospective cohort | U.K. | Diagnostic | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Dobrow | 2007 | Prospective cohort | Canada | Screening | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Kelly | 2007 | Prospective cohort | U.K. | Diagnostic | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Shapero | 2007 | Cross-sectional | Canada | Screening | Nurse | Flexible sigmoidoscopy | *** | *** | |
| Koornstra | 2009 | Prospective cohort | Netherlands | Diagnostic | Nurse, M.D. | Colonoscopy | **** | ** | ** |
| Redwood | 2009 | Prospective cohort | U.S. | Screening | Mid-level | Flexible sigmoidoscopy | *** | * | |
| Shum | 2010 | Prospective cohort | China | Diagnostic | Nurse | Flexible sigmoidoscopy | ** | *** | |
| van Putten | 2012 | Prospective cohort | Netherlands | Diagnostic | Nurse | Colonoscopy | *** | *** | |
| Randomized controlled trials | Randomized | Double-blind | Withdrawals/Dropouts | ||||||
| Schoenfeld | 1999 | Randomized controlled trial | U.S. | Screening | Nurse, M.D. | Flexible sigmoidoscopy | ** | * | |
| Meaden | 2006 | Randomized controlled trial | U.K. | Diagnostic | Nurse, M.D. | Upper endoscopy | ** | ||
| Williams | 2006 | Randomized controlled trial | U.K. | Diagnostic Diagnostic |
Nurse, M.D. | Flexible sigmoidoscopy Upper endoscopy |
** | ||
| Limoges-Gonzalez | 2011 | Randomized controlled trial | U.S. | Screening | Mid-level, M.D. | Colonoscopy | ** | * | |
Screening procedure refers to screening for colorectal cancer whereas diagnostic refers to procedure indication that was symptom based.
Study quality assessment of observational studies was performed using the Newcastle–Ottawa scale9; for randomized controlled trials, study quality was assessed using the Jadad scale10. Each asterisk represents an individual criterion within the subsection (of the method used to asses study quality) being fulfilled.
Figure 1.
Study flow diagram of the inclusion and exclusion of studies for the systematic review and meta-analysis of patients undergoing endoscopic procedures by non-physicians. Note: some studies had more than one endoscopic procedure performed. There were 9 studies in which non-physicians were compared to physicians with respect to performing an endoscopic procedure (flexible sigmoidoscopy (5 studies), colonoscopy (2 studies), upper endoscopy (3 studies), one study included both flexible sigmoidoscopy and upper endoscopy).
Characteristics of included studies
The greatest number of included studies pertained to non-physicians performing flexible sigmoidoscopy for colorectal cancer screening (57.9%) with the majority of studies having nurses performing sigmoidoscopies. A near equal number of studies reported nurses and mid-levels (nurse practitioner/physician assistant) performing colonoscopy with the majority of the indications for diagnostic purposes. There were three studies that included upper endoscopies, all of these procedures were performed by nurses, and the most frequent procedure indication was dyspepsia. Nearly all endoscopic procedures performed by non-physicians were completed in the outpatient setting regardless of procedure type. There were 9 studies in which non-physicians were directly compared to physicians with respect to performing an endoscopic procedure.
Quality assessment of included studies
The assessment of quality among the included studies varied (Table 1). There were more observational studies than randomized controlled trials included in our systematic review. Among observational studies the mean Newcastle-Ottawa score was 6.4 (median of 6) with only five high quality studies. With respect to randomized controlled trials, the mean and median Jadad score was 2.5 with all studies not being double-blinded or having appropriate blinding present.
Meta-analysis for non-physicians versus physicians performing endoscopic procedures
Lower endoscopic procedures
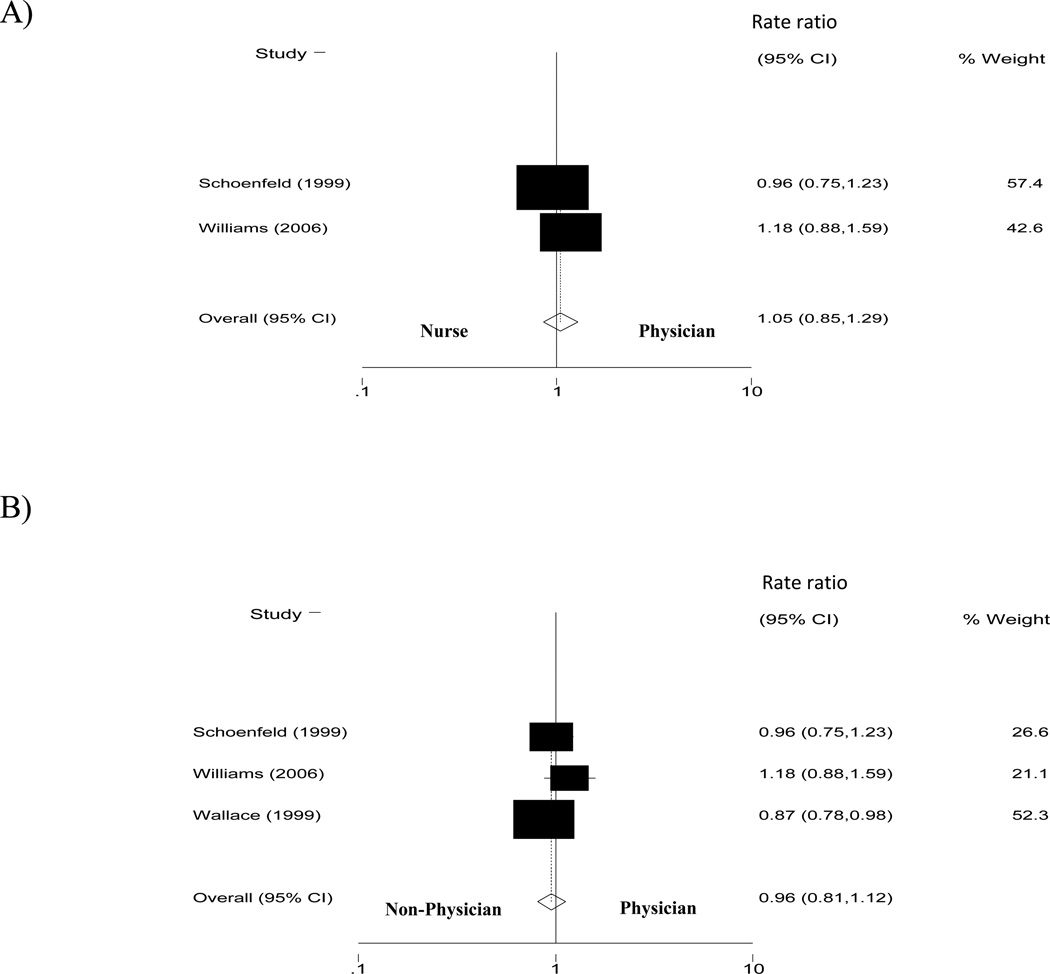
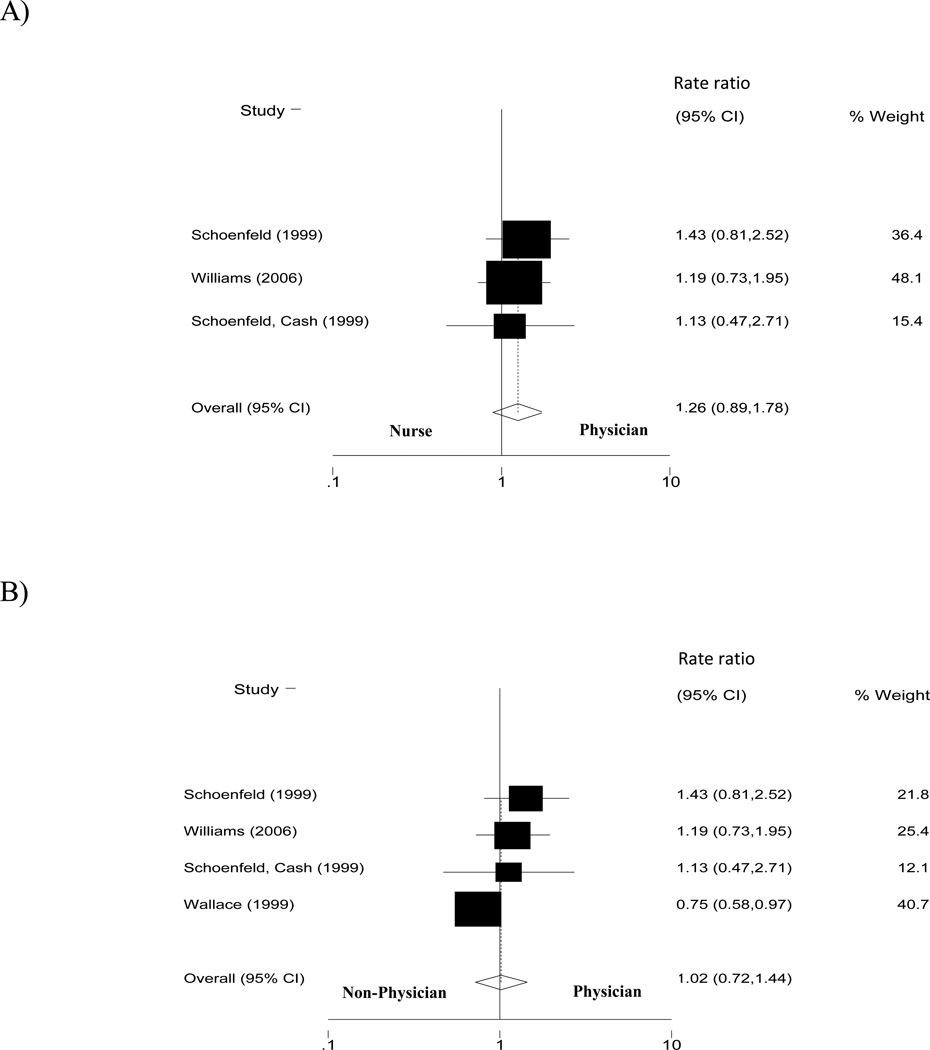
Few studies compared non-physicians to physicians; however, of the limited number of meta-analyses performed, no significant differences were observed between physicians and non-physicians performing endoscopic procedures with respect to pre-specified outcome measures. For example, in studies involving flexible sigmoidoscopy there was no difference between nurses and physicians (RR 1.05, 95% CI 0.85–1.29; p=0.3 for heterogeneity) or non-physicians (combined nurses and mid-levels) and physicians (RR 0.96, 95% CI 0.81–1.12; p=0.2 for heterogeneity) in detecting and removing polyps (Figure 2). Similarly, with regards to adenoma detection rates, no difference was noted between nurses and physicians (RR 1.26, 95% CI 0.89- 1.78; p=0.9 for heterogeneity) or non-physicians and physicians (RR 1.02, 95% CI 0.72–1.44; p=0.1 for heterogeneity) (Figure 3). In addition, both nurses and physicians had similar depth of insertions and total procedure times when performing a flexible sigmoidoscopy. Importantly, the adverse event rate was not significantly different between non-physicians and physicians who performed flexible sigmoidoscopy.
Figure 2.
Rate ratios for the detection and removal of polyps for patients who underwent flexible sigmoidoscopy by non-physicians and physicians (A represents comparison of nurse to physician and B represents comparison of non-physician to physician). Note: Non-physicians include nurses and mid-level providers.
Figure 3.
Adenoma detection rate ratios comparing non-physicians to physicians during flexible sigmoidoscopy (A represents comparison of nurse to physician and B represents comparison of non-physician to physician). Note: Non-physicians include nurses and mid-level providers.
Furthermore, in a sensitivity analysis there were few differences between non-physicians and physicians with respect to sigmoidoscopy outcomes when studies were stratified by procedure indication and study design. With regards to screening versus non-screening flexible sigmoidoscopy, there was no difference between non-physicians and physicians in adenoma detection rates (RR=0.99, 95% CI 0.63–1.56; p=0.1 for heterogeneity). Interestingly, physicians performing screening flexible sigmoidoscopy had a slightly lower polyp detection rate than nonphysicians (RR=0.89, 95% CI 0.80–0.99; p=0.5 for heterogeneity). When restricting studies to randomized controlled trials of screening flexible sigmoidoscopies there was no difference between mid-levels and physicians in polyp detection rates (RR=1.05, 95% CI 0.85–1.29; p=0.3 for heterogeneity).
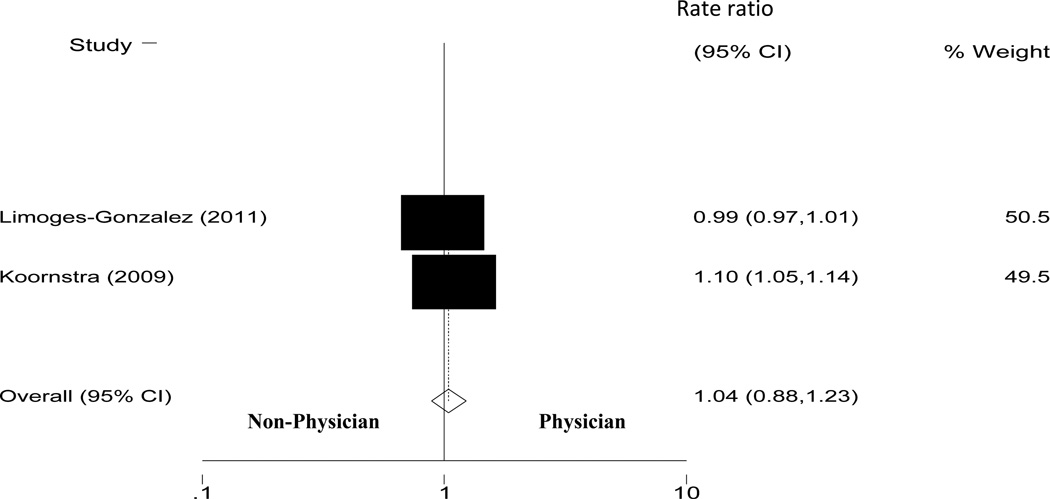
Among studies that involved colonoscopy there was insufficient data to perform meta-analyses comparing non-physicians to physicians with regards to polyp detection rate, adenoma detection rate, colorectal cancer detection rate or adverse event rate; however there was no difference between non-physicians and physicians in cecal intubation rates (RR 1.04, 95% CI 0.88–1.23; p < 0.001 for heterogeneity) (Figure 4).
Figure 4.
Cecal intubation rate ratio comparing non-physicians to physicians during colonoscopy. Note: Non-physicians include nurses and mid-level providers.
Upper endoscopic procedures
No significant differences were noted between nurses and physicians in performing upper endoscopy in our meta-analyses. There was no difference between nurses and physicians in the successful completion of an upper endoscopy (RR 1.00, 95% CI 0.99–1.01, p=0.1 for heterogeneity) as well as total procedure duration did not differ between nurses and physicians. No adverse events were observed in both nurses and physicians who performed upper endoscopy.
Graphical inspection of the Begg’s funnel plot and statistical analysis showed no evidence of significant publication bias for studies included in the meta-analyses.
Systematic review of outcomes for non-physicians performing endoscopic procedures
Lower endoscopic procedures
Table 2 summarizes the rates for specific endoscopic outcomes with respect to procedure and provider type. There were a total of 19 studies with non-physicians performing flexible sigmoidoscopy; 7 studies[5, 13, 17–19, 25, 26] involving mid-levels performing 3,976 flexible sigmoidoscopies and 12 studies[4, 11, 12, 14–16, 20–22, 24, 27, 28] with nurses performing 14, 886 flexible sigmoidoscopies. Among mid-levels performing flexible sigmoidoscopies (N=7), the polyp detection rate was 23.7% (95% CI 22.4–25.1%). The adenoma detection rate for this group was 7.2% (95% CI 6.4–8.2%) with a colorectal cancer detection rate of 1.2% (95% CI 0.7- 1.8%). There were no reported adverse events in mid-levels performing flexible sigmoidoscopy. Mid-levels had a mean insertion depth of 49.1 ± 8.3 cm.
Table 2.
Rates for selected outcomes of endoscopic procedures stratified by type of provider and endoscopic procedure.
| Event/Procedures | Incidence rate % (95% CI) | |
|---|---|---|
| Flexible sigmoidoscopy | ||
| Mid-level | ||
| Polyp[5, 13, 18, 19, 26] | 916/3,865 | 23.7 (22.4–25.1) |
| Adenoma[17, 19, 26] | 235/3,248 | 7.2 (6.4–8.2) |
| Advanced adenoma[19] | 14/825 | 1.7 (0.9–2.8) |
| Colorectal cancer[5, 13, 17, 19, 25] | 18/1,556 | 1.2 (0.7–1.8) |
| Adverse events[5, 13, 17–19, 25, 26] | 0/3,976 | 0 (0–0.09) |
| Number of missed adenomas[5] | 8/100 | 8.0 (3.5–15.2) |
| Patient willing to undergo a repeat procedure by provider[17] | 99/100 | 99.0 (94.6–100.0) |
| Nurse | ||
| Polyp[4, 11, 12, 14–16, 20–22, 24, 27, 28] | 1,432/14,473 | 9.9 (9.4–10.4) |
| Adenoma[4, 11, 12, 14, 20, 22, 24, 27, 28] | 282/9,809 | 2.9 (2.6–3.2) |
| Advanced adenoma[11, 12, 20, 22, 24, 28] | 117/9,444 | 1.2 (1.0–1.5) |
| Colorectal cancer[4, 11, 12, 14–16, 20–22, 24, 28] | 185/14,772 | 1.3 (1.1–1.4) |
| Adverse events[4, 11, 12, 14–16, 20–22, 24, 27, 28] | 4/14,886 | 0.03 (0.007–0.07) |
| Number of missed adenomas[4] | 3/151 | 2.0 (0.4–5.7) |
| Colonoscopy | ||
| Nurse | ||
| Adenoma[23, 29] | 337/1,300 | 25.9 (23.6–28.4) |
| Adverse events[23, 29] | 3/1,300 | 0.2 (0.05–0.7) |
| Cecal intubation[23, 29] | 1,212/1,300 | 93.2 (91.7–94.5) |
| Patient willing to undergo a repeat procedure by provider[29] | 298/300 | 99.3 (97.6–100) |
| Non-physicians | ||
| Adenoma[23, 29, 30] | 357/1,350 | 26.4 (24.1–28.9) |
| Colorectal cancer[29, 30] | 2/350 | 0.6 (0.07–2.0) |
| Adverse events[23, 29, 30] | 3/1,350 | 0.2 (0.05–0.6) |
| Cecal intubation[23, 29, 30] | 1,262/1,350 | 93.5 (92.0–94.7) |
| Patient willing to undergo a repeat procedure by provider[29, 30] | 347/350 | 99.1 (97.5–99.8) |
| Upper endoscopy | ||
| Nurse | ||
| Successful esophageal and gastric pyloric intubation[28, 32] | 1,921/ 1,932 | 99.4 (99.0–99.7) |
| Esophageal/gastric cancer[28] | 2/445 | 0.4 (0.005–1.6) |
| Ulcer[28] | 15/445 | 3.4 (1.9–5.5) |
| Adverse events[28, 31, 32] | 0/2,122 | 0 (0–0.2) |
| Missed lesions[31] | 1/190 | 0.5 (0.01–2.9) |
Note: Mid-level includes nurse practitioners and physician assistants and non-physicians include nurses, nurse practitioners, and physician assistants.
On the other hand, nurses performing flexible sigmoidoscopy (N=12) removed 1,432 polyps with a polyp detection rate of 9.9% (95% CI 9.4–10.4%). Adenoma detection rate was 2.9% (95% CI 2.6–3.2%), advanced adenoma detection rate was 1.2% (95% CI 1.0–1.5%) and the colorectal cancer detection rate was 1.3% (95% CI 1.1–1.4%). There were a total of four adverse events reported in this group which included perforation (2), atrial fibrillation (1) and one unknown resulting in an adverse event rate of 0.3/1,000 sigmoidoscopies. Nurses had a mean depth of insertion of 55.2 ± 2.4 cm and a total procedure time of 13.2 ± 7.1 minutes.
Three studies included non-physicians performing colonoscopy with 2 including nurses[23, 29] and 1 with mid-level providers[30]. Among nurses, there was insufficient data to calculate the polyp detection rate, but the adenoma detection rate was 25.9% (95% CI 23.6–28.4%). Three adverse events were reported among nurses performing colonoscopy and included atrial fibrillation (1), perforation (1), and post-polypectomy syndrome (1) yielding an adverse event rate of 2.2/1,000 colonoscopies. Cecal intubation rates among nurses were 93.2% (95% CI 91.7–94.5%). Overall, non-physicians performing colonoscopy had a total procedure time of 21.5 ± 2.6 minutes with a withdrawal time of 9.4 ± 1.2 minutes.
Upper endoscopic procedures
There were three studies[28, 31, 32] that involved non-physicians performing 1,932 upper endoscopies with all of them performed by nurses. Nurses performing upper endoscopies had a successful esophageal and gastric pyloric intubation rate of 99.4% (95% CI 99.0–99.7%). Procedure duration was 14.1 ± 8.4 minutes and there were no reported adverse events.
Impact of procedure indication and study design on outcomes for non-physicians performing flexible sigmoidoscopy
Given the large number of studies in which non-physicians performed flexible sigmoidoscopy we assessed if procedure indication and study design influenced the pooled rates of outcomes for non-physicians performing flexible sigmoidoscopy (Table 3). For procedure indication, the polyp and adenoma detection rates for non-physicians performing screening flexible sigmoidoscopy appeared to be higher than if the sigmoidoscopy was performed for diagnostic purposes. On the other hand, the colorectal cancer detection rate was lower at 0.4% (95% CI 0.3–0.9%) if done for screening compared to 1.5% (95% CI 1.3–1.7%) if the sigmoidoscopy was performed by non-physicians for diagnostic reasons. Lastly, randomized controlled trials (in comparison to observational studies) that examined non-physicians performing flexible sigmoidoscopy had a numerically higher polyp detection rate (19.7% vs. 12.6%) and adenoma detection rate (6.4 % vs. 3.8%). Conversely, it appeared that more colorectal cancers were detected in observational studies by non-physicians performing flexible sigmoidoscopy.
Table 3.
Differences of non-physicians performing flexible sigmoidoscopy with respect to outcome measures stratified by procedure indication and study design.
| Polyp detection rate % (95% CI) |
Adenoma detection rate % (95% CI) |
Colorectal cancer detection rate % (95% CI) |
Adverse event rate (per 1,000 procedures) (95% CI) |
|
|---|---|---|---|---|
| Procedure indication | ||||
| Colorectal screening | ||||
| Non-physiciana | 19.5 (18.5–20.6) | 6.7 (6.1–7.4) | 0.4 (0.3–0.9) | 0.2 (0.04–0.9) |
| Mid-level | 22.9 (21.5–24.4) | 7.2 (6.4–8.2) | 0.3 (0.06–0.9) | 0 (0–1.0) |
| Nurse | 14.8 (13.5–16.3) | 6.1 (5.2–7.1) | 0.4 (0.2–0.7) | 0.4 (0.09–2.1) |
| Diagnostic | ||||
| Non-physician | 9.7 (9.1–10.2) | 1.6 (1.4–2.0) | 1.5 (1.3–1.7) | 0.2 (0.05–0.7) |
| Mid-level | 43.3 (37.4–49.3) | --- | 3.6 (2.1–5.9) | 0 (0–8.9) |
| Nurse | 8.9 (8.4–9.4) | 1.6 (1.4–2.0) | 1.4 (1.2–1.7) | 0.2 (0.05–0.7) |
| Study design | ||||
| Observational | ||||
| Non-physician | 12.6 (12.1–13.1) | 3.8 (3.5–4.2) | 1.3 (1.1–1.5) | 0.2 (0.03–0.5) |
| Mid-level | 24.5 (23.1–25.9) | 7.2 (6.4–8.2) | 1.3 (0.7–2.0) | 0 (0–0.9) |
| Nurse | 9.4 (8.9–9.9) | 2.6 (2.3–2.9) | 1.3 (1.1–1.5) | 0.2 (0.04–0.6) |
| Randomized controlled trial | ||||
| Non-physician | 19.7 (16.9–22.8) | 6.4 (4.8–8.5) | 1.0 (0.4–2.0) | 1.4 (0.03–7.6) |
| Mid-level | --- | --- | --- | --- |
| Nurse | 19.7 (16.9–22.8) | 6.4 (4.8–8.5) | 1.0 (0.4–2.0) | 1.4 (0.03–7.6) |
Non-physician includes mid-level and nurse providers.
DISCUSSION
With the rapidly growing demand for endoscopic procedures for colorectal cancer screening and diagnostic purposes, innovative methods in health services may need to be considered, especially in high demand settings. One such intervention is the education, training and supervision of nonphysicians to perform endoscopic procedures. Our systematic review and meta-analysis provide data to support the notion that physician and non-physician providers can provide similar quality GI endoscopic procedures, although the data are limited. The largest body of literature on this topic surrounded nurses and mid-level providers performing flexible sigmoidoscopies with non-physicians achieving similar endoscopic quality measures as physicians. While fewer data was available for colonoscopies and upper endoscopies, similar efficacy and safety between nonphysicians and physicians was evident. This data is important in that it may support the incorporation of non-physicians alongside physicians to provide endoscopic services.
Our study raises a number of questions on the topic of non-physicians performing simple endoscopic procedures. The first question that arises: Is there a need for non-physicians to perform simple endoscopic procedures? One of the greatest sources of endoscopic demand hails from indications for colorectal cancer screening and surveillance. Both colonoscopy and flexible sigmoidoscopy are accepted and recommended modalities for colorectal cancer screening[33], yet with the aging population it is estimated that the number of endoscopic procedures that would be required to meet this demand far exceeds the supply of available gastroenterologists[34, 35]. This inequity could lead to impaired access, delayed diagnoses, higher healthcare costs and overall poorer patient satisfaction[1, 3]. Given this demand-supply mismatch some have called for the further training of non-physicians to perform screening endoscopies[36]. Our data supports that non-physicians are a suitable adjunctive to physicians performing simple endoscopic procedures to meet this rising demand.
A second question is whether patients and physicians accept non-physicians performing simple endoscopic procedures. Available data with regards to patient satisfaction is sparse in this area; however limited reports illustrate that patients would be willing to undergo a repeat procedure by a non-physician and that no difference exists between non-physicians and physicians in terms of patient preference for who performs their procedure. In our included studies, there was high patient satisfaction with respect to non-physicians performing flexible sigmoidoscopy[17, 27], colonoscopy[29, 30] and upper endoscopy[32] and in many cases there was greater patient satisfaction and lower pain scores with non-physicians performing endoscopy. At the same time, a number of academic centers and healthcare organizations have adopted the use of nonphysicians to perform simple endoscopic procedures[17, 30, 37–39] with successful outcomes and patient experiences. Lastly, the use of non-physicians in traditionally physician roles is not a new concept in medicine. A large number of medical fields have adopted the use of nonphysicians for clinical practice[40–43]. For example, the use of certified nurse anesthetists to deliver anesthesia care has been prevalent for over a century. Nurse anesthetists have consistently demonstrated efficacy and safety with high provider satisfaction and acceptance[44]. Consequently, expanding the role of non-physicians into endoscopy would not limit the role of gastroenterologists, but rather allow them to increase services and access and further allow gastroenterologists to focus their attention on more complex and demanding procedures/cases.
A third and final question that arises: Are there differences in outcomes between the various types of providers who can perform simple endoscopic procedures? While adverse events, colorectal cancer detection and advanced adenoma detection rates were similar between nurses and mid-level providers in our study, our pooled data also showed that mid-levels detected and removed more polyps and adenomas during flexible sigmoidoscopy as compared to nurses (23.7% vs. 9.9% and 7.2% vs. 2.9% respectively). A number of reasons may have explained these observations. For example, the education and training that mid-levels receive compared to nurses differs, polyps may not have been removed during a flexible sigmoidoscopy in some of the studies given that if a polyp were found then the patient would have been referred for a colonoscopy which may have resulted in underreporting of polyps, and there were much fewer studies available on mid-levels performing sigmoidoscopy that could have potentially led to an overestimation of polyp and adenoma detection rates. Unfortunately, no meta-analyses could be performed comparing these two provider groups given that to date no study has directly compared the two providers together in the performance of an endoscopic procedure. However, our indirect data does raise interesting issues such as the education and training that is required of non-physicians to perform endoscopy as well as the type of non-physician that could be utilized in this role.
There are important limitations to our study. First, there were few studies available in which meta-analyses could be performed with respect to specific endoscopic procedures, particularly with colonoscopy and upper endoscopy, thereby limiting the generalizability of our results. Second, only a limited number of endoscopic quality outcome measures could be evaluated, such as adenoma detection rate and adverse events, yet these have been universally accepted in the GI literature as measurements of quality[45]. Future studies that incorporate withdrawal time, patient satisfaction, minor adverse events such as pain, and amount of sedation required need to be performed. Third, some of the authors of this study have published on non-physicians performing endoscopic procedures[30] and have implemented such programs at their institutions which may have introduced a component of publication bias into the literature; however there was no evidence of publication bias by either funnel plot inspection or statistical analysis of the studies included in the meta-analyses. Fourth, non-physicians may have been assigned low-risk patients in many of the included studies which could explain the low number of adverse events reported and overall favorable outcomes for non-physicians compared to physicians in our analysis. On this issue, with respect to upper endoscopies, nearly all of the included studies were randomized controlled trials (2 of 3) which helped to minimize selection bias of included patients. For studies involving flexible sigmoidoscopy and colonoscopy far fewer randomized controlled trials were available. However, examining the endoscopic outcomes (adenoma, advanced adenoma, colorectal cancer detection and adverse event rates) for non-physicians performing flexible sigmoidoscopy and colonoscopy we discovered that these outcomes for nonphysicians were in line with published data on physicians[45–51] suggesting that the patients included in our studies were very likely similar to the patients included in other studies involving physicians performing endoscopy. Finally, minimal data was available on the optimal method used to train non-physicians, but data suggests it may be comparable to the number of procedures that one performs with direct supervision, akin to the same training advocated for GI trainees[52].
In summary, we found that non-physicians can safely perform endoscopic procedures with similar quality, especially with respect to screening flexible sigmoidoscopy. Far fewer data was reported for non-physicians performing colonoscopy and upper endoscopy, but among this data non-physicians perform both procedures within accepted national benchmarks for quality measures used in endoscopy. Our data supports continued discussion on incorporating and augmenting GI practices with expanding the role of non-physicians to assist with the high volume of endoscopic procedures. Importantly, continued research is required to determine optimal teaching methods and patient acceptance of this practice and to begin the development of standard guidelines for the scope of practice for non-physicians performing endoscopy.
Acknowledgments
Funding: This work was supported by grants from the National Cancer Institute K23 CA157929 (MS). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Lukejohn Day (conception and design; analysis and interpretation of data of the article; critical revision of the article for important intellectual content; final approval of the article)
Derrick Siao (analysis and interpretation of data of the article, critical revision of the article for important intellectual content; final approval of the article)
John Inadomi (critical revision of the article for important intellectual content; final approval of the article)
Ma Somsouk (conception and design; analysis and interpretation of data of the article; critical revision of the article for important intellectual content; final approval of the article)
Conflicts of interest: None
REFERENCES
- 1.Vijan S, Inadomi J, Hayward RA, Hofer TP, Fendrick AM. Projections of demand and capacity for colonoscopy related to increasing rates of colorectal cancer screening in the United States. Aliment Pharmacol Ther. 2004;20(5):507–515. doi: 10.1111/j.1365-2036.2004.01960.x. [DOI] [PubMed] [Google Scholar]
- 2.Elta GH. GI training: where are we headed? Am J Gastroenterol. 2011;106(3):395–397. doi: 10.1038/ajg.2010.416. [DOI] [PubMed] [Google Scholar]
- 3.Leek RD, Landers RJ, Harris AL, Lewis CE. Necrosis correlates with high vascular density and focal macrophage infiltration in invasive carcinoma of the breast. Br J Cancer. 1999;79(5–6):991–995. doi: 10.1038/sj.bjc.6690158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoenfeld P, Lipscomb S, Crook J, Dominguez J, Butler J, Holmes L, Cruess D, Rex D. Accuracy of polyp detection by gastroenterologists and nurse endoscopists during flexible sigmoidoscopy: a randomized trial. Gastroenterology. 1999;117(2):312–318. doi: 10.1053/gast.1999.0029900312. [DOI] [PubMed] [Google Scholar]
- 5.Schroy PC, Wiggins T, Winawer SJ, Diaz B, Lightdale CJ. Video endoscopy by nurse practitioners: a model for colorectal cancer screening. Gastrointest Endosc. 1988;34(5):390–394. doi: 10.1016/s0016-5107(88)71402-9. [DOI] [PubMed] [Google Scholar]
- 6.Maule WF. Screening for colorectal cancer by nurse endoscopists. N Engl J Med. 1994;330(3):183–187. doi: 10.1056/NEJM199401203300307. [DOI] [PubMed] [Google Scholar]
- 7.DiSario JA, Sanowski RA. Sigmoidoscopy training for nurses and resident physicians. Gastrointest Endosc. 1993;39(1):29–32. doi: 10.1016/s0016-5107(93)70006-1. [DOI] [PubMed] [Google Scholar]
- 8.Ikenberry SO, Anderson MA, Banerjee S, Baron TH, Dominitz JA, Gan SI, Harrison ME, Jagannath S, Levy M, Lichtenstein D, et al. Endoscopy by nonphysicians. Gastrointest Endosc. 2009;69(4):767–770. doi: 10.1016/j.gie.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Wells GA, SB OCD, Petersen J, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Google Scholar]
- 10.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 11.Dobrow MJ, Cooper MA, Gayman K, Pennington J, Matthews J, Rabeneck L. Referring patients to nurses: outcomes and evaluation of a nurse flexible sigmoidoscopy training program for colorectal cancer screening. Can J Gastroenterol. 2007;21(5):301–308. doi: 10.1155/2007/719634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duthie GS, Drew PJ, Hughes MA, Farouk R, Hodson R, Wedgwood KR, Monson JR. A UK training programme for nurse practitioner flexible sigmoidoscopy and a prospective evaluation of the practice of the first UK trained nurse flexible sigmoidoscopist. Gut. 1998;43(5):711–714. doi: 10.1136/gut.43.5.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodfellow PB, Fretwell IA, Simms JM. Nurse endoscopy in a district general hospital. Ann R Coll Surg Engl. 2003;85(3):181–184. doi: 10.1308/003588403321661343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gruber M. Performance of flexible sigmoidoscopy by a clinical nurse specialist. Gastroenterol Nurs. 1996;19(3):105–108. doi: 10.1097/00001610-199605000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Kelly SB, Murphy J, Smith A, Watson H, Gibb S, Walker C, Reddy R. Nurse specialist led flexible sigmoidoscopy in an outpatient setting. Colorectal Dis. 2008;10(4):390–393. doi: 10.1111/j.1463-1318.2007.01271.x. [DOI] [PubMed] [Google Scholar]
- 16.Maruthachalam K, Stoker E, Nicholson G, Horgan AF. Nurse led flexible sigmoidoscopy in primary care--the first thousand patients. Colorectal Dis. 2006;8(7):557–562. doi: 10.1111/j.1463-1318.2006.00973.x. [DOI] [PubMed] [Google Scholar]
- 17.Morcom J, Dunn SV, Luxford Y. Establishing an Australian nurse practitioner-led colorectal cancer screening clinic. Gastroenterol Nurs. 2005;28(1):33–42. doi: 10.1097/00001610-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Redwood D, Joseph DA, Christensen C, Provost E, Peterson VL, Espey D, Sacco F. Development of a flexible sigmoidoscopy training program for rural nurse practitioners and physician assistants to increase colorectal cancer screening among Alaska Native people. J Health Care Poor Underserved. 2009;20(4):1041–1048. doi: 10.1353/hpu.0.0223. [DOI] [PubMed] [Google Scholar]
- 19.Rosevelt J, Frankl H. Colorectal cancer screening by nurse practitioner using 60-cm flexible fiberoptic sigmoidoscope. Dig Dis Sci. 1984;29(2):161–163. doi: 10.1007/BF01317059. [DOI] [PubMed] [Google Scholar]
- 20.Shapero TF, Hoover J, Paszat LF, Burgis E, Hsieh E, Rothwell DM, Rabeneck L. Colorectal cancer screening with nurse-performed flexible sigmoidoscopy: results from a Canadian community-based program. Gastrointest Endosc. 2007;65(4):640–645. doi: 10.1016/j.gie.2006.06.037. [DOI] [PubMed] [Google Scholar]
- 21.Shum NF, Lui YL, Choi HK, Lau SC, Ho JW. A comprehensive training programme for nurse endoscopist performing flexible sigmoidoscopy in Hong Kong. J Clin Nurs. 2010;19(13–14):1891–1896. doi: 10.1111/j.1365-2702.2009.03093.x. [DOI] [PubMed] [Google Scholar]
- 22.Spencer RJ, Ready RL. Utilization of nurse endoscopists for sigmoidoscopic examinations. Dis Colon Rectum. 1977;20(2):94–96. doi: 10.1007/BF02587321. [DOI] [PubMed] [Google Scholar]
- 23.van Putten PG, Ter Borg F, Adang RP, Koornstra JJ, Romberg-Camps MJ, Timmer R, Poen AC, Kuipers EJ, Van Leerdam ME. Nurse endoscopists perform colonoscopies according to the international standard and with high patient satisfaction. Endoscopy. 2012;44(12):1127–1132. doi: 10.1055/s-0032-1310154. [DOI] [PubMed] [Google Scholar]
- 24.Wu K, Titzer D, Soetikno R, Triadafilopoulos G. Use of a colonoscope instead of a sigmoidoscope to screen asymptomatic adults for colorectal cancer. Gastrointest Endosc. 2003;58(5):720–724. doi: 10.1016/s0016-5107(03)02015-7. [DOI] [PubMed] [Google Scholar]
- 25.Arumugam PJ, Rao GN, West J, Foster ME, Haray PN. The impact of open access flexible sigmoidoscopy: a comparison of two services. J R Coll Surg Edinb. 2000;45(6):366–368. [PubMed] [Google Scholar]
- 26.Wallace MB, Kemp JA, Meyer F, Horton K, Reffel A, Christiansen CL, Farraye FA. Screening for colorectal cancer with flexible sigmoidoscopy by nonphysician endoscopists. Am J Med. 1999;107(3):214–218. doi: 10.1016/s0002-9343(99)00225-9. [DOI] [PubMed] [Google Scholar]
- 27.Schoenfeld PS, Cash B, Kita J, Piorkowski M, Cruess D, Ransohoff D. Effectiveness and patient satisfaction with screening flexible sigmoidoscopy performed by registered nurses. Gastrointest Endosc. 1999;49(2):158–162. doi: 10.1016/s0016-5107(99)70480-3. [DOI] [PubMed] [Google Scholar]
- 28.Williams J, Russell I, Durai D, Cheung WY, Farrin A, Bloor K, Coulton S, Richardson G. What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET) Health Technol Assess. 2006;10(40):iii–iv. ix–x, 1–195. doi: 10.3310/hta10400. [DOI] [PubMed] [Google Scholar]
- 29.Koornstra JJ, Corporaal S, Giezen-Beintema WM, de Vries SE, van Dullemen HM. Colonoscopy training for nurse endoscopists: a feasibility study. Gastrointest Endosc. 2009;69(3 Pt 2):688–695. doi: 10.1016/j.gie.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 30.Limoges-Gonzalez M, Mann NS, Al-Juburi A, Tseng D, Inadomi J, Rossaro L. Comparisons of screening colonoscopy performed by a nurse practitioner and gastroenterologists: a single-center randomized controlled trial. Gastroenterol Nurs. 2011;34(3):210–216. doi: 10.1097/SGA.0b013e31821ab5e6. [DOI] [PubMed] [Google Scholar]
- 31.Meaden C, Joshi M, Hollis S, Higham A, Lynch D. A randomized controlled trial comparing the accuracy of general diagnostic upper gastrointestinal endoscopy performed by nurse or medical endoscopists. Endoscopy. 2006;38(6):553–560. doi: 10.1055/s-2006-925164. [DOI] [PubMed] [Google Scholar]
- 32.Smale S, Bjarnason I, Forgacs I, Prasad P, Mukhood M, Wong M, Ng A, Mulcahy HE. Upper gastrointestinal endoscopy performed by nurses: scope for the future? Gut. 2003;52(8):1090–1094. doi: 10.1136/gut.52.8.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 34.Ladabaum U, Song K. Projected national impact of colorectal cancer screening on clinical and economic outcomes and health services demand. Gastroenterology. 2005;129(4):1151–1162. doi: 10.1053/j.gastro.2005.07.059. [DOI] [PubMed] [Google Scholar]
- 35.Wendt E. Screening for colorectal cancer. N Engl J Med. 2001;345(25):1851. author reply 1852. [PubMed] [Google Scholar]
- 36.Steinwachs D, Allen JD, Barlow WE, Duncan RP, Egede LE, Friedman LS, Keating NL, Kim P, Lave JR, Laveist TA, et al. National Institutes of Health state-of-the-science conference statement: Enhancing use and quality of colorectal cancer screening. Ann Intern Med. 2010;152(10):663–667. doi: 10.7326/0003-4819-152-10-201005180-00237. [DOI] [PubMed] [Google Scholar]
- 37.Hutfless S, Kalloo AN. Screening colonoscopy: a new frontier for nurse practitioners. Clin Gastroenterol Hepatol. 2013;11(2):106–108. doi: 10.1016/j.cgh.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Lieberman DA, Ghormley JM. Physician assistants in gastroenterology: should they perform endoscopy? Am J Gastroenterol. 1992;87(8):940–943. [PubMed] [Google Scholar]
- 39.Gossman ER. Endoscopy by nonphysicians. Can J Gastroenterol. 2007;21(1):17–18. doi: 10.1155/2007/258760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferraro KF, Southerland T. Domains of medical practice: physicians' assessment of the role of physician extenders. J Health Soc Behav. 1989;30(2):192–205. [PubMed] [Google Scholar]
- 41.Norris B, Harris T, Stringer S. Effective use of physician extenders in an outpatient otolaryngology setting. Laryngoscope. 2011;121(11):2317–2321. doi: 10.1002/lary.22192. [DOI] [PubMed] [Google Scholar]
- 42.Burgess SE, Pruitt RH, Maybee P, Metz AE, Jr, Leuner J. Rural and urban physicians' perceptions regarding the role and practice of the nurse practitioner, physician assistant, and certified nurse midwife. J Rural Health. 2003;19(Suppl):321–328. doi: 10.1111/j.1748-0361.2003.tb01051.x. [DOI] [PubMed] [Google Scholar]
- 43.Mathur M, Rampersad A, Howard K, Goldman GM. Physician assistants as physician extenders in the pediatric intensive care unit setting-A 5-year experience. Pediatr Crit Care Med. 2005;6(1):14–19. doi: 10.1097/01.PCC.0000149133.50687.A1. [DOI] [PubMed] [Google Scholar]
- 44.Matsusaki T, Sakai T. The role of Certified Registered Nurse Anesthetists in the United States. J Anesth. 2011;25(5):734–740. doi: 10.1007/s00540-011-1193-5. [DOI] [PubMed] [Google Scholar]
- 45.Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2006;63(4 Suppl):S16–S28. doi: 10.1016/j.gie.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 46.Littlejohn C, Hilton S, Macfarlane GJ, Phull P. Systematic review and meta-analysis of the evidence for flexible sigmoidoscopy as a screening method for the prevention of colorectal cancer. Br J Surg. 2012;99(11):1488–1500. doi: 10.1002/bjs.8882. [DOI] [PubMed] [Google Scholar]
- 47.Atkin W, Rogers P, Cardwell C, Cook C, Cuzick J, Wardle J, Edwards R. Wide variation in adenoma detection rates at screening flexible sigmoidoscopy. Gastroenterology. 2004;126(5):1247–1256. doi: 10.1053/j.gastro.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 48.Neale AV, Demers RY, Budev H, Scott RO. Physician accuracy in diagnosing colorectal polyps. Dis Colon Rectum. 1987;30(4):247–250. doi: 10.1007/BF02556164. [DOI] [PubMed] [Google Scholar]
- 49.Rozen P, Ron E, Fireman Z, Hallak A, Grossman A, Baratz M, Rattan J, Gilat T. The relative value of fecal occult blood tests and flexible sigmoidoscopy in screening for large bowel neoplasia. Cancer. 1987;60(10):2553–2558. doi: 10.1002/1097-0142(19871115)60:10<2553::aid-cncr2820601034>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 50.Verne JE, Aubrey R, Love SB, Talbot IC, Northover JM. Population based randomized study of uptake and yield of screening by flexible sigmoidoscopy compared with screening by faecal occult blood testing. BMJ. 1998;317(7152):182–185. doi: 10.1136/bmj.317.7152.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Paillot B, Czernichow P, Michel P, Merle V, Queuniet AM, Duval C, Daubert H. Incidence of rectosigmoid adenomatous polyps in subjects without prior colorectal adenoma or cancer: a prospective cohort study. Gut. 1999;44(3):372–376. doi: 10.1136/gut.44.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wexner SD, Litwin D, Cohen J, Earle D, Ferzli G, Flaherty J, Graham S, Horgan S, Katz BL, Kavic M, et al. Principles of privileging and credentialing for endoscopy and colonoscopy. Gastrointest Endosc. 2002;55(2):145–148. doi: 10.1016/s0016-5107(02)70480-x. [DOI] [PubMed] [Google Scholar]