Abstract
Objective
Hypospadias is usually treated in childhood. Therefore, the natural history of untreated mild hypospadias is unknown. We hypothesized that men with untreated hypospadias, especially mild, do not have adverse outcomes.
Materials
Facebook was used to advertise an electronic survey to men older than 18 years. Men with untreated hypospadias identified themselves and indicated the severity of hypospadias with a series of questions. Outcomes included: Sexual Health Inventory for Men (SHIM), penile curvature and difficulty with intercourse, International Prostate Symptom Score (IPSS), Penile Perception Score (PPS), psychosexual milestones, paternity, infertility, sitting to urinate, and the CDC HRQOL-4 module.
Results
736 men completed self-anatomy questions and 52 (7.1%) self-identified with untreated hypospadias. Untreated hypospadias participants reported worse SHIM (p < 0.001) and IPSS scores (p = 0.05), more ventral penile curvature (p = 0.003) and resulting difficulty with intercourse (p < 0.001), worse satisfaction with meatus (p = 0.011) and penile curvature (p = 0.048), and more sitting to urinate (p = 0.07). When stratified by mild and severe hypospadias, severe hypospadias was associated with more adverse outcomes than mild hypospadias.
Conclusion
Men with untreated hypospadias reported worse outcomes compared with non-hypospadiac men. Mild untreated hypospadias had fewer adverse outcomes than severe hypospadias. Research is needed to determine if treatment of childhood hypospadias improves outcomes in adults, especially for mild hypospadias.
Keywords: Hypospadias, Penile curvature, Chordee
Introduction
Hypospadias is a congenital penile abnormality repaired surgically, usually in childhood [1,2]. Hypospadias is defined as an abnormal proximal location of the urethral meatus on the ventral penis and often includes ventral foreskin deficiency and ventral penile curvature [1,2]. Hypospadias has varying degrees of severity from mild where the meatus is near the tip of penis with minimal or no curvature, to severe cases with the meatus near the peno-scrotal junction with marked curvature [3,4]. In general, the more severe the hypospadias the less common it is [5]. Reasons given to parents for treating hypospadias include splaying of urinary stream or other bothersome urinary symptoms, difficulty with sperm deposition leading to infertility, ventral curvature leading to difficulty with intercourse, and decreased satisfaction with penile appearance which may lead to delayed sexual development. The degree to which these potential concerns become actual issues in men with untreated hypospadias likely depends on the severity of the abnormalities, but the natural history of untreated hypospadias is not well defined [6].
There are occasional adult patients who present to urologists for unrelated issues and are found to have untreated hypospadias, usually mild. These patients often do not know that they have an abnormality, have fathered children, report no sexual difficulties, and stand to urinate without difficulty. Regarding the prevalence of untreated hypospadias in adults, two studies examined 500 and 1244 adult males, respectively, and reported the prevalence of the meatus located on the proximal one-third of the glans or further proximal as 13% and 0.2%, respectively [7,8]. A study in children reported the prevalence of untreated hypospadias as 0.6% [9]. Regarding complications of untreated mild hypospadias, one study identified 56 adult males with untreated mild hypospadias [6]. Of the 56 patients, only one presented with a chief complaint related to hypospadias, 5% expressed dissatisfaction with the appearance of their penis, 32% were unaware they had an abnormality, 5% patients reported sitting to void preferentially, and 95% of the men who attempted fertility were successful. In another study, none of 65 men with untreated hypospadias reported problems with sexual intercourse or preferentially standing to urinate [8]. These studies suggest that untreated mild hypospadias may have a benign course with a low risk of complications.
Urethroplasty surgery for hypospadias has inherent risks such as meatal stenosis, urethrocutanous fistula, and multiple surgeries [3,10–12]. These complications can be severe and lead to multiple surgeries throughout childhood. This raises the question of why mild forms of hypospadias are treated with urethroplasty when many of these patients will potentially have no complications if left untreated. In addition, with lack of data on the long-term consequences of treating or not treating the mild hypospadias, parents cannot be properly counseled.
Given the low prevalence of untreated hypospadias in adults, one way to recruit enough subjects to have a meaningful study would be by developing an effective advertisement method that can reach hundreds of thousands of adult males. According to statistics on Facebook; there are close to 225 million active users in the USA, and 50% of the users log onto their Facebook account at least once a day [13]. Advertising on social media is a potentially powerful method to advertise clinical research surveys that need a large number of subjects or to find subjects with rare diseases or conditions to participate in clinical research and has been used successfully in the past [14–19].
We hypothesized that men with untreated mild hypospadias would have similar outcomes to normal men in terms of penile satisfaction, sexual health, bother from penile curvature, urination symptoms, paternity, frequency of sitting to urinate, and health related quality of life (HRQOL). To test this hypothesis, we performed a pilot survey study using a targeted advertising campaign on Facebook.
Methods
Survey
Following Institutional Review Board approval, study data were collected over a 4-month period (October 2012–January 2013) and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at University of California San Francisco and described previously [20].
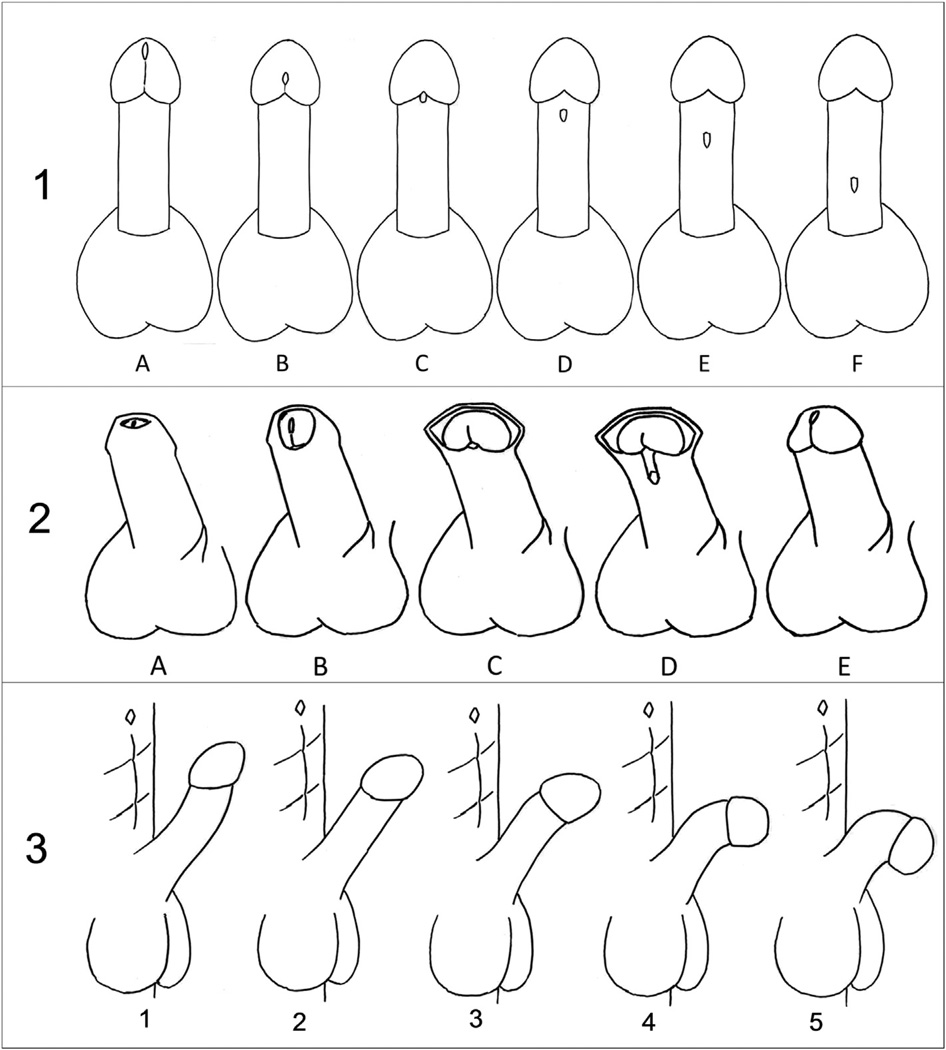
The predictor was whether or not a participant self-identified as having possible untreated hypospadias and the severity of hypospadias based on answers to self-reported anatomy questions supplemented with penile sketches (Fig. 1). Outcomes included the Penile Perception Score (PPS) [21], the sexual health inventory for men (SHIM) score [22–24], the International Prostate Symptom Score (IPSS) [25,26], CDC Healthy Days Core Module (CDC HRQOL-4) [27], paternity status, history of infertility diagnosis or treatment, frequency of sitting to urinate modeled after IPSS questions, penile curvature based on sketches of curvature (Fig. 1), reported degree of difficulty with intercourse from penile curvature modeled after SHIM questions, and sexual milestones attained and age when attained. The survey is shown in Appendix A.
Figure 1.
Sketches used for participants to report anatomy. Question 1: Which of the above sketches is most like where your urethral opening is located? The urethral opening is where urine exits when you urinate. Choose the best answer (A–F). Question 2: Which of the above sketches is most like the appearance of your penis and foreskin? Choose the best answer (A–E). Question 3: Which of the above sketches is most like the curvature of your penis when you have an erection (penis gets hard)? We are only asking about up/down curvature not left/right curvature. Choose the best answer (1–5).
Pretesting
Because our target population is rare, a proxy measure for the criterion validity of the self-reported anatomy questions was used. Questions were pretested on 26 subjects without hypospadias that included 22 males and four females. Subjects took an online survey that showed a series of penis images with varying anatomy from normal to severe hypospadias. The subjects were asked to pick the sketch that best depicted the anatomy in question in the picture. Results are summarized in Appendix B.
The urethral meatus question had a sensitivity of 100% and specificity of 100% for detecting hypospadias. Pretest subjects’ answers to five foreskin/glans appearance questions were able to identify normal circumcised or normal uncircumcised penises with a 100% sensitivity and specificity and hypospadias was identified by the instrument with a sensitivity of 77–100% and specificity of 100%. Pretest subjects’ answers to five penile curvature questions had 100% sensitivity and between 96% and 100% specificity in detecting ventral curvature.
The criterion validity of the self-reported anatomy questions was tested in our survey population by asking participants to upload an image of their penis that demonstrated relevant anatomy. The goal was to have 5% of men upload an image and then compare the participants self-reported anatomy to the consensus opinion of two pediatric urologists.
Identification of untreated hypospadias
Participants were considered to have possible untreated hypospadias if they chose a meatus location at the proximal one-third of the glans or more proximal (B–F on question 1 in Fig. 1) or if they chose a foreskin/penis appearance that corresponded to hypospadias (C or D on question 2 in Fig. 1). Participants were considered to have possible mild untreated hypospadias if they answered B or C on question 1 or C on question 2 (Fig. 1). Participants were considered to have possible severe untreated hypospadias if they answered D, E, or F on question 1 or D on question 2 (Fig. 1). Severe untreated hypospadias was assigned if the participant answered one question consistent with mild hypospadias and one question consistent with severe hypospadias.
Statistical analysis
Outcomes in participants with possible untreated hypospadias were compared with those of non-hypospadiac men. All participants with possible untreated hypospadias were compared with normal and then participants were compared with normal by severity as defined above. Continuous outcomes were compared by student’s t-test, ordinal outcomes were compared by Wilcoxon rank sum test, and dichotomous by chi-square test or Fisher Exact test. Stata 12 (College Station, TX, USA) was used for all analysis and α of 0.05 chosen for significance.
Results
Participants
Of the men who started the survey (1075), 736 completed questions regarding self-anatomy (Table 1). Of those 736 participants, 52 (7.1%) self-identified as having possible untreated hypospadias. Participants with possible untreated hypospadias were less likely to report being circumcised (64 vs. 80%, p = 0.006), being born in USA (85 vs. 91%, p = 0.1) and being born in a hospital (80 vs. 93%, p = 0.001).
Table 1.
Patient characteristics.
| All (N = 736) | No hypospadias (N = 684) | Possible untreated hypospadias (N = 52) | pa | |
|---|---|---|---|---|
| Race | ||||
| White (Caucasian) | 621 (84.4%) | 580 (84.8%) | 41 (78.9%) | 0.3 |
| Black | 25 (3.4%) | 22 (3.2%) | 3 (5.8%) | |
| Asian | 15 (2.0%) | 14(2.1%) | 1 (1.9%) | |
| Pacific Islander | 3 (0.4%) | 3 (0.4%) | 0 | |
| Native American | 4 (0.5%) | 3 (0.4%) | 1 (1.9%) | |
| Hispanic or Latino | 32 (4.4%) | 30 (4.4%) | 2 (3.9%) | |
| Other | 21 (2.9%) | 17(2.5%) | 4 (7.7) | |
| No answer | 15 (2.0%) | 15 (2.2%) | 0 | |
| Sexual orientation | 0.7 | |||
| Homosexual | 178 (24.2%) | 167(24.4%) | 11 (21.2%) | |
| Bisexual | 72 (9.8%) | 65 (9.5%) | 7 (13.5%) | |
| Heterosexual | 449 (61.0%) | 416 (60.8%) | 33 (63.5%) | |
| Asexual | 13 (1.8%) | 12 (1.8%) | 1 (1.9%) | |
| Queer | 16 (2.2%) | 16 (2.3%) | 0 | |
| No answer | 8 (1.1%) | 8 (1.2%) | 0 | |
| Age in years (SD) | 43.5 (38.8) | 43.0 (39.9) | 50.1 (20.4) | 0.2 |
| Circumcised | 569/719 (79.1%) | 537/669 (80.3%) | 32/50 (64.0%) | 0.006 |
| Born in USA | 661/731 (90.4%) | 617/679 (90.8%) | 44/52 (84.6%) | 0.1 |
| Born in hospital | 663/717(92.5%) | 622/666 (93.4%) | 41/51 (80.4%) | 0.001 |
Dichotomous and categorical variables compared by chi-square test, continuous variables compared by student’s t-test.
Association of possible untreated hypospadias with outcomes
The association of all men with possible untreated hypospadias and outcomes is reported in Table 2. As a group, all men with possible untreated hypospadias reported worse SHIM scores (17.1 vs. 20.7, p < 0.001) and worse IPSS scores (7.8 vs. 5.9, p = 0.05). They also reported more ventral penile curvature (p = 0.003), were more likely to report that curvature made sexual intercourse difficult (p < 0.001), and had worse satisfaction on the PPS regarding position and shape of urethral meatus (p = 0.011) and penile axis/curvature (p = 0.048). Men with possible untreated hypospadias trended towards more frequent sitting to urinate (p = 0.07). Other measures were not significantly different between groups.
Table 2.
Association of outcomes with possible untreated hypospadias.
| All | Normal | Possible untreated hypospadias |
pa | |
|---|---|---|---|---|
| PPSb | ||||
| Length of penis | 1.9 (0.7) | 1.9 (0.7) | 1.9 (0.7) | 0.9 |
| Position and shape of urethral opening | 2.4 (0.6) | 2.4 (0.6) | 2.2 (0.6) | 0.011 |
| Shape of glans | 2.4 (0.6) | 2.4 (0.6) | 2.3 (0.7) | 0.4 |
| Shape of penile skin | 2.3 (0.6) | 2.3 (0.6) | 2.3 (0.5) | 0.7 |
| Penile axis (curvature) | 2.3 (0.7) | 2.3 (0.7) | 2.0 (0.9) | 0.048 |
| General appearance | 2.2 (0.7) | 2.2 (0.7) | 2.2 (0.7) | 0.9 |
| Overall PPS | 9.4 (2.0) | 9.4 (2.0) | 9.1 (2.0) | 0.3 |
| SHIM score | 20.4 (5.4) | 20.7 (5.3) | 17.1 (6.1) | <0.001 |
| IPSS score | 6.0 (6.2) | 5.9 (6.0) | 7.8 (7.6) | 0.05 |
| CDC HRQOL-4 | ||||
| Would you say your general health isc | 2.5 (1.0) | 2.5 (1.0) | 2.7(1.0) | 0.2 |
| Mean number of physically unhealthy days | 3.6(7.1) | 3.5 (7.0) | 5.1 (8.8) | 0.1 |
| Mean number of mentally unhealthy days | 6.6 (8.8) | 6.5 (8.7) | 8.3 (10.2) | 0.2 |
| Caused a pregnancy | 346/725 (47.7%) | 317/674 (47.0%) | 29/51 (56.7%) | 0.2 |
| Diagnosis of infertility | 24/729 (3.3%) | 22/677 (3.2%) | 2/52 (3.8%) | 0.8 |
| How often to you sit on toilet to just urinate?d | 1.9 (1.2) | 1.9 (1.2) | 2.3 (1.5) | 0.07 |
| Of those who sit to urinate; how much does it bother you to sit down to just urinate?e | 1.4(0.7) | 1.4(0.7) | 1.5 (1.0) | 0.8 |
| Penile curvaturef | 1.9 (0.8) | 1.8 (0.7) | 2.3 (1.1) | 0.003 |
| How difficult does the curvature of your penis make intercourse?g | 4.8 (0.6) | 4.8 (0.6) | 4.4(1.0) | <0.001 |
| Have you ever kissed anyone? | 697/728 (95.7%) | 647/676 (95.7%) | 50/52 (96.2%) | 1.0 |
| Age in years | 14.1 (4.5) | 14.1 (4.5) | 13.8 (3.9) | 0.7 |
| Have you ever been in love? | 642/726 (88.4%) | 595/674 (88.3%) | 47/52 (90.4%) | 0.8 |
| Age in years | 18.1 (6.0) | 18.2 (6.0) | 17.8 (6.4) | 0.7 |
| Have you ever had sexual intercourse? | 643/728 (88.3%) | 598/678 (88.2%) | 45/50 (90.0%) | 0.8 |
| Age in years | 18.3 (5.1) | 18.3 (5.0) | 17.8 (6.3) | 0.5 |
| Have you ever masturbated? | 712/728 (97.8%) | 663/678 (97.8%) | 49/50 (98.0%) | 1.0 |
| Age in years | 12.3 (2.7) | 12.3 (2.7) | 11.7(2.7) | 0.2 |
Data presented as mean (standard deviation) or proportion with “yes” answer.
Continuous outcomes compared by student’s t-test, ordinal by Wilcoxon rank sum test, dichotomous by chi-square or Fisher Exact test.
All questions coded as 3 = very satisfied; 2 = satisfied; 1 = dissatisfied; 0 = very dissatisfied.
1 = excellent; 2 = very good, 3 = good, 4 = fair, 5 = poor.
1 = Almost never or never; 2 = a few times (much less than half the time); 3 = sometimes (about half the time); 4 = most times (much more than half the time); 5 = almost always or always.
1 = not at all bothered; 2 = very little bothered; 3 = moderately bothered; 4 = significantly bothered; 5 = extremely bothered.
Higher number corresponds to more ventral curvature. See Fig. 1.
1 = did not attempt intercourse; 2 = extremely difficult; 3 = very difficult; 4 = difficult; 5 = slightly difficult; 6 = not difficult.
Association of mild and severe untreated hypospadias with outcomes
Possible untreated hypospadias participants were stratified into mild (n = 37) and severe (n = 15) groups and each group compared with normal (Table 3). Participants with possible mild untreated hypospadias had similar measures to normal men except worse SHIM scores (p = 0.003), more ventral curvature (p = 0.003), and more difficulty with intercourse from penile curvature (p = 0.007). They also had slightly less satisfaction with position and shape of urethral meatus (p = 0.041). Participants with possible severe untreated hypospadias had worse IPSS scores (p = 0.004), worse SHIM scores (p = 0.017), more ventral curvature (p = 0.09), more difficulty with intercourse from (p < 0.001) and dissatisfaction with (p = 0.02) penile curvature, more frequent sitting to urinate (p = 0.003), and reported more unhealthy physical (p = 0.003) and mental (p = 0.017) days than normal men.
Table 3.
Association of outcomes with possible untreated hypospadias by severity.
| Normal | Mild untreated hypospadias |
pa | Severe untreated hypospadias |
pb | |
|---|---|---|---|---|---|
| PPSc | |||||
| Length of penis | 1.9 (0.7) | 1.8 (0.8) | 0.7 | 2.0 (0.7) | 0.5 |
| Position and shape of urethral opening | 2.4 (0.6) | 2.2 (0.5) | 0.044 | 2.1 (0.8) | 0.063 |
| Shape of glans | 2.4 (0.6) | 2.4 (0.6) | 0.6 | 2.2 (0.9) | 0.3 |
| Shape of penile skin | 2.3 (0.6) | 2.4 (0.5) | 0.6 | 2.4 (0.4) | 0.1 |
| Penile axis (curvature) | 2.3 (0.7) | 2.2 (0.8) | 0.4 | 1.7 (1.0) | 0.016 |
| General appearance | 2.2 (0.7) | 2.2 (0.8) | 0.9 | 2.2 (0.6) | 0.9 |
| Overall PPS | 9.4 (2.0) | 9.3 (1.9) | 0.6 | 8.6 (2.3) | 0.2 |
| SHIM score | 20.7 (5.3) | 17.4 (6.2) | 0.003 | 16.1 (6.1) | 0.017 |
| IPSS score | 5.9 (6.0) | 6.5 (7.3) | 0.6 | 10.8 (7.7) | 0.004 |
| CDC HRQOL-4 | |||||
| Would you say your general health isd | 2.5 (1.0) | 2.7 (1.0) | 0.2 | 2.7 (0.9) | 0.5 |
| Mean number of physically unhealthy days | 3.5 (7.0) | 3.5 (6.9) | 0.9 | 9.2 (11.9) | 0.003 |
| Mean number of mentally unhealthy days | 6.5 (8.7) | 6.8 (9.0) | 0.8 | 12.1 (12.4) | 0.017 |
| Caused a pregnancy | 317/674 (47.0%) | 20/37 (54.0%) | 0.4 | 9/14 (64.3%) | 0.2 |
| Diagnosis of infertility | 22/677 (3.2%) | 1/37(2.7%) | 0.8 | 1/15 (6.7%) | 0.4 |
| How often to you sit on toilet to just urinate?e | 1.9 (1.2) | 2.0 (1.3) | 0.8 | 3.1 (1.7) | 0.003 |
| Of those who sit to urinate; how much does it bother you to sit down to just urinate?f | 1.4(0.7) | 1.3 (0.6) | 0.7 | 1.7 (0.8) | 0.8 |
| Penile curvatureg | 1.8 (0.7) | 2.2 (1.1) | 0.015 | 2.3 (1.2) | 0.09 |
| How difficult does the curvature of your penis make intercourse?h | 4.8 (0.6) | 4.5 (1.0) | 0.007 | 4.0 (1.0) | <0.001 |
| Have you ever kissed anyone? | 647/676 (95.7%) | 36/37 (97.3%) | 1.0 | 14/15 (93.3%) | 0.5 |
| Age in years | 14.1 (4.5) | 13.4(4.2) | 0.4 | 14.9 (3.0) | 0.5 |
| Have you ever been in love? | 595/674 (88.3%) | 32/37 (86.5%) | 0.8 | 15/15 (100%) | 0.2 |
| Age in years | 18.2 (6.0) | 17.3 (6.0) | 0.7 | 18.9 (7.0) | 0.7 |
| Have you ever had sexual intercourse? | 598/678 (88.2%) | 31/35 (88.6%) | 1.0 | 14/15 (93.3%) | 1.0 |
| Age in years | 18.3 (5.0) | 18.3 (6.8) | 1.0 | 16.6 (4.9) | 0.2 |
| Have you ever masturbated? | 663/678 (97.8%) | 34/35 (97.1%) | 1.0 | 15/15 (100%) | 1.0 |
| Age in years | 12.3 (2.7) | 11.6 (2.9) | 0.2 | 11.9 (2.3) | 0.6 |
Data presented as mean (standard deviation) or proportion with “yes” answer. Continuous outcomes compared by student’s t-test, ordinal by Wilcoxon rank sum test, dichotomous by chi-square or Fisher Exact test.
p for comparison of normal and mild untreated hypospadias.
p for comparison of normal and severe untreated hypospadias.
All questions coded as 3 = very satisfied; 2 = satisfied; 1 = dissatisfied; 0 = very dissatisfied.
1 = excellent; 2 = very good, 3 = good, 4 = fair, 5 = poor.
1 = Almost never or never; 2 = a few times (much less than half the time); 3 = sometimes (about half the time); 4 = most times (much more than half the time); 5 = almost always or always.
1 = not at all bothered; 2 = very little bothered; 3 = moderately bothered; 4 = significantly bothered; 5 = extremely bothered.
Higher number corresponds to more ventral curvature. See Fig. 1.
1 = did not attempt intercourse; 2 = extremely difficult; 3 = very difficult; 4 = difficult; 5 = slightly difficult; 6 = not difficult.
Analysis of participant images
There were 52 (7.1%) of participants who uploaded an image of their penis. Of the 52, there were 49 who reported having normal anatomy and three who reported having possible untreated hypospadias. Two pediatric urologists (HC and MD) who were blinded to self-reported anatomy reviewed the images. Of the 49 who reported normal anatomy, 38 were normal, 11 were inconclusive, and none had hypospadias. Of the three who reported untreated hypospadias, all three were inconclusive.
Discussion
This study examined whether men with untreated hypospadias have similar outcomes to normal men, especially men with mild hypospadias. Because men with untreated hypospadias are rare, we utilized an electronic survey advertised as a survey on male anatomy and symptoms on Facebook. When analyzed as one large group, participants with possible untreated hypospadias did have several potential adverse outcomes compared with normal men. They reported more dissatisfaction with the position and shape of their meatus, more dissatisfaction with penile axis/curvature, worse SHIM scores, worse IPSS scores, more ventral penile curvature, and more difficulty with intercourse from penile curvature. However, when stratified by mild and severe untreated hypospadias, the most significant differences between participants with possible mild (proximal glans or glans margin) untreated hypospadias and non-hypospadiac participants were related to presence and difficulty with intercourse caused by penile curvature as well as a worse SHIM score. Men with possible severe (meatus on penile shaft) untreated hypospadias had significant differences compared with normal participants with regard to difficulty with intercourse caused by penile curvature, worse SHIM score, worse IPSS score, more frequent sitting to urinate, and worse HRQOL as measured by the CDC HRQOL-4 instrument. This suggests that men with milder forms of untreated hypospadias may have the most adverse outcomes from associated penile curvature, whereas men with more severe forms of untreated hypospadias have more bothersome urination symptoms, more frequent sitting to urinate, as well as more bother from associated penile curvature. Based on these results, one could hypothesize that correcting the associated penile curvature and avoiding urethroplasty in milder forms of hypospadias could prevent most adverse outcomes in those patients as well as avoid the surgical complications of urethroplasty. This hypothesis is also supported by the limited but uncontrolled series of men with mild untreated hypospadias having minimal if any adverse outcomes [6,8].
A study of long-term outcomes in patients with untreated hypospadias and comparison of those outcomes with those of normal men has never been attempted to our knowledge. The small number of studies reporting on men with untreated hypospadias is limited by the lack of any comparison with a control group, the lack of standardized outcome measures, and the small number of patients [6,8]. Our pilot study demonstrates the feasibility of using a survey advertised on social media to quickly perform a survey which can study outcomes for a rare condition where the natural history is not well defined. In addition, 7% of participants were willing to upload an image that could be used to validate instruments used to identify participants’ anatomy in a much larger study. Participants identified through such surveys could potentially be recruited to be more thoroughly evaluated in person to confirm results.
Not only is the natural history of untreated hypospadias unknown, long-term outcomes after treatment of hypospadias are not well defined. Similar types of social media advertised studies specifically targeting men with a history of hypospadias surgery could be used to study outcomes in these patients as well. Another important unanswered question is whether surgical treatment of milder forms of hypospadias improves long-term outcomes when compared with the natural history of mild untreated hypospadias. Our pilot study has shown that the use of social media is a novel and useful method for recruiting participants for studies that may help shed some light on the above questions.
Study weaknesses
This study has several weaknesses. Validated survey instruments were used to measure outcomes related to hypospadias when available, but for other outcomes novel questions were used. For some outcomes with novel questions, such as paternity and sexual milestones, the questions were yes/no and have high face validity. For other novel questions for outcomes, such as frequency of sitting to urinate and difficulty with sexual intercourse from penile curvature, the questions were modeled after other validated surveys such as the IPSS and SHIM. The questions used to identify participants as having possible untreated hypospadias were pretested and found to have good construct validity in a group of subjects looking at images of normal and hypospadiac penises. However, the number of participants in this study was limited by the pilot nature of the funding, which led to an inability to recruit enough subjects to validate the self-identification of hypospadias. The population of individuals who answered this survey on Facebook is not representative of the entire population. Selection bias would have contributed to the observed associations if men who reported adverse outcomes were also more likely to incorrectly identify themselves as having hypospadias. It is possible that men who were unsatisfied with their penis or its function for a variety of reasons were more likely to incorrectly select that they had hypospadias and also report adverse outcomes.
Conclusions
Men who reported possible untreated hypospadias reported adverse outcomes compared with normal men The most significant adverse outcomes reported by men with possible mild untreated hypospadias appeared to be the presence of penile curvature and difficulty with intercourse caused by penile curvature. Men who reported more severe untreated hypospadias had more adverse outcomes, including worse IPSS scores and more frequent sitting to urinate in addition to more difficulty with and bother from penile curvature. The natural history of untreated mild hypospadias remains poorly defined and it is unknown if surgical treatment of mild hypospadias in childhood improves long-term outcomes.
Supplementary Material
Acknowledgments
Funding
This study was supported by a University of California San Francisco Research Evaluation and Allocation Committee (REAC) grant.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jpurol.2014.01.024.
Appendix 2. Pretesting questions regarding anatomy
| Urethral meatus location pretest | ||||||
|---|---|---|---|---|---|---|
| Meatus image | Gold standarda | Normal |
Possible hypospadias (severity increases from B to E) |
|||
| A | B | C | D | E | ||
| Image 1 | C | 0 | 1 | 25 | 0 | 0 |
| Image 2 | D | 0 | 1 | 6 | 19 | 0 |
| Image 3 | B | 0 | 20 | 6 | 0 | 0 |
| Image 4 | E | 0 | 0 | 0 | 0 | 26 |
| Image 5 | A | 26 | 0 | 0 | 0 | 0 |
| Image 6 | D | 0 | 0 | 6 | 26 | 0 |
| Image 7 | D | 0 | 1 | 4 | 21 | 0 |
| Foreskin/Penile appearance pretest | ||||||
| Appearance image | Gold Standarda | Circumcised | Uncircumcised | Hypospadias | ||
| Image 1 | Hypospadias | 0 | 1 | 25 | ||
| Image 2 | Uncircumcised | 0 | 26 | 0 | ||
| Image 3 | Hypospadias | 0 | 0 | 26 | ||
| Image 4 | Circumcised | 26 | 0 | 0 | ||
| Image 5 | Hypospadias | 4 | 2 | 20 | ||
| Penile curvature pretest | ||||||
| Curvature image | Gold Standarda | 1 | 2 | 3 | 4 | 5 |
| Image 1 | 4 | 0 | 0 | 0 | 12 | 14 |
| Image 2 | 4 | 0 | 0 | 4 | 20 | 2 |
| Image 3 | 2 | 0 | 25 | 1 | 0 | 0 |
| Image 4 | 1 | 26 | 0 | 0 | 0 | 0 |
| Image 5 | 5 | 0 | 0 | 0 | 1 | 25 |
Gold Standard = consensus opinion of 2 pediatric urologists.
Footnotes
Conflict of interest
None.
References
- 1.Baskin LS, Ebbers MB. Hypospadias: anatomy, etiology, and technique. J Pediatr Surg. 2006;41(3):463–472. doi: 10.1016/j.jpedsurg.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 2.Kraft KH, Shukla AR, Canning DA. Hypospadias. Urol Clin North Am. 2010;37(2):167–181. doi: 10.1016/j.ucl.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Snodgrass WT, Bush N, Cost N. Tubularized incised plate hypospadias repair for distal hypospadias. J Pediatr Urol. 2009;6(4):408–413. doi: 10.1016/j.jpurol.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Snodgrass WT, Bush N, Cost N. Algorithm for comprehensive approach to hypospadias reoperation using 3 techniques. J Urol. 2009;182(6):2885–2891. doi: 10.1016/j.juro.2009.08.062. [DOI] [PubMed] [Google Scholar]
- 5.Brouwers MM, van der Zanden LF, de Gier RP, Barten EJ, Zielhuis GA, Feitz WF, et al. Hypospadias: risk factor patterns and different phenotypes. BJU Int. 2010;105(2):254–262. doi: 10.1111/j.1464-410X.2009.08772.x. [DOI] [PubMed] [Google Scholar]
- 6.Dodds PR, Batter SJ, Shield DE, Serels SR, Garafalo FA, Maloney PK. Adaptation of adults to uncorrected hypospadias. Urology. 2008;71(4):682–685. doi: 10.1016/j.urology.2007.07.078. discussion 685. [DOI] [PubMed] [Google Scholar]
- 7.Uygur MC, Ersoy E, Erol D. Analysis of meatal location in 1,244 healthy men. Definition of the normal site justifies the need for meatal advancement in pediatric anterior hypospadias cases. Pediatr Surg Int. 1999;15(2):119–120. doi: 10.1007/s003830050530. [DOI] [PubMed] [Google Scholar]
- 8.Fichtner J, Filipas D, Mottrie AM, Voges GE, Hohenfellner R. Analysis of meatal location in 500 men: wide variation questions need for meatal advancement in all pediatric anterior hypospadias cases. J Urol. 1995;154(2):833–834. [PubMed] [Google Scholar]
- 9.Gene A, Taneli C, Oksel F, Balkan C, Bilgi Y. Analysis of meatal location in 300 boys. Int Urol Nephrol. 2001;33(4):663–664. doi: 10.1023/a:1020570900143. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson DJ, Farrelly P, Kenny SE. Outcomes in distal hypospadias: a systematic review of the Mathieu and tubularized incised plate repairs. J Pediatr Urol. 2012;8(3):307–312. doi: 10.1016/j.jpurol.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Scarpa MG, Castagnetti M, Berrettini A, Rigamonti W, Musi L. Urinary function after Snodgrass repair of distal hypospadias: comparison with the Mathieu repair. Pediatr Surg Int. 2010;26(5):519–522. doi: 10.1007/s00383-010-2569-6. [DOI] [PubMed] [Google Scholar]
- 12.Al-Ghorairy BA, Elashry OM, Al-Housain AE, Mattar AA. Analysis of five-year experience with tubularized incised plate urethroplasty for anterior and mid penile hypospadias. Eur J Pediatr Surg. 2009;19(2):90–95. doi: 10.1055/s-0029-1214408. [DOI] [PubMed] [Google Scholar]
- 13.Facebook’s latest news, announcements and media resources. www.facebook.com/press/info.php?statistics.
- 14.Bull SS, Breslin LT, Wright EE, Black SR, Levine D, Santelli JS. Case study: an ethics case study of HIV prevention research on facebook: The Just/Us Study. J Pediatr Psychol. 2011;36(10):1082–1092. doi: 10.1093/jpepsy/jsq126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lord S, Brevard J, Budman S. Connecting to young adults: an online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Subst Use Misuse. 2011;46(1):66–76. doi: 10.3109/10826084.2011.521371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breyer BN, Smith JF, Eisenberg ML, Ando KA, Rowen TS, Shindel AW. The impact of sexual orientation on sexuality and sexual practices in North American medical students. J Sex Med. 2010;7(7):2391–2400. doi: 10.1111/j.1743-6109.2010.01794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breyer BN, Van den Eeden SK, Horberg MA, Eisenberg ML, Deng DY, Smith JF, et al. HIV status is an independent risk factor for reporting lower urinary tract symptoms. J Urol. 2011;185(5):1710–1715. doi: 10.1016/j.juro.2010.12.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shindel AW, Horberg MA, Smith JF, Breyer BN. Sexual dysfunction, HIV, and AIDS in men who have sex with men. AIDS Patient Care STDS. 2011;25(6):341–349. doi: 10.1089/apc.2011.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith JF, Breyer BN, Eisenberg ML, Sharlip ID, Shindel AW. Sexual function and depressive symptoms among male North American medical students. J Sex Med. 2011;8(2):391–399. doi: 10.1111/j.1743-6109.2010.02085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) –a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weber DM, Landolt MA, Gobet R, Kalisch M, Greeff NK. The penile perception score: an instrument enabling evaluation by surgeons and patient self-assessment after hypospadias repair. J Urol. 2013;189(1):189–193. doi: 10.1016/j.juro.2012.08.178. [DOI] [PubMed] [Google Scholar]
- 22.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11(6):319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 23.Rhoden EL, Teloken C, Sogari PR, Vargas Souto CA. The use of the simplified International Index of Erectile Function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res. 2002;14(4):245–250. doi: 10.1038/sj.ijir.3900859. [DOI] [PubMed] [Google Scholar]
- 24.Cappelleri JC, Rosen RC. The Sexual Health Inventory for Men (SHIM): a 5-year review of research and clinical experience. Int J Impot Res. 2005;17(4):307–319. doi: 10.1038/sj.ijir.3901327. [DOI] [PubMed] [Google Scholar]
- 25.Barry MJ, Fowler FJ, Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549–1557. doi: 10.1016/s0022-5347(17)36966-5. discussion 1564. [DOI] [PubMed] [Google Scholar]
- 26.Cockett AT, Aso Y, Denis L, Khoury S, Barry M, Carlton CE, et al. World Health Organization Consensus Committee recommendations concerning the diagnosis of BPH. Prog Urol. 1991;1(6):957–972. [PubMed] [Google Scholar]
- 27.U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. Atlanta, Georgia: CDC; 2000. Nov, [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.