Abstract
Objective
The purpose of this study was to establish, using a quasi-experimental design, whether two family risk factors, parental psychological dysfunction and nonsupportive parenting, during preadolescence could longitudinally predict elevated sympathetic nervous system (SNS) activity 9 years later, and to determine whether participation in an efficacious family-centered prevention program could moderate these associations if they emerged.
Methods
Rural African American preadolescents (N = 476) were assigned randomly to the Strong African American Families (SAAF) program or to a control condition. When youths were 11 years of age (M = 11.2 years), primary caregivers provided data on their own depressive symptoms and self-esteem, and youths provided data on their receipt of nonsupportive parenting. When the youths were 20 years of age, indicators of SNS activity, the catecholamines epinephrine and norepinephrine, were assayed from their overnight urine voids.
Results
Parental psychological dysfunction and nonsupportive parenting forecast elevated catecholamine levels for youths in the control condition, but not for those in the SAAF condition.
Conclusions
The demonstration that a prevention program can induce reduction of catecholamine levels is important from both theoretical and public health perspectives, because it shows that the developmental progression from family risk factors to heightened sympathetic nervous system activity is not immutable.
Keywords: family intervention, health promotion, human development, parenting, sympathetic nervous system
A growing body of research has tested the hypothesis that family emotional climate during childhood and adolescence may contribute to chronic diseases later in life (Chen & Miller, 2012). The risky family model offers a psychosocial account of the impact that stress during childhood exerts on health (Repetti, Taylor, & Seeman, 2002). It posits that some families confer risk for later health problems by producing emotionally cold, nonsupportive rearing environments in which primary caregivers evince elevated depressive symptoms and low self-esteem. Such rearing environments are hypothesized to influence the development of the body’s stress response systems, calibrating the way in which they respond to threats across the life course. Most of the research to date on risky family environments has focused on the HPA axis, but for long-term health outcomes it is also important to consider the sympathetic nervous system (SNS).
The SNS enables people to mount biobehavioral responses, such as flight or fight, that mobilize bodily resources to cope with threats. Everyday SNS activity is typically indexed by overnight urinary concentrations of the system’s hormonal end products, the catecholamines epinephrine and norepinephrine. Although SNS responses can be adaptive for managing short-term threats, considerable research with animal models suggests they can take a physiological toll on affected organs if frequent, prolonged, or both (Manuck, Marsland, Kaplan, & Williams, 1995; Sloan, Capitanio, & Cole, 2008). The impact of chronic hormonal surges from the SNS may accumulate with time, leading to multisystem dysregulation that contributes to health problems (Reuben, Talvi, Rowe, & Seeman, 2000).
This study was designed to advance understanding of the association between risky family processes and SNS activity. A quasi-experimental design was used to test two hypotheses with a representative sample of rural African American youths who took part in a randomized prevention trial. The first hypothesis proposed that youths assigned randomly to the control condition who, at age 11, were living with a primary caregiver who reported psychological dysfunction—defined as relatively high levels of depressive symptoms and low self-esteem—or provided nonsupportive parenting would evince relatively high catecholamine levels at age 20. This study was also designed to test the hypothesis that, among youths exposed to nonsupportive parenting or low caregiver functioning, random assignment to the Strong African American Families (SAAF) program (Brody et al., 2004) would be associated with relatively low catecholamine levels at age 20. SAAF is a family-centered prevention program designed to prevent risk behaviors by enhancing parental warmth, involvement, and communication. In observational studies, these practices have buffered youths from the effects of stress on biological regulatory systems (Chen & Miller, 2012). Evaluations of SAAF confirmed its efficacy in enhancing these protective parenting practices (Brody, Kogan, & Grange, 2012).
Method
Overview
A pretest assessment, which included the collection of data on low parental support and parental psychological dysfunction, was conducted when the youths were 11 years of age (M = 11.2, SD = 0.34). Participation in the SAAF trial began when the youths were 11.5 years of age. The data on the catecholamines epinephrine and norepinephrine were obtained from overnight urine voids when the youths were 20 years of age (M = 20.4, SD = 0.61).
Participants
Participants in the SAAF trial included 667 African American families who resided in rural Georgia. At pretest, although the primary caregivers in the sample worked an average of 39.4 hours per week, 46.3% lived below federal poverty standards; the proportion was 53.7% at the age 20 assessment. From a sample of 561 at the age 18 data collection (a retention rate of 84%), 500 emerging adults were selected randomly to take part in the assessment of catecholamines at age 20; the selection of a random subsample was made necessary by financial constraints associated with the costs of assaying the catecholamines. Of this subsample, 476 agreed to participate; they constituted the sample in the present study. At age 11, 277 of these participants had been assigned randomly to the SAAF condition and 199 had been assigned randomly to the control condition. The original random assignment oversampled participants into the SAAF condition; this accounts for the greater number of 20-year-olds in the SAAF group. Written informed consent was provided. Each family was paid $100 after the assessment. Comparisons of pretest data collected at age 11 and data collected at age 18, using independent t tests and chi-square tests, of the youths who provided catecholamine data at age 20 with those who did not provide them did not reveal any differences on any demographic or study variables.
Intervention Implementation
The SAAF prevention program consisted of 7 consecutive weekly meetings held at community facilities, with separate parent and youth skill-building curricula and a family curriculum (see Brody et al., 2012, for a complete description). Each meeting included separate, concurrent training sessions for parents and youths, followed by a joint parent–youth session during which the families practiced the skills they learned in the separate sessions. Concurrent and family sessions each lasted 1 hour; thus, parents and youths received 14 hours of prevention programming. During the weeks when the intervention families participated in the prevention sessions, the control families received three leaflets via postal mail describing early adolescent development, stress management, and the benefits of exercise. Parents in the prevention condition were taught the consistent provision of instrumental and emotional support, high levels of monitoring and control, adaptive racial socialization strategies, and the establishment of clear norms for the use of alcohol and other drugs. Youths were taught adaptive behaviors to use when encountering racism, the importance of forming goals for the future and making plans to attain them, and resistance efficacy skills. Coverage of the curriculum components (fidelity) exceeded .80 for the primary caregiver and target sessions. To preserve the random nature of the group assignment, the analyses reported here included all families who completed the pretest regardless of the number of prevention sessions that they actually attended (an intent-to-treat analysis). These families were retained in the analysis to preclude the introduction of self-selection bias into the findings.
Data Collection Procedures
Data on parenting, parental psychological adjustment, and demographic characteristics were collected in participants’ homes using a standardized protocol at pretest. Two African American field researchers worked separately with the primary caregiver and the target child. Interviews were conducted privately, with no other family members present or able to overhear the conversation. Catecholamines, alcohol use, smoking, exercise, BMI, and general health problems were assessed when youths were 20 years of age.
Measures
Socioeconomic risk index
Six dichotomous variables formed a socioeconomic risk index that was used as a control in the data analyses. A score of 1 was assigned to each of the following: family poverty based on federal guidelines, primary caregiver unemployment, receipt of Temporary Assistance for Needy Families, primary caregiver single parenthood, primary caregiver education level less than high school graduation, and caregiver-reported inadequacy of family income. The scores were summed to form the index.
Alcohol use, smoking, exercise, BMI, and health problems
At age 20, youths reported their alcohol use, cigarette smoking, exercise, BMI, and health problems. Youths reported past-month alcohol use on a 6-point scale ranging from none to 20 or more days and smoking on a 7-point scale ranging from not at all to about two packs a day. Because the distributions of both smoking and alcohol use were skewed, we applied a log transformation to normalize the ratings. Youths also indicated the number of days during the past week on which they were physically active for a total of at least 60 minutes. Each participant’s weight and height were recorded and used to calculate BMI (weight in kilograms divided by the square of height in meters). Finally, youths reported their health problems using the General Health Perceptions subscale from the RAND 36-Item Short-Form Health Survey (Hays, Sherbourne, & Mazel, 1993); α = .75.
Intervention status and gender
Intervention status and gender were dummy coded. SAAF participants were coded 1 and control participants were coded 0; male participants were coded 1 and female participants were coded 0.
Nonsupportive parenting
Three scales, which were reverse coded so that high scores indicated less supportive parenting, were used to create the nonsupportive parenting construct. Youths reported nurturant-involved parenting using a nine-item instrument developed for research with rural African American families (Brody et al., 2001); α = .76. Supportive communication was assessed with 15 true-false items from the Interaction Behavior Questionnaire (IBQ; Prinz, Foster, Kent, & O’Leary, 1979); α = .78. Family rules and routines were assessed with a seven-item scale (Brody et al., 2001); α = .66. These measures were standardized and summed to form a nonsupportive parenting score.
Parental psychological dysfunction
Parental psychological dysfunction was operationalized as high levels of depressive symptoms in conjunction with low self-esteem. Parental depressive symptoms were measured via self-report on the Center for Epidemiologic Studies Depression scale (CES–D; Radloff, 1977), which is widely used with community samples; α = .85. Parental self-esteem was assessed with the Rosenberg Self-Esteem scale (Rosenberg, 1965); α = .73. Parental depressive symptom and self-esteem scores were standardized, and self-esteem was subtracted from depressive symptoms. High values indicated that parents had high levels of depressive symptoms and low self-esteem.
Emerging adult SNS catecholamines
Participants collected their overnight (8 p.m. to 8 a.m.) urine voids. All urine voided during this time was stored on ice in a container with metabisulfite as a preservative. Total volume was recorded, and four 10-ml samples were randomly extracted and deep frozen at -80° C. The pH of two of these samples was adjusted to 3 to inhibit oxidation of catecholamines. The frozen urine was delivered to the Emory University Hospital medical laboratory in Atlanta, Georgia, for assaying. Epinephrine and norepinephrine were assayed with high-pressure liquid chromatography with electrochemical detection (Riggin & Kissinger, 1977), with intra-assay coefficients of variation averaging < 8%. Creatinine assay via Jaffe rate methods controlled for body size differences and incomplete urine voiding (Tietz, 1976). SNS catecholamine scores were calculated by summing the standardized scores of overnight epinephrine and norepinephrine.
Results
Plan of Analysis
Two regression models were executed, with nonsupportive parenting or parental dysfunction as predictors, to test the first study hypothesis. These models included controls for gender, socioeconomic risk at age 11, and alcohol use, smoking, exercise, BMI, and general health problems at age 20. Two additional regression models were executed to test the second study hypothesis. These models tested the contributions to catecholamine levels of nonsupportive parenting or parental psychological dysfunction, assignment to SAAF or the control group, and the interaction of nonsupportive parenting/parental psychological dysfunction with prevention status. Interactions were interpreted through the plotting of estimated levels of catecholamines at low (1 standard deviation below the mean; -1 SD) and high (1 standard deviation above the mean; +1 SD) levels of either nonsupportive parenting or parental psychological dysfunction according to prevention status.
Tests of Hypotheses
Family risks at age 11 and catecholamine levels at age 20
Supplemental Table 1, available online, presents descriptive statistics along with bivariate correlations. Tests of the first study hypothesis indicated that, for youths assigned randomly to the control group, both nonsupportive parenting, β = .175, p < .05; ΔF(1,190) = 6.111, p < .02, ΔR2 = .030, and parental psychological dysfunction, β = .203, p < .01; ΔF(1,190) = 7.198, p < .01, ΔR2 = .035, at age 11 forecast elevated catecholamine levels 9 years later, with gender, SES risk, alcohol use, smoking, exercise, BMI, and general health problems controlled (see Supplemental Table 2, online). The results did not change when epinephrine and norepinephrine were analyzed separately.
Prevention programming and risk for elevated catecholamines
The second hypothesis proposed interaction effects between each of the hypothesized risk factors and prevention program participation status on catecholamine levels at age 20. Participants assigned randomly to SAAF were assigned a code of 1, and those assigned randomly to the control condition were assigned a code of 0. The analysis for nonsupportive parenting revealed an interaction with prevention status, β = -.195, p < .05; ΔF(1,465) = 6.007, p < .02, ΔR2 = .012. A significant interaction also emerged for parental psychological dysfunction, β = -.143, p < .05; ΔF(1,465) = 4.078, p < .05, ΔR2 = .008. (See Models 1 and 2 in Supplemental Table 3, online, for additional information about these analyses.) These interactions are illustrated in Figures 1a and 1b. Nonsupportive parenting, simple-slope = 0.176, SE = 0.062, p < .01, and parental psychological dysfunction, simple-slope = 0.217, SE = 0.068, p < .01, when youths were 11 were significantly associated with youth catecholamine levels at age 20 among those randomly assigned to the control group. These risk factors were not associated with catecholamine levels among youths randomly assigned to the prevention group, simple-slope = -0.010, SE = 0.044, p = ns for nonsupportive parenting; simple-slope = 0.042, SE = 0.058, p = ns for parental psychological dysfunction. When the analyses were executed separately for norepinephrine and epinephrine, the prevention buffering effect was more apparent for norepinephrine (both ps < .05) than for epinephrine (both ps < .10).
Figure 1.
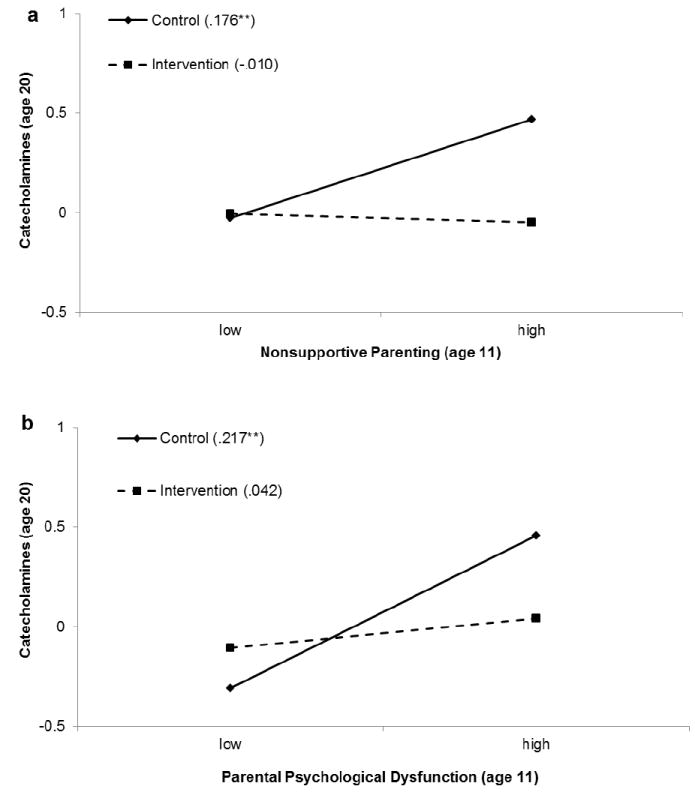
The effect of nonsupportive parenting (1a) and parental psychological dysfunction (1b) on youths’ catecholamines by intervention status. Numbers in parentheses refer to simple slopes for the control group and the intervention group.
Discussion
This quasi-experimental study tested hypotheses about the effects of prevention at age 11 on catecholamines at age 20. Young adults who had experienced high parental psychological dysfunction or nonsupportive parenting at age 11 and were assigned to the prevention condition evinced lower catecholamines than did their control group counterparts. From a public health perspective, these results suggest that developmentally appropriate interventions designed to enhance supportive parenting practices may buffer the effects of family risks on later SNS activity, particularly for families evincing high levels of risk.
A comment is warranted about intermediate or mediating processes that may contribute to a refined understanding of the obtained protective effects. Participation in SAAF, but not assignment to the control condition, was associated with a decrease in nonsupportive parenting from pretest to posttest; see Supplemental Table 4, online. This suggests that, among youths exposed to high family risk levels, those assigned to SAAF may have had caregivers whose parenting skills enhanced youth self-regulation and emotion-regulation abilities. These abilities would help youths to avoid a stress-generation loop in which low self-regulation and emotion regulation levels lead to heightened experiences with life stress that, in turn, would intensify SNS activity. Because examination of the effect of SAAF on SNS activity was not anticipated when the prevention trial began, no measures were included to index these potential mediating processes. This conjecture awaits further research.
Several limitations of the present study should be addressed in future research. First, it is not known whether the results of this study would generalize to urban African Americans or to families of other ethnicities. Second, because catecholamines were not one of the outcomes of interest when the study started, no baseline assessment for them is available. Hence, we cannot conclude that the intervention changed catecholamine levels. Third, the assay of catecholamines did not indicate how much of the variance is tonic versus phasic and did not indicate where the catecholamines were released (e.g., lungs, heart, or muscle). Future research should determine how exposure to family risks affects the nature of catecholamine release. Nevertheless, this analysis is one of the first to examine the ways in which family risk factors “get under the skin” to increase risk for heightened SNS activity and to suggest that family-centered preventive intervention can interrupt this process.
Supplementary Material
Acknowledgments
This research was supported by Award Number P30DA027827 from the National Institute on Drug Abuse and Award Number R01HD030588 from the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, or the National Institutes of Health.
Contributor Information
Gene H. Brody, Center for Family Research, University of Georgia
Tianyi Yu, Center for Family Research, University of Georgia.
Edith Chen, Department of Psychology and Institute for Policy Research, Northwestern University.
Gregory E. Miller, Department of Psychology and Institute for Policy Research, Northwestern University
References
- Brody GH, Ge X, Conger RD, Gibbons FX, Murry VM, Gerrard M, Simons RL. The influence of neighborhood disadvantage, collective socialization, and parenting on African American children’s affiliation with deviant peers. Child Development. 2001;72:1231–1246. doi: 10.1111/1467-8624.00344. [DOI] [PubMed] [Google Scholar]
- Brody GH, Kogan SM, Grange CM. Translating longitudinal, developmental research with rural African American families into prevention programs for rural African American youth. In: King RB, Maholmes V, editors. The Oxford handbook of poverty and child development. New York, NY: Oxford University Press-USA; 2012. pp. 553–570. [Google Scholar]
- Brody GH, Murry VM, Gerrard M, Gibbons FX, Molgaard V, McNair LD, Neubaum-Carlan E, et al. The Strong African American Families program: Translating research into prevention programming. Child Development. 2004;75:900–917. doi: 10.1111/j.1467-8624.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- Chen E, Miller GE. “Shift-and-persist” strategies: Why low socioeconomic status isn’t always bad for health. Perspectives on Psychological Science. 2012;7:135–158. doi: 10.1177/1745691612436694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Economics. 1993;2:217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- Manuck SB, Marsland AL, Kaplan JR, Williams JK. The pathogenicity of behavior and its neuroendocrine mediation: An example from coronary artery disease. Psychosomatic Medicine. 1995;57:275–283. doi: 10.1097/00006842-199505000-00009. Retrieved from http://www.psychosomaticmedicine.org/content/57/3/275.full.pdf+html. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster SL, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother–adolescent dyads. Journal of Applied Behavior Analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–336. doi: 10.1037/0033-2909.128.2.330. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Talvi SLA, Rowe JW, Seeman TE. High urinary catecholamine excretion predicts mortality and functional decline in high-functioning, community-dwelling older persons: MacArthur Studies of Successful Aging. Journals of Gerontology: Series A Biological Sciences and Medical Sciences. 2000;55:M618–M624. doi: 10.1093/gerona/55.10.M618. [DOI] [PubMed] [Google Scholar]
- Riggin RM, Kissinger PT. Determination of catecholamines in urine by reverse-phase liquid chromatography with electrochemical detection. Analytical Chemistry. 1977;49:2109–2111. doi: 10.1021/ac50021a052. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Sloan EK, Capitanio JP, Cole SW. Stress-induced remodeling of lymphoid innervation. Brain, Behavior, and Immunity. 2008;22:15–21. doi: 10.1016/j.bbi.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tietz NW, editor. Fundamentals of clinical chemistry. 2. Philadelphia, PA: Saunders; 1976. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


