Abstract
Objective:
We aimed to describe hospitalizations in the multiple sclerosis (MS) population, and to evaluate temporal trends in hospitalizations in the MS population compared to the general population.
Methods:
Using population-based administrative data, we identified 5,797 persons with MS and a matched general population cohort of 28,769 persons. Using general linear models, we evaluated temporal trends in hospitalization rates and length of stay in the 2 populations over the period 1984–2011.
Results:
In 1984 the hospitalization rate was 35 per 100 person-years in the MS population and 10.5 in the matched population (relative risk [RR] 3.33; 95% confidence interval: 1.67–6.64). Over the study period hospitalizations declined 75% in the MS population but only 41% in the matched population. The proportion of hospitalizations due to MS declined substantially from 43.4% in 1984 to 7.8% in 2011. The 3 most common non–MS-related reasons for admission in the MS population were diseases of the digestive, genitourinary, and circulatory systems. Admissions for bacterial pneumonia, influenza, urinary tract infections, and pressure ulcers occurred more often in the MS population than in the general population, while admissions for circulatory system disease and neoplasms occurred less often. Older age, male sex, and lower socioeconomic status were associated with increased hospitalization rates for non–MS-related reasons.
Conclusions:
Although hospitalization rates have declined dramatically in the MS population over the last quarter century, they remain higher than in the general population. Admissions for MS-related reasons now constitute only a small proportion of the reasons for hospitalization.
Substantial changes in multiple sclerosis (MS) care have occurred over the last 20 years. Diagnostic criteria have changed, diagnostic delays are shorter,1,2 and disease-modifying therapies were introduced.3,4 Despite these changes, little information is available regarding changes in health care utilization in the MS population.5,6 The annual frequency of hospitalizations in the MS population reportedly ranges from 2.7% to 25.8%.7–12 However, most prior studies were not population-based and relied on self-report. In British Columbia, Canada, hospitalization rates based on administrative data decreased by 1.4% annually in the MS population from 1986 to 200813 but were not compared to hospitalization rates in the general population, in which hospitalizations are declining.14 The British Columbia study also found that hospital length of stay (LOS) increased over time, contrasting with an American study in which the mean LOS decreased from 1993 to 1998.6
To understand the changing burden of MS on the health system, plan for future needs, and assess costs and benefits of emerging therapies, longitudinal studies of health care utilization are needed. We conducted a population-based study of rates of and reasons for hospitalization in the MS population vs a matched general population cohort over 25 years. We hypothesized that hospitalization rates are declining faster in the MS population than in the general population.
METHODS
Data source.
We used administrative (health claims) data from the Canadian province of Manitoba. Manitoba Health, the provincial health department, oversees health services delivery to 98% of the region's approximately 1.2 million residents15,16 and maintains electronic records of health services claims. A population registry is updated when an individual moves into or out of Manitoba or dies. Since 1984, all claims have included a unique personal health identification number identifying the person to whom the service was delivered. To protect confidentiality, data linkage was performed via scrambled personal health identification number using anonymized versions of these databases for the period 1984–2011.
Standard protocol approvals, registrations, and patient consents.
The University of Manitoba Health Research Ethics Board approved the study, and the Manitoba Health Information Privacy Committee approved data access.
Study populations.
Using a validated case definition,17 we identified Manitobans with MS from 1984 to 2011 as persons with ≥3 hospital, physician, or prescription claims for MS. We identified controls from the general population, excluding anyone with ≥1 ICD-9-CM/ICD-10-CA diagnostic code for any demyelinating disease (see supplemental methods on the Neurology® Web site at Neurology.org). This ensured that individuals with one demyelinating event who might ultimately meet the case definition for MS were not misclassified as controls and allowed a distinct comparison between the MS and general populations. We selected up to 5 controls for each MS case, matched on sex, exact year of birth, and region of residence (postal code). For persons with MS we assigned the date of diagnosis (index date) as the date of the first demyelinating disease claim (e.g., optic neuritis), and we assigned the same date to their matched controls.
Outcomes.
We focused on acute care hospitalizations, as this is the largest component of health resource use in industrialized countries.18–21 We used hospital claims to identify inpatient (overnight) hospitalizations after excluding admissions related to long-term care, respite, or pregnancy, as the factors that influence such admissions may differ from those influencing hospitalizations for acute illness. To avoid double counting hospitalizations related to transfers between facilities for continued care, overnight hospitalizations beginning within ±1 day of another hospital discharge with the same primary or secondary diagnosis codes were considered part of the same hospitalization.22 We determined the LOS for each hospitalization.
For the MS population, we classified hospitalizations as MS-related, possibly MS-related, and not MS-related (see appendix e-1 for details). Non–MS-related hospitalizations were classified according to ICD-10 chapters for the MS and matched populations.
Analyses.
Continuous variables were summarized as mean (SD), while categorical variables were summarized as frequency (percent). We estimated the crude annual rate of hospitalizations per 100 person-years from 1984 to 2011. To estimate temporal changes in hospitalization rates, we used Poisson regression models with generalized estimating equations using an exchangeable correlation to account for repeated hospitalizations by individuals. We included the log of person-years as an offset in the models. Year was categorized into 5-year groups (1984–1989, 1990–1994, 1995–1999, 2000–2004, 2005–2009, and 2010–2011). Covariates included sex (female as reference group); age at observation year categorized as <40 years (reference group), 40–60 years, and >60 years to ensure adequate cell sizes; and socioeconomic status (SES) in quintiles. We determined SES by linking forward sortation area (first 3 digits of postal code) to Canadian census data in 2001 to determine median household income for the residential area.23 We did not include a separate variable for region as forward sortation area was being used to determine SES. Findings from the regression models are reported as adjusted rate ratios (RRs) with 95% confidence intervals (CIs). Additional analyses using the same methods included evaluation of temporal trends in hospitalizations for non–MS-related reasons in both populations, and MS-related and non–MS-related reasons in the MS population.
Using a logistic regression model with generalized estimating equations to account for repeated hospitalizations by individuals, we evaluated the association between year of admission and reason for admission (MS-related vs not MS-related). We excluded hospitalizations that were possibly MS-related (n = 649). To ensure adequate cell sizes, year was categorized as previously described. Covariates included sex, age at observation year, and SES in quintiles. We report odds ratios and 95% CIs.
Statistical analyses used SAS 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
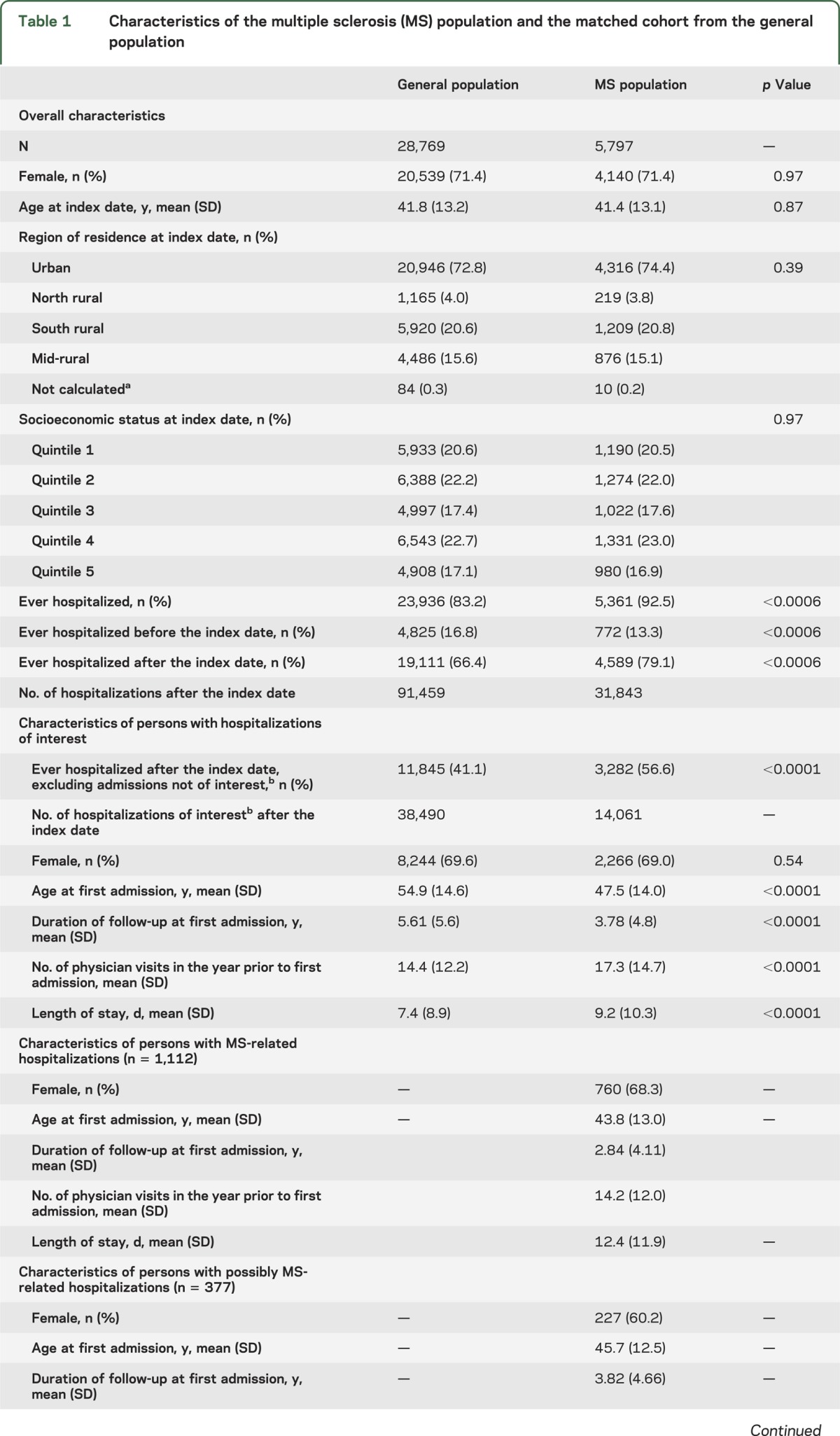
We identified 5,797 persons with MS and 28,769 controls. The cohorts were well-matched (table 1). After the index date, excluding hospitalizations related to long-term care, respite, and pregnancy, 3,282 persons with MS had 14,061 admissions, while 11,845 controls had 38,490 admissions. On average, the age at first admission was 7 years earlier in the MS population.
Table 1.
Characteristics of the multiple sclerosis (MS) population and the matched cohort from the general population
All-cause hospitalizations.
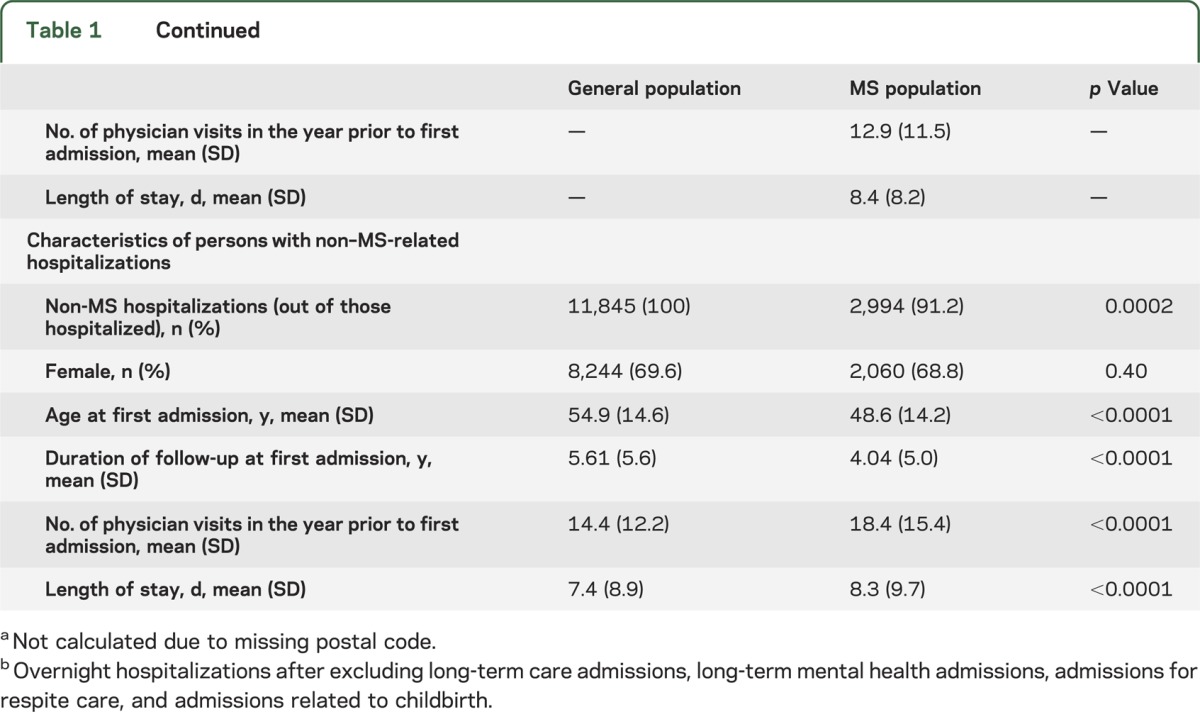
In 1984, 24.5% of the MS population was hospitalized. At 35.0 hospitalizations per 100 person-years, rates were higher than in matched controls (RR 3.33; 1.67–6.64). Only 7.5% of the controls were hospitalized, for a rate of 10.5 hospitalizations per 100 person-years. In a linear regression model, the annual rate of hospitalizations declined by −0.80 (−0.93, −0.67) per year overall in the MS population (figure 1). We observed a steep decline of −3.09 (−4.04, −2.14) in 1984–1988. In the period before the introduction of disease-modifying therapies (1984–1997), the average decline was −1.42 (−1.77, −1.07), whereas it was only −0.38 (−0.48, −0.29) from 1999 onward. In 2011, the hospitalization rate was 75% lower than it had been 27 years earlier. The hospitalization rate declined more slowly in the matched cohort (−0.20; −0.23, −0.17). In 2011, the hospitalization rate was only 41% lower than in 1984.
Figure 1. Annual rate of hospitalizations in the multiple sclerosis (MS) and general populations.
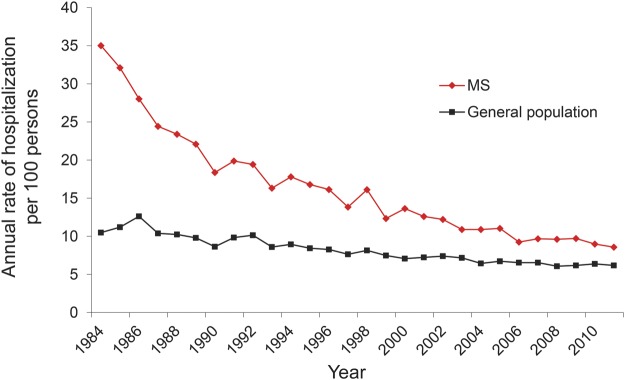
In both cohorts, hospitalization rates were lower in men than in women (RR 0.84; 0.76–0.93) and increased with age (table 2 shows age-specific rates for 2011). Due to an interaction between population and both year and age (both p < 0.0001), we constructed separate regression models for the 2 populations (table 3). After adjustment for sex, age, and SES, we still observed higher hospitalization rates in both populations at the beginning of the study period than at the end. Findings were unchanged after adjustment for other health care utilization (table e-1).
Table 2.
Age-specific rates (95% confidence intervals [CIs]) of hospitalization in the multiple sclerosis population and the matched cohort from the general population in Manitoba in 2011
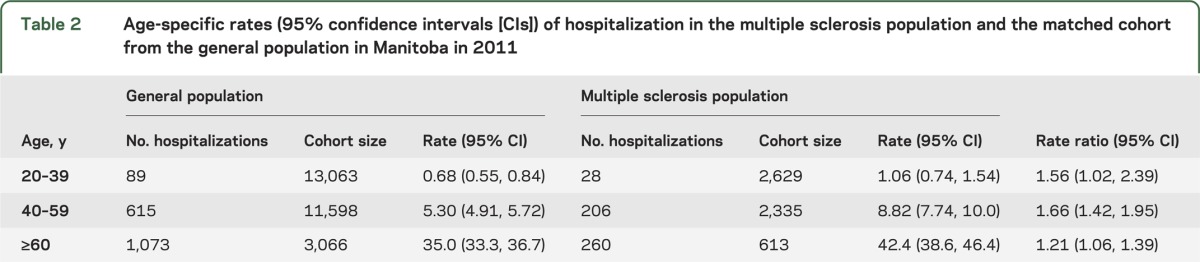
Table 3.
Association of calendar year with hospitalization rate adjusted for age, sex, and socioeconomic status at the time of admission

Compared to 2010–2011, the risks of hospitalization in the MS population were 2-fold higher in 1984–1989, while they were 1.3-fold higher in the matched population. In the MS population, older age and lower SES were associated with higher hospitalization rates. The magnitude of the associations between hospitalizations and age and SES differed in the matched population. Although persons with MS aged ≥60 years had only 1.5-fold the hospitalization rate of persons <40 years, persons in the matched population aged ≥60 years had 3-fold the hospitalization rate.
Reasons for hospitalization.
In the MS population, 20.6% of 14,061 hospitalizations over the study period were MS-related, 4.6% were possibly MS-related, and 74.8% were non–MS-related. Hospital admissions for MS-related reasons declined annually at a similar rate (−0.39; −0.46, −0.32) to hospitalizations for non–MS-related reasons (−0.37; −0.44, −0.30, see figure e-1). The annual proportion of admissions for MS-related reasons decreased from 43.4% in 1984 to 7.8% in 2011. An individual with MS who was hospitalized in 1984–1989 was 80% less likely to be admitted for reasons unrelated to MS than in 2010–2011 (table e-2). Older age was associated with increased odds of being admitted for non–MS-related rather than MS-related reasons.
As for all-cause hospitalizations, we evaluated temporal trends in rates of hospitalization for MS-related reasons in a regression model (table 3). Hospitalization rates were 8-fold higher in 1984–1989 than in 2010 or later. These temporal trends persisted after adjusting for sex, age, SES, and other health care utilization (table e-1), or when MS-related admissions were defined solely by the primary discharge diagnosis (table e-3). After adjusting for year, sex was not associated with rates of hospitalization for MS-related reasons. Compared to persons <40 years of age, persons aged ≥60 years were less likely to be hospitalized for MS-related reasons. A slightly steeper dose-response relationship was observed between MS-related hospitalization rates and lower SES than we observed for all-cause hospitalizations.
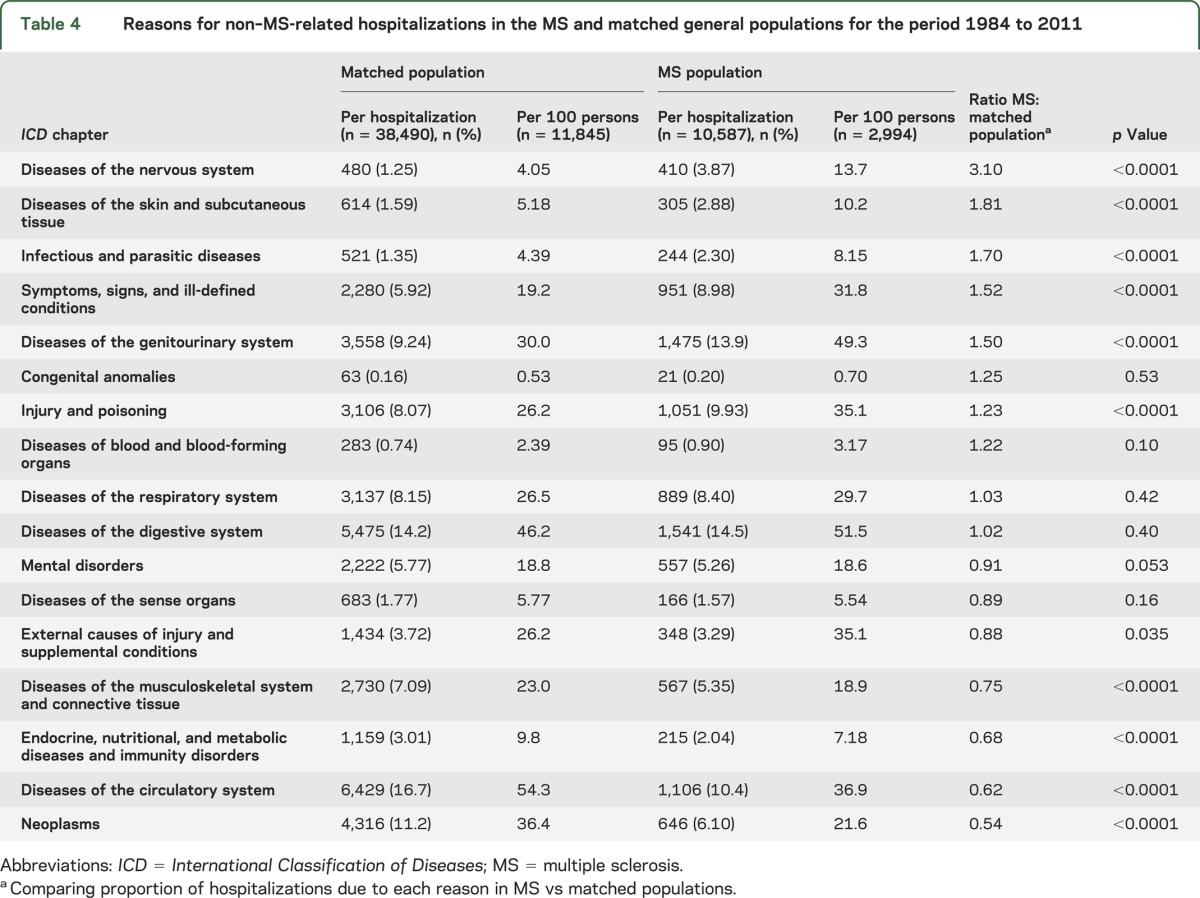
We further classified the non–MS-related hospitalizations over the entire study in both populations according to ICD-9 chapters (table 4). The 3 most common reasons for admission in the MS population were diseases of the digestive, genitourinary, and circulatory systems. In the matched controls, the most common reasons for admission were diseases of the circulatory and digestive systems, and neoplasms. Compared to the matched population, the MS population was more likely to be hospitalized for diseases of the nervous system, skin conditions, infections, diseases of the genitourinary system, and injury. We then evaluated admissions for bacterial pneumonia, influenza, urinary tract infections, and pressure ulcers; all occurred more often in the MS population (table e-4). However, the MS population was less likely to be hospitalized for several conditions, most notably diseases of the circulatory system and neoplasms. In further evaluating the disparity in admissions for circulatory system diseases, we found that the MS population was 33% less likely to be admitted for cardiac revascularization procedures than the matched population (p < 0.0001, table e-4).
Table 4.
Reasons for non–MS-related hospitalizations in the MS and matched general populations for the period 1984 to 2011
Length of stay.
The mean (SD) LOS for all inpatient hospitalizations from 1984 through 2011 was longer in the MS population than in the matched population (table 1). Mean LOS for all hospitalizations declined more over time in the MS population (−0.11 days/year) than in the matched population (−0.069 days/year). Given the differences observed, we categorized admissions according to LOS (1–8, 9–15, 16–22, ≥23 days). In the MS population, the proportion of admissions that were 1–8 days long increased from 41.5% in 1984–1988 to 50.9% in 2007–2011, and the proportion of longest stay admissions decreased from 9.80% to 6.09%. In the matched population, the proportion of shortest stay admissions increased from 53.2% in 1984–1988 to 63.6% in 2007–2011, and the proportion of longest stay admissions decreased from 5.80% to 5.02%.
In the MS population, LOS was longer for MS-related admissions (12.4 [11.9]) than for admissions that were possibly MS-related (8.4 [8.2]) or not MS-related (8.3 [9.7], p < 0.0001). The difference in the LOS between MS-related and non–MS-related admissions persisted over time (figure e-2). The proportion of MS-related admissions that were 1–8 days long increased from 38.3% in 1984–1988 to 58.0% in 2007–2011, while the proportion of longest stay admissions decreased from 19.2% to 15.5% (data not shown). Changes in LOS for non–MS-related reasons were less dramatic. The proportion of non–MS-related admissions that were 1–8 days long increased from 62.1% in 1984–1988 to 70.5% in 2007–2011, while the proportion of longest stay admissions decreased from 9.25% to 7.83%.
DISCUSSION
Hospitalizations are the biggest component of health resource use in industrialized countries, including Canada, a nation with universal health care.18–21 In 2000–2001, 11 neurologic diseases accounted for 6.7% of the total attributable cost of illness and nearly 10% of hospitalizations in Canada.24 We found that 56.8% of the MS population was hospitalized during the more than 25-year study period, excluding admissions related to pregnancy and long-term care, substantially exceeding the frequency of hospitalizations in the matched population. All-cause hospitalization rates declined more over time in the MS population than in the matched population, and individuals with MS were less likely to be admitted for MS-related reasons over time.
In both populations older age was associated with increased all-cause hospitalization rates, consistent with expectations in the general population14 and with prior reports in the MS population in British Columbia, Canada.13 However, older age was not associated with increased hospitalizations for MS-related reasons. Lower SES was associated with increased rates of all-cause hospitalizations in both populations and with MS-related hospitalizations in the MS population. Even in countries with universal health care, SES is associated with health care utilization in the general population.25 In a Swedish study of MS-related hospitalizations, the risk of hospitalization was slightly lower among men (standardized incidence ratio 0.83; 0.73–0.94) and women (0.91; 0.84–0.98) with higher levels of education.26 Given that both Sweden and Canada have universal health care, the stronger relationship we observed may reflect the use of income rather than education as a measure of SES.
All-cause hospitalizations declined sharply in the MS population over time, and the observed declines exceeded those observed in an age-, sex-, and geographically matched cohort from the general population. In the general population, age-standardized acute care hospitalization rates and LOS across Canada have declined over the last 10 years.14 The delivery of care has changed over time; for example, many elective surgeries have shifted from inpatient to outpatient day surgery settings. Admission rates for cardiovascular and cerebrovascular disease have declined as have in-hospital mortality rates, suggesting improvements in care for some conditions27 and improved community supports.28 In the MS population, the rates of decline in hospitalizations were similar for both MS-related and non–MS-related reasons; however, the proportion of MS-related admissions was lower in 2011 than in 1984. The most substantial declines in hospitalization rates preceded the introduction of disease-modifying therapies; thus, the observed declines may reflect changes in health care delivery, including administration of IV therapy for relapses in the outpatient rather than the inpatient setting, increased use of home care services, or improved symptom management. A study from British Columbia, Canada found that all-cause hospitalizations in the MS population decreased 1.4% annually over the period 1986 to 2008; MS-related hospitalizations also declined. However, an American study reported that the annual number of admissions with MS as the primary or secondary diagnosis increased from 102,473 in 2001 to 144,716 in 2010. However, the findings of this study are difficult to interpret since they lacked knowledge of the prevalence of MS and could not calculate hospitalization rates. A rise in the prevalence of MS, as reported elsewhere,29 could lead to an apparent increase in number of admissions without an increase in rates.
We also found that hospital LOS declined over time in the MS population, consistent with an American study but contrasting with findings from British Columbia.6,13 The reasons for the discrepancy are uncertain but may reflect differences in the hospitalizations studied or the proportion of admissions for MS-related reasons. We excluded hospitalizations for pregnancy and long-term care. The proportion of admissions that were short (1–8 days long) increased 20% for MS-related reasons and 8.4% for non–MS-related reasons; therefore, the most dramatic changes in LOS have been for MS-related admissions.
Admissions for bacterial pneumonia, influenza, urinary tract infections, and pressure ulcers were more common in the MS population than in the matched population, consistent with findings in Sweden30 and reported higher risks of pneumonia, pressure ulcers, and urinary tract infections on death certificates of the MS population compared to the general population.31 This suggests that specific efforts to prevent these conditions are warranted. Admissions for cancer and circulatory system diseases were lower in the MS population. The lower frequency of admissions for cancer is consistent with the lower reported incidence of cancer in the MS population.32 However, the lower frequency of admissions for circulatory diseases was not. We previously reported an increased incidence and prevalence of ischemic heart disease in the MS population but did not examine hospitalizations for ischemic heart disease specifically.33 Two American studies reported that hospitalizations for ischemic heart disease occurred less often than expected in persons with MS.34,35 Our finding that cardiac revascularization procedures were less common in the MS population raises questions regarding differences in disease severity or in perceived procedural risks.
Limitations of this study should be considered. We lacked clinical data regarding such factors as disability status. We also lacked individual level measures of SES, but the area-based measures of SES we used are associated with health status36 and give similar results to individual level measures when geographic units are small and capture a homogenous population.37 Also, we did not evaluate the impact of such therapies on changes in hospitalization rates at the individual level. Although this is an important issue, it would require a different study design. We also did not evaluate the impact of specific comorbidities on hospitalization rates due to challenges in consistently identifying comorbidities over the entire study period. Nervous system disorders were a more common non–MS-related reason for admission in the MS population, suggesting that some admissions that were classified as non–MS-related may have been MS-related. However, several nervous system disorders such as stroke and migraine would be expected to occur in the MS population.38–40 Since nervous system disorders accounted for <4% of all non–MS-related admissions over more than 25 years, it is unlikely that any misclassification influenced our findings. Findings may differ in other regions and replication is needed. Strengths of this study include the population-based design, the use of a matched cohort from the general population for comparisons, and the study duration.
Hospitalization rates have declined dramatically in the MS population over time, exceeding the declines in hospitalizations in the general population. As MS-related admissions accounted for fewer than 8% of admissions in 2011, efforts to further reduce hospitalizations will need to be directed at preventing complications such as infection.
Supplementary Material
GLOSSARY
- CI
confidence interval
- ICD-9-CM
International Classification of Diseases, 9th revision, Clinical Modification
- ICD-10-CA
International Classification of Diseases, 10th revision, Canadian enhancement
- LOS
length of stay
- MS
multiple sclerosis
- RR
rate ratio
- SES
socioeconomic status
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
The corresponding author (R.A.M.) and analyst (A.T.) had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Ruth Ann Marrie, Nancy Yu, Lawrence Elliott, and James Blanchard designed the study and obtained funding. All authors contributed to the analysis and interpretation of the data. Ruth Ann Marrie drafted the manuscript. All authors revised the manuscript and approved of the final version to be published.
STUDY FUNDING
Supported (in part) by operating grants and a Don Paty Career Development Award from the MS Society of Canada. The results and conclusions presented are those of the authors. No official endorsement by Manitoba Health is intended or should be inferred.
DISCLOSURE
R. Marrie receives research funding from Canadian Institutes of Health Research, Public Health Agency of Canada, Manitoba Health Research Council, Health Sciences Centre Foundation, Multiple Sclerosis Society of Canada, Multiple Sclerosis Scientific Foundation, and Rx & D Health Research Foundation; and has conducted clinical trials funded by sanofi-aventis. L. Elliott receives research support from the Canadian Institutes of Health Research, Public Health Agency of Canada, and the Multiple Sclerosis Society of Canada. J. Marriott received research support for MS trials from Biogen Idec, Roche, and sanofi-aventis and honoraria from Biogen Idec, Roche, and EMD Serono. He has received research support from the Consortium of MS Centers and the Manitoba Medical Service Foundation. M. Cossoy has received an honorarium for educational activities from EMD Serono. J. Blanchard receives research support from the Multiple Sclerosis Society of Canada, CIHR, Bill & Melinda Gates Foundation, Canadian International Development Agency, and the United States Agency for International Development. A. Tennakoon reports no disclosures relevant to the manuscript. N. Yu receives research support from the Canadian International Development Agency, the Multiple Sclerosis Society of Canada, CIHR, and Manitoba Health. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Marrie RA, Cutter G, Tyry T, Hadjimichael O, Campagnolo D, Vollmer T. Changes in the ascertainment of multiple sclerosis. Neurology 2005;65:1066–1070 [DOI] [PubMed] [Google Scholar]
- 2.Kingwell E, Leung AL, Roger E, Duquette P, Rieckmann P, Tremlett H. Factors associated with delay to medical recognition in two Canadian multiple sclerosis cohorts. J Neurol Sci 2010;292:57–62 [DOI] [PubMed] [Google Scholar]
- 3.The IFNB Multiple Sclerosis Study Group. Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. Neurology 1993;43:655–661 [DOI] [PubMed] [Google Scholar]
- 4.Rudick RA, Stuart WH, Calabresi PA, et al. Natalizumab plus interferon beta-1a for relapsing multiple sclerosis. N Engl J Med 2006;354:911–923 [DOI] [PubMed] [Google Scholar]
- 5.Marrie RA, Yu N, Wei Y, Elliott L, Blanchard J. High rates of physician services utilization at least five years before multiple sclerosis diagnosis. Mult Scler J 2013;19:1113–1119 [DOI] [PubMed] [Google Scholar]
- 6.Lad S, Chapman C, Vaninetti M, Steinman L, Green A, Boakye M. Socioeconomic trends in hospitalization for multiple sclerosis. Neuroepidemiology 2010;35:93–99 [DOI] [PubMed] [Google Scholar]
- 7.Stolp-Smith KA, Atkinson EJ, Campion ME, O'Brien PC, Rodriguez M. Health care utilization in multiple sclerosis. Neurology 1998;50:1594–1600 [DOI] [PubMed] [Google Scholar]
- 8.Pope GC, Urato CJ, Kulas ED, Kronick R, Gilmer T. Prevalence, expenditures, utilization, and payment for persons with MS in insured populations. Neurology 2002;58:37–43 [DOI] [PubMed] [Google Scholar]
- 9.Kobelt G, Berg J, Lindgren P, Fredrikson S, Jonsson B. Costs and quality of life of patients with multiple sclerosis in Europe. J Neurol Neurosurg Psychiatry 2006;77:918–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asche CV, Singer ME, Jhaveri M, Chung H, Miller A. All-cause health care utilization and costs associated with newly diagnosed multiple sclerosis in the United States. J Manag Care Pharm 2010;16:703–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCrone P, Heslin M, Knapp M, Bull P, Thompson A. Multiple sclerosis in the UK: service use, costs, quality of life and disability. PharmacoEconomics 2008;26:847–860 [DOI] [PubMed] [Google Scholar]
- 12.Prescott JD, Factor S, Pill M, Levi GW. Descriptive analysis of the direct medical costs of multiple sclerosis in 2004 using administrative claims in a large nationwide database. J Manag Care Pharm 2007;13:44–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans C, Kingwell E, Zhu F, Oger J, Zhao Y, Tremlett H. Hospital admissions and MS: temporal trends and patient characteristics. Am J Manag Care 2012;18:735–742 [PubMed] [Google Scholar]
- 14.Canadian Institute for Health Information. Highlights of 2008–2009 Inpatient Hospitalizations and Emergency Department Visits. Ottawa, ON: CIHI; 2010 [Google Scholar]
- 15.Manitoba Bureau of Statistics. Manitoba's Population Trends Past, Present and Future. Winnipeg, MB: Manitoba Bureau of Statistics; 2008 [Google Scholar]
- 16.Health Information Management Branch. Population Report. Winnipeg, MB: Manitoba Health and Healthy Living; 2008 [Google Scholar]
- 17.Marrie RA, Yu N, Blanchard JF, Leung S, Elliott L. The rising prevalence and changing age distribution of multiple sclerosis in Manitoba. Neurology 2010;74:465–471 [DOI] [PubMed] [Google Scholar]
- 18.Jacobs P, Noseworthy TW. National estimates of intensive care utilization and costs: Canada and the United States. Crit Care Med 1990;18:1282–1286 [DOI] [PubMed] [Google Scholar]
- 19.Sirio CA, Tajimi K, Taenaka N, Ujike Y, Okamoto K, Katsuya H. A cross-cultural comparison of critical care delivery: Japan and the United States. Chest 2002;121:539–548 [DOI] [PubMed] [Google Scholar]
- 20.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med 2008;36:2787–2793 [DOI] [PubMed] [Google Scholar]
- 21.Halpern NA, Bettes L, Greenstein R. Federal and nationwide intensive care units and healthcare costs: 1986–1992. Crit Care Med 1994;22:2001–2007 [PubMed] [Google Scholar]
- 22.Longobardi T, Bernstein CN. Health care resource utilization in IBD. Clin Gastroenterol Hepatol 2006;4:731–743 [DOI] [PubMed] [Google Scholar]
- 23.Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med 2003;163:101–106 [DOI] [PubMed] [Google Scholar]
- 24.Canadian Institute for Health Information. The Burden of Neurological Diseases, Disorders and Injuries in Canada. Ottawa, Canada: Canadian Institute for Health Information; 2007 [Google Scholar]
- 25.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med 1999;341:1359–1367 [DOI] [PubMed] [Google Scholar]
- 26.Li X, Hemminki K, Sundquist K. Regional, socioeconomic and occupational groups and risk of hospital admission for multiple sclerosis: a cohort study in Sweden. Mult Scler 2008;14:522–529 [DOI] [PubMed] [Google Scholar]
- 27.Tu JV, Nardi L, Fang J, et al. National trends in rates of death and hospital admissions related to acute myocardial infarction, heart failure and stroke, 1994–2004. Can Med Assoc J 2009;180:E118–E125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roos N, Stranc L, Peterson S, Mitchell L, Bogdanovic B, Shapiro E. A Look at Home Care in Manitoba. Winnipeg, MB: Manitoba Centre for Health Policy and Evaluation; 2001 [Google Scholar]
- 29.Evans C, Beland S, Kulaga S, et al. Incidence and prevalence of multiple sclerosis in the Americas: a systematic review. Neuroepidemiology 2013;40:195–210 [DOI] [PubMed] [Google Scholar]
- 30.Montgomery S, Hillert J, Bahmanyar S. Hospital admission due to infections in multiple sclerosis patients. Eur J Neurol 2013;20:1153–1160 [DOI] [PubMed] [Google Scholar]
- 31.Redelings MD, McCoy L, Sorvillo F. Multiple sclerosis mortality and patterns of comorbidity in the United States from 1990 to 2001. Neuroepidemiology 2006;26:102–107 [DOI] [PubMed] [Google Scholar]
- 32.Kingwell E, Bajdik C, Phillips N, et al. Cancer risk in multiple sclerosis: findings from British Columbia, Canada. Brain 2012;135:2973–2979 [DOI] [PubMed] [Google Scholar]
- 33.Marrie RA, Yu BN, Leung S, et al. Prevalence and incidence of ischemic heart disease in multiple sclerosis: a population-based validation study. Mult Scler Relat Disord 2013;2:355–361 [DOI] [PubMed] [Google Scholar]
- 34.Allen NB, Lichtman JH, Cohen HW, Fang J, Brass LM, Alderman MH. Vascular disease among hospitalized multiple sclerosis patients. Neuroepidemiology 2008;30:234–238 [DOI] [PubMed] [Google Scholar]
- 35.Fleming ST, Blake RL., Jr Patterns of comorbidity in elderly patients with multiple sclerosis. J Clin Epidemiol 1994;47:1127–1132 [DOI] [PubMed] [Google Scholar]
- 36.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992;82:703–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mustard CA, Derksen S, Berthelot JM, Wolfson M. Assessing ecologic proxies for household income: a comparison of household and neighbourhood level income measures in the study of population health status. Health & Place 1999;5:157–171 [DOI] [PubMed] [Google Scholar]
- 38.Christiansen CF, Christensen S, Farkas DK, Miret M, Sørensen HT, Pedersen L. Risk of arterial cardiovascular diseases in patients with multiple sclerosis: a population-based cohort study. Neuroepidemiology 2010;35:267–274 [DOI] [PubMed] [Google Scholar]
- 39.Jadidi E, Mohammadi M, Moradi T. High risk of cardiovascular diseases after diagnosis of multiple sclerosis. Mult Scler J 2013;19:1336–1340 [DOI] [PubMed] [Google Scholar]
- 40.Putzki N, Pfriem A, Limmroth V, et al. Prevalence of migraine, tension-type headache and trigeminal neuralgia in multiple sclerosis. Eur J Neurol 2009;16:262–267 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


