Abstract
Multiple lines of evidence suggest that the Sonic Hedgehog (Shh) signaling pathway is aberrantly reactivated in pancreatic cancer stem cells (CSCs). The objectives of this study were to examine the molecular mechanisms by which GANT-61 (Gli transcription factor inhibitor) regulates stem cell characteristics and tumor growth. Effects of GANT-61 on CSC’s viability, spheroid formation, apoptosis, DNA-binding and transcriptional activities, and epithelial-mesenchymal transition (EMT) were measured. Humanized NOD/SCID/IL2Rgammanull mice were used to examine the effects of GANT-61 on CSC’s tumor growth. GANT-61 inhibited cell viability, spheroid formation, and Gli-DNA binding and transcriptional activities, and induced apoptosis by activation of caspase-3 and cleavage of Poly-ADP ribose Polymerase (PARP). GANT-61 increased the expression of TRAIL-R1/DR4, TRAIL-R2/DR5 and Fas, and decreased expression of PDGFRα and Bcl-2. GANT-61 also suppressed EMT by up-regulating E-cadherin and inhibiting N-cadherin and transcription factors Snail, Slug and Zeb1. In addition, GANT-61 inhibited pluripotency maintaining factors Nanog, Oct4, Sox-2 and cMyc. Suppression of both Gli1 plus Gli2 by shRNA mimicked the changes in cell viability, spheroid formation, apoptosis and gene expression observed in GANT-61-treated pancreatic CSCs. Furthermore, GANT-61 inhibited CSC tumor growth which was associated with up-regulation of DR4 and DR5 expression, and suppression of Gli1, Gli2, Bcl-2, CCND2 and Zeb1 expression in tumor tissues derived from NOD/SCID IL2Rγ null mice. Our data highlight the importance of Shh pathway for self-renewal and metastasis of pancreatic CSCs, and also suggest Gli as a therapeutic target for pancreatic cancer in eliminating CSCs.
Keywords: Pancreatic cancer stem cells, GANT-61, Sonic hedgehog, Gli transcription factor
1. Introduction
Cancer stem cells (CSCs) comprise a subset of hierarchically organized, rare cancer cells with the ability to initiate cancer in genetically modified murine models [1; 2]. CSCs may be responsible for tumor onset, self-renewal/maintenance, mutation accumulation, and metastasis [3; 4]. The existence of CSCs in pancreatic cancer could explain the high frequency of cancers relapse and resistance to chemotherapy. Several lines of evidence indicate that Sonic Hedgehog (Shh) signaling system plays a key role in CSC biology. In general, it plays an essential role in the regulation of CSCs self-renewal, differentiation, and tumorigenic potential, suggesting Shh signaling could be a promising therapeutic target in pancreatic cancer. Inhibition of Shh signaling may abrogate the resistance of CSCs to chemotherapy and could lead to the development of novel therapeutic approaches for the treatment of pancreatic cancer.
During embryonic development, conserved signaling pathways such as Hedgehog (Hh), Wingless (Wnt) and Notch regulate morphogenesis by dictating cell fate decisions such as self-renewal and differentiation. These pathways are subsequently silenced in most adult tissues but frequently reactivated in a wide range of human malignancies. Recent evidence suggests that the Shh signaling pathway [5] is aberrantly reactivated and recognized as one of the mediators in the majority of pancreatic cancers, and that hedgehog blockade has the potential to prevent disease progression and metastatic spread [6]. The binding of short-acting polypeptide ligands (namely; Shh, Ihh, or Dhh) to the Patched receptor diminishes its inhibitory effects on Smoothened, allowing signal transduction through the Shh pathway that results in activation and nuclear translocation of Gli family transcription factors (Gli1 and Gli2). Shh is a morphogen required for proper pattern formation during embryogenesis; however, deregulation of this pathway is responsible for several human cancers, syndromes and malformations [7]. Shh signaling is also critical in the regulation of cellular proliferation, cellular survival, stemness, and cell fate determination in a variety of organs [6]. Multiple lines of evidence support the idea that Shh signaling has a role in normal pancreas development and there is mounting evidence that dysregulated Shh signaling plays some role in pancreatic cancer [8]. Increased Hh signaling has been described in a wide range of other human cancers, including chronic myeloid leukemia (CML), multiple myeloma (MM), glioblastoma, prostate cancer, breast cancer and small cell lung cancer.
The Gli family of transcription factors has dual functions such as activator and repressor, and can respond to combinatorial and cooperative Gli activity. They play critical roles in the mediation and interpretation of Shh signals [9]. Shh-driven cancers arise from a variety of mutations that affect different components, including the key transcriptional effector Gli proteins, and lead to a variety of human malignancies including medulloblastoma, rhabdomyosarcoma, melanoma, basal cell carcinoma, and breast, lung, liver, stomach and prostate cancers [10; 11; 12; 13]. However, very little is known regarding the specific role of Shh signaling in maintaining pancreatic CSC characteristics, and the downstream target genes involved in determination of cell fate. In comparison to Gli1, a little is known about the role of Gli2-mediated Shh signaling in tumors [14]. Gli2 is mostly regarded as a primary transcriptional activator of Shh signaling, even though it is also suggested to have a weak repressing activity. With Gli1 as a transcriptional target of Gli2, this may amplify Shh induced Gli2-mediated transcription of Gli1 target genes [15]. Gli1 and Gli2 also induce transcription of overlapping and distinct sets of target genes which regulate cell proliferation, cell cycle, cell survival and metastasis [16; 17; 18; 19; 20]. However, the roles of Shh pathway in maintaining pluripotency of pancreatic CSCs are unknown.
The majority of mitogenic/oncogenic signal-activated signaling pathways stimulate epithelial-mesenchymal transition (EMT), a complex reprogramming process which plays an indispensable role in tumor invasion and metastasis [21]. The main features of EMT include loss of epithelial markers (α- and γ-catenin and E-cadherin), gain of mesenchymal cell markers (fibronectin, N-cadherin and vimentin), and the acquisition of migratory and invasive properties [22]. Currently, studies show that EMT is controlled by a group of transcriptional repressors, such as Snail, Slug, Twist1 and Zeb1/2. Upon activation, these repressors recruit histone deacetylases to the E-box elements of the E-cadherin promoter, resulting in transcriptional silencing of E-cadherin expression [23].
The main objective of this paper is to examine the molecular mechanisms by which GANT-61 (Gli transcription inhibitor) regulate pancreatic cancer stem cell characteristics and tumor growth. Our data demonstrated that GANT-61 inhibited pancreatic CSC proliferation and self-renewal, and induced apoptosis. In further detailed analyses of pancreatic CSCs, GANT-61 decreased both Gli1 and Gli2 expressions, and Gli-DNA binding and Gli-luciferase reporter activities. Furthermore, GANT-61 decreased the expression of PDGFRα concomitant with elevated levels of Fas, increased the expressions of TRAIL-R1/DR4 and TRAIL-R2/DR5, decreased Bcl-2 expression, and induced cleavage of caspase-3 and PARP. In addition, GANT-61-induced changes in gene expression related to self- renewal, proliferation and apoptosis were modulated by Gli1 plus Gli2 shRNA, thus pointing a role of Shh pathway in modulating pancreatic CSC characteristics. Most importantly, GANT-61 inhibited CSC tumor growth in the NOD/SCID IL2Rγ null mice. These data suggest that GANT-61 suppresses pancreatic CSC characteristics and tumor growth by modulating genes involved in cell proliferation, self-renewal and metastasis, and thus can be used as a potential chemotherapeutic agent for the treatment of human pancreatic cancer.
2. Materials and Methods
2.1. Reagents
Antibodies against Shh, Smoothened, Fas, TRAIL-R1/DR4, TRAIL-R2/DR5, and β-actin were purchased from Santa Cruz Biotechnology Inc. (Santa Cruz, CA). Antibodies against Gli1, Gli2, Patched-1, Patched-2, Cyclin D2, Zeb1, PDGFRα, PARP and caspase-3 were obtained from Cell Signaling Technology (Danvers, MA). GANT-61 (2,2′-[[Dihydro-2-(4-pyridinyl)-1,3(2H,4H)-pyrimidinediyl]bis(methylene)]bis[N,N-dimethylbenzenamine) was purchased from Tocris (Ellisville, MO). All other chemicals used were of analytical grade and were purchased from Fisher Scientific (Suwanee, GA) and Sigma-Aldrich (St. Louis, MO).
2.2. Cell culture
Human pancreatic CSCs (CD133+/CD44+/CD24+/ESA+) were isolated from primary tumors as we described previously [24]. The CSCs were cultured in pancreatic cancer stem cell growth medium (Celprogen) with 1% N2 Supplement (Invitrogen), 2% B27 Supplement (Invitrogen), 20 ng/ml human platelet growth factor (Sigma-Aldrich), 100 ng/ml epidermal growth factor (Invitrogen) and 1% antibiotic-antimycotic (Invitrogen) at 37 °C in a humidified atmosphere of 95% air and 5% CO2.
2.3. Lentiviral particle production and Gli1 and Gli2 shRNA transduction
Gli1 shRNA (5′-GCCTGAATCTGTGTATGAA-3′; 5′-GTTTGAATCTGAATGCTAT-3′; 5′-AGCTAGAGTCCAGAGGTTC-3′; 5′-CCGGAGTGCAGTCAAGTTG-3′ and 5′-GGCTGGACCAGCTACATCA-3′) and Gli2 shRNA (5′-CCGAGAAGCAAGAAGCCAA-3′; 5′-CACAGCATGCTCTACTACT-3′; 5′-TCGCTAGTGGCCTACATCA-3′; 5′-TCCGAGAAGCAAGAAGCCA-3′ and 5′-CCAGACGACGTGGTGCAGT-3′) were obtained from Open Biosystems, Huntsville, AL) and cloned into TRIPZ vector. Lentivirus was produced by triple transfection of HEK 293T cells. Packaging 293T cells were plated in 10-cm plates at a cell density of 5 × 106 a day prior to transfection in DMEM containing 10% heat-inactivated fetal bovine serum without antibiotics. Transfection of packaging cells and infection of pancreatic CSCs were carried out using standard protocols [25] with some modifications. In brief, 293T cells were transfected with 4 μg of plasmid and 4 μg of lentiviral vector using lipid transfection (Lipofectamine-2000/Plus reagent, Invitrogen) according to the manufacturer’s protocol. Viral supernatants were collected and concentrated by adding PEG-it virus precipitation solution (SBI System Biosciences) to produce virus stocks with titers of 1 × 108 to 1 × 109 infectious units per ml. Viral supernatant was collected for three days by ultracentrifugation and concentrated 100-fold. Titers were determined on 293T cells. Pancreatic CSCs were transduced with lentivirus expressing scrambled shRNA (control), Gli1 shRNA, or Gli2 shRNA. Pancreatic CSCs simultaneously expressing both Gli1 plus Gli2 shRNA were also generated. Following transduction, the CSCs were washed 3 times with 1X PBS and allowed to grow for 3 passages before screening for gene expression. Once decreased expression of the targeted gene was confirmed, the cells were used for experiments. Stable expression of Gli1 ShRNA or Gli2 shRNA was ensured by culturing cells in the presence of a selection antibiotic puromycin (6.0 μg/ml), whereas induction of both Gli1 shRNA and Gli2 shRNA was performed in the presence of doxycycline (2.0 μg/ml). The transduced CSCs were washed three times with PBS (without Ca++ or Mg++) and used for experiments.
2.4. Cell viability and apoptosis assays
Cells (1.5 × 104) were incubated with 0, 1, 5 and 10 μM of GANT-61 in 250 μl of culture medium in 96-well plate for 48 and 72 h. Cell viability was determined by the XTT assay. In brief, a freshly prepared XTT-PMS labeling mixture (50 μl) was added to the cell culture. The absorbance was measured at 450 nm with λ correction at 650 nm. The cell viability was expressed as ΔOD (OD450 − OD650). The apoptosis was determined by FACS analysis of propidium iodide (PI)-stained cells. In brief, cells were trypsinized, washed with PBS and resuspended in 200 μl PBS with 10 μl RNAase (10 mg/ml) and incubated at 37 °C for 30 min. After incubation, 50 μl PI solution was added and cells were analyzed for apoptosis using a flow cytometry (Accuri C6 flow cytometer, BD Biosciences, San Jose, CA).
2.5. Tumor spheroid assay
For spheroid forming assay, cells were plated in six-well ultralow attachment plates (Corning Inc., Corning, NY) at a density of 1,000 cells/ml in stem cell growth medium with 1% N2 Supplement (Invitrogen), 2% B27 Supplement (Invitrogen), 20 ng/ml human platelet growth factor (Sigma-Aldrich), 100 ng/ml epidermal growth factor (Invitrogen) and 1% antibiotic-antimycotic (Invitrogen) at 37 °C in a humidified atmosphere of 95% air and 5% CO2. Spheroids were collected after 7 days and dissociated with Accutase (Innovative Cell Technologies, Inc.). The CSCs obtained from dissociation were counted by coulter counter using trypan blue dye.
2.6. Motility assay
Scratch migration assay was used to study the horizontal movement of cells. A confluent monolayer of cells was established and then a scratch is made through the monolayer, using a standard 200 μl plastic pipette tip, which gives rise to an in vitro wound, washed twice with PBS, and replaced in media with or without GANT-61. Cancer stem cells migrate into the scratch area as single cells from the confluent sides. The width of the scratch gap is viewed under the microscope in four separate areas each day until the gap is completely filled in the untreated control wells. Three replicate wells from a 6-well plate were used for each experimental condition.
2.7. Transwell migration assay
For transwell migration assays, 1 × 105 pancreatic CSCs were plated in the top chamber onto the noncoated membrane (24-well insert; pore size, 8 μm; Corning Costar) and allowed to migrate toward serum-containing medium in the lower chamber. Cells were fixed after 24 hours of incubation with methanol and stained with 0.1% crystal violet (2 mg/ml, Sigma-Aldrich). The number of cells invading through the membrane was counted under a light microscope (three random fields per well).
2.8. Transwell invasion assay
For invasion assay, 1 × 105 cells were plated in the top chamber onto the Matrigel coated Membrane (24-well insert; pore size, 8 μm; Corning Costar). Each well was coated freshly with Matrigel (60 μg; BD Bioscience) before the invasion assay. Pancreatic CSCs were plated in medium without serum or growth factors, and medium supplemented with serum was used as a chemoattractant in the lower chamber. The cells were incubated for 48 hours and cells that did invade through the pores were removed by a cotton swab. CSCs on the lower surface of the membrane were fixed with methanol and stained with crystal violet. The number of cells invading through the membrane was counted under a light microscope (40X, three random fields per well).
2.9. Western blot analysis
Pancreatic CSCs were treated with GANT-61 for various time points. At the end of incubation period, cell lysates were prepared using RIPA lysis buffer containing 1 X protease inhibitor cocktail. Cell lysates containing 50 μg of protein were loaded and separated on 10% Tris-HCl gel. Proteins from the gel were transferred on polyvinylidene difluoride membranes and subsequently blocked in blocking buffer [5% nonfat dry milk in 1 X Tris Buffer Saline (TBS)] and incubated overnight with primary antibodies. Membranes were washed three times with TBS-T for 10, 5, and 5 min each. After washing, membranes were incubated with secondary antibodies conjugated with horseradish peroxidase at 1:5,000 dilution in TBS for 1 h at room temperature. Membranes were again washed three times in TBS-T and developed using ECL Substrate. Protein bands were visualized on X-ray film using an enhanced chemiluminescence system.
2.10. Quantitative real-time PCR
Total RNA was isolated using an RNeasy Mini Kit (Qiagen, Valencia, CA). Briefly, cDNA was synthesized using a high capacity cDNA reverse transcription kit (Applied Biosystems). Primers specific for each of the signaling molecules were designed using NCBI/Primer-BLAST and used to generate the PCR products. For the quantification of gene amplification, Real-time PCR was performed using an ABI 7300 Sequence Detection System in the presence of SYBR- Green. The following gene-specific primers were used:
Smoothened (5′-TCG CTA CCC TGC TGT TAT TC-3′, 5′-GAC GCA GGA CAG AGT CTC AT-3′)
Patched1 (5′-TGA CCT AGT CAG GCT GGA AG-3′, 5′-GAA GGA GAT TAT CCC CCT GA-3′)
Patched2 (5′-AGG AGC TGC ATT ACA CCA AG-3′, 5′-CCC AGG ACT TCC CAT AGA GT-3′)
Gli1 (5′-CTG GAT CGG ATA GGT GGT CT -3′, 5′-CAG AGG TTG GGA GGT AAG GA-3′)
Gli2 (5′-GCC CTT CCT GAA AAG AAG AC -3′, 5′-CAT TGG AGA AAC AGG ATT GG-3′)
Myc (5′-CGA CGA GAC CTT CAT CAA AA-3′, 5′-TGC TGT CGT TGA GAG GGT AG-3′
Nanog (5′-ACC TAC CTA CCC CAG CCT TT-3′, 5′-CAT GCA GGA CTG CAG AGA TT-3′)
Sox2 (5′-AAC CCC AAG ATG CAC AAC TC-3′, 5′-GCT TAG CCT CGT CGA TGA AC-3′)
Oct4 (5′-GGA CCA GTG TCC TTT CCT CT-3′, 5′-CCA GGT TTT CTT TCC CTA GC-3′)
Snail (5′ACC CCA CAT CCT TCT CAC TG-3′, 5′-TAC AAA AAC CCA CGC AGA CA-3′)
Slug (5′ACA CAC ACA CAC CCA CAG AG-3′, 5′-AAA TGA TTT GGC AGC AAT GT-3′)
Zeb1 (5′-GCA CAA CCA AGT GCA GAA GA-3′, 5′-CAT TTG CAG ATT GAG GCT GA-3′)
E-cadherin (5′-TGC TCT TGC TGT TTC TTC GG-3′, 5′-TGC CCC ATT CGT TCA AGT AG-3′)
N-cadherin (5′-TGG ATG GAC CTT ATG TTG CT-3′, 5′-AAC ACC TGT CTT GGG ATC AA-3′)
HK-GAPD (5′-GAG TCA ACG GAT TTG GTC GT-3′, 5′-TTG ATT TTG GAG GGA TCT CG-3′)
Target sequences were amplified at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. HK-GAPD was used as endogenous normalization control. All assays were performed in triplicate and were calculated on the basis of ΔΔCt method. The n-fold change in mRNAs expression was determined according to the method of 2−ΔΔCT.
2.11. Gli reporter assay
Gli reporter activity was measured as we described elsewhere [26]. In brief, cop-GFP and luciferase genes were cloned downstream of Gli-response element, containing four Gli binding motifs (pGreen Fire1-4xGli-mCMV-EF1-Neo). Pancreatic CSCs were transduced with lentiviral particles and stable cells were selected. For transcription assay, CSCs (5–10,000 cells per well) were seeded in 12-well plates and treated with or without GANT-61 (0–10 μM) for up to 48 h. After incubation, CSCs were harvested and analyzed for luciferase reporter activity (Promega Corp., Madison, WI).
2.12. Immunofluorescence
Pancreatic CSCs were grown on fibronectin-coated coverslips (Beckton Dickinson, Bedford, MA) in the presence or absence of GANT-61 (10 μM). Subsequently, cells were fixed with 4% paraformaldehyde for 15 min, permeabilized with 0.1% Triton X-100 in 1 X PBS, washed and blocked in 10% normal goat serum. After washing with PBS, cells were stained with Gli1 and Gli2 primary antibodies (1:100) for 16 h at 4 °C and washed with PBS. Afterwards, cells were incubated with fluorescently labeled secondary antibody (1:200) along with DAPI (1 mg/ml) for 1 h at room temperature. Finally, coverslips were washed and mounted using Vectashield (Vector Laboratories, Burlington, CA). Isotype-specific negative controls were included with each staining. Stained cells were mounted and visualized under a fluorescent microscope. Imunohistochemistry of pancreatic tumor tissues was performed as we described elsewhere [24].
2.13. Electrophorectic mobility shift assay
Electrophorectic mobility shift assay (EMSA) was performed as we described elsewhere [26]. In brief, Gli probes were end-labeled with [γ-32P] dATP by incubating oligodeoxyribonucleotide strands with 5 x reaction buffer and 10 U T4 polynucleotide kinase for 1 h at 37 °C. Then labeled oligonucleotides were allowed to anneal at room temperature for 10 min and 20 mg protein from each sample was used in 25 ml binding reactions, which consisted of 1 mg poly dI-dC, in 5 X binding buffer (50 mM Tris HCl; pH 8.0, 750 mM KCl, 2.5 mM EDTA, 0.5% Triton-X 100, 62.5% glycerol (v/v) and 1 mM DTT). To determine specificity of DNA binding, samples were incubated with or without 20 ng of unlabeled competitor DNA for 10 min at room temperature. Then 0.1 ng of labeled probe of Gli was added and samples were further incubated for 20 min at room temperature. Samples were separated on a 5% non-denaturing polyacrylamide gel in 0.5% TBE and visualized by autoradiography.
2.14. Antitumor activity of GANT-61
We used humanized NOD/SCID/IL2Rgammanull mice because these mice are better predictor for the biological response to therapy. Before CSC’s injection, mice were humanized with tail vein injection of human normal CD34+ peripheral blood stem/progenitor cells. CD34+ peripheral blood stem/progenitor cells (500 cells/mouse, 50–75 μl volume) were injected through tail vein. After 3 days, human pancreatic CSCs (1×103 cells mixed with Matrigel, Becton Dickinson, Bedford, MA, in 75 μl total volume, 50:50 ratio) were injected subcutaneously into the flanks of NOD/SCID IL2Rγnull mice (4–6 weeks old). Experiments were conducted under Celprogen’s approved IACUC protocol. After two weeks of CSC implantation, mice (10 mice per group) were treated with GANT-61(0 and 40 mg/kg body weight) ip three times per week for 6 weeks. At the end of the experiment, mice were euthanized, and tumors were isolated for biochemical analysis.
2.15. Statistical Analysis
The mean and SD were calculated for each experimental group. Differences between groups were analyzed by one or two way ANOVA, followed by Bonferoni’s multiple comparison tests using PRISM statistical analysis software (GrafPad Software, Inc., San Diego, CA). Significant differences among groups were calculated at P < 0.05.
3. Results
3.1. GANT-61 inhibits cell viability and induces apoptosis in pancreatic CSCs
We first measured the expression of various components of Shh pathway in pancreatic CSCs by qRT-PCR. Analyses of pancreatic CSCs showed consistent expression of components of Shh signaling pathway including the signaling molecules Smoothened, Patched-1, Patched-2, Gli1 and Gli2 and the ligand Shh (Fig. 1A). These data suggest that all the components of Shh pathway are expressed in pancreatic CSCs, and may respond to Shh pathway inhibition.
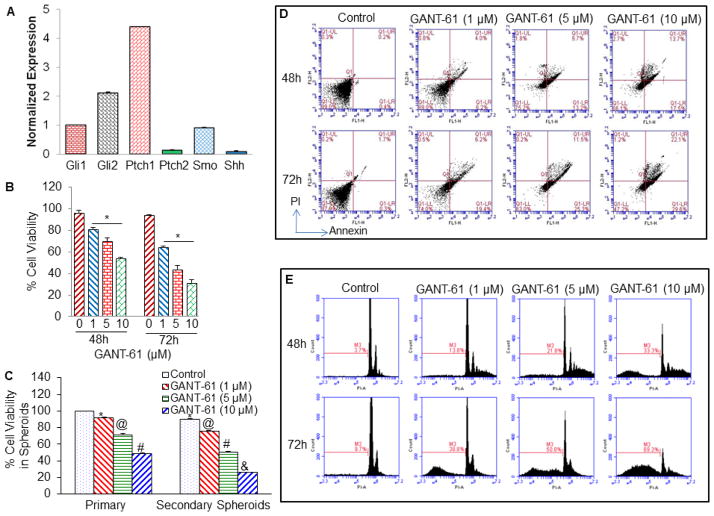
Fig. 1. Expression of components of Sonic Hedgehog (Shh) pathway, and the effects of GANT61 on cell viability, spheroid formation and apoptosis in pancreatic CSCs.
(A), Expression of various components of Shh pathway in pancreatic CSCs. Total RNA was isolated and expression of Gli-1, Gli-2, Patched-1, Patched-2, Smoothened, and Shh was measured by qRT-PCR. (B), Cell Viability in 2-D culture. CSCs were treated with GANT-61 (0, 1, 5 and 10 μM) for 48 and 72 h. At the end of incubation period, cell viability was measured as described in Materials and Methods. Data represent mean ± SD. @ and # significantly different from respective control (P < 0.05). (C), Cell Viability in Spheroids (3-D culture). Pancreatic CSCs were seeded in suspension and treated with GANT-61 (0–10 μM) for 7 days. At the end of incubation period, spheroids were collected, and dissociated with Accutase (Innovative Cell Technologies, Inc.). For secondary spheroids, cells were reseeded and treated with GANT-61 for additional 7 days. Cell viability was measured by trypan blue assay. Data represent mean ± SD. @, # and & significantly different from respective controls, P < 0.05. (D and E), CSCs were treated with GANT-61 (0, 1, 5 and 10 μM) for 48 and 72 h. At the end of incubation period, cells were harvested and apoptosis was measured by annexin-V/PI (D), and PI staining (E). Data represent mean ± SD.
Recently, GANT-61 has been identified as a Gli transcription inhibitor. We therefore examined the effect of GANT-61 on cell viability in 2-D (monolayer) and 3-D (spheroids in suspension) cultures and apoptosis in pancreatic CSCs as described in Materials and Methods. GANT-61 inhibited cell viability in 2-D cultures at 48 and 72 h (Fig. 1B), and also inhibited cell viability in primary and secondary spheroids in suspension (Fig. 1C). Furthermore, GANT-61 induced apoptosis at 48 and 72 h in pancreatic CSCs (Fig. 1D). These data suggest that GANT-61 inhibits cell viability and spheroid formation, and induces apoptosis in a dose- and time-dependent manner, and thus can be used for the treatment of pancreatic cancer by targeting CSCs.
3.2. GANT-61 inhibits expression of downstream targets of Shh pathway, decreases Gli-DNA interaction, Gli transcriptional activity and Gli nuclear translocation in pancreatic CSCs
Since GANT-61 inhibited cell viability and induced apoptosis in pancreatic CSCs, we next sought to examine its effects on various components of Shh pathway in pancreatic CSCs by q-RT-PCR analysis (Fig. 2). GANT-61 (10 μM) inhibited the expressions of effectors (Gli1 and Gli2) and receptors (Patched-1, Patched-2, and Smoothened) of Shh pathway in pancreatic CSCs (Fig. 2A). Interestingly, the expression of Shh was not detected in CSCs treated with GANT-61. These data suggest that GANT-61 can regulate CSC characteristics by inhibiting various components of Shh pathway.
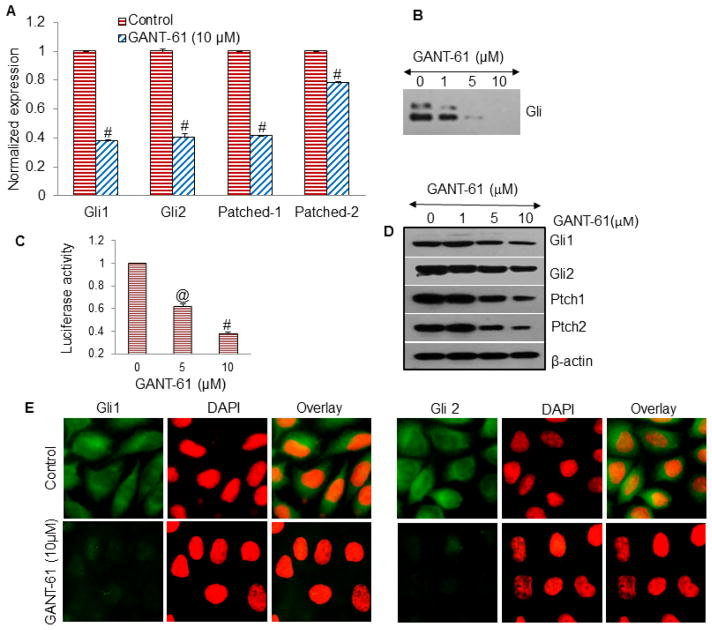
Fig. 2. GANT-61 downregulates Shh signaling pathway in pancreatic CSCs.
(A), Pancreatic CSCs were treated with GANT-61 (10 μM) for 36 h. At the end of incubation period, RNA was extracted and the expression of Gli1, Gli2, Patched-1 and Patched-2 was measured by qRT-PCR. Data represent the mean ± SD. # significantly different from respective control (P < 0.05). (B) Pancreatic CSCs were treated with GANT-61 (0–10 μM) for 48 h. Nuclear extracts were prepared and the gelshift experiment was performed as described in Materials and Methods. Control (without GANT-61), and GANT-61 treated samples (1, 5 and 10 μM), respectively. (C), Gli-dependent luciferase activity is reduced by GANT-61. Pancreatic CSCs were transduced with lentiviral particles expressing Gli-dependent luciferase reporter, and treated with GANT-61 (0, 5 and 10 μM) for 48 h. Lysates were prepared, and luciferase activity was measured as described in Materials and Methods. Normalized luciferase activity is presented as mean ± SD. @ and # significantly different from respective control (P< 0.05). (D), Protein Expression. Pancreatic CSCs were treated with GANT-61 (0–10 μM) for 48 h, and expression of Gli1, Gli2, Ptch1, Ptch2 and β-actin was measured by the Western blot analysis. (E), GANT-61 inhibits total expression of Gli1 and Gli2 in human pancreatic CSCs. The cells were seeded on fibronectin-coated coverslips and treated with GANT-61 (10 μM) for 48 h. Subsequently, cells were fixed with 4% paraformaldehyde, blocked in 10% normal goat serum and stained with Gli1 and Gli2 primary antibodies (1:100) for 16 h at 4 °C and washed with PBS. Afterwards, cells were incubated with fluorescently labeled secondary antibody (1:200) along with DAPI (1 mg/ml) for 1 h at room temperature and cells were mounted and visualized under a fluorescent microscope.
The influence of GANT-61 on the Gli-DNA interaction was subsequently determined by EMSA in human pancreatic CSCs at 48 h treatment (Fig. 2B). Treatment of CSCs with GANT-61 (0–10 μM) resulted in decreased Gli-DNA binding activity. The incubation of nuclear protein with probe only had no effect on Gli-DNA binding activity.
We next examined the effect of GANT-61 on Gli transcriptional activity. Pancreatic CSCs were transduced with a Gli-dependent luciferase reporter construct and treated with GANT-61 for 48 h (Fig. 2C). GANT-61 inhibited Gli-dependent luciferase reporter activity in a dose-dependent manner. Hence, these data suggest that inhibition of Shh pathway by GANT-61 can modulate Gli target genes. We next employed immunofluorescence technique to examine the effect of GANT-61 on Gli1 and Gli2 translocation to nuclei (Fig. 2D). Pancreatic CSCs were treated with GANT-61 (10 μM), and the expression/translocation of Gl1 and Gli2 was observed under a fluorescence microscope. GANT-61 inhibited translocation Gli1 and Gli2 to the nuclei. Overall, these results suggest that GANT-61 can inhibit Gli nuclear translocation, Gli-DNA binding potential and transcriptional activity.
3.3. GANT-61 differentially regulates genes involved in cell survival, cell death and pluripotency
Since GANT-61 inhibited Shh pathway, we next examined the expression of genes which play roles in cell survival, apoptosis and pluripotency. Pancreatic CSCs were exposed to GANT-61 (1, 5 and 10 μM) for 48 h followed by Western blot analysis to determine the expression of genes involved in the regulation of cell death (PDGFRα, Fas, DR4/TRAIL-R1, DR5/TRAIL-R2) and cell survival (Bcl-2), of which PDGFRα can be regulated by Gli1 [27], and Bcl-2 is a direct transcriptional target of Gli2 [14]. Treatment of pancreatic CSCs with GANT-61 increased the expression of DR4/TRAIL-R1, DR5/TRAIL-R2 and Fas (Fig. 3). Expression of PDGFRα was decreased following GANT-61 treatment with concomitant increase in Fas. In contrast, Bcl-2 expression was inhibited by GANT-61 treatment. Cleaved caspase-3 and PARP, both markers of apoptosis, were also increased after GANT-61 exposure, correlating with the change in expression of genes that regulate cell death. Maximum effects of GANT-61 on gene expression were obtained with 10 μM exposure, correlating with the extent on cell survival and apoptosis.
Fig. 3. GANT-61 differentially regulates genes involved in cell death and cell survival.
(A), Pancreatic CSCs were incubated without or with GANT-61 (0, 1, 5 and 10 μM) for 48 h. Cell lysates containing 50 μg of protein were loaded and separated on 10% Tris-HCl gel. Proteins from the gel were transferred on polyvinylidene difluoride membranes and subsequently blocked in blocking buffer and incubated overnight with primary antibodies. Membranes were washed and incubated with secondary antibodies for 1 h at room temperature, and subsequently developed using ECL kit to measure the expression of Fas, DR4/TRAIL-R1, DR5/TRAIL-R2, Bcl-2, Caspase-3 and PARP by the Western blot analysis. β-Actin was used as a loading control. (B), Pancreatic CSCs were treated with GANT-61 (0–10 μM) for 36 h and the expression of c-Myc, Nanog, Sox-2 and Oct-4 was measured by qRT-PCR. HK-GAPD was used as the endogenous normalization control. Data represent mean ± SD. * = significantly different from control, P < 0.05.
Since pluripotency maintaining factors are highly expressed in pancreatic cancer stem cells [28], we next sought to examine the effects of GANT-61 on the expression of cMyc, Nanog, Sox-2 and Oct-4. GANT-61 inhibited the expression of cMyc, Nanog, Sox-2 and Oct-4 in pancreatic CSCs in a dose-dependent manner (Fig. 3B). These data suggest that inhibition of Shh pathway can suppress the self-renewal of CSCs by inhibiting the factors required for maintaining pluripotency.
3.4. Human pancreatic CSCs require active Gli gene function for sustain expression of genes involved in the cell survival and proliferation
In order to examine the effects of Gli1 and Gli2 on cell proliferation, apoptosis and down-stream targets, we inhibited the expression of Gli1 and Gli2 transcription factors by shRNA. As shown in Fig. 4A, lentiviral mediated expression of Gli1 and Gli2 shRNA inhibited the expression of Gli1 and Gli2 proteins in pancreatic CSCs. To confirm the Gli-dependent anti-proliferative and pro-apoptotic effects of GANT-61, we used pancreatic CSCs expressing Gli1 shRNA + Gli2 shRNA (Fig. 4B). GANT-61 inhibited cell viability and induced apoptosis in CSCs/scrambled cells. Inhibition of Gli1 plus Gli2 together by shRNA also inhibited cell viability and induced apoptosis. GANT-61 has no further effects on cell viability and apoptosis when combined with Gli1 plus Gli2 shRNA, suggesting the specificity of GANT-61. These data suggest that both Gli1 and Gli2 genes are required for anti-proliferative and pro-apoptotic effects of GANT-61.
Fig. 4. Impact of Shh signaling pathway on the regulation of cell survival and apoptosis by GANT-61.
(A), Knockout of Gli1 shRNA and Gli2 shRNA in human pancreatic CSCs. Pancreatic CSCs were transduced with lentiviral particles expressing Scrambled, Gli1 shRNA, Gli2 shRNA or Gli1 plus Gli2 shRNA. (B), Pancreatic CSCs were treated with GANT-61 (1, 5 and 10 μM) for 72 h, and cell viability and apoptosis was measured in scrambled and Gli1 plus Gli2 shRNA CSCs. Data represent mean ± SD. *, @ and # significantly different from respective control (P<0.05). (C), Scrambled and Gli1 plus Gli2 shRNA pancreatic CSCs were treated with GANT-61 (0 and 10 μM) for 48 h, and lysates were extracted to determine the expression of DR4, DR5, PDGFRα, Fas and Bcl-2 by Western blot analysis. β-actin was used as the loading control. (D), Inhibition of primary and secondary spheroids by GANT-61. Pancreatic CSCs (scrambled, and Gli1 + Gli2 shRNA) were seeded in suspension and treated with GANT-61 (10 μM) for 7 days. At the end of incubation period, spheroids were collected, and dissociated with Accutase (Innovative Cell Technologies, Inc.). For secondary spheroids, cells were reseeded and treated with GANT-61 (10 μM) for additional 7 days. Cell viability was measured by trypan blue assay. Data represent mean ± SD. @ and # significantly different from respective controls, P < 0.05.
We next examined the role of Gli1 and Gli2 genes on downstream targets of Shh pathway in human pancreatic CSCs. To genetically determine the effects of Gli1 and Gli2, expression of both genes in pancreatic CSCs was inhibited by Gli1 shRNA + Gli2 shRNA (Fig. 4C). Transduced pancreatic CSCs were treated with GANT-61 (10 μM) for 48 h, and the Western blot analysis was performed to determine the expression of genes involved in the regulation of cell death (Fas, DR4/TRAIL-R1 and DR5/TRAIL-R2) and cell survival (PDGFRα and Bcl-2). GANT-61 inhibited the expressions of PDGFRα and Bcl-2, and induced the expressions of Fas, DR4 and DR5 in CSC/scrambled cells. By comparison, GANT-61 had no significant effects on expression of these downstream targets of Shh signaling pathway in Gli1 shRNA + Gli2 shRNA pancreatic CSCs, supporting Gli-mediated cytotoxic effects of GANT-61 in pancreatic CSCs.
We next examined the effect of GANT-61 on primary and secondary spheroid formation (Fig. 4D). GANT-61 inhibited the formation of primary and secondary spheroids in CSC/scrambled cells. By comparison, transduction of Gli1 shRNA + Gli2 shRNA in pancreatic CSCs also inhibited the formation of primary and secondary spheroids. GANT-61 had no further effects on spheroid formation in CSCs transduced with Gli1 shRNA + Gli2 shRNA. These data suggest that GANT-61 can inhibit pancreatic CSC characteristics by modulating the expression of genes which play roles in cell survival and apoptosis.
3.5. GANT-61 inhibits motility, invasion and migration of CSCs
During cancer metastasis, the mobility and invasiveness of cancer cells increase [29]. To detach from neighboring cells and invade adjacent cell layers, carcinoma cells must lose cell-cell adhesion and acquire motility. The highly conserved EMT program has been implicated in dissemination of carcinoma cells from primary epithelial tumors [29]. Tumor progression is frequently associated with the down-regulation of E-cadherin [29], and up-regulation of vimentin and several transcription factors including Snail, ZEB1 and Slug [30]. Cancer stem cells undergoing metastasis usually express low levels of epithelial markers and high levels of mesenchymal markers.
Since CSCs appear to play a significant role in early metastasis [31; 32], we sought to measure the effects of GANT-61 on motility, migration and invasion of CSCs (Fig. 5A and B). GANT-61 inhibited motility, migration and invasion of CSCs. These data suggest that GANT-61 can inhibit early metastasis of pancreatic CSCs.
Fig. 5. Regulation of migration, invasion and epithelial mesenchymal transition factors by GANT-61 in pancreatic CSCs.

(A), Motility Assay. Photomicrographs demonstrating the results of the in vitro motility of pancreatic CSCs using the simple scratch technique. Pancreatic CSCs were grown in monolayer, scratched and treated with or without GANT-61 for 24 or 48 h. (B), Transwell migration assay. Pancreatic CSCs were plated in the top chamber of the transwell and treated with GANT-61 (0–10 μM) for 24 h. Cells migrated to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. * # or % = significantly different from respective controls, P < 0.05. Matrigel invasion assay. CSCs were plated onto the Matrigel-coated membrane in the top chamber of the transwell and treated with GANT-61 (0–10 μM) for 48 h. Cells invaded to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. *, # or % = significantly different from respective controls, P < 0.05. (C), Pancreatic CSCs were treated with GANT-61 (0–10 μM) for 36 h. At the end of incubation period, the expression of Snail, ZEB1 and Slug was measured by q-RT-PCR. Data represent mean ± SD. *, # or % = significantly different from respective controls, P < 0.05. (D), Pancreatic CSCs were treated with GANT-61 (0–10 μM) for 36 h. At the end of incubation period, the expression of E-cadherin and N-cadherin was measured by q-RT-PCR. Data represent mean ± SD. *, @, #, $, %, and & = significantly different from respective controls, P < 0.05.
Since GANT-61 inhibited EMT, we next examined the regulation of EMT inducing transcription factors Snail, Slug and Zeb1 (Fig. 5C). GANT-61 inhibited the expression of Snail, Slug and Zeb1 as measured by q-RT-PCR. Expression of cadherins in CSCs changes during EMT [26]. We therefore examined the effects of GANT-61 on the expression of E-cadherin and N-cadherin (Fig. 5D). GANT-61 enhanced the expression of E-cadherin and inhibited the expression of N-cadherin, a phenomenon known as cadherin switch during EMT. These data suggest that GANT-61 can regulate early metastasis by modulating the expression of cadherins and EMT transcription factors.
3.6. GANT-61 inhibits CSC tumor growth in NOD/SCID mice
Since GANT-61 inhibited cell viability, spheroid formation and induced apoptosis, we next examined its effects on CSC tumor growth in a humanized NOD/SCID IL2Rγ null mouse model. Pancreatic CSCs (50 cells per mouse) were injected subcutaneously into humanized NOD/SCID IL2Rγ null mice (harboring CD34+ peripheral blood stem/progenitor cells). After tumor formation, mice were treated with GANT-61 (40 mg/kg) ip three days per week for six weeks. As shown in Fig 6A, GANT-61 inhibited CSC tumor growth.
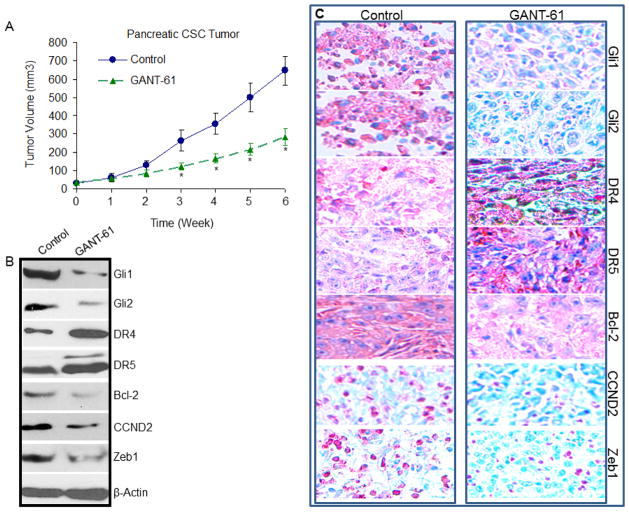
Fig. 6. GANT-61 inhibits CSC tumor growth in NOD/SCID IL2Rγ null mice.
(A), Effects of GANT-61 on CSC tumor growth in NOD/SCID IL2Rγ null mice. Tumor-bearing nude mice (10 mice per group) were injected with vehicle or GANT-61 (40 mg/kg) i.p. three times per week for 6 weeks. Tumor volume was measured weekly. Data represent mean ± SD. * = significantly different from respective control, P < 0.05. (B), Western Blot Analysis. Effects of GANT-61 on the expression of Gli1, Gli2, DR4, DR5, Bcl-2, CCND2 and Zeb1. Lysates were prepared from tumor tissues isolated from control and GANT-61 treated mice. Western blot analysis was performed to measure the expression of Gli1, Gli2, DR4, DR5, Bcl-2, CCND2 and Zeb1. (C), Immunohistochemistry. Effects of GANT-61 on the expression of Gli1, Gli2, DR4, DR5, Bcl-2, CCND2 and Zeb1. Tumor samples derived from mice were subjected to immunohistochemistry with anti-Gli1, anti-Gli2, anti-DR4, anti-DR5, anti-Bcl-2, anti-CCND2 or anti-Zeb1 antibody.
Since GANT-61 inhibited CSC tumor growth in humanized NOD/SCID IL2Rγ null mice, we next examined the effects of GANT-61 on the expression of Gli1 and Gli2, and their downstream targets Bcl-2, CCND2, TRAIL-R1/DR4, TRAIL-R2/DR5 and Zeb1 by Western blot analysis. The data demonstrate that GANT-61 inhibited the expression of Gli1, Gli2, Bcl-2, CCND2 (Cyclin D2) and Zeb1, and induced the expression of death receptor DR4 and DR5 (Fig. 6B). We next confirmed the expression of these proteins by immunohistochemistry. As shown in Fig. 6C, GANT-61 inhibited the expression of Gli1, Gli2, Bcl-2, CCND2 and Zeb1, and induced the expression of DR4 and DR5. These data suggest that GANT61 can inhibit CSC tumor growth by regulating cell survival and cell death proteins and may be combined with death receptor agonist (TRAIL or TRAIL receptor agonistic antibody) to get maximum therapeutic benefits.
4. Discussion
Constitutive activation of the Shh signaling has been implicated in tumor cell proliferation and survival as well as is the molecular hallmark of different human tumor entities that include esophageal squamousm cell carcinoma, basal cell carcinoma [33], subsets of medulloblastoma [34], prostate cancer [35], colon cancer [36], brain tumors [37], rhabdomyosarcoma [38], and breast cancer [39]. In the present study, to analyse the status of Shh signaling components in human pancreatic CSCs, we found these CSCs consistently express various components of Shh signaling pathway including signaling molecules: Gli1, Gli2, Patched-1, Patched-2, and Smoothened, and most importantly the ligand: Shh, suggesting Shh pathway is one of the “core” signaling pathway or an autocrine mode of Shh signaling in these cells. GANT-61 inhibited EMT which was associated with inhibition in Snail, Slug, Zeb1 and N-Cadherin and up-regulation in E-cadherin. Furthermore, GANT-61 inhibited CSC tumor growth in the NOD/SCID IL2Rγ null mice by inhibiting the expression of Gli1, Gli2, Bcl-2, CCND2 and Zeb1, and inducing the expression of death receptor DR4 and DR5, suggesting its clinical potential. Activation of the Shh signaling cascade consistently induces Gli family transcription factors (Gli1 and Gli2), hence both Gli genes mRNA [40], expressed in pancreatic CSCs, stating potential involvement of Shh signaling in human pancreatic carcinogenesis.
Pancreatic cancer is among the most lethal human cancer because it is insensitive to many chemotherapeutic drugs. Multiple lines of evidence support the idea that Shh pathway is essential for the growth of human pancreatic cancer cells. To overcome this problem, inhibition of Shh signaling by new therapeutic targets has been attempted in multiple human cancers [36; 41; 42]. Therapeutic blockade of the Shh pathway by GDC-0449 [42; 43], cyclopamine [42], IPI-926 [41] or Smoothened shRNA [44] inhibited proliferation and survival, and suppressed tumor formation. However, a number of tumors have been shown to be refractory to the direct effects of pharmacologic Hh inhibition with SMO antagonists due to natural or acquired mutations in Smo [6; 45] or amplification of downstream effector Gli2 [46]. Previous reports have shown that tumor growth was blunted when paracrine Hh signaling was inhibited in stromal components of the microenvironment, even when the tumor itself is SMO independent [6; 47; 48]. GDC-0449 induced dramatic reductions in tumor growth with activating Hh mutations [43]. Interestingly, GDC-0449 has little direct effect on tumors without Hh mutations; however, it significantly blocked Hh signaling in tumor stroma and decreased tumor burden. These observations highlight the need for identifying better therapeutic targets that will effectively block Shh signaling pathway. Gli1 and Gli2 are members of Shh pathway, act as downstream mediators of Shh signaling and they have regulatory effects on self-renewal, cell cycle and apoptosis. Recently, GANT-61 has been identified as potent Shh signaling pathway inhibitor for treatment of various cancers [36; 42]. In the context of pancreatic cancer previous attempts to block Shh signaling at the level of Smoothened, induced only low apoptosis and cytotoxicity in genetically engineered mouse model and cell lines [49; 50]. In the present study, exposure to GANT-61 induced significant cytotoxicity in human pancreatic CSCs and inhibited CSC tumor growth in vivo by modulating the expression of Gli1/2-target genes. Recently, Nolan-Stevaux and their colleagues [51] observed that TGF-β-KRAS signaling-dependent activation of Gli proteins in pancreatic ductal adenocarcinoma. Although comprehensive data are lacking, it has been suggested that oncogenic signals such as KRAS may affect Shh signaling, because both aberrant activation of Shh signaling and prevalence RAS oncogene mutations are found in pancreatic cancer [52].
GANT-61 treatment effectively decreased Gli-DNA binding and transcriptional activity in the human pancreatic CSCs, as determined by EMSA and luciferase reporter assay, respectively. The posttranscriptional modifications of Gli by phosphorylation can either prevent DNA binding or destabilize the Gli-DNA complex. The precise nature of this Gli modification is currently under investigation. Post-translational modification of Gli proteins is an important mechanism that regulates the ability of different transcription factors to inhibit distinct gene sets, involved in cell cycle inhibition [36], and apoptosis [49]. Gli activators upregulate CCND1 and CCND2 for cell cycle acceleration, FOXA2, FOXC2, FOXE1, FOXF1, FOXL1, FOXP3, POU3F1, RUNX2, SOX13 and TBX2 for cell fate determination, and JAG2, INHBC and INHBE for stem cell signaling regulation. Of particular interest, GANT-61 markedly inhibited Shh pathway in pancreatic CSCs in vitro and in vivo, thereby showing potential for therapeutic application for treatment of pancreatic cancer. GANT-61 was identified as an inhibitor of Gli1 transcriptional activity, and also abrogated Gli2-mediated transcription [53]. Subsequently, it was observed that reduction in Gli2 mRNA and protein expression preceded that of Gli1 in pancreatic CSCs. Further, studies in mice have revealed that Gli2 is primary mediators of Shh signaling and is known to transcriptionally regulate Gli1 expression [15]. Because the Shh signaling pathway is already activated in human pancreatic CSCs, studies using shRNA knockdown of both Gli1 and Gli2 were conducted. Interestingly, significant protection from GANT-61-induced cytotoxicity and apoptosis was recorded in shRNA knockdown of both Gli1 and Gli2. These data further support the Gli-specific direct mode of action of GANT-61 and further show the importance of functional Gli genes in maintaining cellular proliferation in human pancreatic CSCs.
To assess anticancer effect of GANT-61 in more detail, we next examined its effects on down-stream targets of Gli, and correlated the death receptors expression with apoptosis. Apoptosis can be induced through the activation of death receptors including Fas, DR4/TRAIL-R1, and DR5/TRAIL-R2 by their ligands in the mammalian cells [54]. The specific DRs including DR4, DR5 and Fas are expressed in pancreatic cancers. Treatment of GANT-61 induced a marked increase in the expression levels of DR4, DR5 and Fas, suggesting the potential involvement of these DRs in GANT-61-induced apoptosis. Surprisingly, in promoter region of DR4 and DR5 no Gli binding sites have been identified. The regulation of DR5 expression by Gli is currently unknown and may be via an indirect mechanism. However, GANT-61 induced up-regulation of DR4 and DR5 levels in pancreatic CSCs, suggesting transcriptional regulation of both the DRs by a currently unknown mechanism. We also determined the contributions of apoptotic cell death pathways (mitochondria-mediated intrinsic and death receptor signaling–mediated extrinsic), based on the known regulation of PDGFRα upstream of Fas [52; 55], and of Bcl-2, which may be a direct transcriptional target of both Gli1 and Gli2 [14]. We have shown that GANT-61 treatment inhibited pro-survival protein Bcl-2 and induced DR4 and DR5 expression in pancreatic CSCs in vitro and in vivo. Thus, our data demonstrate that activation of Shh pathway can regulate genes involved in both cell-extrinsic and cell-intrinsic pathways of apoptosis.
EMT during embryogenesis, adult tissue homeostasis and carcinogenesis is characterized by class switch from E-cadherin to N-cadherin. Accumulating evidence suggests that EMT plays an important role during malignant tumor progression. During EMT, transformed epithelial cells can activate embryonic programs of epithelial plasticity and switch from a sessile, epithelial phenotype to a motile, mesenchymal phenotype. Induction of EMT can, therefore, lead to invasion of surrounding stroma, intravasation, dissemination and colonization of distant sites. It is now clear that sustained metastatic growth requires the dissemination of CSCs from the primary tumor followed by their re-establishment in a secondary site. Thus, EMT can confer metastatic ability on carcinomas. SNAI1 (Snail), SNAI2 (Slug), SNAI3, ZEB1, ZEB2 (SIP1), KLF8, TWIST1, and TWIST2 are EMT regulators repressing CDH1 gene encoding E-cadherin. Hedgehog signals induce JAG2 upregulation for Notch-CSL-mediated SNAI1 upregulation, and also induce TGFβ1 secretion for ZEB1 and ZEB2 upregulation via TGFβ receptor and NF-κB. Hedgehog signaling activation indirectly leads to EMT through FGF, Notch, TGFβ signaling cascades, and miRNA regulatory networks. Our results indicate a key and essential role of the Shh-Gli pathway in promoting pancreatic CSC tumor growth, stem cell self-renewal and metastatic behavior. GANT-61 inhibited EMT as demonstrated by inhibition in cell motility, invasion and migration. The inhibition of EMT was associated with suppression of EMT transcription factors (ZEB1, Snail and Slug) and cadherin switch (up-regulation of E-Cadherin and down-regulation of N-Cadherin) in pancreatic CSCs, suggesting a potential role of GANT-61 in early metastasis. Targeting Gli-1/2 is thus predicted to decrease tumor bulk and eradicate CSCs and metastases.
In conclusion, this study has defined two molecular bases of cell death following the inhibition of Shh signaling by GANT-61 in human pancreatic CSCs that include functional death receptor signaling pathway, and suppression of cell-intrinsic/mitochondrial pathway. Tumor spheres express high levels of Hedgehog pathway components and of embryonic pluripotent stem cell factors SOX2, NANOG, OCT4 and cMyc. Inhibition of Gli1 and Gli2 expression and function in pancreatic CSCs using RNA interference technology mimicked the effects of GANT-61 treatment, supporting the specificity of GANT-61. The inhibition of Gli function by GANT-61 resulted in modulation of CSC proliferation, EMT, and apoptosis. Furthermore, GANT-61 inhibited CSC tumor growth which was associated with inhibition of Gli1, Gli2, Bcl-2, CCND2 and Zeb1, and induction of death receptor DR4 and DR5. These findings highlight the potential role of Shh signaling in CSC biology, and the possibility of targeting Gli transcription factors by GANT-61 for the treatment of pancreatic cancer.
Acknowledgments
Grant Support
This work was supported in part by the grants from the National Institutes of Health (R01CA125262, RO1CA114469 and RO1CA125262-02S1) and Kansas Bioscience Authority.
We thank our lab members for critical reading of the manuscript.
Footnotes
Disclosure of Potential Conflicts of Interest
The authors have declared that no competing interests exist.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Greaves M, Maley CC. Clonal evolution in cancer. Nature. 2012;481:306–313. doi: 10.1038/nature10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Margueron R, Reinberg D. The Polycomb complex PRC2 and its mark in life. Nature. 2011;469:343–349. doi: 10.1038/nature09784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biddle A, Mackenzie IC. Cancer stem cells and EMT in carcinoma. Cancer Metastasis Rev. 2012 doi: 10.1007/s10555-012-9345-0. [DOI] [PubMed] [Google Scholar]
- 4.Visvader JE. Cells of origin in cancer. Nature. 2011;469:314–322. doi: 10.1038/nature09781. [DOI] [PubMed] [Google Scholar]
- 5.Ogden SK, Ascano M, Jr, Stegman MA, Robbins DJ. Regulation of Hedgehog signaling: a complex story. Biochemical pharmacology. 2004;67:805–814. doi: 10.1016/j.bcp.2004.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yauch RL, Gould SE, Scales SJ, Tang T, Tian H, Ahn CP, Marshall D, Fu L, Januario T, Kallop D, Nannini-Pepe M, Kotkow K, Marsters JC, Rubin LL, de Sauvage FJ. A paracrine requirement for hedgehog signalling in cancer. Nature. 2008;455:406–410. doi: 10.1038/nature07275. [DOI] [PubMed] [Google Scholar]
- 7.Ingham PW, McMahon AP. Hedgehog signaling in animal development: paradigms and principles. Genes & development. 2001;15:3059–3087. doi: 10.1101/gad.938601. [DOI] [PubMed] [Google Scholar]
- 8.Ruiz i Altaba A. Therapeutic inhibition of Hedgehog-GLI signaling in cancer: epithelial, stromal, or stem cell targets? Cancer Cell. 2008;14:281–283. doi: 10.1016/j.ccr.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz i Altaba A. Gli proteins and Hedgehog signaling: development and cancer. Trends Genet. 1999;15:418–425. doi: 10.1016/s0168-9525(99)01840-5. [DOI] [PubMed] [Google Scholar]
- 10.Dahmane N, Sanchez P, Gitton Y, Palma V, Sun T, Beyna M, Weiner H, Ruiz i Altaba A. The Sonic Hedgehog-Gli pathway regulates dorsal brain growth and tumorigenesis. Development. 2001;128:5201–5212. doi: 10.1242/dev.128.24.5201. [DOI] [PubMed] [Google Scholar]
- 11.Gerber AN, Wilson CW, Li YJ, Chuang PT. The hedgehog regulated oncogenes Gli1 and Gli2 block myoblast differentiation by inhibiting MyoD-mediated transcriptional activation. Oncogene. 2007;26:1122–1136. doi: 10.1038/sj.onc.1209891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasper M, Regl G, Frischauf AM, Aberger F. GLI transcription factors: mediators of oncogenic Hedgehog signalling. Eur J Cancer. 2006;42:437–445. doi: 10.1016/j.ejca.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Wu X, Pasca di Magliano M, Peters EC, Wang Y, Hong J, Hebrok M, Ding S, Cho CY, Schultz PG. A small-molecule antagonist of the hedgehog signaling pathway. Chembiochem. 2007;8:1916–1919. doi: 10.1002/cbic.200700403. [DOI] [PubMed] [Google Scholar]
- 14.Regl G, Kasper M, Schnidar H, Eichberger T, Neill GW, Philpott MP, Esterbauer H, Hauser-Kronberger C, Frischauf AM, Aberger F. Activation of the BCL2 promoter in response to Hedgehog/GLI signal transduction is predominantly mediated by GLI2. Cancer Res. 2004;64:7724–7731. doi: 10.1158/0008-5472.CAN-04-1085. [DOI] [PubMed] [Google Scholar]
- 15.Katoh Y, Katoh M. Integrative genomic analyses on GLI1: positive regulation of GLI1 by Hedgehog-GLI, TGFbeta-Smads, and RTK-PI3K-AKT signals, and negative regulation of GLI1 by Notch-CSL-HES/HEY, and GPCR-Gs-PKA signals. Int J Oncol. 2009;35:187–192. doi: 10.3892/ijo_00000328. [DOI] [PubMed] [Google Scholar]
- 16.Hidalgo M, Maitra A. The hedgehog pathway and pancreatic cancer. N Engl J Med. 2009;361:2094–2096. doi: 10.1056/NEJMcibr0905857. [DOI] [PubMed] [Google Scholar]
- 17.Chen MH, Wilson CW, Li YJ, Law KK, Lu CS, Gacayan R, Zhang X, Hui CC, Chuang PT. Cilium-independent regulation of Gli protein function by Sufu in Hedgehog signaling is evolutionarily conserved. Genes & development. 2009;23:1910–1928. doi: 10.1101/gad.1794109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams JA. Hedgehog signaling pathway as a target for therapeutic intervention in basal cell carcinoma. Drug News Perspect. 2003;16:657–662. doi: 10.1358/dnp.2003.16.10.829296. [DOI] [PubMed] [Google Scholar]
- 19.Hutchin ME, Kariapper MS, Grachtchouk M, Wang A, Wei L, Cummings D, Liu J, Michael LE, Glick A, Dlugosz AA. Sustained Hedgehog signaling is required for basal cell carcinoma proliferation and survival: conditional skin tumorigenesis recapitulates the hair growth cycle. Genes & development. 2005;19:214–223. doi: 10.1101/gad.1258705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grachtchouk M, Mo R, Yu S, Zhang X, Sasaki H, Hui CC, Dlugosz AA. Basal cell carcinomas in mice overexpressing Gli2 in skin. Nat Genet. 2000;24:216–217. doi: 10.1038/73417. [DOI] [PubMed] [Google Scholar]
- 21.Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 22.Huber MA, Kraut N, Beug H. Molecular requirements for epithelial-mesenchymal transition during tumor progression. Curr Opin Cell Biol. 2005;17:548–558. doi: 10.1016/j.ceb.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Peinado H, Olmeda D, Cano Snail A. Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer. 2007;7:415–428. doi: 10.1038/nrc2131. [DOI] [PubMed] [Google Scholar]
- 24.Shankar S, Nall D, Tang SN, Meeker D, Passarini J, Sharma J, Srivastava RK. Resveratrol inhibits pancreatic cancer stem cell characteristics in human and KrasG12D transgenic mice by inhibiting pluripotency maintaining factors and epithelial-mesenchymal transition. PLoS One. 2011;6:e16530. doi: 10.1371/journal.pone.0016530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiznerowicz M, Trono D. Conditional suppression of cellular genes: lentivirus vector-mediated drug-inducible RNA interference. J Virol. 2003;77:8957–8961. doi: 10.1128/JVI.77.16.8957-8961.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh BN, Fu J, Srivastava RK, Shankar S. Hedgehog signaling antagonist GDC-0449 (Vismodegib) inhibits pancreatic cancer stem cell characteristics: molecular mechanisms. PLoS One. 2011;6:e27306. doi: 10.1371/journal.pone.0027306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie J, Aszterbaum M, Zhang X, Bonifas JM, Zachary C, Epstein E, McCormick F. A role of PDGFRalpha in basal cell carcinoma proliferation. Proc Natl Acad Sci U S A. 2001;98:9255–9259. doi: 10.1073/pnas.151173398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang SN, Fu J, Nall D, Rodova M, Shankar S, Srivastava RK. Inhibition of sonic hedgehog pathway and pluripotency maintaining factors regulate human pancreatic cancer stem cell characteristics. Int J Cancer. 2011 doi: 10.1002/ijc.26323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Iwatsuki M, Mimori K, Fukagawa T, Ishii H, Yokobori T, Sasako M, Baba H, Mori M. The clinical significance of vimentin-expressing gastric cancer cells in bone marrow. Ann Surg Oncol. 2010;17:2526–2533. doi: 10.1245/s10434-010-1041-0. [DOI] [PubMed] [Google Scholar]
- 31.Monteiro J, Fodde R. Cancer stemness and metastasis: therapeutic consequences and perspectives. Eur J Cancer. 2010;46:1198–1203. doi: 10.1016/j.ejca.2010.02.030. [DOI] [PubMed] [Google Scholar]
- 32.Merchant JL. Hedgehog signalling in gut development, physiology and cancer. J Physiol. 2012;590:421–432. doi: 10.1113/jphysiol.2011.220681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogt A, Chuang PT, Hebert J, Hwang J, Lu Y, Kopelovich L, Athar M, Bickers DR, Epstein EH., Jr Immunoprevention of basal cell carcinomas with recombinant hedgehog-interacting protein. J Exp Med. 2004;199:753–761. doi: 10.1084/jem.20031190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ward RJ, Lee L, Graham K, Satkunendran T, Yoshikawa K, Ling E, Harper L, Austin R, Nieuwenhuis E, Clarke ID, Hui CC, Dirks PB. Multipotent CD15+ cancer stem cells in patched-1-deficient mouse medulloblastoma. Cancer Res. 2009;69:4682–4690. doi: 10.1158/0008-5472.CAN-09-0342. [DOI] [PubMed] [Google Scholar]
- 35.Thiyagarajan S, Bhatia N, Reagan-Shaw S, Cozma D, Thomas-Tikhonenko A, Ahmad N, Spiegelman VS. Role of GLI2 transcription factor in growth and tumorigenicity of prostate cells. Cancer Res. 2007;67:10642–10646. doi: 10.1158/0008-5472.CAN-07-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazumdar T, DeVecchio J, Shi T, Jones J, Agyeman A, Houghton JA. Hedgehog signaling drives cellular survival in human colon carcinoma cells. Cancer Res. 2011;71:1092–1102. doi: 10.1158/0008-5472.CAN-10-2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruiz i Altaba A, Stecca B, Sanchez P. Hedgehog--Gli signaling in brain tumors: stem cells and paradevelopmental programs in cancer. Cancer Lett. 2004;204:145–157. doi: 10.1016/S0304-3835(03)00451-8. [DOI] [PubMed] [Google Scholar]
- 38.Ecke I, Petry F, Rosenberger A, Tauber S, Monkemeyer S, Hess I, Dullin C, Kimmina S, Pirngruber J, Johnsen SA, Uhmann A, Nitzki F, Wojnowski L, Schulz-Schaeffer W, Witt O, Hahn H. Antitumor effects of a combined 5-aza-2′deoxycytidine and valproic acid treatment on rhabdomyosarcoma and medulloblastoma in Ptch mutant mice. Cancer Res. 2009;69:887–895. doi: 10.1158/0008-5472.CAN-08-0946. [DOI] [PubMed] [Google Scholar]
- 39.Vorechovsky I, Benediktsson KP, Toftgard R. The patched/hedgehog/smoothened signalling pathway in human breast cancer: no evidence for H133Y SHH, PTCH and SMO mutations. Eur J Cancer. 1999;35:711–713. doi: 10.1016/s0959-8049(99)00017-9. [DOI] [PubMed] [Google Scholar]
- 40.Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, Lin MT, Calhoun ES, Kamiyama M, Walter K, Nikolskaya T, Nikolsky Y, Hartigan J, Smith DR, Hidalgo M, Leach SD, Klein AP, Jaffee EM, Goggins M, Maitra A, Iacobuzio-Donahue C, Eshleman JR, Kern SE, Hruban RH, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801–1806. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, Madhu B, Goldgraben MA, Caldwell ME, Allard D, Frese KK, Denicola G, Feig C, Combs C, Winter SP, Ireland-Zecchini H, Reichelt S, Howat WJ, Chang A, Dhara M, Wang L, Ruckert F, Grutzmann R, Pilarsky C, Izeradjene K, Hingorani SR, Huang P, Davies SE, Plunkett W, Egorin M, Hruban RH, Whitebread N, McGovern K, Adams J, Iacobuzio-Donahue C, Griffiths J, Tuveson DA. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457–1461. doi: 10.1126/science.1171362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, Weiss GJ, Borad MJ, Hann CL, Brahmer JR, Mackey HM, Lum BL, Darbonne WC, Marsters JC, Jr, de Sauvage FJ, Low JA. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164–1172. doi: 10.1056/NEJMoa0905360. [DOI] [PubMed] [Google Scholar]
- 43.Lorusso PM, Rudin CM, Reddy JC, Tibes R, Weiss GJ, Borad MJ, Hann CL, Brahmer JR, Chang I, Darbonne WC, Graham RA, Zerivitz KL, Low JA, Von Hoff DD. Phase I Trial of Hedgehog Pathway Inhibitor Vismodegib (GDC-0449) in Patients with Refractory, Locally Advanced or Metastatic Solid Tumors. Clin Cancer Res. 2011;17:2502–2511. doi: 10.1158/1078-0432.CCR-10-2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Varnat F, Duquet A, Malerba M, Zbinden M, Mas C, Gervaz P, Ruiz i Altaba A. Human colon cancer epithelial cells harbour active HEDGEHOG-GLI signalling that is essential for tumour growth, recurrence, metastasis and stem cell survival and expansion. EMBO Mol Med. 2009;1:338–351. doi: 10.1002/emmm.200900039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnson RW, Nguyen MP, Padalecki SS, Grubbs BG, Merkel AR, Oyajobi BO, Matrisian LM, Mundy GR, Sterling JA. TGF-beta promotion of Gli2-induced expression of parathyroid hormone-related protein, an important osteolytic factor in bone metastasis, is independent of canonical Hedgehog signaling. Cancer Res. 2011;71:822–831. doi: 10.1158/0008-5472.CAN-10-2993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lauth M, Bergstrom A, Shimokawa T, Toftgard R. Inhibition of GLI-mediated transcription and tumor cell growth by small-molecule antagonists. Proc Natl Acad Sci U S A. 2007;104:8455–8460. doi: 10.1073/pnas.0609699104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dierks C, Grbic J, Zirlik K, Beigi R, Englund NP, Guo GR, Veelken H, Engelhardt M, Mertelsmann R, Kelleher JF, Schultz P, Warmuth M. Essential role of stromally induced hedgehog signaling in B-cell malignancies. Nature medicine. 2007;13:944–951. doi: 10.1038/nm1614. [DOI] [PubMed] [Google Scholar]
- 48.Tian H, Callahan CA, DuPree KJ, Darbonne WC, Ahn CP, Scales SJ, de Sauvage FJ. Hedgehog signaling is restricted to the stromal compartment during pancreatic carcinogenesis. Proc Natl Acad Sci U S A. 2009;106:4254–4259. doi: 10.1073/pnas.0813203106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feldmann G, Fendrich V, McGovern K, Bedja D, Bisht S, Alvarez H, Koorstra JB, Habbe N, Karikari C, Mullendore M, Gabrielson KL, Sharma R, Matsui W, Maitra A. An orally bioavailable small-molecule inhibitor of Hedgehog signaling inhibits tumor initiation and metastasis in pancreatic cancer. Mol Cancer Ther. 2008;7:2725–2735. doi: 10.1158/1535-7163.MCT-08-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hashimoto-Torii K, Motoyama J, Hui CC, Kuroiwa A, Nakafuku M, Shimamura K. Differential activities of Sonic hedgehog mediated by Gli transcription factors define distinct neuronal subtypes in the dorsal thalamus. Mech Dev. 2003;120:1097–1111. doi: 10.1016/j.mod.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Nolan-Stevaux O, Lau J, Truitt ML, Chu GC, Hebrok M, Fernandez-Zapico ME, Hanahan D. GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation. Genes & development. 2009;23:24–36. doi: 10.1101/gad.1753809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marchese R, Muleti A, Pasqualetti P, Bucci B, Stigliano A, Brunetti E, De Angelis M, Mazzoni G, Tocchi A, Brozzetti S. Low correspondence between K-ras mutations in pancreatic cancer tissue and detection of K-ras mutations in circulating DNA. Pancreas. 2006;32:171–177. doi: 10.1097/01.mpa.0000202938.63084.e3. [DOI] [PubMed] [Google Scholar]
- 53.Lauth M, Toftgard R. The Hedgehog pathway as a drug target in cancer therapy. Curr Opin Investig Drugs. 2007;8:457–461. [PubMed] [Google Scholar]
- 54.Srivastava RK. TRAIL/Apo-2L: mechanisms and clinical applications in cancer. Neoplasia. 2001;3:535–546. doi: 10.1038/sj.neo.7900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363:1049–1057. doi: 10.1016/S0140-6736(04)15841-8. [DOI] [PubMed] [Google Scholar]