Abstract
Objective
This study investigated the prescription patterns for Korean patients with schizophrenia with a particular focus on antipsychotic polypharmacy. All data were gathered from patients presenting at 41 tertiary university hospitals and 8 secondary hospitals.
Methods
Data from three multicenter studies conducted in Korea were retrospectively reviewed and integrated to identify patients with schizophrenia who had their antipsychotic medication switched to paliperidone extended-release between 2008 and 2009. The rates for antipsychotic polypharmacy, combined use of different antipsychotic classes with a special focus on atypical antipsychotics, and psychotropic polypharmacy using benzodiazepines, mood stabilizers, and other relevant drugs were identified.
Results
Of the 851 Korean patients analyzed in this study, 20.4% (n=173) had been prescribed antipsychotic polypharmacy. Of the 678 patients receiving antipsychotic monotherapy, 6.9% (n=47) were prescribed a typical antipsychotic and 93.1% (n=631) were prescribed an atypical antipsychotic. Of the 173 patients receiving a combination of antipsychotic drugs, only 6.4% (n=11) had been prescribed polypharmacy with typical antipsychotics, while 46.82% (n=81) were prescribed atypical+atypical antipsychotics or typical+atypical antipsychotics. The highest co-prescription rates for other psychotropic drugs in conjunction with antipsychotics included benzodiazepines (30.3%), anticholinergic drugs (28.8%), antidepressants (13.3%), β-blockers (10.1%), and mood stabilizers (8.7%).
Conclusion
The present findings demonstrate that the rate of antipsychotic polypharmacy is relatively low in Korea and that Korean clinicians prefer to prescribe atypical, rather than typical, antipsychotic drugs. This suggests that there is a distinct prescription pattern in Korea that is focused on antipsychotic polypharmacy.
Keywords: Schizophrenia, Antipsychotic agents, Polypharmacy, Psychotropic drugs
INTRODUCTION
Antipsychotic polypharmacy has been associated with risk of adverse events,1) high cost,2) metabolic syndromes,3) and a lowered patient's adherence to medications.4) Therefore, many schizophrenia treatment guidelines emphasize antipsychotic monotherapy as a first principle.5,6,7) However, antipsychotic polypharmacy is very common in real clinical practice and previous studies have found a broad range of antipsychotic polypharmacy rates (4.1-48.0%)2,8,9,10,11,12) depending on the study method and characteristics of the patient group. Sim et al.11) reported that the rates of antipsychotic polypharmacy was 45.7% in East Asia with wide intercountry variations and the result was likely to be influenced by the clinical settings as well as cultural and personal practice factors. The high rate of polypharmacy indicated that available pharmacological treatments and treatment guidelines are still far from meeting all the needs in the management of schizophrenia.12)
Atypical antipsychotics, which have less adverse effects and potentially have superior effects on the negative and cognitive symptoms compared with the typical antipsychotics, were introduced in the 1990s and have become the first-line drugs for the treatment for schizophrenia. In spite of the superiority and wide distribution of the atypical antipsychotics, clinicians often attempt experimental use of high atypical antipsychotic doses, antipsychotic polypharmacy or augmentation in clinical practice hoping for early and robust responses when faced with patients having severe and disabling symptoms.13)
Along with the increasing prescription rate of atypical antipsychotics for schizophrenia, there is a growing tendency for atypical antipsychotic polypharmacy wherein two or more atypical antipsychotics are concomitantly prescribed. Gilmer et al.14) reported that the proportion of atypical antipsychotic polypharmacy increased from 3.3% in 1999 to 13.7% in 2004. Gallego et al.15) observed that the rates of antipsychotic polypharmacy were not different between decades, but antipsychotic class combinations have shifted from 2 typical antipsychotics to combinations of an atypical and a typical antipsychotics or 2 atypical antipsychotics. These trends were mainly due to the introduction of atypical antipsychotics after 1990.
Naturally, the patterns of antipsychotic prescription vary from country to country and are likely to be influenced by their respective health-care policies, preferred treatment modalities, cost and the availability of drugs. Chong et al.16) studied antipsychotic prescribing patterns for patients with schizophrenia in six countries in East Asia including China, Japan, and Korea. According to the study conducted in 2001 and published in 2004, the atypical antipsychotics comprised 28.1% of all prescribed antipsychotics and the rate in East Asia is much lower than in the United States. Moreover, Japan had the highest rate of antipsychotic polypharmacy and the most frequently used second-generation antipsychotic drug in China was clozapine due to its cheap generic forms.16)
However, the antipsychotic prescribing pattern seemed to change with time. A previous study conducted at a university hospital in Korea revealed that a significant proportional increase of atypical agents was prescribed in 2009-2010 compared to 2003-2004 and 1997. And there was also a significant proportional increase in patients receiving two or more antipsychotics across a decade.17)
Work is now in progress to study the coprescription of other psychotropic drugs, especially benzodiazepines, mood stabilizers, and other relevant drugs with antipsychotics. According to Vares et al.18) most patients with psychosis have been prescribed a combination of medications at some point but the treatment periods were relatively short, corresponding to 14% of the total time of antipsychotics treatment, apart from anti-parkinsonism drugs.
To date, only a few articles have been published regarding prescription patterns for schizophrenia patients in East Asian countries, and no studies have investigated nationwide prescription patterns specifically for these patients in Korea. However, a report by Choi et al.19) evaluated antipsychotic prescription patterns in 467 patients with schizophrenia who were admitted to a Korean general hospital and found that 9% of patients received more than two antipsychotic drugs and that the rate of antipsychotic use in combination with other psychotropic medications increased between 2001 and 2008. Because this study utilized a relatively small sample size and was conducted at only one study site, the results may not be generalized to the whole country.
A thorough investigation of antipsychotic prescription patterns for the treatment of schizophrenia in Korea will have particular significance in several ways. The information obtained will assist psychiatrists to make sound clinical judgments regarding the appropriate antipsychotic medications for an individual. Furthermore, clinical evidence concerning Korean schizophrenic patients with specific clinical circumstances and cultural customs will aid in the development of proper therapeutic strategies for this particular population. A study of this nature will also gather data about prescription patterns across the decades and establish a basis for future research investigating schizophrenia in Korea. Conducting a local study of this type is necessary because the findings of similar studies conducted in other countries may not necessarily be generalized to the Korean population due to the varied availability of specific drugs and preferred treatment modalities in Korea and the fact that the unique health care system in Korea may restrict certain prescriptions. Thus, the present study aimed to investigate prescription patterns in patients with schizophrenia using data from multiple centers in Korea, with a particular focus on antipsychotic polypharmacy and the combination of atypical antipsychotics with other psychotropic drugs.
METHODS
Study Design
We integrated and retrospectively reviewed the data of three studies involving 41 tertiary university hospitals and 8 secondary hospitals in Korea wherein antipsychotic medications for patients with schizophrenia were switched to paliperidone extended-release (paliperidone ER) from 2008 to 2009. These three studies are the Paliperidone ER Effectiveness Study to Evaluate the Objective Symptom Change and Symptomatic Remission (Pal-KOR-4002), the Subjective Symptom Change (PAL-KOR-4003), and the Change of Subjective Well-being & Drug Attitude in Schizophrenic Patients (PAL-KOR-4004). Excluding the 27 patients who did not take the antipsychotic drug on screening, a total of 851 patients were included in this study. We reviewed the antipsychotics and other psychotropic drugs prescribed at the time of screening for the three studies mentioned above. We determined the rate of antipsychotic polypharmacy, antipsychotic class combination with special focus on atypical antipsychotics, the rate of psychotropic polypharmacy using benzodiazepines, mood stabilizers, and other relevant drugs. The doses of the antipsychotics were converted to chlorpromazine equivalents (CPZeq) as per previous articles.20,21)
There is no clear consensus on the definition of polypharmacy. We focused on antipsychotic polypharmacy and psychotropic polypharmacy in this article by applying the concept of 'antipsychotic polypharmacy' (concurrent use of more than one antipsychotic drug) and 'psychotropic polypharmacy' (combination of an agent from a different class of psychotrpic drugs with an antipsychotics) mentioned by Fleischhacker et al.4)
The Clinical Global Impression-Schizophrenia-Severity (CGI-SCH-S) scale, and the Personal and Social Performance (PSP) scale were used to assess the patients' psychiatric status. The CGI-SCH scale, which was adapted from the CGI scale, is a brief assessment instrument designed to evaluate positive, negative, depressive, and cognitive symptoms and overall severity of the schizophrenia. This scale is a valid and reliable instrument used to evaluate the severity and treatment response of schizophrenia.22) We used the PSP scale to study social functions. It has four domains of behavior used to measure the severity of dysfunction: (1) socially useful activities (including work and academic study), (2) personal and social relationships, (3) self-care, and (4) disturbing and aggressive behaviors. PSP produces reliable and valid outcome measurements in patients during acute23) and stable stages of schizophrenia.24)
Subjects
The original three studies from which the present date were gathered were conducted on males and females between the ages of 18 and 65 who were diagnosed with schizophrenia in accordance based on criteria in the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV). The exclusion criteria were as follows: 1) a previous history of neuroleptic malignant syndrome, 2) a history of allergic or hypersensitivity reactions to risperidone or paliperidone, 3) the receipt of clozapine within a month of screening, 4) the possibility of suicidal or aggressive behavior in a patient which rendered them not qualified in a clinical study by a clinician, or 5) a history of long acting antipsychotic injection within one month of screening.
Statistical Analysis
All analyses were performed with the PASW Statistics program version 18.0 for Windows (IBM Co., Armonk, NY, USA) and two-tailed statistical significance was set at p<0.05. The normality of the distribution for continuous measures was assessed with the Kolmogorov-Smirnov test and the Shapiro-Wilk test prior to further analysis.
Patients were divided into two groups according to their prescribed antipsychotics; the polypharmacy group or the monotherapy group. To identify predictors of antipsychotic polypharmacy, stepwise backward elimination logistic regression analyses were conducted with any characteristic that was significantly different at a level of p<0.1 between the two groups was entered into the model; namely, duration of illness, CGI-SCH-S-Positive score, PSP score, and occupation status.
The prevalence of antipsychotic polypharmacy was correlated with the demographic and clinical characteristics and then compared between the two groups. Differences in the rate of use of antipsychotics in combination with other psychotropic drugs and the rate of use of psychotropic drugs including benzodiazepines, antidepressants, mood stabilizers, β-blockers, and anticholinergic drugs were also compared between groups. A chi-square test was used to analyze categorical variables and the Mann-Whitney U-test was used to analyze non-normally distributed continuous data.
RESULTS
Frequencies of Antipsychotic Monotherapy and Polypharmacy
For the entire sample (n=851), 79.7% (n=678) of patients were treated with a single antipsychotic drug, while 19.2% (n=163) were prescribed two antipsychotic drugs and 1.2% (n=10) were prescribed three antipsychotic drugs (Table 1). In total, 20.4% (n=173) had received antipsychotic polypharmacy in Korea.
Table 1.
The rates of antipsychotic monotherapy and polypharmacy
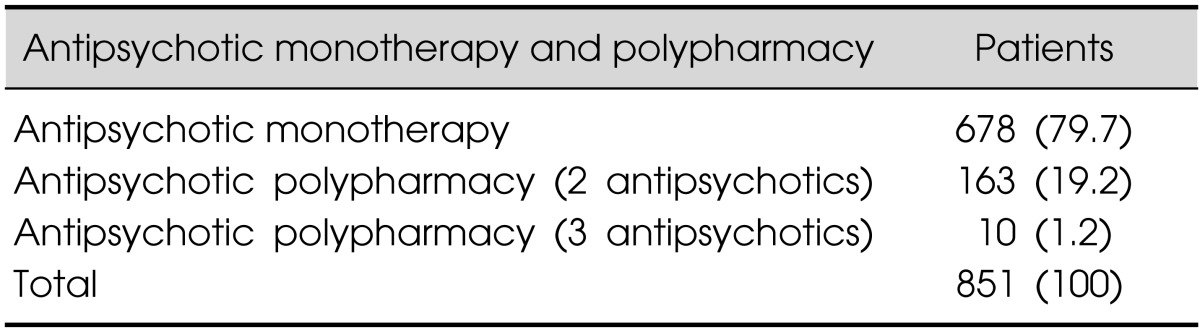
Values are presented as number (%).
Demographic and Clinical Characteristics of the Antipsychotic Monotherapy and Polypharmacy Groups
Patients in the polypharmacy group had a significantly longer duration of illness (p=0.001) and a higher unemployed status (p=0.018) than patients in the antipsychotic monotherapy group. No statistically significant differences were detected in relation to the sex, age, education, body mass index, or hospitalization between the groups (Table 2).
Table 2.
Demographic and clinical characteristics of the antipsychotic monotherapy and polypharmacy groups
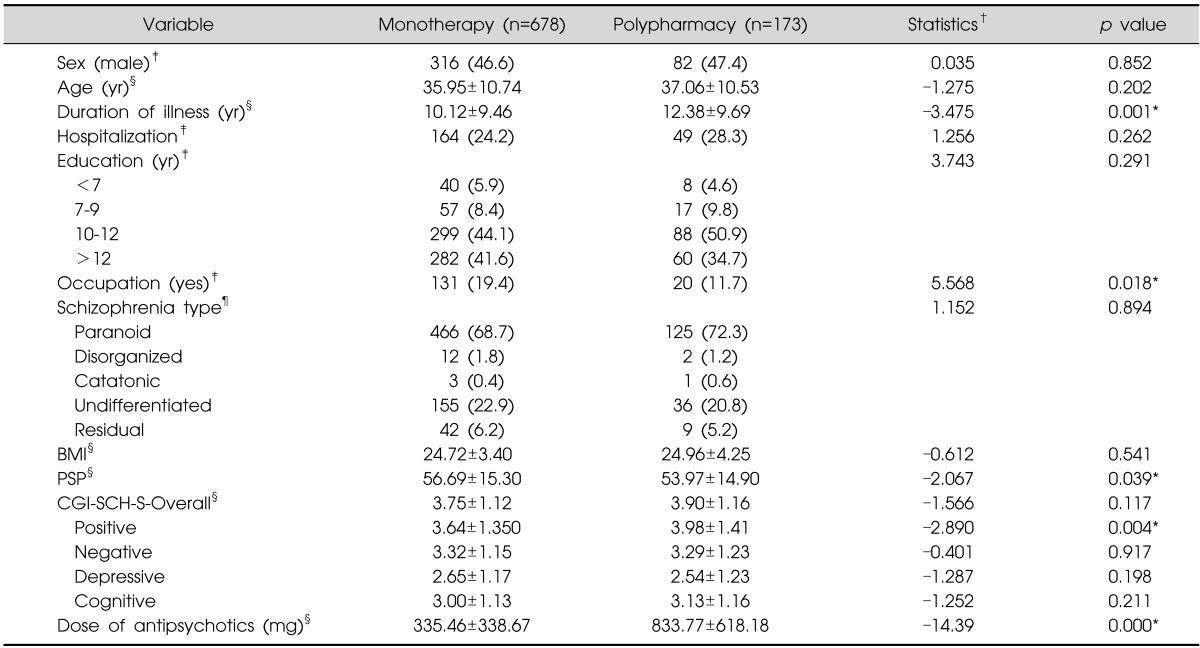
Values are presented as number (%) or mean±standard deviation.
*p<0.05.
†Statistics are based on chi-square test, Z, and Fisher's exact test value.
‡Pearson chi-square test, §Mann-Whitney test, ¶Fisher's exact test.
BMI, body mass index; PSP, Personal and Social Performance scale; CGI-SCH-S, Clinical Global Impression-Schizophrenia-Severity scale.
The PSP score for the polypharmacy group was lower than that of the monotherapy group (p=0.039) and the CGI-SCH-S-Positive score of the polypharmacy group was higher than that of the monotherapy group (p=0.004). However, no statistically significant differences were detected between the groups in terms of the CGI-SCH-S-Overall, -Negative, -Depressive, or -Cognitive scores. The dosage of antipsychotics prescribed was significantly higher in the polypharmacy group (CPZeq=833.774 mg) than in the monotherapy group (CPZeq=335.457 mg; p<0.001) (Table 2).
Predictors of Prescription of Antipsychotic Polypharmacy
A stepwise backward logistic regression model was used to explore the possible predictors for antipsychotic polypharmacy; duration of illness, the CGI-SCH-S-Positive score, the PSP score, and occupation status were entered into the regression model. The standardized β coefficients, standard errors, and odds ratios (OR; 95% confidence interval) for each of the factors predicting antipsychotic polypharmacy are provided (Table 3). Duration of illness, CGI-SCH-S-Positive score, and occupation status were found to be predictors for the prescription of antipsychotic polypharmacy.
Table 3.
Logistic regression results for predicting antipsychotic polypharmacy
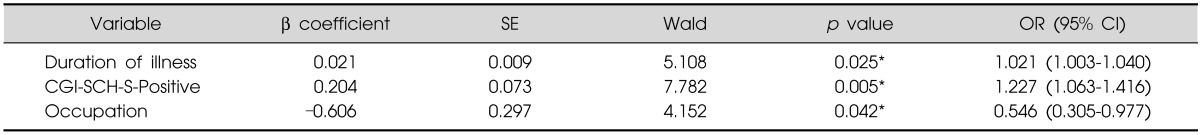
*p<0.05.
SE, standard error; OR, odds ratio; CI, confidence interval; CGI-SCH-S, Clinical Global Impression-Schizophrenia-Severity scale.
Frequencies of Typical and Atypical Antipsychotic Use
The frequencies of typical and atypical antipsychotic prescriptions in the monotherapy and polypharmacy groups are provided (Table 4). Of the 678 patients receiving monotherapy, only 6.9% (n=47) were prescribed a typical antipsychotic, while 93.1% (n=631) were prescribed an atypical antipsychotic (Table 4). Of the 173 patients receiving polypharmacy, 6.4% (n=11) were prescribed a combination of typical+typical antipsychotics, 46.82% (n=81) were prescribed a combination of atypical+atypical antipsychotics, and 46.82% (n=81) were prescribed a combination of typical+atypical antipsychotics.
Table 4.
The frequencies of typical and atypical antipsychotic prescriptions
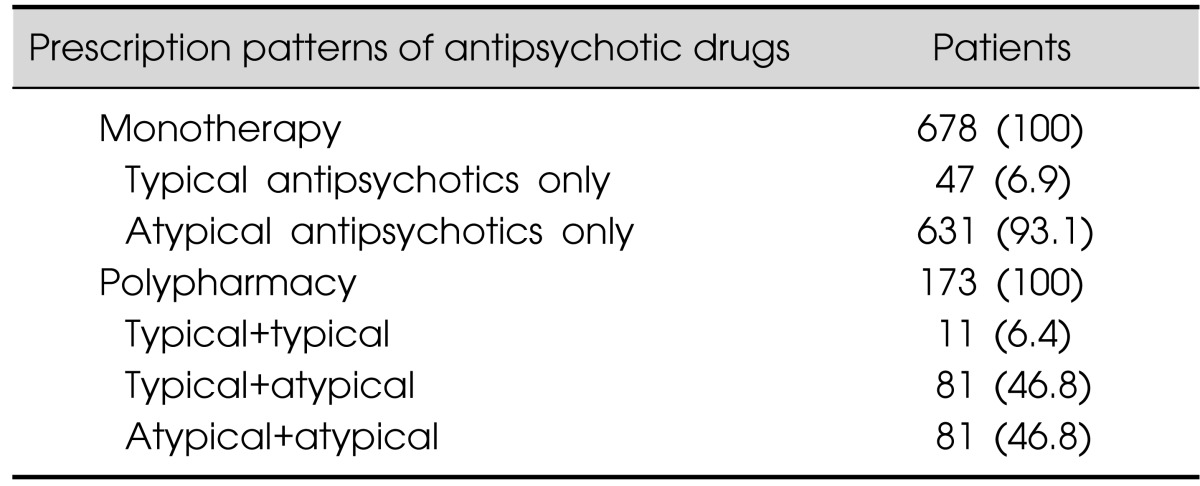
Values are presented as number (%).
The most frequently prescribed antipsychotic medications in the monotherapy group were risperidone (n=320, 47.2%), olanzapine (n=98, 14.5%), and aripiprazole (n=77, 11.4%). The most frequent combinations of antipsychotic medications in the polypharmacy group were risperidone+haloperidol (n=21, 12.1%), risperidone+quetiapine (n=18, 10.4%), and risperidone+chlorpromazine (n=13, 7.51%).
Prescription Patterns for Other Psychotropic Medications
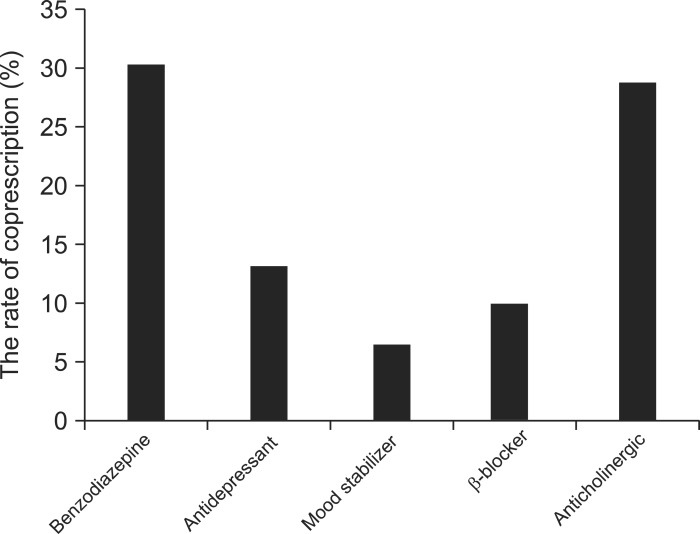
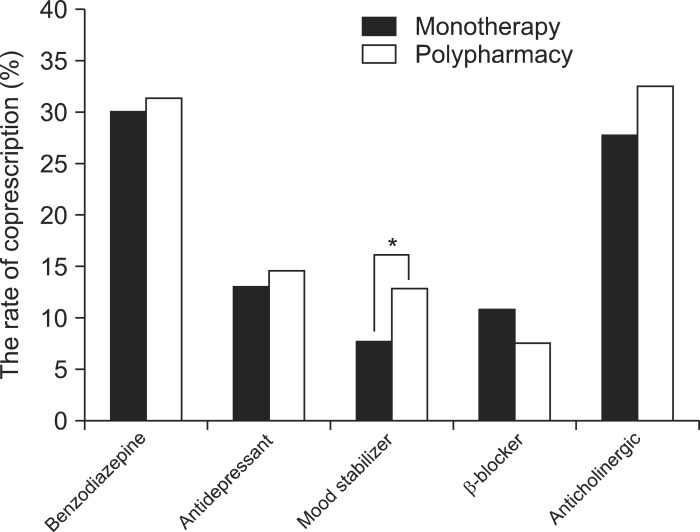
The most common psychotropic drugs other than antipsychotics that were prescribed to Korean patients with schizophrenia were benzodiazepines (n=258, 30.3%), anticholinergic drugs (n=245, 28.8%), antidepressants (n=113, 13.3%), β-blockers (n=86, 10.1%), and mood stabilizers (n=74, 8.7%) (Fig. 1). A greater rate of co-prescription for benzodiazepines, mood stabilizers, antidepressants, and anticholinergic drugs, but not β-blockers, was observed, but the only statistically significant difference between the two groups was in the rate of prescription of mood stabilizers (p=0.035) (Table 5, Fig. 2).
Fig. 1.
Prescription patterns of other psychotropic medications for schizophrenia.
Table 5.
Comparison of other psychotropic medications used for schizophrenia between the antipsychotic monotherapy and polypharmacy groups
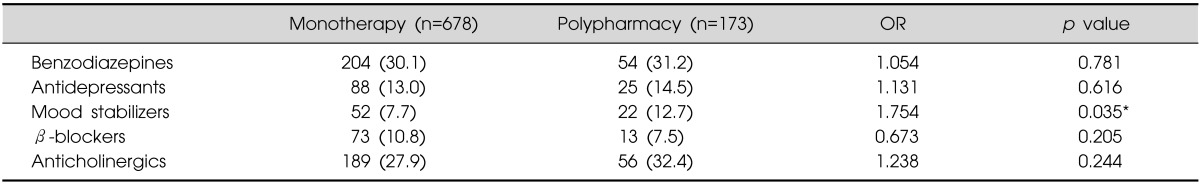
Values are presented as number (%).
*p<0.05.
OR, odds ratio.
Fig. 2.
Comparison of other psychotropic medications used for schizophrenia between the antipsychotic monotherapy and polypharmacy groups.
*p<0.05.
DISCUSSION
The present study investigated the rates of antipsychotic polypharmacy, the use of atypical antipsychotics, and the prescription patterns for other psychotropic drugs in schizophrenic patients in Korea. To our knowledge, this is the first relatively large-scale study to evaluate the prescription patterns of patients with schizophrenia in Korea.
Approximately 20% of patients were prescribed antipsychotic polypharmacy, and this treatment regimen was associated with a longer duration of illness, more severe positive symptoms, and poorer social function. In 2012, Gallego et al.15) performed a systemic review of studies from 1970 to 2009 and found that the global median rate for the prescription of antipsychotic polypharmacy was 19.6%, and that the rate of 32% in Asia was higher compared to in regions such as North America and Oceania. Similarly, the rate of antipsychotic polypharmacy in six East Asian countries was 43.4% in 2009.25) According to the present findings, there is a relatively low percentage of Korean schizophrenic patients (approximately 20%) receiving antipsychotic polypharmacy compared to other East Asian countries.
The present findings revealed that, in Korea, the rate of typical antipsychotics used in antipsychotic monotherapy was ~7% and the rate of atypical antipsychotics used was ~93%. Of the patients receiving antipsychotic polypharmacy, ~7% were prescribed a combination of typical+typical antipsychotics, ~47% were prescribed a combination of atypical+atypical antipsychotics, and ~47% were prescribed a combination of typical+atypical antipsychotics. There are several reasons why Korean clinicians generally prefer to use atypical rather than typical antipsychotics when combining antipsychotic medications. First, atypical antipsychotics are widely distributed in Korea and the cost of these drugs is typically only half to one-third of those in the United States. For example, in the United States, olanzapine costs 2.2 times more than in Korea.26) Second, it may be assumed that the spread and influence of the Korean Medication Algorithm Project (KMAP) for schizophrenia has had a non-negligible effect in Korea. Several follow-up studies to assess the feasibility of this algorithm in Korean clinical settings provided the initial rationale for the prescription of atypical antipsychotics. The KMAP algorithm was developed in 2001 and recommended the prescription of atypical antipsychotics regardless of the history of typical antipsychotic failure.27) Third, the preferential use of atypical antipsychotics may be due to their superiority with regards to side effects, especially extrapyramidal symptoms (EPS). Comparative studies evaluating typical and atypical antipsychotics have reported the occurrence of deleterious side effects associated with the use of typical antipsychotics28,29) and, in this sense, particular sociocultural factors in Korea must be taken into consideration. Because of the social stigma associated with schizophrenia in Korea, patients and clinicians are reluctant to use typical antipsychotics that can result in EPS, an easily recognizable outward characteristic of functional disability in a psychiatric patient.30) Lastly, the present results may be due to the fact that the majority of the data (81.6%) were gathered from 41 tertiary university hospitals. Compared to private hospitals or chronic mental hospitals, tertiary university hospitals are more likely to accept and use atypical antipsychotics due to their cost effectiveness and are less likely to be influenced by external factors, such as the Medicare and Medicaid systems of Korea, which could direct the choice of treatment.7)
Furthermore, the tendency to use atypical antipsychotic polypharmacy may be due to the increased availability of newer antipsychotics or the changing pattern of prescriptions in recent years. Additionally, difficulties in computing titrations between typical and atypical antipsychotics may also be a factor.31) It has been shown that antipsychotic polypharmacy may be superior to monotherapy in certain clinical situations32) and a pharmacological justification for the combination and long-term use of atypical drugs with conventional drugs based on differing receptor profiles has been proposed.33) The present findings reflect a trend towards the prescription of atypical antipsychotic medications for schizophrenia patients in Korea.
When compared with studies completed in the last decade, the present findings indicate that the prescription pattern for antipsychotics in Korea has changed over time. An international collaborative study by Chong et al.16) investigating the prescription patterns of antipsychotic drugs for schizophrenia in six East Asian countries demonstrated that in 2001 the rate of antipsychotic polypharmacy was 46% and the rate of atypical antipsychotic use was 28.1%. These findings also showed a wide inter-country variation in the prescription of atypical antipsychotics; the rate of atypical antipsychotic prescription was 27.1% in Korea. The authors highlighted these differences in prescription patterns as well as the under-utilization of atypical antipsychotic drugs in East Asia compared with the United States, which is inconsistent with the results of the present study. In this study of an exclusively Korean population there was an increasing preference for the use of atypical antipsychotics for the treatment of schizophrenia.
Recently, the range of choices for antipsychotic medication has been broadened for clinicians and patients as newer antipsychotics become available. This enables patients to receive a greater percentage of atypical antipsychotic prescriptions as those being treated with typical antipsychotics are switched to atypical antipsychotics.33) It could be inferred that the rate of antipsychotic polypharmacy has decreased and that the rate of atypical antipsychotic use has increased. The reason for this trend is not clear, but it is possible that the replacement of typical antipsychotic polypharmacy (typical antipsychotics+typical antipsychotics) with atypical antipsychotic monotherapy due to greater efficacy and less EPS is associated with the use of atypical antispsychotics.15) Another remarkable finding from the present study is the marked change in the antipsychotic prescription pattern over a relatively short period of time. Therefore, the therapeutic guidelines directing the prescription of drugs for schizophrenic patients should undergo frequent review as new drugs enter the Korean market.34)
Approximately one-third of patients were prescribed antipsychotics in conjunction with benzodiazepines, while the co-prescription of anticholinergic drugs, antidepressants, or β-blockers occurred at a lesser rate. The use of benzodiazepines was associated with a marked increase in mortality among patients with schizophrenia, whereas the concomitant use of antidepressants or other antipsychotics was not.35) Therefore, the co-prescription of benzodiazepines with antipsychotics for schizophrenia patients should be monitored. Vares et al.18) observed that, at some point, almost all patients (95%) in their study had been co-prescribed antipsychotics and benzodiazepines but that these treatment periods were short, at only ~14% of the total duration of antipsychotic medication. Given that in the present study there was a risk of increased mortality and limited information regarding the duration of polypharmacy relative to the total time of antipsychotic use, further studies will be needed to evaluate this point.
In the present study, 8.7% of patients were co-prescribed mood stabilizers along with antipsychotics with the most frequent being valproate, then lithium, carbamazepine, and lamotrigine. The utilization of mood stabilizers is lower in Europe and Asia compared to in North America, possibly due to the use of different medications to address similar symptoms and various side effects in different regions.15) It has been noted that Asian clinicians utilize other antipsychotics to treat residual/acute symptoms while aggression and hostility are treated with benzodiazepines or low-potency first-generation antipsychotics by European clinicians and mood stabilizers by North American clinicians.36) This may explain why the rate of mood stabilizers is low in Korea compared to in other regions.
The rate of co-prescription for mood stabilizers was higher in the polypharmacy group, and this was the only class of psychotropic drug that showed a significantly different rate of use between the two groups. Although this study does not include information regarding symptomatology ratings, such as the Positive and Negative Symptom Scale (PANSS), the correlation between scores on the CGI-SCH-S and PANSS is high and is greatest for positive symptoms.22) The higher rate of mood stabilizer co-prescription in the polypharmacy group may be associated with attempts to control aggression, irritability, or persistent positive symptoms, as suggested by the higher CGI-SCH-S-Positive score in the polypharmacy group.
The rate of coprescription of an antidepressant with antipsychotics was 13.3% in this study. The rate of coprescription of antidepressants in Korea was relatively low compared to a report showing that 28% of patients with schizophrenia in the United States were prescribed an antidepressant in combination with their antipsychotics.37) It also referred to a prior report that Asian clinicians did not use antidepressants as much as clinicians in other regions. According to the review assessing the prevalence of antipsychotic polypharmacy across regions, the use of antidepressants was less common in Asia (7%) compared to Europe (24%), Oceania (24.7%) and North America (19.3%). This low use of antidepressants in Asia can be explained by their use of a second antipsychotic to target depression. The under-recognition of depression in schizophrenia patients can also be a factor for the low use of antidepressants in Asia.15)
The present study had several limitations. First, the original three studies were not designed with the intention to identify prescription patterns in a real-world setting but rather to assess the effects of switching antipsychotic medications. Patients taking certain antipsychotics, including clozapine and long-acting injections, were excluded from the current study, as were patients with the possibility of suicidal thoughts or aggression. Most of the patients were moderately ill but could voluntarily agree to participate in the study continually. It is quite possible that there was a selection bias due to the inclusion and exclusion criteria of the original studies and, thus, the generalizability of the results may be limited. Second, this study was based on cross-sectional research regarding antipsychotic prescription patterns. Consequently, the present study was unable to discriminate continuous antipsychotic polypharmacy from temporary antipsychotic polypharmacy during a cross-titration period. Additional studies will be needed to reflect the longitudinal definitions of antipsychotic polypharmacy. Third, information concerning psychopathology and adverse effects were not included.
Despite these limitations, the present study demonstrated that little is known regarding the prescription patterns of antipsychotic medications and other psychotropic drugs in schizophrenic patients in Korea. This study also revealed distinct prescription patterns in Korea, especially concerning antipsychotic polypharmacy.
References
- 1.Centorrino F, Goren JL, Hennen J, Salvatore P, Kelleher JP, Baldessarini RJ. Multiple versus single antipsychotic agents for hospitalized psychiatric patients: case-control study of risks versus benefits. Am J Psychiatry. 2004;161:700–706. doi: 10.1176/appi.ajp.161.4.700. [DOI] [PubMed] [Google Scholar]
- 2.Stahl SM, Grady MM. High-cost use of second-generation antipsychotics under California's Medicaid program. Psychiatr Serv. 2006;57:127–129. doi: 10.1176/appi.ps.57.1.127. [DOI] [PubMed] [Google Scholar]
- 3.Correll CU, Frederickson AM, Kane JM, Manu P. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Schizophr Res. 2007;89:91–100. doi: 10.1016/j.schres.2006.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fleischhacker WW, Uchida H. Critical review of antipsychotic polypharmacy in the treatment of schizophrenia. Int J Neuropsychopharmacol. 2012:1–11. doi: 10.1017/S1461145712000399. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13:318–378. doi: 10.3109/15622975.2012.696143. [DOI] [PubMed] [Google Scholar]
- 6.Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. American Psychiatric Association; Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl):1–56. [PubMed] [Google Scholar]
- 7.Ahn YM, Kwon JS, Bahk WM, Kim CE, Park JI, Lee SY, et al. The feasibility test of Korean medication algorithm for the treatment with schizophrenic patients (II): the problem for applying algorithm to the real clinical situation and opinion of revision. Korean J Psychopharmacol. 2006;17:35–49. [Google Scholar]
- 8.Paton C, Lelliott P, Harrington M, Okocha C, Sensky T, Duffett R. Patterns of antipsychotic and anticholinergic prescribing for hospital inpatients. J Psychopharmacol. 2003;17:223–229. doi: 10.1177/0269881103017002012. [DOI] [PubMed] [Google Scholar]
- 9.Procyshyn RM, Honer WG, Wu TK, Ko RW, McIsaac SA, Young AH, et al. Persistent antipsychotic polypharmacy and excessive dosing in the community psychiatric treatment setting: a review of medication profiles in 435 Canadian outpatients. J Clin Psychiatry. 2010;71:566–573. doi: 10.4088/JCP.08m04912gre. [DOI] [PubMed] [Google Scholar]
- 10.Santone G, Bellantuono C, Rucci P, Picardi A, Preti A, de Girolamo G. Patient characteristics and process factors associated with antipsychotic polypharmacy in a nationwide sample of psychiatric inpatients in Italy. Pharmacoepidemiol Drug Saf. 2011;20:441–449. doi: 10.1002/pds.2083. [DOI] [PubMed] [Google Scholar]
- 11.Sim K, Su A, Fujii S, Yang SY, Chong MY, Ungvari GS, et al. Antipsychotic polypharmacy in patients with schizophrenia: a multicentre comparative study in East Asia. Br J Clin Pharmacol. 2004;58:178–183. doi: 10.1111/j.1365-2125.2004.02102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suokas JT, Suvisaari JM, Haukka J, Korhonen P, Tiihonen J. Description of long-term polypharmacy among schizophrenia outpatients. Soc Psychiatry Psychiatr Epidemiol. 2013;48:631–638. doi: 10.1007/s00127-012-0586-6. [DOI] [PubMed] [Google Scholar]
- 13.Stahl SM, Grady MM. A critical review of atypical antipsychotic utilization: comparing monotherapy with polypharmacy and augmentation. Curr Med Chem. 2004;11:313–327. doi: 10.2174/0929867043456070. [DOI] [PubMed] [Google Scholar]
- 14.Gilmer TP, Dolder CR, Folsom DP, Mastin W, Jeste DV. Antipsychotic polypharmacy trends among Medicaid beneficiaries with schizophrenia in San Diego County, 1999-2004. Psychiatr Serv. 2007;58:1007–1010. doi: 10.1176/ps.2007.58.7.1007. [DOI] [PubMed] [Google Scholar]
- 15.Gallego JA, Bonetti J, Zhang J, Kane JM, Correll CU. Prevalence and correlates of antipsychotic polypharmacy: a systematic review and meta-regression of global and regional trends from the 1970s to 2009. Schizophr Res. 2012;138:18–28. doi: 10.1016/j.schres.2012.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chong MY, Tan CH, Fujii S, Yang SY, Ungvari GS, Si T, et al. Antipsychotic drug prescription for schizophrenia in East Asia: rationale for change. Psychiatry Clin Neurosci. 2004;58:61–67. doi: 10.1111/j.1440-1819.2004.01194.x. [DOI] [PubMed] [Google Scholar]
- 17.Shim IH, Woo YS, Jun TY, Kim KS, Bahk WM. Changes in antipsychotic drug usage in the psychiatric inpatients at a university hospital between 1997, 2003-2004 and 2009-2010. Korean J Psychopharmacol. 2012;23:57–64. [Google Scholar]
- 18.Vares M, Saetre P, Strålin P, Levander S, Lindström E, Jönsson EG. Concomitant medication of psychoses in a lifetime perspective. Hum Psychopharmacol. 2011;26:322–331. doi: 10.1002/hup.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi HJ, Jung SH, Kang MH, Lee JS, Bae JN, Kim CE. Antipsychotics prescribing patterns of patients with schizophrenia admitted to Korean general hospital psychiatric unit: 2001 to 2008. Clin Psychopharmacol Neurosci. 2011;9:17–22. doi: 10.9758/cpn.2011.9.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 1997;154(4 Suppl):1–63. doi: 10.1176/ajp.154.4.1. [DOI] [PubMed] [Google Scholar]
- 21.Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663–667. doi: 10.4088/jcp.v64n0607. [DOI] [PubMed] [Google Scholar]
- 22.Haro JM, Kamath SA, Ochoa S, Novick D, Rele K, Fargas A, et al. SOHO Study Group. The clinical global impression-schizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatr Scand Suppl. 2003;(416):16–23. doi: 10.1034/j.1600-0447.107.s416.5.x. [DOI] [PubMed] [Google Scholar]
- 23.Patrick DL, Burns T, Morosini P, Rothman M, Gagnon DD, Wild D, et al. Reliability, validity and ability to detect change of the clinician-rated Personal and Social Performance scale in patients with acute symptoms of schizophrenia. Curr Med Res Opin. 2009;25:325–338. doi: 10.1185/03007990802611919. [DOI] [PubMed] [Google Scholar]
- 24.Nasrallah H, Morosini P, Gagnon DD. Reliability, validity and ability to detect change of the Personal and Social Performance scale in patients with stable schizophrenia. Psychiatry Res. 2008;161:213–224. doi: 10.1016/j.psychres.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Xiang YT, Wang CY, Si TM, Lee EH, He YL, Ungvari GS, et al. Antipsychotic polypharmacy in inpatients with schizophrenia in Asia (2001-2009) Pharmacopsychiatry. 2012;45:7–12. doi: 10.1055/s-0031-1286345. [DOI] [PubMed] [Google Scholar]
- 26.Han CH. A cost-effectiveness of atypical antipsychotics. Korean J Psychopharmacol. 2005;16:163–176. [Google Scholar]
- 27.Bae SO, Ahn YM, Kwon JS, Bahk WM, Kang DY, Kee BS, et al. The feasibility test of Korean medication algorithm for the treatment with schizophrenic patients (I): analysis focusing on the effectiveness of treatment. Korean J Psychopharmacol. 2006;17:24–34. [Google Scholar]
- 28.Voruganti L, Cortese L, Oyewumi L, Cernovsky Z, Zirul S, Awad A. Comparative evaluation of conventional and novel antipsychotic drugs with reference to their subjective tolerability, side-effect profile and impact on quality of life. Schizophr Res. 2000;43:135–145. doi: 10.1016/s0920-9964(99)00154-1. [DOI] [PubMed] [Google Scholar]
- 29.Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo. A meta-analysis of randomized controlled trials. Schizophr Res. 1999;35:51–68. doi: 10.1016/s0920-9964(98)00105-4. [DOI] [PubMed] [Google Scholar]
- 30.Woo YS, Chae JH, Jun TY, Bahk WM. Concomitant use of anticholinergic agents with atypical antipsychotics in schizophrenic patients: a preliminary report. Korean J Psychopharmacol. 2006;17:174–180. [Google Scholar]
- 31.Wang PS, West JC, Tanielian T, Pincus HA. Recent patterns and predictors of antipsychotic medication regimens used to treat schizophrenia and other psychotic disorders. Schizophr Bull. 2000;26:451–457. doi: 10.1093/oxfordjournals.schbul.a033465. [DOI] [PubMed] [Google Scholar]
- 32.Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35:443–457. doi: 10.1093/schbul/sbn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ganguly R, Kotzan JA, Miller LS, Kennedy K, Martin BC. Prevalence, trends, and factors associated with antipsychotic polypharmacy among Medicaid-eligible schizophrenia patients, 1998-2000. J Clin Psychiatry. 2004;65:1377–1388. doi: 10.4088/jcp.v65n1013. [DOI] [PubMed] [Google Scholar]
- 34.Shinfuku N, Tan CH. Pharmacotherapy for schizophrenic inpatients in East Asia-changes and challenges. Int Rev Psychiatry. 2008;20:460–468. doi: 10.1080/09540260802397560. [DOI] [PubMed] [Google Scholar]
- 35.Tiihonen J, Suokas JT, Suvisaari JM, Haukka J, Korhonen P. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry. 2012;69:476–483. doi: 10.1001/archgenpsychiatry.2011.1532. [DOI] [PubMed] [Google Scholar]
- 36.Volavka J, Citrome L. Heterogeneity of violence in schizophrenia and implications for long-term treatment. Int J Clin Pract. 2008;62:1237–1245. doi: 10.1111/j.1742-1241.2008.01797.x. [DOI] [PubMed] [Google Scholar]
- 37.Cascade EF, Kalali AH, Buckley PF. Current management of schizophrenia: antipsychotic monotherapy versus combination therapy. Psychiatry (Edgmont) 2008;5:28–30. [PMC free article] [PubMed] [Google Scholar]