Abstract
A case of snoring-induced angioedema of uvula is described in a patient who was treated with ACE inhibitor. The patient partially responded to complement C1-inhibitor concentrate and did not suffer any recurrences after the medication was withdrawn. When encountering a patient suffering from swellings of the orofacial area it should be considered whether the mechanism is mast-cell associated or not, as classical antiallergic treatment is ineffective in non-mast-cell-associated disease (ie, bradykinin-mediated angioedema). Other causes of uvular oedema are also discussed.
Background
Oedema of the oropharynx is a potentially lethal condition, as the airways might be compromised. Several causes for uvular oedema have been identified including allergic reactions, infectious diseases, trauma, adverse reactions, genetic diseases and intense snoring. However, in more than half of patients presenting with this symptom the cause is never identified (idiopathic uvular oedema).1 When encountering a patient with uvular oedema, one needs to immediately determine whether the airway is safe, as some forms of oedema (angioedema) are prone to progression when not timely treated and may also involve the mouth and laryngeal structures.2 3 In patients without anaphylactic symptoms (ie, urticaria, shortness of breath, low blood pressure), a non-allergic mechanism should be considered. If the patient reports intense snoring, this in itself might be the trigger and the symptom is usually self-limiting. However, other more serious or rare causes should also be considered. Local toxic reactions, for instance, can also give rise to isolated uvular oedema, so a thorough history of these patients should be obtained in the initial contact.4 Special attention should be drawn to the possibility of a bradykinin-induced angioedematous disease. Patients suffering from the genetic disease hereditary angioedema have a mortality rate of about 30% when left untreated, and this is due to oropharyngeal and laryngeal swellings.5 One case of snoring-related life-threatening angioedema of the uvula has been described in a patient with hereditary angioedema.6 Three cases of isolated uvular angioedema have been described in patients receiving ACE-inhibitors, but none of these were associated with snoring.7–9
The main consideration is to secure a safe airway, which in some cases requires endotracheal intubation (or in extreme cases cricothyrotomy) and intensive care admission. Emergency treatment with antiallergic drugs such as antihistamines, corticosteroids and epinephrine has proven ineffective against a bradykinin-mediated angioedema. Instead, bradykinin receptor antagonists or complement C1-inhibitor concentrate should be used.2 10 11
Case presentation
A 50-year-old Caucasian male was admitted to the department of otorhinolaryngology—head and neck surgery, due to difficulties in breathing and a sensation of a lump in the throat combined with a slight soreness. The patient's voice had changed and sounded more nasal. In the previous year he had already experienced two similar episodes of the same symptomatology, where the symptoms had subsided within 24 h in both incidents. All episodes had been associated with intense snoring the previous night and the patient had been admitted to the department of otorhinolaryngology for observation without receiving any treatment. The patient suffered from hypertension, hypercholesterolaemia, HIV infection, goitre, reflux and diabetes type II. He was treated with ACE-inhibitor, statin, anti-HIV nucleoside—and non-nucleoside reverse transcriptase inhibitors, a non-steroidal anti-inflammatory drug, proton pump inhibitor, calcium and a non-β cell stimulating antidiabetic drug. No new drugs were recently introduced and the patient had no known allergies. No itching or other skin symptoms were present. Family history revealed no association with angioedema.
Investigations
Vital signs were normal. Breathing was unrestricted. The oral cavity and oropharynx showed no other pathology than angioedema of the uvula (figure 1). There was no swelling of the face, tongue or peritonsillary area. Fiberoptic assessment of the pharynx and larynx showed no oedema other than the uvula. No urticaria or other rashes were observed at the physical assessment. The patient was slightly overweight.
Figure 1.

Isolated angioedema of the uvula.
Differential diagnosis
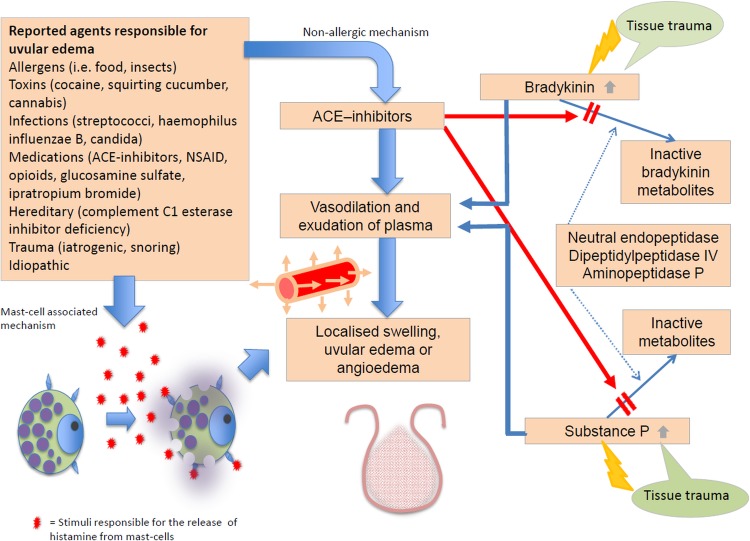
In patients experiencing oedema of the orofacial area, anaphylaxis should always be ruled out, as this can progress rapidly and become life threatening within minutes. Another differential diagnosis is iatrogenic angioedema due to adverse reactions (allergic, pseudoallergic or non-allergic) to medication, that is, ACE inhibitor-induced angioedema.12 Herpes simplex and other viral or bacterial infections can also cause oedema of the mucosa or submucosa of the oropharynx, however, isolated uvular oedema would be unusual in such cases.13 Hereditary and acquired angioedema represent other differential diagnoses and should be excluded by complement analyses whenever relevant.11 Trauma to the oropharyngeal tissue, including intense snoring, must be regarded as possible causes. Lastly, toxic reactions should be ruled out, as not all patients will voluntarily report an exposure to, for instance, cocaine or cannabis (figure 2).4 14
Figure 2.
Pathophysiology of different types of (angio)oedema of the uvula.
Treatment
The patient was suspected of having an adverse reaction to his ACE inhibitor, causing the on-call physician to target the bradykinin-pathway rather than the histamine-pathway. The patient received complement C1-inhibitor concentrate ∼15 units/kg injected intravenously over 10 min, as a bradykinin receptor antagonist was not available.
Outcome and follow-up
Within about 40 min significant improvement of the oedema was observed and the patient's voice had normalised. A slight soreness in the throat persisted. The next morning the uvula was still elongated, but the oedema had resolved. The ACE inhibitor was withdrawn. After some months the patient presented one more time to the ear, nose and throat department with soreness in the throat, but with no visible oedema and without the sensation of fullness in the back of the mouth.
Discussion
ACE inhibitor-induced angioedema is an underestimated clinical situation and currently the magnitude of this problem is unknown, although the incidence is reportedly rising as ACE inhibitors are increasingly prescribed.12 Owing to the large number of patients treated with this class of medication, ACE inhibitor-induced angioedema accounts for almost one-third of angioedema treated in emergency departments.10 This patient had a snoring-induced oedema of the uvula that responded partially to treatment with C1-inhibitor concentrate. We therefore assume that this could be the combination of ACE inhibitor-induced angioedema and the more classically described mechanically snoring-induced oedema. There are several case reports showing that trauma on its own can trigger angioedema attacks in patients suffering from hereditary angioedema, and a single report of a snoring-induced angioedema attack exists.6 There are fewer descriptions of trauma-induced angioedema in patients receiving ACE inhibitors and no reports of snoring-induced angioedema. Hereditary angioedema was an unlikely diagnosis in this case due to the age of the patient. The patient suffered no recurrence after withdrawal from ACE inhibitor, which further supports the theory that this medication could be involved in the pathogenesis.
Swelling of the orofacial area should always be considered a sign of potential airway closure, and patients should be observed in a hospital setting until the swelling is evidently regressing and the airway rendered secure.
Learning points.
Snoring can precipitate angioedema in patients receiving ACE inhibitors.
Uvular oedema is a serious symptom signalling a risk of suffocation.
Snoring is a well-known predisposing factor to uvular oedema.
Angioedema of the oropharynx can be mediated by bradykinin (ACE inhibitor-induced angioedema, hereditary and acquired complement C1-inhibitor deficiency).
Bradykinin-mediated angioedema should be treated with bradykinin-receptor antagonist or complement C1-inhibitor concentrate.
Footnotes
Contributors: ERR was involved in writing of manuscript, communication with patient, finding reference papers, final approval of manuscript and photography. KM was involved in writing of manuscript, final approval of manuscript and producing figures. AB was involved in critical reviewing of the paper, finding reference papers, final approval of manuscript.
Competing interests: ERR has received payment for teaching at one scientific meeting sponsored by MSD Norway. KM: None. AB has been involved in clinical research or educational events involving CSL Behring, Shire and Viropharma.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Alcoceba E, Gonzalez M, Gaig P, et al. Edema of the uvula: etiology, risk factors, diagnosis, and treatment. J Investig Allergol Clin Immunol 2010;20:80–3 [PubMed] [Google Scholar]
- 2.Rasmussen ER, Bindslev-Jensen C, Bygum A. Angioedema—assessment and treatment. Tidsskr Nor Legeforen 2012;132:2391–5 [DOI] [PubMed] [Google Scholar]
- 3.Ishoo E, Shah UK, Grillone GA, et al. Predicting airway risk in angioedema: staging system based on presentation. Otolaryngol Head Neck Surg 1999;121:263–8 [DOI] [PubMed] [Google Scholar]
- 4.Satar S, Gokel Y, Toprak N, et al. Life-threatening uvular angioedema caused by Ecbalium elaterium. Eur J Emerg Med 2001;8:337–9 [DOI] [PubMed] [Google Scholar]
- 5.Agostoni A, Cicardi M. Hereditary and acquired C1-inhibitor deficiency: biological and clinical characteristics in 235 patients. Medicine (Baltimore) 1992;71:206–15 [DOI] [PubMed] [Google Scholar]
- 6.Bork K, Koch P. Episodes of severe dyspnea caused by snoring-induced recurrent edema of the soft palate in hereditary angioedema. J Am Acad Dermatol 2001;45:968–9 [DOI] [PubMed] [Google Scholar]
- 7.Kuo DC, Barish RA. Isolated uvular angioedema associated with ace inhibitor use. J Emerg Med 1995;13:327–30 [DOI] [PubMed] [Google Scholar]
- 8.Stokes NA, Lemos JP. Male patient with throat swelling and painful swallowing. J Emerg Med 2013;44:1142–3 [DOI] [PubMed] [Google Scholar]
- 9.Viana-Tejedor A, Nunez-Gil IJ. Images in clinical medicine. Isolated uvular angioedema. N Engl J Med 2014;370:e24. [DOI] [PubMed] [Google Scholar]
- 10.Banerji A, Clark S, Blanda M, et al. Multicenter study of patients with angiotensin-converting enzyme inhibitor-induced angioedema who present to the emergency department. Ann Allergy Asthma Immunol 2008;100:327–32 [DOI] [PubMed] [Google Scholar]
- 11.Bowen T, Cicardi M, Farkas H, et al. 2010 International consensus algorithm for the diagnosis, therapy and management of hereditary angioedema. Allergy Asthma Clin Immunol 2010;6:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasmussen ER, Mey K, Bygum A. ACE inhibitor-induced angioedema—a dangerous new epidemic. Acta Derm Venereol 2014;94:260–4 [DOI] [PubMed] [Google Scholar]
- 13.Wedi B, Raap U, Wieczorek D, et al. Urticaria and infections. Allergy Asthma Clin Immunol 2009;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welling A. Enlarged uvula (Quincke's Oedema)—a side effect of inhaled cocaine? A case study and review of the literature. Int Emerg Nurs 2008;16:207–10 [DOI] [PubMed] [Google Scholar]