Abstract
Recent reports suggest that topical imiquimod cream is an effective treatment option for certain types of melanomas. No reports exist on the efficacy of using imiquimod cream to treat melanoma located on the plantar surface of the foot. We present two patients with a melanoma of the foot who had residual melanoma following surgical excision with acceptable margins. The patients were then treated with topical imiquimod for 8 weeks after which a repeat biopsy of the affected region showed no evidence of residual melanoma in situ. The use of topical imiquimod cream should be considered in the management of residual melanoma in situ of the plantar surface of the foot.
Background
Melanoma is responsible for 80% of deaths from skin cancer. One increasingly investigated treatment option for melanoma is the use of topical imiquimod cream. Imiquimod is a synthetic imidazoquinoline amine that has been approved for topical use in the treatment of superficial basal cell carcinoma, actinic keratosis and genital warts.1 Imiquimod modulates the immune response by activating Toll-like receptor 7 (TLR7), located on antigen-presenting cells.2 TLR7 activation subsequently induces release of proinflammatory cytokines that facilitates CD4+ T-cell induction as well as the CD8+ T-cell antitumour response.3 Topical imiquimod has been commonly used off-label to treat lentigo maligna4–9 and metastatic melanoma.10–12 Until now, all published cases of topical imiquimod use have been limited to application on non-acral areas of skin, such as on the head and neck.13 Plantar skin has a thick and compact cornified layer, which may hinder percutaneous absorption of a topically applied drug. Additionally, recurrence rates following surgical resection of plantar melanomas can be high. Therefore, we sought to investigate a mechanism for using this promising drug for the treatment of plantar melanomas. We report the first cases of successful use of topical imiquimod on a cutaneous melanoma located on the plantar surface of the foot.
Case presentation
An 83-year-old Caucasian man who presented with a skin lesion on his left heel (figure 1A), which on pathology was diagnosed as a stage II 2.5 mm malignant melanoma. There was no clinical or radiological evidence of distant metastasis. A wide local excision of the left heel with a minimum of 2 cm margins was performed (figure 1B) along with a partial calcanectomy to aid in the reconstruction of his left heel using a rotational flap. A sentinel lymph node biopsy of his left inguinal region was negative. A small focus of residual melanoma in situ was present at the peripheral margin (figure 2) between 8 o'clock and 2 o'clock in the excised specimen with the marking suture at 12 o'clock.
Figure 1.
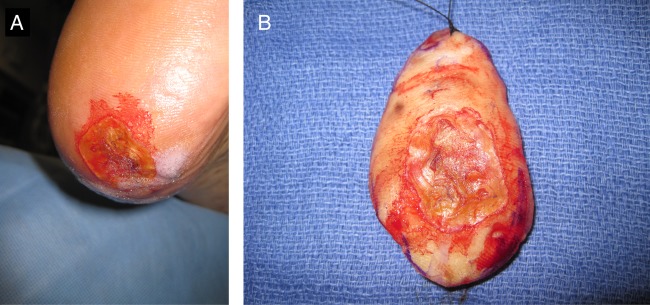
Preoperative view of the melanoma on the patient's left heel (A). Surgically resected specimen (B).
Figure 2.
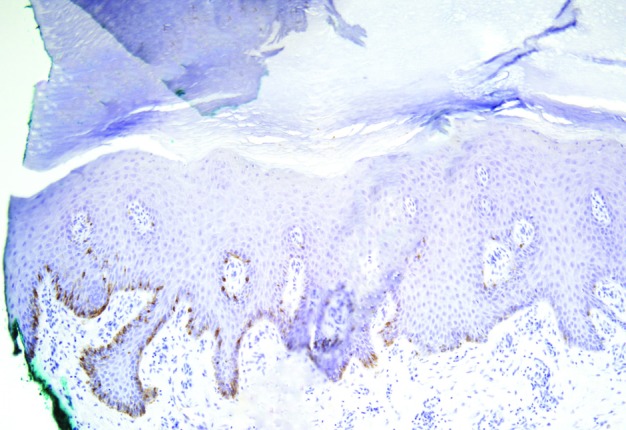
Residual melanoma in situ. A junctional proliferation of single melanocytes highlighted by Medical Entomology Laboratory-5, an immunohistochemical stain for melanocytes. The number of melanocytes on the right is normal whereas on the left they are crowded together and extend to the peripheral margin of the re-excision specimen (magnification ×10).
An 81-year-old Caucasian woman who presented with melanoma in situ on the medial side of her left great toe extending inferiorly to the plantar surface of the toe. A wide local excision of the medial and plantar surfaces of the left great toe was performed. The surgical pathology report was notable for residual melanoma in situ located almost circumferentially between 5 o'clock and 3 o'clock with the marking suture at 12 o'clock.
Treatment
After consultation with the patient and his family, the Caucasian man was treated with topical imiquimod 5% cream (Aldara, Medicis Pharmaceutical Corporation, Scottsdale, Arizona, USA) on the affected margins three times a week for 8 weeks given the presence of residual melanoma in situ. This modality was chosen instead of a surgical re-excision because of minimal residual disease and because the latter would have necessitated a complicated reconstructive procedure that the patient opted to forgo.
The Caucasian woman was also treated with a course of topical imiquimod 5% cream on the affected margins from 5 o'clock to 3 o'clock three times a week for 12 weeks.
Outcome and follow-up
For the Caucasian man, a re-excision of the entire involved area after 8 weeks of treatment revealed no evidence of residual melanoma on repeat histological examination. The patient did not have recurrent disease 4 years postprocedure.
In the follow-up of the Caucasian woman, a repeat excisional biopsy revealed clearance of the melanoma in situ between 5 o'clock and 3 o'clock, though a small focus of melanoma in situ was detected between 3 o'clock and 5 o'clock, in a region where the topical imiquimod was not applied. A second 12-week course of topical imiquimod was performed on the region with the newly positive margins. A subsequent excisional biopsy of this region revealed no evidence of residual melanoma in situ.
Discussion
These two cases demonstrate the response of a cutaneous plantar melanoma to the application of topical imiquimod 5% cream. We postulate that the use of topical imiquimod over the incision lines on the plantar foot may have enhanced the absorption of the drug through otherwise thick and impenetrable skin. Our outcomes further support current research demonstrating the utility of treating cutaneous melanomas with topical imiquimod cream.
Plantar melanomas are relatively rare in Caucasian population, though the foot is the most common site of melanoma involvement in Asian and African population.14 The currently recommended primary treatment of cutaneous melanoma is a wide excision with margins from 0.5 to 2.0 cm depending on the tumour thickness.15 In addition to the surgery, other alternative forms of therapy for melanoma include immunotherapy and chemotherapy.
The treatment of the margins of a surgical excision that are positive for melanoma in situ is undergoing change. Surgery is the traditionally the mainstay of treatment. However, the use of topical imiquimod may produce oncologically similar results. Additionally, the presentation of melanoma on the plantar surface of the foot often present a unique challenge for the treatment by surgical excision because of potential reconstructive difficulty. A wide excision of plantar melanomas is usually impossible to repair by direct closure given the lack of laxity of skin on the plantar foot. Surgery on this region often requires flap reconstruction or full-thickness skin grafts to enable a non-sedentary lifestyle16 which generally entails a more complex surgical procedure. Therefore, topical imiquimod potentially enhances the available treatment options for plantar melanomas.
Learning points.
Imiquimod can be used to treat a residual melanoma in situ after the definitive treatment of acral melanoma.
This should be proven by complete re-excision of the margins.
The dramatic response may have been enhanced by diffusion of imiquimod through the healing suture line.
Imiquimod is a viable option to treat melanoma on plantar surfaces.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Erickson C, Miller SJ. Treatment options in melanoma in situ: topical and radiation therapy, excision and Mohs surgery. Int J dermatol 2010;49:482–91 [DOI] [PubMed] [Google Scholar]
- 2.Hemmi H, Kaisho T, Takeuchi O, et al. Small anti-viral compounds activate immune cells via the TLR7 MyD88-dependent signaling pathway. Nat Immunol 2002;3:196–200 [DOI] [PubMed] [Google Scholar]
- 3.Narayan R, Nguyen H, Bentow JJ, et al. Immunomodulation by imiquimod in patients with high-risk primary melanoma. J Invest Dermatol 2011;321:163–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naylor MF, Crowson N, Kuwahara R, et al. Treatment of lentigo maligna with topical imiquimod. Br J Dermatol 2003;149(Suppl 66):66–70 [DOI] [PubMed] [Google Scholar]
- 5.Fleming CJ, Bryden AM, Evans A, et al. A pilot study of treatment of lentigo maligna with 5% imiquimod cream. Br J Dermatol 2004;151:485–8 [DOI] [PubMed] [Google Scholar]
- 6.Powell AM, Russell-Jones R, Barlow RJ. Topical imiquimod immunotherapy in the management of lentigo maligna. Clin Exp Dermatol 2004;29:15–21 [DOI] [PubMed] [Google Scholar]
- 7.Cotter MA, McKenna JK, Bowen GM. Treatment of lentigo maligna with imiquimod before staged excision. Dermatol Surg 2008;34:147–51 [DOI] [PubMed] [Google Scholar]
- 8.Van Meurs T, Van Doorn R, Kirtschig G. Treatment of lentigo maligna with imiquimod cream: a long-term follow-up study of 10 patients. Dermatol Surg 2010;36:853–8 [DOI] [PubMed] [Google Scholar]
- 9.Buettiker UV, Yawalkar NY, Braathen LR, et al. Imiquimod treatment of lentigo maligna: an open-label study of 34 primary lesions in 32 patients. Arch Dermatol 2008;144:943–5 [DOI] [PubMed] [Google Scholar]
- 10.Bong AB, Bonnekoh B, Franke I, et al. Imiquimod, a topical immune response modifier, in the treatment of cutaneous metastases of malignant melanoma. Dermatology 2002;205:135–8 [DOI] [PubMed] [Google Scholar]
- 11.Garcia MS, Ono Y, Martinez SR, et al. Complete regression of subcutaneous and cutaneous metastatic melanoma with high-dose intralesional interleukin 2 in combination with topical imiquimod and retinoid cream. Melanoma Res 2011;21:235–43 [DOI] [PubMed] [Google Scholar]
- 12.Miller AK, Dusing R, Meggison A, et al. Regression of internal melanoma metastases following application of topical imiquimod to overlying skin. J Drugs Dermatol 2011;10:302–5 [PubMed] [Google Scholar]
- 13.Missall TA, Hurley MY, Fosko SW. Lentiginous melanoma in situ treatment with topical imiquimod: need for individualized regimens. Arch Dermatol 2010;146:1309–10 [DOI] [PubMed] [Google Scholar]
- 14.Dwyer PK, Mackie RM, Watt DC, et al. Plantar malignant melanoma in a white Caucasian population. Br J Dermatol 1993;128:115–20 [DOI] [PubMed] [Google Scholar]
- 15.Coit DG, Andtbacka R, Bichakjian CK, et al. Melanoma. J Natl Compr Canc Netw 2009;7:250–75 [DOI] [PubMed] [Google Scholar]
- 16.Jung JY, Roh HJ, Lee SH, et al. Comparison of secondary intention healing and full-thickness skin graft after excision of acral lentiginous melanoma on foot. Dermatol Surg 2011;37:1245–51 [DOI] [PubMed] [Google Scholar]


