Abstract
Focal myositis secondary to an intramuscular vascular malformation has rarely been reported in the literature. We describe a 21-year-old woman presenting with left thigh pain. Imaging of the thigh muscles showed a vascular malformation and muscle biopsy demonstrated focal changes diagnosed initially as myositis. Ischaemia is thought to be the responsible mechanism.
Background
The two broad categories of vascular anomalies are vascular neoplasms and vascular malformations (VMs), differentiated by the absence of endothelial proliferative activity in the latter.1 VMs are further subcategorised into high flow (arteriovenous malformations and arteriovenous fistulas) and low flow (venous, lymphatic, capillary or a combination thereof).2 VMs can occur in the brain, liver, lungs, uterus and the limbs including the subcutaneous tissues and muscles.3 4 There are several case reports of VMs of the muscles of the limbs and the head and neck region,5–9 but to our knowledge none with a biopsy proven myositis. Intramuscular VMs tend to occur in younger age groups, more commonly affecting the lower extremities.10–12
We describe a young woman presenting with focal myositis in association with an intramuscular VM with an emphasis on the muscle biopsy features.
Case presentation
A 21-year-old woman presented to our clinic with a history of pain in the inner left thigh for 2 years. The pain was continuous, graded at 4/10 on the visual analogue pain scale, and was exacerbated by exercise and by prolonged sitting. She had limited mobility due to the pain. There was no history of visual disturbances, dysphagia, dysarthria, limbs weakness, backache, sphincteric dysfunction, trauma to the lower limb, fever, weight loss, skin rash, joint pain or change in urine colour. The patient has type 1 diabetes mellitus, well controlled on insulin and the last HbA1C was 7%. Her family history was unremarkable. The neurological examination was normal.
Investigations
The CK level was 45 IU/L (normal range: 29–165 IU/L). Rheumatological work-up was normal without evidence of vasculitis. Ultrasound (US) of the lower limb muscles showed a 4×1.3×1.5 cm, well defined ovoid hypoechoic lesion within the left adductor muscles with no internal vascularity. MRI of the left thigh showed a focal lesion, isointense on T1 and hyperintense on T2, within the adductor magnus muscle with surrounding oedema interpreted as myositis ossificans. Nerve conduction studies and electromyographic examination were normal. Biopsy of the left adductor muscle showed fasciitis, frequent degenerating, regenerating and necrotic fibres (perifascicular in some regions), chronic inflammatory infiltrates with a moderate number of T lymphocytes, often in the vicinity of blood vessels (figure 1). There were no ragged red fibres or inclusion bodies. Larger numbers of lymphocytes were present in the adjacent fibroconnective tissue. Electron microscopy showed no evidence of tubuloreticular inclusions in endothelial cells. A diagnosis of focal inflammatory myopathy was made and the patient was treated with methotrexate but did not improve after 4 months of therapy. A repeat MRI showed an isointense T1; hyperintense T2 lesion in the left adductor magnus muscle measuring 3.5×1.5×1.5 cm, with no muscle atrophy or fatty infiltration, suggestive of haemangioma (figure 2). Repeated US of the lower limb muscles showed an irregular solid hypoechoic mass in the left adductor magnus muscle measuring 3.3×1.7×1.2 cm. An intramuscular low-flow venous vascular malformation (VVM) was diagnosed and angiography was not deemed necessary in this patient.
Figure 1.
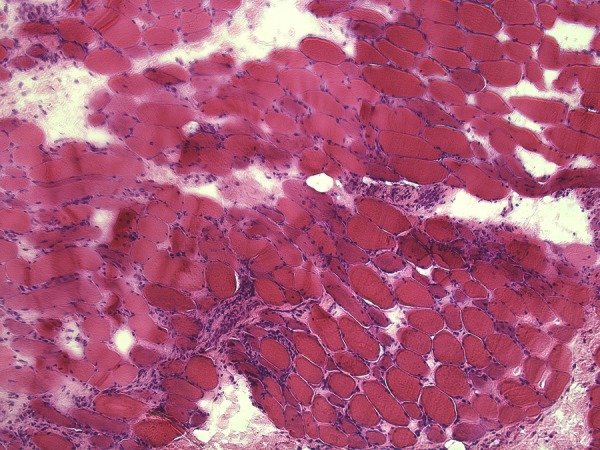
H&E-stained section (×10 magnification) reveals moderate infiltration by lymphocytes (confirmed by immunohistochemistry for CD45 and CD3 (not shown). Frequent severely atrophic fibres are present, often showing signs of regeneration.
Figure 2.
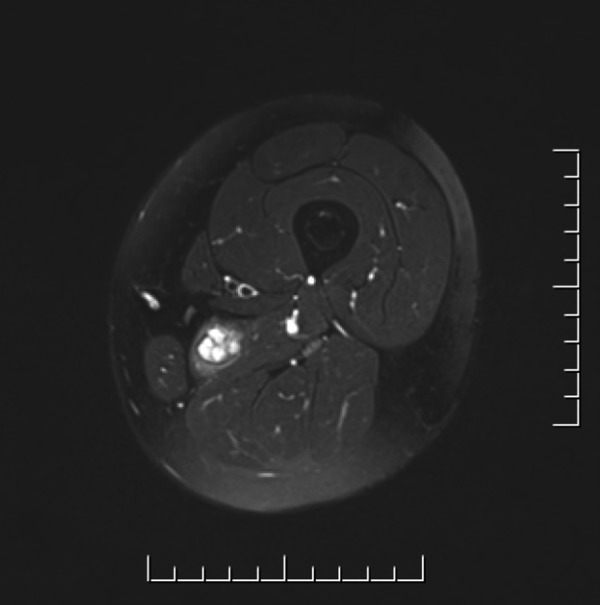
MRI of the left thigh showing T2 high-signal intensity lesion in the adductor magnus muscle.
Differential diagnosis
Polymyositis.
Myositis ossificans.
Infectious myositis.
Primary or secondary muscle tumours.
Idiopathic focal myositis.
Treatment
The patient was treated with sclerotherapy (figure 3) and the symptoms resolved.
Figure 3.

Ultrasound-guided sclerotherapy of the left thigh venous malformation.
Outcome and follow-up
The patient's symptoms resolved giving support to the VVM as the cause of the underlying symptoms.
Discussion
The large and heterogeneous group of inflammatory myopathies includes the forms known as polymyositis, dermatomyositis and inclusion body myositis. Idiopathic focal myositis was first described in 1977 by Heffner et al who published 16 cases presenting with a rapidly enlarging focal muscle mass with inflammatory myopathic features on biopsy.13 Generalisation of focal myositis is variable.9 14 Ischaemia has long been implicated in the pathogenesis of muscle inflammation.15 16 Most focal myositis cases reported in the literature are idiopathic, however, atheromatous emboli and diabetic angiopathy have been reported in association with acute focal myositis secondary to ischaemia.16–18 Less than 1% of VMs occur in skeletal muscle.19 In general, 90% of VMs—outside the central nervous system—are low flow (capillary, venous or lymphatic); the commonest among them are the VVMs.20 VVMs are usually present at birth and females are more commonly affected.10 21 Patients usually present with pain exacerbated by menses or pregnancy, swelling, bluish discolouration of the skin, bony deformities, fractures and intralesional bleeding, but some are asymptomatic.9 10 Our patient presented only with pain. Perhaps a clue to the underlying aetiology was the worsening of pain with exercise and with sitting upright, perhaps due to mechanical compression of the malformation with obstruction of venous outflow, or due to higher blood flow rates with exercise. MRI is the imaging modality of choice for primary classification and localisation, in addition to post treatment follow-up; however, some authorities suggest that rigorous assessment requires an angiogram, although that did not appear to be necessary in our case.22 US imaging has multiple disadvantages, being operator dependent with a limited field of view and restricted penetration.10 23 Treatment is tailored to the specific patient. It includes: aspirin and compressive garments, sclerotherapy and surgical resection.10 VMs are an important differential diagnostic consideration when assessing patients presenting with focal myositis in order to avoid unnecessary and potentially harmful treatments.
Learning points.
Consider vascular malformations (VMs) in the differential diagnosis of focal myositis.
The most common VMs outside the central nervous system are VVMs.
Exacerbation of pain by positions/activities that increase blood flow to the involved limb is a clue to the diagnosis.
Footnotes
Acknowledgements: The authors thank Dr Carolina Barnett who helped by removing the patient's name from the MRI and US figures.
Contributors: NMA reviewed the case and wrote the manuscript; T-RK contributed to the writing of the manuscript; VB contributed to the writing of the manuscript and to the revisions of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lowe LH, Marchant TC, Rivard DC, et al. Vascular malformations: classification and terminology the radiologist needs to know. Semin Roentgenol 2012;47:106–17 [DOI] [PubMed] [Google Scholar]
- 2.Donnelly LF, Adams DM, Bisset GS., III Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol 2000;174:597–608 [DOI] [PubMed] [Google Scholar]
- 3.Wulff C, Lorentzen T. Extracranial arteriovenous malformation diagnosed on color Doppler imaging. Eur J Ultrasound 1998;7:205–8 [DOI] [PubMed] [Google Scholar]
- 4.Ciani S, Merino J, Vijayalakhsmi S, et al. Acquired uterine arteriovenous malformation with massive endometrial stromal component. Histopathology 2005;46:234–5 [DOI] [PubMed] [Google Scholar]
- 5.Theruvil B, Kapoor V, Thalava R, et al. Vascular malformations in muscles around the knee presenting as knee pain. Knee 2004;11:155–8 [DOI] [PubMed] [Google Scholar]
- 6.Geibprasert S, Fanning NF, Pedroza A, et al. Imaging characteristics of arteriovenous malformations simulating vascular tumors of the temporalis muscle: a report of two cases. Int J Oral Maxillofac Surg 2010;39:402–6 [DOI] [PubMed] [Google Scholar]
- 7.Karaman E, Mercan H, Ozdilek A, et al. Huge arteriovenous malformation in masseter muscle. J Craniofac Surg 2009;20:1292–4 [DOI] [PubMed] [Google Scholar]
- 8.Jung HC, Kim DH, Park BK, et al. Extensive intramuscular venous malformation in the lower extremity. Ann Rehabil Med 2012;36:893–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hein KD, Mulliken JB, Kozakewich HP, et al. Venous malformations of skeletal muscle. Plast Reconstr Surg 2002;110:1625–35 [DOI] [PubMed] [Google Scholar]
- 10.Rogalski R, Hensinger R, Loder R. Vascular abnormalities of the extremities: clinical findings and management. J Pediatr Orthop 1993;13:9–14 [DOI] [PubMed] [Google Scholar]
- 11.Breugem CC, Maas M, Breugem SJ, et al. Vascular malformations of the lower limb with osseous involvement. J Bone Joint Surg Br 2003;85:399–405 [DOI] [PubMed] [Google Scholar]
- 12.Heffner RR, Jr, Armbrustmacher VW, Earle KM. Focal myositis. Cancer 1977;40:301–6 [DOI] [PubMed] [Google Scholar]
- 13.Froissart A, Pagnoux C, Koskas F, et al. [Intramuscular vascular malformations as a differential diagnosis of focal myositis]. Rev Med Interne 2006;27:50–3 [DOI] [PubMed] [Google Scholar]
- 14.Heffner RR, Jr, Barron SA. Polymyositis beginning as a focal process. Arch Neurol 1981;38:439–42 [DOI] [PubMed] [Google Scholar]
- 15.Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet 2003;362:971–82 [DOI] [PubMed] [Google Scholar]
- 16.Reyes CV, Espiritu BR. Skin infarcts and myositis associated with atheromatous microemboli. Int J Dermatol 1985;24:522–3 [DOI] [PubMed] [Google Scholar]
- 17.Silberstein L, Britton KE, Marsh FP, et al. An unexpected cause of muscle pain in diabetes. Ann Rheum Dis 2001;60:310–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vatca M, Tejwani S, Yates T. Ischemic myositis in a diabetic patient receiving chemotherapy. Community Oncol 2009;6:69, 79 [Google Scholar]
- 19.Rai P, Setia S, Kalra N, et al. Intramuscular vascular malformation of the masseter muscle presenting with turkey wattle sign. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:618. [DOI] [PubMed] [Google Scholar]
- 20.Alessandrino F, Maira A, Tarantino CC. US and MRI features in venous vascular malformation of the abdominal wall. A case report. J Ultrasound 2012;15:171–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mazoyer E, Enjolras O, Bisdorff A, et al. Coagulation disorders in patients with venous malformation of the limbs and trunk: a case series of 118 patients. Arch Dermatol 2008;144:861–7 [DOI] [PubMed] [Google Scholar]
- 22.Flors L, Leiva-Salinas C, Maged IM, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics 2011;31:1321–40; discussion 40–1 [DOI] [PubMed] [Google Scholar]
- 23.Moukaddam H, Pollak J, Haims AH. MRI characteristics and classification of peripheral vascular malformations and tumors. Skeletal Radiol 2009;38:535–47 [DOI] [PubMed] [Google Scholar]


