Abstract
Amoebiasis is an uncommon infection in developed countries caused by the protozoan Entamoeba histolytica. Amoebic liver abscess is the most frequent extraintestinal presentation of the disease; pleuropulmonary involvement is rare, occurring mostly by rupture of the abscess into the pleural space or lung parenchyma. We describe a case of a 48-year-old migrant from São Tomé e Príncipe, with fever, wasting, dry cough and right upper abdominal pain for the past 2 months. The CT scan revealed a voluminous liver abscess with thrombosis of the right suprahepatic and inferior vena cava, right pulmonary lobar abscess and multiple diffuse condensations in both lungs. Aspirated pus resembled anchovy sauce; blood and aspirated material cultures for infectious agents were negative. Serology for E. histolytica was positive, and the diagnosis of hepatopulmonary amoebiasis with infectious phlebitis was confirmed by positive PCR in the liver pus. Treatment with metronidazole+paramomycin led to clinical and radiological resolution.
Background
Although it is not often possible to make an aetiological distinction solely based on the presentation, amoebiasis should be considered as a cause of primary liver abscess, especially in patients who are from or have travelled to an endemic area within the past 6 months. In Portugal there is a higher than expected incidence of amoebic disease, in part due to its close relation with African countries that were once Portuguese colonies. We found this case of particular interest because of the rare form of pleuropulmonary affection, with dissemination of the disease from infectious and thrombotic phlebitis by direct invasion of the protozoan. The diagnosis was possible due to application of an experimental confirmatory method involving Entamoeba histolytica determination by PCR in the aspirated pus.
Case presentation
The patient is a 48-year-old man from São Tomé e Príncipe (Western Africa), resident of Portugal for 8 months. Previously healthy, he developed a clinical picture of intermittent fever, wasting and anorexia 2 months before the ward admittance, with dry cough and pain in the right upper abdominal quadrant. He reported no relevant medical illnesses.
Investigations
The clinical evaluation included a thoracoabdominal CT scan, which revealed a 9 cm thickened-wall hepatic lesion of liquid content in segment VII, suspicious for hepatic abscess. The hepatic abscess involved the right suprahepatic vein where a thrombus was identified, with extension to the inferior vena cava (figure 1). Abscess of the right superior pulmonary lobe of 8 cm diameter with air–fluid level. Diffuse foci of nodular condensation in both lung parenchyma, some with cavitation, namely in the left superior lobe, left inferior lobe and right inferior lobe, with dimensions between 2 and 3 cm diameter. Right pleural effusion with small volume (figure 2).
Figure 1.

Image from CT acquisition showing liver abscess (arrow) with associated inferior vena cava thrombus (double arrow) and pulmonary abscess (arrowhead).
Figure 2.
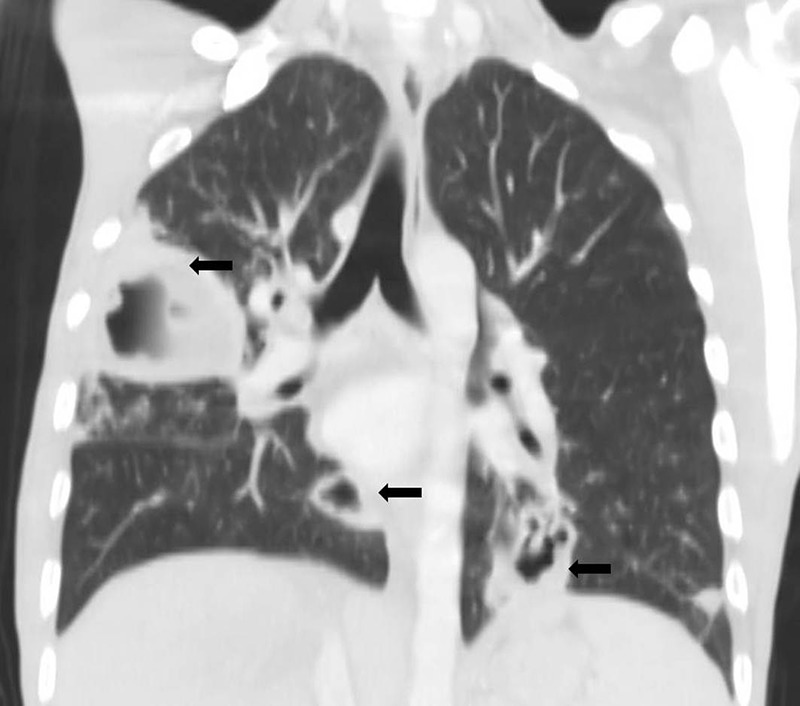
Image from CT acquisition showing several cavitated pulmonary lesions (arrows).
Laboratory analyses were unremarkable, except for C reactive protein moderately elevated; blood cultures were negative. Macroscopic examination of the aspirated hepatic and lung pus resembled anchovy sauce. Direct and cultural examinations, including for mycobacteria, were negative. Serology was positive for E. histolytica (indirect immunohaemagglutination and ELISA); negative for HIV antibodies;and positive PCR for E. histolytica.
Treatment
After collecting the blood cultures, treatment for pyogenic liver abscess was started with piperacillin–tazobactam (4.5 g 6/6 h) and metronidazole (750 mg three times a day). The first antibiotic was stopped due to the laboratory results; metronidazole was administered for 11 days and the intraluminal agent paramomycin (30 mg/kg in three divided doses) for 7 days thereafter.
Outcome and follow-up
The patient was re-evaluated 3 weeks later with the following results: disappearance of the smaller pulmonary lesions and hepatic abscess; frank volume reduction of the bigger lung abscess (figures 3 and 4); and symptomatic resolution.
Figure 3.
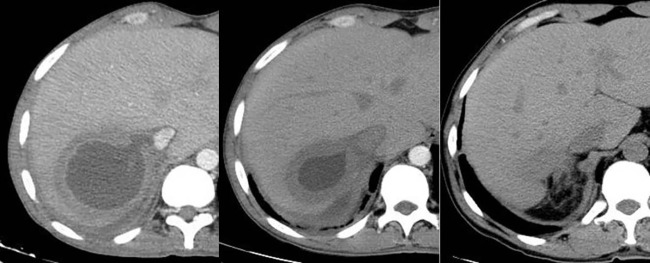
Axial CT images showing resolution of liver abscess, from left to right.
Figure 4.
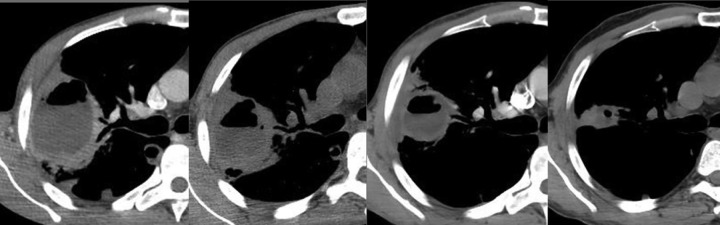
Axial CT images from several acquisitions showing pulmonary abscess response to therapy, from left to right.
Discussion
Symptoms of pain localised to the right upper abdominal quadrant together with protracted fever and other systemic symptoms suggest a hepatobiliary cause. Pyogenic liver abscesses usually develop following peritonitis due to leakage of intra-abdominal bowel contents, but they may also result from arterial haematogenous seeding in the setting of systemic infection. The aetiology is often polymicrobial but usually includes streptococci species.1–3 We managed to exclude the several infectious agents of hepatopulmonary abscesses. The chronicity of the process (2 months), the geographic origin of the patient and the presence of a bulky hepatic right lobe abscess implies admitting an amoebic aetiology. The abscess located in the right hepatic lobe is the most frequent extraintestinal lesion4; the majority of pleuropulmonary amoebiasis cases reported in the literature suggest that it occurs contiguously with (rupture of) the liver abscess or by lymphatic drainage from it.5 6 Infection may also pass to the thorax directly from the primary intestinal lesion through haematogenous spread, and inhalation of dust containing cysts or aspiration of cysts/trophozoites of E. histolytica in the lungs are some other hypothetical routes.6 Rarely, a posterior amoebic liver abscess can burst into the inferior vena cava7 and develop an embolism and thromboembolic disease of the lungs with congestive cardiac failure or cor pulmonale.
This case included pulmonary abscesses at different levels, suggesting haematogenous dissemination. The non-hepatic extraintestinal foci, namely in the lungs, are usually described in this context and have been associated with alcoholism, malnutrition and left-to-right cardiac shunt.6 The inferior vena cava thrombosis leads us to presume that there was involvement of the suprahepatic veins and inferior vena cava by E. histolytica, occurring infectious phloebitis, with pulmonary embolisation resulting from it.
In countries with high prevalence of the disease a negative serology allows the exclusion of amoebic aetiology. Positive serology occurs in intestinal colonisation, parenchymatous lesions and in 35% of healthy people, not making the distinction between past and active infection possible.8 9 The isolation of E. histolytica in the aspirated pus is extremely improbable, since the parasite is active in the wall abscess.10 The determination of E. histolytica by PCR in the aspirated content of the lesions is an experimental method with good results that confirms the diagnosis.11–14
Learning points.
Amoebiasis is an important aetiology of pyogenic liver abscess, to be considered in the relevant epidemiological context.
Pleuropulmonary amoebiasis is an infrequent presentation of the disease, usually presenting as a pleural effusion or empyema resulting from rupture of the liver abscess, but may also result from haematogenous spread via systemic circulation or by direct venous invasion of the microorganism.
Diagnosis is difficult since serology, the most common method used, does not distinguish between past and active infection. Standard development of PCR may be a useful arm to diagnosis in the future.
Early detection and prompt treatment of the disease is essential and curative, with elimination of the possible complications of the disease.
Acknowledgments
The authors would like to acknowledge Dr Vítor Brotas and Professor Francisco Oliveira Martins, who always guided them with their wisdom. The authors also acknowledge Professor Sónia Lima and the coworkers of the “Instituto de Higiene e Medicina Tropical”, who contributed for the diagnosis with the PCR technique.
Footnotes
Contributors: CP a major contributor in writing and preparing the manuscript. PA the surgeon who accompanied the patient parallel to CP and revised the manuscript. JL aspirated the pyogenic content of the liver abscess via CT scan guidance and provided the images for the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Huang CJ, Pitt HA, Lipsett PA, et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg 1996;223:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohsen AH, Green ST, Read RC, et al. Liver abscess in adults: ten years experience in a UK centre. QJM 2002;95:797. [DOI] [PubMed] [Google Scholar]
- 3.Rahimian J, Wilson T, Oram V, et al. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis 2004;39:1654. [DOI] [PubMed] [Google Scholar]
- 4.Haque R, Huston CD, Hughes M, et al. Amebiasis. N Engl J Med 2003;348:1565. [DOI] [PubMed] [Google Scholar]
- 5.Shenoy VP, Vishwanath S, Indira B, et al. Hepato-pulmonary amebiasis: a case report. Braz J Infect Dis 2010;14:372–3 [PubMed] [Google Scholar]
- 6.Shamsuzzaman SM, Hashiguchi Y. Thoracic amebiasis. Clin Chest Med 2002;23:479–92 [DOI] [PubMed] [Google Scholar]
- 7.Sodhi KS, Ojili V, Sakhuja V, et al. Hepatic and inferior vena caval thrombosis: vascular complication of amebic liver abscess. J Emerg Med 2008;34:155. [DOI] [PubMed] [Google Scholar]
- 8.Joyce MP, Ravdin JI. Antigens of Entamoeba histolytica recognized by immune sera from liver abscess patients. Am J Trop Med Hyg 1988;38:74. [DOI] [PubMed] [Google Scholar]
- 9.Aucott JN, Ravdin JI. Amebiasis and “nonpathogenic” intestinal protozoa. Infect Dis Clin North Am 1993;7:467. [PubMed] [Google Scholar]
- 10.Salata RA, Ravdin JI. The interaction of human neutrophils and Entamoeba histolytica increases cytopathogenicity for liver cell monolayers. J Infect Dis 1986;154:19. [DOI] [PubMed] [Google Scholar]
- 11.Salles JM, Salles MJ, Moraes LA, et al. Invasive amebiasis: an update on diagnosis and management. Expert Rev Anti Infect Ther 2007;5:893. [DOI] [PubMed] [Google Scholar]
- 12.Petri WA, Singh U. Enteric amebiasis. In: Guerrant R, Walker DH, Weller PF, eds. Tropical infectious diseases: principles, pathogens, and practice. 2nd edn Philadelphia: Elsevier, 2006:967 [Google Scholar]
- 13.Khan U, Mirdha BR, Samantaray JC, et al. Detection of Entamoeba histolytica using polymerase chain reaction in pus samples from amebic liver abscess. Indian J Gastroenterol 2006;25:55. [PubMed] [Google Scholar]
- 14.Mehmet T, William A Petri., Jr Laboratory diagnosis of amebiasis. Clin Microbiol Rev 2003;16:713–29 [DOI] [PMC free article] [PubMed] [Google Scholar]


