Abstract
This study examines the ability of the theory of reasoned action (TRA) and the theory of planned behavior (TPB) to predict whether or not pediatricians encourage parents to get their adolescent daughters vaccinated against the human papillomavirus (HPV). Four-hundred and six pediatricians completed a mail survey measuring attitudes, subjective norms, perceived behavioral control, intentions, and behavior. Results indicate that pediatricians have positive attitudes, subjective norms, and perceived behavioral control toward encouraging parents to get their daughters vaccinated, that they intend to regularly encourage parents to get their daughters vaccinated against HPV in the next 30 days, and that they had regularly encouraged parents to get their daughters vaccinated against HPV in the past 30 days (behavior). Though the data were consistent with both the TRA and TPB models, results indicate that perceived behavioral control adds only slightly to the overall predictive power of the TRA, suggesting that attitudes and norms may be more important targets for interventions dealing with this topic and audience. No gender differences were observed for any of the individual variables or the overall fit of either model. These findings have important theoretical and practical implications for the development of health communication messages targeting health care providers in general, and for those designed to influence pediatricians’ communication with parents regarding the HPV vaccine in particular.
Genital human papillomavirus (HPV) is the most common sexually transmitted infection (STI), and it will infect most sexually active people in the United States at some time in their lives (Weinstock, Berman, & Cates, 2000). In June 2006, the U.S. Food and Drug Administration (FDA) approved an HPV vaccine for females between the ages of 9 and 26 years (FDA, 2006). Daley et al. (2006) note that “pediatricians will have an important role in promoting HPV vaccination, given that young adolescents are more likely to be seen by pediatricians than any other providers and that providers are known to have substantial influence on their patients’ immunization decisions” (p. 2281). As such, understanding the predictors of pediatricians’ intentions and behavior represents an important step in establishing effective vaccine delivery programs (Duval et al., 2007). The main purpose of this study is to help meet this need by determining if the theory of reasoned action (TRA) accurately predicts whether or not pediatricians encourage parents to get their 9- to 17-year-old daughters vaccinated against HPV.
BACKGROUND AND NEED
More than 20 million men and women are infected with HPV, with 6.2 million new cases each year (Dinh, Sternberg, Dunne, & Markowitz, 2008). Most cases of HPV do not have any symptoms, making it likely that an infected person will unknowingly transmit the virus to others. Although both men and women are equally likely to have HPV, it is more common for women to suffer adverse effects of HPV infection (Dihn et al., 2008; Freeman & Wingrove, 2005). One of the most common manifestations of HPV infection in both men and women is genital warts. Although both men and women can contract genital warts, a recent study found that women were three times more likely than men to report ever having a diagnosis of genital warts (Dihn et al., 2008). HPV infection can also cause more serious health problems such as cancer of the cervix, vulva, vagina, and anus in women, and penile and anal cancer in men (Parkin, 2006). The most common is cervical cancer, with sexually transmitted HPV infection responsible for 90–95% of all cervical cancer cases (Freeman & Wingrove, 2005). Each year, approximately 14,000 new cases of cervical cancer are diagnosed, and 4,000 women will die from the disease (Jansen & Shaw, 2004).
In 2006, the FDA approved a new vaccine administered in a three-shot series that protects young women from four strains of HPV, two of which cause more than 70% of cervical cancer cases and two of which cause approximately 90% of genital wart infections (Twombly, 2006). This vaccine is only the second vaccine to protect against an STI and prevent a form of cancer (the first was the hepatitis B vaccine that prevents liver cancer) (Pagliusi & Aguado, 2004). The HPV vaccine is most effective if administered before a woman becomes sexually active (Zimet, 2005). The vaccine is currently approved for girls and young women age 9 to 26 years, and the Advisory Committee on Immunization Practices (Markowitz et al., 2007) recommends routine vaccination of 11- and 12-year-old females. Use of the vaccine is expected to significantly reduce the occurrence of both genital warts and cervical cancer (Dihn et al., 2006; Duval et al., 2007)
Although many physicians report a willingness to recommend that girls be vaccinated against HPV, a number of specific concerns about the vaccine have been identified (Duval et al., 2007). The most common concern is that parents will be unreceptive to vaccinating their children (Kahn, 2007; Sussman et al., 2007). One study found that a majority (60%) of pediatricians believed parents would be concerned that administering the vaccine would encourage risky sexual behavior, and such concerns about upsetting a parent by offering the vaccine were negatively associated with intent to vaccinate patients (Daley et al., 2006). Other concerns include uncertainty about whether the vaccine will provide long-term immunity against cervical cancer and genital warts, and potential for the vaccination to give adolescents a false sense of security about their sexual health (Sussman et al., 2007). Guided by the theory of reasoned action, the current study was designed to gain a better understanding of how pediatricians’ attitudes and norms impact their intentions and behavior when it comes to recommending the HPV vaccine to parents of adolescent girls.
THEORY OF REASONED ACTION AND THEORY OF PLANNED BEHAVIOR
According to the theory of reasoned action (TRA; Ajzen & Fishbein, 1980; Fishbein & Ajzen, 1975), the best predictor of behavior (i.e., what a person actually does) is behavioral intention (i.e., a person’s intention to perform or not perform the behavior). Behavioral intention, in turn, is a joint function of a person’s attitude toward performing the behavior (i.e., the individual’s favorable or unfavorable predispositions toward the behavior) and subjective norms (i.e., the individual’s perception of the behavior expected by relevant significant others). A visual representation of this model is included in Figure 1. The theory of planned behavior (TPB; Ajzen, 1985) extends the TRA by adding a direct link from perceived behavioral control (i.e., the degree to which a person believes he or she can control the behavior in question) to both behavioral intention and behavior (see Figure 2). Several meta-analyses offer consistent support for the ability of both theories to predict intentions and behavior (Albarracin, Johnson, Fishbein, & Albarracin, 2001; Downs & Hausenblas, 2005).
FIGURE 1.
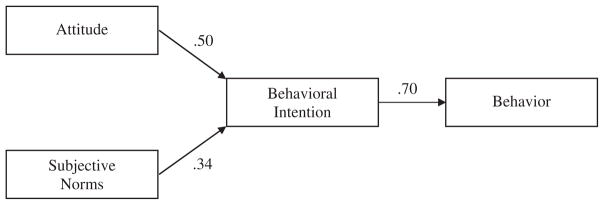
Path model predicting pediatrician HPV vaccination recommendations using the theory of reasoned action; χ2(2, N = 390) = 1.53, p = .47.
FIGURE 2.
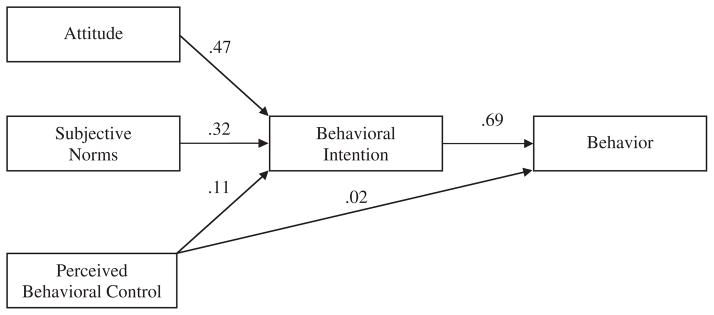
Path model predicting pediatrician HPV vaccination recommendations using the theory of planned behavior; χ2(2, N = 390) = 1.46, p = .48.
Though these theories are typically used to help explain patient behavior, Millstein (1996) argues that they should also be applicable to physician behavior. For example, Perkins et al. (2007) conducted a review of the literature and found nine studies that applied one or both of these theories to physician populations on a variety of topics, including mammography screening (Taylor, 1994), intention to prescribe antibiotics (Walker et al., 2001), and delivery of STI education services to adolescents (Millstein, 1996). A brief overview of the Millstein (1996) study is provided next, as it most closely relates to the current investigation. Millstein (1996) sent mail surveys measuring TRA constructs to 765 primary care physicians (including family physicians, obstetricians–gynecologists, pediatricians, and internists) in California. Results indicate that both the TRA and TPB accurately predicted primary care physicians’ intentions and behavior in Millstein’s study, with the TPB accounting for an additional 12% of the variance in physicians’ behavioral intentions and 2% of the variance in subsequent behavior.
While clearly related to the current investigation, it should be noted that the study conducted by Millstein (1996) took place more than a decade ago, focused on primary care physicians in general, and focused on education of male and female adolescents about STIs in general. On a related note, all nine of the studies reviewed by Perkins et al. (2007) took place between 1992 and 2003 (i.e., between 8 and 19 years ago), and only four of these nine studies focused on physician behavior, with the majority limiting their investigation to physician intentions. Thus, there seems to be a clear need for more recent research dealing with this important topic and target audience. To help meet this need, the current investigation took place in the summer of 2008, focused specifically on pediatricians, included a behavioral measure, and focused on communication with parents of 9-to 17-year-old female patients about a very specific behavior (i.e., encouraging parents to get their adolescent daughters vaccinated against HPV).
In sum, though several studies pertaining to physician knowledge, attitudes, and behavior regarding HPV and the HPV vaccine have been published since the HPV vaccine was approved in 2006 (Daley et al., 2006; Duval, 2007; Kahn et al., 2007; Keating et al., 2008; Sussman et al., 2007), few (Keating et al., 2008) were conducted after the vaccine was approved (i.e., most were conducted before the vaccine was approved and were therefore hypothetical in nature), few selected survey items based on established theory (Kahn et al., 2007), and none were explicitly guided by or designed to test theory. Further, though previous applications of the TRA and TPB in the health arena have focused primarily on predicting patient behavior, work by Perkins et al. (2007) suggests that they should provide a solid theoretical framework for predicting physician behavior in general, and the Millstein (1996) results indicate they might also predict physician communication with patients about STIs in particular. With the preceding discussion in mind, we hypothesize that: both the TRA and TPB will accurately predict whether or not pediatricians encourage parents to get their adolescent daughters vaccinated against HPV. Further, this study also seeks to answer the following research question: Does the TPB add significantly and substantially to the predictive power of the TRA for this behavior?
GENDER DIFFERENCES
Though females make up approximately 37% of primary care physicians overall, they make up nearly 52% of primary care physicians with a pediatrics specialty (Smart, 2007). This is relevant to the current study because Roter and Hall (2004) found that female primary care physicians tend to spend more time with patients and engage in more patient-centered communication. Further, both female and male physicians report significantly greater discomfort when taking a sexual history with patients of the opposite sex (Burd, Nevadunsky, & Bachmann, 2006). Unfortunately, there is limited information regarding pediatricians and their communication practices about sexually related topics with patients and their patients’ caregivers. In one recent study, however, there were no gender differences documented in pediatricians’ practices regarding providing guidance to parents about sexual risk reduction (Miller et al., 2008). Due to the lack of consistent evidence regarding gender differences in this area, we also advance the following two research questions: (1) Are there any gender differences in pediatricians’ attitudes, subjective norms, perceived behavioral control, behavioral intentions, and behavior toward encouraging parents to get their adolescent daughters vaccinated against HPV, and (2) are there any gender differences in the TRA’s or TPB’s ability to predict whether or not pediatricians encourage parents to get their adolescent daughters vaccinated against HPV?
METHOD1
Response Rate and Research Participants
Response rate
A database of more than 5,000 primary care physicians located in a Midwestern state included 1,307 physicians with a pediatrics specialty. All physicians with a pediatrics specialty were mailed a short survey focusing on the HPV vaccine. Response rate was calculated as the number of surveys returned divided by the number of surveys that were sent out and not returned as undeliverable (n = 136). In total, 406 pediatricians completed and returned this survey, for an overall response rate of 34.7%. This sample size compares favorably to those obtained in other recent health communication studies using a survey research method with physicians as research participants (M = 101, range = 46–152) (Roberto, Goodall, West, & Mahan, 2010; Bertakis & Azari, 2007; Kelly, Thompson, & Waters, 2006). This sample size also compares favorably to the nine TRA studies that used physicians as research patricians reviewed by Perkins et al. (2007). Specifically, though one of these studies (Millstein, 1996) had 786 research participants, the remaining eight included far fewer research participants (M = 122, range = 49–223).
Research participant characteristics
The participants (N = 406 pediatricians) were 50.6% male and 49.4% female, and the majority (84.4%) reported their race as European American. The remaining participants reported their race/ethnicity as Asian or Pacific Islander (9.8%), African American (3.0%), Hispanic (0.5%), and “other” (2.3%). The mean years as a practicing physician was 20.18 (SD = 10.02).
Instrumentation
Survey instructions
The survey defined “patients” as “girls between the ages of 9 and 17,” and pediatricians were instructed to “please think about just these patients and their parents when responding to the items on this survey” at multiple points throughout the survey. As noted previously, this age range was selected because the Advisory Committee on Immunization Practices (Markowitz et al., 2007), the American Cancer Society (Saslow et al., 2007), and the Centers for Disease Control and Prevention (2008) provide recommendations regarding the HPV vaccine for girls as young as age 9 years, and because we were interested in pediatricians’ communication with parents about the HPV vaccine.
Measures of TRA and TPB variables
All measures were developed using procedures outlined by Ajzen and Fishbein (1980) (see also Bergkvist & Rossiter, 2007). Behavior was measured by asking, “In the past 30 days, approximately how often have you encouraged the parents of your 9- to 17-year-old female patients to get their daughters vaccinated against HPV?” Response categories for this six-point item were, “0% of the time, 1–20% of the time, 21–40% of the time, 41–60% of the time, 61–80% of the time, and 81–100% of the time.” Behavioral intention was assessed by asking, “In the next 30 days, I intend to regularly encourage the parents of my 9- to 17-year-old female patients to get their daughters vaccinated against HPV.” Subjective norms was assessed by asking, “Most people who are important to me think I should encourage the parents of my 9- to 17-year-old female patients to get their daughters vaccinated against HPV.” Perceived behavioral control was measured by asking, “It would be easy for me to encourage the parents of my patients to get their daughters vaccinated against HPV.” Response categories for the intention, subjective norms, and perceived behavioral control items ranged from “strongly disagree” to “strongly agree” on a seven-point scale. Finally, attitude was measured by asking, “My attitude toward encouraging the parents of my 9- to 17-year-old female patients to get their daughters vaccinated against HPV is:” Response categories ranged from “very unfavorable” to “very favorable” on a seven-point scale.
Demographic and other variables
Because we were interested in pediatricians’ communication with parents about the HPV vaccine, the first item on the survey asked, “Approximately what percent of your patients are girls between the ages of 9 and 17 years old?” This question was followed by a blank in which pediatricians could write their response. The survey also contained measures of gender, race/ethnicity, and years of practice. In a previous study with physicians, Roberto et al. (in press) found a very strong correlation between age and years of practice, r (149) = .88, p < .001. Thus, this survey included the less sensitive years of practice question rather than the more sensitive age question in an effort to maximize the response rate (Dillman, Smyth, & Christian, 2009).
Procedures
Data collection was guided by the tailored design method (Dillman et al., 2009). Specifically, each pediatrician was contacted up to four times in an effort to get a survey returned (though once a pediatrician returned the survey, he or she was removed from the mailing list and did not receive subsequent mailings). The initial contact consisted of a personal postcard that informed the pediatrician to expect the survey within the next few days. The second contact included a consent form, survey, and business-reply envelope so pediatricians could return the survey at no cost to them. Approximately two weeks later, reminder/thank you postcards were sent to all pediatricians who had not yet returned the survey, informing them that a replacement survey would be sent in about a week in case they misplaced the original survey. Approximately one week later, a second copy of the consent form, survey, and business-reply envelope were sent.
To ensure that there was no systematic bias in responses due to order effects, two different versions of the survey were randomly distributed to pediatricians. All versions of the survey contained the same questions, but the order of the attitude, subjective norms, behavioral intention, and behavior differed on the two versions of the survey to minimize the possibility of order effects.
RESULTS
Preliminary Analysis and Descriptive Statistics
Since the focus of this study was pediatricians’ communication about the HPV vaccine with parents who have daughters between the ages of 9 and 17 years, the survey included a question to determine what percentage of participating pediatricians’ patients met this criteria. Pediatricians reported that a mean of 22.59% (SD = 12.37) of their patients were girls between the ages of 9 and 17 years. As a reminder, pediatricians were asked to consider just these patients and their parents when answering questions at multiple points throughout the survey.
Next, since the order in which the attitude, subjective norms, perceived behavioral control, behavioral intention, and behavior items were asked was different on the two versions of the survey that were distributed to pediatricians, it was possible to test for order effects. Two-tailed t-tests were conducted to see whether there were any order effects on any of the variables under investigation. The only significant difference between the two versions of the survey was for perceived behavioral control, t (403) = −2.08, p = .04. No other differences were observed (all p values >.05). Our review of the survey revealed no obvious reasons for this difference, which most likely is due to the large sample size and number of tests conducted. Thus, no precautionary measures seemed warranted in this instance. Descriptive statistics for all variables are included in Table 1.
TABLE 1.
Mean (and Standard Deviation) Item Scores for All TRA Variables
| Variable | M (SD) |
|---|---|
| Attitude | 6.47 (1.07) |
| Subjective norms | 5.84 (1.38) |
| Perceived behavioral control | 5.97 (1.13) |
| Behavioral intentions | 6.42 (1.12) |
| Behavior | 5.48 (1.09) |
Note. All variables measured on 7-point scales, except behavior which was measured on a 6-point scale.
Theory of Reasoned Action
The theory of reasoned action proposes that attitudes and subjective norms are independently and positively related to behavior intention and that behavioral intention is positively related to behaviors. To test the model, the ordinary least-squares criterion was used to estimate the parameters, parameter size was examined, and the fit of the model was assessed using path analysis (Hunter & Gerbing, 1982). Parameter size is determined in the path model by performing a simple or a multiple regression of each endogenous variable onto its causal antecedents. If the obtained effect size is not substantial, then the path connecting the two is removed and the revised model is tested before examining overall model fit. Comparing the observed correlation to the predicted correlation for each unconstrained relationship tests model fit. The difference between the observed and the predicted correlations constitutes the error estimate. If all of the individual errors, as well as the aggregate error, are not substantial and fall within the realm of sampling error, then the data can be claimed to be consistent with the model.
As can be seen from the zero-order correlations in Table 2, there were significant and substantial positive relationships between intentions and behavior, attitudes and intentions, and subjective norms and intentions. To test the hypothesis regarding the overall fit of the TRA, these correlations were then used to compute the path coefficients in the hypothesized TRA path model. All three predicted paths were of sufficient size and achieved standard levels of statistical significance (Figure 1). The path coefficient between attitude and behavioral intention was substantial, β = .50, P (.42 ≤ β ≤ .58) = .95. The coefficient between social norms and behavioral intention was not as large as that between attitude and behavior intention, but it was still substantial and statistically significant, β = .34, P (.26 ≤ β ≤ .42) = .95. Also, the coefficient between behavioral intentions and behaviors was large and significant, r = .70, P (.64 ≤ ρ ≤ .76) = .95. Given this analysis no path warranted removal. Because the attitude-intention and subjective norms-intention confidence intervals do not overlap, however, it appears that attitudes emerged as a stronger predictor of intentions in this instance.
TABLE 2.
Zero-Order Correlations Between All Theory of Reasoned Action and Theory of Planned Behavior Variables
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| (1) Attitude | ||||
| (2) Subjective norms | .48 | |||
| (3) Perceived behavioral control | .34 | .31 | ||
| (4) Behavioral intention | .66 | .58 | .37 | |
| (5) Behavior | .53 | .39 | .28 | .70 |
Note. All correlations are significant at p < .01 (N = 390).
Next, we tested the extent to which the data fit the model by comparing the observed to the predicted correlations. There are only two unconstrained relationships in this model, that between attitudes and behaviors and that between social norms and behaviors. Errors between the observed and the predicted correlations were very small (errors = .07 and −.02) and did not exceed what would be expected from sampling error alone. Moreover, the overall test of model fit showed that the errors as a whole did not exceed expectations due to sampling error, χ2 (2, N = 390) = 1.53, p = .47. From these data we concluded that the data were consistent with the model and that the theory of reasoned action is an acceptable model for explaining pediatricians’ decisions to encourage parents to get their daughters vaccinated against HPV.
The Theory of Planned Behavior
The TRA and the TPB share all of the same variables with only the addition of perceived behavioral control in the TPB. The inclusion of perceived behavioral control in the model brings with it two additional paths: one from perceived behavioral control to behavioral intent and another from perceived behavioral control to behavior. Both paths are predicted to be positive such that perceived behavioral control should increase both behavioral intent and behavior. Results indicate significant and substantial positive relationships between intentions and behavior, attitudes and intentions, subjective norms and intentions, perceived behavioral control and intentions, and perceived behavioral control and behavior (see Table 2).
To test the overall fit of the TPB, the correlations from Table 2 were used to compute the path coefficients in the hypothesized TPB path model. All of the TPB predictions that overlapped with the TRA were again supported. The path coefficient between attitude and behavioral intention, β = .47, P (.39 ≤ β ≤ .55) = .95, the coefficient between social norms and behavioral intention, β = .32, P (.24 ≤ β ≤ .40) = .95, and the coefficient between behavioral intentions and behaviors, r = .69, P (.63 ≤ ρ ≤ .75) = .95, were each substantial and did not include zero within their confidence intervals. The addition of perceived behavioral control did not change the overall fit of the model. Put differently: As was the case with the TRA, the overall model fit test suggested that the data were consistent with the TPB, χ2(2, N = 390) = 1.46, p = .48. That finding, however, seems to be largely due to the influence of the core TRA variables as perceived behavioral control did not have a substantial effect on either behavioral intent, β = .11, P (.01 ≤ β ≤ .21) = .95 or behavior, β = .02, P (−.08 ≤ β ≤ .12) = .95. These findings suggest the removal of the direct path between perceived behavioral control and behavior. Moreover, although the effect of perceived behavioral control on intentions was statistically significant, it still adds only slightly to the overall predictive power of the model. A stepwise regression that regressed intentions on, in the first step, the core TRA variables and, in the second step, perceived behavioral control showed a small but significant increase in the predictive power of the model including perceived behavioral control, R2change = .008, p = .02. This significant effect, however, is much more an artifact of the large sample size than of effect size.
Gender Differences
The first research question asked whether there were any gender differences on any of the TRA or TPB variables. To answer this question we conducted a series of two-tailed independent-sample t-tests to compare male and female pediatricians on each of the variables under investigation. Results indicate that male and female pediatricians did not differ on attitudes (male M = 6.44, female M = 6.51), t(391) = .63, p = .53; subjective norms (male M = 5.93, female M = 5.74), t(369) = −1.29, p = .20; perceived behavioral control (male M = 5.97, female M = 6.01), t(369) = −.36, p = .72; behavioral intentions (male M = 6.42, female M = 6.42), t(388) = −.01, p = .99; or behavior (male M = 5.42, female M = 5.55), t(389) = 1.18, p = .24.
The second research question asked whether there were any gender differences in the TRA’s or the TPB’s ability to predict whether or not pediatricians encourage parents to get their adolescent daughter vaccinated against HPV. To investigate this question we split the data set by sex, computed the correlations between the TRA variables, and examined the fit of the models for both males and females as described earlier. The effect sizes for all paths in both the TRA and the TPB split by sex fell within sampling error of one another and both tests of model fit were parallel. Therefore, we conclude that predicting pediatrician behavior to encourage parents to get their daughters vaccinated against HPV is not affected by the physician’s sex.
DISCUSSION
According to the TRA, an individual’s behavior is best predicted by his or her behavioral intentions, and these intentions are best predicted by both attitudes and subjective norms. The TPB extends the TRA by adding direct links between perceived behavioral control and both intentions and behavior. The primary purpose of this study was to determine if the TRA and TPB accurately predicted whether or not pediatricians encouraged parents to get their 9- to 17-year-old daughters vaccinated against HPV. Thus, a survey measuring attitudes, subjective norms, perceived behavioral control, behavioral intentions, and behavior was mailed to 1,307 pediatricians, and 406 (34.7%) of these pediatricians completed and returned this survey. On average, pediatricians indicated that they regularly encouraged parents to get their daughters vaccinated against HPV in the past 30 days, that they intended to continue doing so in the next 30 days, and that their attitudes, subjective norms, and perceived behavioral control toward this behavior were generally high. Further, path analysis results indicate that the data fit the TRA and TPB models for this target audience and behavior, though the TPB did not add substantially to the explanatory power on pediatrician behavior. Finally, there were no gender differences in the overall fit of the TRA or TPB, or for any of the individual variables in these models.
Few health communication scholars or practitioners would disagree with the premise that interventions should be theory based. Unfortunately, “little is known about the factors that influence [pediatricians’] cervical cancer prevention counseling” (Sussman et al., 2007, p. 298). Thus, one very important and unique outcome of the present investigation is that it provides a broader context of factors that influence pediatricians’ recommendations about HPV prevention by demonstrating the applicability of the TRA and TPB in this area. Since pediatricians’ recommendations influence the types of preventive care parents will allow their children to receive, they will play a particularly important role in the success of HPV and cervical cancer prevention programs (Sussman et al, 2007). The current investigation provides some important information that will be useful for those interested in developing health communication interventions and community-based interventions focused on cervical cancer prevention.
When used to explain behaviors that are not fully volitional, the TPB is expected to perform better than the TRA. For behaviors that are fully volitional, Ajzen (1985) predicts there should be little difference between the TRA and TPB. Thus, since whether or not a pediatrician communicates with parents is largely within their control, it is not surprising there was little difference between the two models in this instance. These results suggest that interventions targeting pediatricians would be effective if organized along the constructs of the TRA. For example, an intervention might attempt to change negative or neutral attitudes to be more positive, or attempt to reinforce already existing positive attitudes toward encouraging parents to get their daughters vaccinated against HPV. Similarly, Duval et al. (2006) identify at least three important normative referent groups for physicians with regard to the HPV vaccine: their colleagues, parents, and adolescents. Thus, changing negative or neutral subjective norms or reinforcing existing positive subjective norms for one or more of these groups might also prove to be an effective strategy. However, if resources are limited, intervention designers would be well advised to focus more on attitudes, which emerged as a somewhat stronger predictor of behavioral intention in this study: a finding that is consistent with two previous meta-analyses on the TRA (Albarracin et al., 2001; Downs & Hausenblas, 2005).
To illustrate the potential impact of a large-scale health communication intervention design to get pediatricians to encourage parents to get their daughters vaccinated against HPV, consider the following. There are more than 55,000 board certified pediatricians in the United States (Smart, 2007). Previous research indicates that the typical pediatrician sees approximately 120 patients per week (Weeks & Wallice, 2003)—or approximately 6,000 patients per year. From our data, we estimate that approximately 22% (or 1,300) of these patients are girls between the ages of 9 and 17 years. Thus, even a small (5%) increase in behavior would mean that the average pediatrician is encouraging 66 more parents per year to get their 9- to 17-year-old daughters vaccinated against HPV, which translates to more than 3.5 million more recommendations per year in the United States. In other words, and as Synder et al. (2004) note, even “small percentage changes may affect very large numbers of people in a community, state, or national campaign” (p. 89). And, as the preceding example illustrates, these changes would be magnified considerably when targeting pediatricians (each of whom sees a large number of patients), rather than individual parents or patients.
Before moving to a discussion of the strengths and limitations of this study, several possible directions for future research are worth noting. First, further research can attempt to extend the applicability of the TRA and TPB to other physician samples (i.e., those with a family practice specialty, or even to primary care physicians in general). Second, and on a related note, this study focused on communication with parents of 9- to 17-year-old girls. However, given that the vaccine is approved and recommended for women up to 26 years old, studies regarding physician communication with women between the ages of 18 and 26 years also seem warranted. Third, since the HPV vaccine has now been approved for males, it will be important to see whether these results generalize to this target audience as well. Finally, once interventions targeting pediatricians or other primary care physicians are developed and implemented, they will need to be evaluated. And as noted previously, results of this study provide a nice theoretical model to guide such evaluation efforts.
Strengths and Limitations
This investigation benefits from at least three key strengths. First, it is theory-based and extends the scope of the TRA and TPB to a topic (i.e., the HPV vaccine) and target audience (i.e. pediatricians) that have not previously been studied using these theories. This is particularly important given the atheoretical nature of most physician-related HPV studies that have been published to date (e.g., Daley et al., 2006; Duval, 2007; Keating et al., 2008; Sussman et al., 2007). Second, the rigor associated with our data collection procedures and statistical analyses provides a high level of confidence in the results. For example, our survey was designed using procedures outlined by Ajzen and Fishbein (1980), and data were collected using the Dillman et al. (2009) tailored design method. Further, path analysis was conducted using procedures outlined by Hunter and Gerbing (1982), and with a sample size that is adequate for this type of analysis. Third, and on a related note, the number of participants is relatively large, especially given that pediatricians’ communicative behavior was being studied. Finally, these results have important practical implications. HPV is the most common STI and has severe consequences for both men and women. While our results are generalizable to other pediatricians, it seems reasonable to assume they might also be applicable to other types of primary care physicians, other STIs, and perhaps even to other vaccine preventable diseases as well.
Some potential limitations must also be noted. A first limitation is that single-item measures were used. To help minimize this concern, the attitude, subjective norms, intention, and behavior items were based on verbiage suggested by Ajzen and Fishbein (1980). Further, a recent study by Bergkvist and Rossiter (2007) explicitly compared single-item and multiple-item attitude measures and found no differences in terms of their predictive validity. However, even with this in mind, single-item and self-report measures represent an important limitation to this study. Thus, it is important to acknowledge the need for future research using multiple-item measures and where the self-report measure of behavior is corroborated using a more objective measure (e.g., patient records, patient interviews, etc.).
A second potential limitation concerns the response rate, and the possibility that there is a self-selection bias with our sample (i.e., it is possible that pediatricians who were less likely to engage in the target behavior were also less likely to respond to our survey). While sampling issues such as this are very important when studying individual variables or trying to make population inferences, they are less important when studying multivariate relationships or trying to make process inferences (Basal, 1996; Hayes, 2005), and the current investigation looked at multivariate relationships in an effort to make process inferences about the TRA and TPB. Fortunately, we were aware of these potential issues before the study began, and we were able develop a survey and obtain a high-quality sample that was large enough to lead to a data set from which meaningful results could still be drawn.
A third limitation is that both the behavioral intention and behavior items were measured on the same survey. To put this in terms used by other TRA researchers, we assessed behavior retrospectively in this study, and are therefore “postdicting” past behavior (as opposed to measuring behavior prospectively and predicting future behavior). However, this is a common and accepted practice in TRA research in general, and especially for TRA studies using physicians as research participants. To illustrate, Albarracin et al. (2001) conducted a meta-analysis of 40 TRA and TPB studies. They found that 43% measured behavior prospectively (i.e., they measured behavioral intentions at one point in time and behavior at a later point in time), another 23% measured behavior retrospectively (i.e., they measured both behavioral intentions and behavior on the same survey, as we did in the current investigation), and 35% did not measure behavior at all (i.e., they simply measured attitudes, subjective norms, and behavioral intentions). The Perkins et al. (2007) review of nine physician TRA studies revealed a similar pattern. However, now that there is evidence that the TRA and TPB are relevant to this topic and target audience, future research is needed to test these theories with prospective behavior measures.
Practically, however, this decision does have one important implication. Specifically, the Albarracin et al. (2001) meta-analysis compared TRA and TPB studies that measured behavior both prospectively and retrospectively, and found that studies had somewhat larger intention–behavior associations when behavior was assessed retrospectively (i.e., .57) rather than prospectively (i.e., .45). Since we assessed behavior retrospectively in this study, it is likely that the .70 correlation between intentions and behavior would be attenuated somewhat had we measured it prospectively. To illustrate, given the 20% reduction between behavioral intention and prospective and retrospective measures of behavior found in the Albarracin et al. (2001) meta-analysis, the observed .70 correlation between intention and behavior in this study would likely have been reduced to .55 had we included a prospective measure of behavior. However, a correlation of this size still represents a significant and substantial relationship between intentions and behavior.
A final limitation is that this study did not include measures of the predictors of attitudes (i.e., behavioral beliefs and outcome evaluations), subjective norms (i.e., normative beliefs and motivation to comply), or perceived behavioral control (i.e., self-efficacy and controllability). While this is not uncommon in TRA and TPB research, the primary motivation for not measuring these variables in this instance was practical (i.e., to keep the survey short in order to increase the response rate). However, understanding the factors that underlie these three variables would provide valuable information for both theoretical and practical reasons. Therefore, future research might investigate these variables in general, and in the context of the TRA and TPB in particular.
In conclusion, most sexually active individuals will contract HPV at some point in their lives, and HPV can have very severe and even deadly consequences. One promising strategy for increasing vaccine awareness and acceptance rates is to develop interventions targeting pediatricians and other health care providers involved in the vaccination process (Daley et al., 2006; Sussmen et al., 2007). Our results suggest that developing theory-based interventions using the TRA or TPB should be effective when targeting pediatricians to encourage parents of female adolescents to get their daughters vaccinated against HPV. Future studies designed to change physician behavior focused on the HPV vaccine can build upon these findings in attempt to reduce cervical cancer disparities. Thus, results from this study have clear and important theoretical and practical implications for increasing the quality and quantity of life for a significant portion of society.
Footnotes
The data in this study are part of a larger study designed to describe and provide a better understanding of pediatrician communication with parents about the HPV vaccine. In order to reduce complexity and provide a more focused report, we present just the analyses testing the theory of reasoned action and theory of planned behavior in this article. Studies testing other theoretical perspectives will also be developed.
Contributor Information
Anthony J. Roberto, Hugh Downs School of Human Communication, Arizona State University
Janice L. Krieger, School of Communication, Ohio State University
Mira L. Katz, College of Public Health, Ohio State University
Ryan Goei, Department of Communication, University of Minnesota, Duluth.
Parul Jain, School of Communication, The Ohio State University.
References
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action control: From cognition to behavior. Berlin: Springer-Verlag; 1985. pp. 11–39. [Google Scholar]
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basil MD. The use of student samples in communication research. Journal of Broadcasting and Electronic Media. 1996;40:431–440. [Google Scholar]
- Bergkvist L, Rossiter JR. The predictive validity of multiple-item versus single-item measures of the same construct. Journal of Marketing Research. 2007;XLIV:175–184. [Google Scholar]
- Bertakis KD, Azari R. Determinants of physician discussion regarding tobacco and alcohol abuse. Journal of Health Communication. 2007;12:513–525. doi: 10.1080/10810730701508187. [DOI] [PubMed] [Google Scholar]
- Burd ID, Nevadunsky N, Bachmann G. Impact of physician gender on sexual history taking in a multispecialty practice. Journal of Sexual Medicine. 2006;3:194–200. doi: 10.1111/j.1743-6109.2005.00168.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HPV vaccine information for clinicians. 2008 Retrieved from http://www.cdc.gov/STD/HPV/STDFact-HPV-vaccine-hcp.htm.
- Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Kempe A, Babbel C. A national survey of pediatrician knowledge and attitudes regarding human papillomavirus vaccination. Pediatrics. 2006;118:2280–2289. doi: 10.1542/peds.2006-1946. [DOI] [PubMed] [Google Scholar]
- Dillman DA, Smyth JD, Christian LM. Internet, mail, and mixed-mode surveys: The tailored design method. 3. New York: Wiley; 2009. [Google Scholar]
- Dinh T, Sternberg M, Dunne EF, Markowitz L. Genital warts among 18- to 59-year-olds in the United States, National Health and Nutrition Examination Survey, 1999–2004. Sexually Transmitted Diseases. 2008;35:357–360. doi: 10.1097/OLQ.0b013e3181632d61. [DOI] [PubMed] [Google Scholar]
- Downs DS, Hausenblas HA. The theories of reasoned action and planned behavior applied to exercise: A meta-analytic update. Journal of Physical Activity and Health. 2005;2:76–97. [Google Scholar]
- Duval B, Gilca V, McNeil S, Dobson S, Money D, Ouakki M. Vaccination against human papillomavirus: A baseline survey of Canadian clinicians’ knowledge, attitudes, and beliefs. Vaccine. 2006;25:7841–7847. doi: 10.1016/j.vaccine.2007.08.041. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Freeman HP, Wingrove BK. Excess cancer mortality: A marker for low access to health care in poor communities. Rockville, MD: National Cancer Institute, Center to Reduce Cancer Health Disparities; 2005. NIH pub. no. 05–5282. [Google Scholar]
- Hayes AF. Statistical methods for communication science. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. [Google Scholar]
- Hunter JE, Gerbing DW. Unidimensional measurement, second order factor analysis, and causal models. In: Staw BB, Cummings LL, editors. Research in organizational behavior. 4. Greenwich, CT: JAI Press; 1982. pp. 267–320. [Google Scholar]
- Jansen KU, Shaw AR. Human papillomavirus vaccines and prevention of cervical cancer. Annual Review of Medicine. 2004;55:319–331. doi: 10.1146/annurev.med.55.091902.103520. [DOI] [PubMed] [Google Scholar]
- Kahn JA, Rosenthal SL, Tissot AM, Bernstein DI, Wetzel C, Zimet GD. Factors influencing pediatricians’ intentions to recommend human papillomavirus vaccines. Ambulatory Pediatrics. 2007;5:367–373. doi: 10.1016/j.ambp.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Keating KM, Brewer NT, Gottlieb SL, Liddon N, Ludema C, Smith JS. Potential barriers to HPV vaccine provision among medical practices in an area with high rates of cervical cancer. Journal of Adolescent Health. 2008;43:S61–S67. doi: 10.1016/j.jadohealth.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Kelly KS, Thompson MF, Waters RD. Improving the way we die: A coorientation study assessing agreement/disagreement in the organization-public relationship of hospices and physicians. Journal of Health Communication. 2006;11:607–627. doi: 10.1080/10810730600830047. [DOI] [PubMed] [Google Scholar]
- Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H. Quadrivalent human papillomavirus vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly. 2007;56(early release):1–24. [PubMed] [Google Scholar]
- Miller KS, Wyckoff SC, Lin CY, Whitaker DJ, Sukalac T, Fowler MG. Pediatricians’ role and practices regarding provision of guidance about sexual risk reduction to parents. Journal of Primary Prevention. 2008;29:279–291. doi: 10.1007/s10935-008-0137-9. [DOI] [PubMed] [Google Scholar]
- Millstein SG. Utility of the theories of reasoned action and planned behavior for predicting physician behavior. A prospective analysis. Health Psychology. 1996;15:398–402. doi: 10.1037//0278-6133.15.5.398. [DOI] [PubMed] [Google Scholar]
- Pagliusi SR, Aguado MT. Efficacy and other milestones for human papillomavirus vaccine introduction. Vaccine. 2004;23:569–578. doi: 10.1016/j.vaccine.2004.07.046. [DOI] [PubMed] [Google Scholar]
- Parkin DM. The global health burden of infection-associated cancers in the year 2002. International Journal of Cancer. 2006;118:3030–3044. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- Perkins MB, Jensen PS, Jaccard J, Gollwitzer P, Oettingen G, Pappadopulos E. Applying theory-driven approaches to understanding and modifying clinicians’ behavior: What do we know? Psychiatric Services. 2007;58:342–348. doi: 10.1176/ps.2007.58.3.342. [DOI] [PubMed] [Google Scholar]
- Riedesel JM. Attitudes about human papillomavirus vaccine among family physicians. Journal of Pediatric and Adolescent Gynecology. 2005;18:391–398. doi: 10.1016/j.jpag.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Roberto AJ, Goodall CE, West P, Mahan JD. Persuading physicians to test their patients’ level of kidney functioning: The effects of framing and point of view. Health Communication. 2010;25:107–118. doi: 10.1080/10410230903544902. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA. Physician gender and patient-centered communication: A critical review of empirical research. Annual Review of Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- Saslow D, Castle PE, Cox T, Davey DD, Einstein MH. American Cancer Society guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and its precursors. CA: A Cancer Journal for Clinicians. 2007;57:7–28. doi: 10.3322/canjclin.57.1.7. [DOI] [PubMed] [Google Scholar]
- Smart DR. Physician characteristics and distribution in the US. Chicago: American Medical Association Press; 2007. [Google Scholar]
- Snyder LB, Hamilton MA, Mitchell EW, Kiwanuka-Tondo J, Proctor D. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. Journal of Health Communication. 2004;11:71–96. doi: 10.1080/10810730490271548. [DOI] [PubMed] [Google Scholar]
- Sussman AL, Helitxzer D, Sanders M, Urquieta B, Salvador M, Ndiaye K. HPV and cervical cancer prevention counseling with younger adolescents: Implications for primary care. Annals of Family Medicine. 2007;5:298–304. doi: 10.1370/afm.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Montano DE, Koepsell T. Use of screening mammography by general internists. Cancer Detection and Prevention. 1994;18:455–462. [PubMed] [Google Scholar]
- Twombly R. U.S. girls to receive HPV vaccine but picture unclear on potential worldwide use, acceptance. Journal of the National Cancer Institute. 2006;15:1030–1032. doi: 10.1093/jnci/djj341. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. FDA licenses new vaccine for prevention of cervical cancer and other diseases in females caused by human papillomavirus. 2006 Retrieved from www.fda.gov/bbs/topics/NEWS/2006/NEW01385.html.
- Walker AE, Grimshaw JM, Armstrong EM. Salient beliefs and intentions to prescribe antibotics for patients with a sore throat. British Journal of Health Psychology. 2001;6:347–360. doi: 10.1348/135910701169250. [DOI] [PubMed] [Google Scholar]
- Weeks WB, Wallace AE. A retrospective evaluation of inputs, outputs, efficiency, and incomes of physicians. Archives of Internal Medicine. 2003;163:944–948. doi: 10.1001/archinte.163.8.944. [DOI] [PubMed] [Google Scholar]
- Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: Incidence and prevalence estimates, 2000. Perspectives on Sexual and Reproductive Health. 2000;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- Zimet GD. Improving adolescent health: Focus on HPV vaccine acceptance. Journal of Adolescent Health. 2005;37:S17–S23. doi: 10.1016/j.jadohealth.2005.09.010. [DOI] [PubMed] [Google Scholar]


