Abstract
Aims:
The aim was to study the trichoscopy features of selected hair and scalp conditions by two dermoscopic devices with different modes that is, polarized (noncontact) and nonpolarized (contact) mode.
Materials And Methods:
The present study included 11 clinical varieties of cases with total 112 patients, attending Sir Takhtasinh Hospital, Bhavnagar in the last 2 years. The clinical history was recorded for each case, and images were taken in both the Heine and DermLite II pro dermatoscope. We used polarized mode of the noncontact device (DermLite II) and the nonpolarized mode of the contact device (Heine) for our study.
Statistical Analysis Used:
Fisher's exact test to study dermoscopic observations for each mode.
Results:
We observed different nonscarring alopecia cases such as alopecia areata, androgenetic alopecia, trichotillomania, and tinea capitis. Scarring alopecia included discoid lupus erythematosus, lichen planopilaris, pseudopelade of Brocq, systemic lupus erythematosus. Scaling disorders included the psoriasis and seborrheic dermatitis. Furthermore, infestations like pediculosis capitis were included in the study. Various features were divided into follicular, interfollicular, pigmentary, vascular and hair shaft patterns. Each of the features was correlated in both the Heine (nonpolarized) and DermLite II (polarized) dermoscope, and observational finding was put forward accordingly.
Conclusions:
Various variations were observed in the documentation of dermoscopic patterns of the two dermatoscopes with certain features such as vascular patterns, scaling, and reticular pigmentation being better appreciated in polarized mode, while certain features were better documented in nonpolarized mode that is, black dots and tapered hair.
Keywords: Nonpolarized dermoscopy, polarized, trichoscopy
INTRODUCTION
Almost every other branch has some form of its own scopes. Why shouldn't we? Dermoscopy is a recent enlightening tool in the dermatological diagnostic field.
It is a diagnostic tool used to visualize deep epidermis and underlying structures also known as epilluminence microscopy. It was initially used in the evaluation of pigmentory dermatoses. Trichoscopy refers to the evaluation of hair and scalp disorders using a dermoscope. It was coined by Rudnicka and Olszewska in 2006.[1] Until now, most of the studies conducted till now have been using either polarized or the nonpolarized mode. Very few studies have used both the modes simultaneously for hair and scalp disorders.
MATERIALS AND METHODS
The study was conducted after prior approval by the Local Ethics Committee Institutional Review Board Bhavnagar. A total of 112 patients were selected from the out-patient department (OPD) in the Department of Dermatology. Patients having hair and scalp lesion were sorted and included in the study.
Instruments used
DermLite II dermoscope
It is a noncontact device used in the crosspolarized mode having 32 light emitting diode system. It is used with adjustable Sony handycam for magnifying as for storing images.
Heine dermoscope
It is the contact mode device used in the nonpolarized mode. It has a system of six light emitting diodes. It is attached Canon digital camera with adjustable photo SLR adaptor. Contact media used was alcoholic solution (70% ethanol).
Patient selection
We included patients having any hair and scalp lesions like inflammatory scalp lesions (psoriasis, lichen planus etc.), alopecia, hair shaft disorders and we excluded patients having highly infectious lesions, painful lesions in children and patient refusal for the examination.
Study design
It was a nonrandomized, single-arm observational study conducted from May 2012 to August 2013. Any patients attending the skin OPD or the ward having hair or scalp disorder were included. Clinical photographs along with normal naked eye inspection of the lesion were taken. A detailed clinical history and local examination along with clinical photographs were taken. Then the dermoscopic images of the same lesion in the nonpolarized mode were taken using Heine 20 Delta dermoscope, whereas the polarized mode images were taken using DermLite II. The dermoscopic features were confirmed by simultaneous documentation of the observation by two observers. Biopsies were performed only for cicatricial alopecia cases. The skin conditions were diagnosed according to clinical as well as dermoscopic pattern. A total analysis of the dermoscopic features and patterns were analyzed later.
The dermoscopic terms used in the study are broadly classified into six features namely.
Follicular epidermis, interfollicular epidermis, vascular patterns, pigmentory patterns, hair shaft changes (distorted, coiled, broken, vellus terminal, comma) and other patterns.
Statistical analysis
The various patterns were then studied later for individual diseases and also for frequencies within each disease to study their association. Since two modes of two dermoscopes were compared and as the sample value is less, the dermoscopic patterns were then compared using the Fisher's exact test and calculated using the Graph Pad software Inc, ( San Diego, California, USA).
RESULTS
A total of 112 cases was broadly subdivided in 11 disorders.
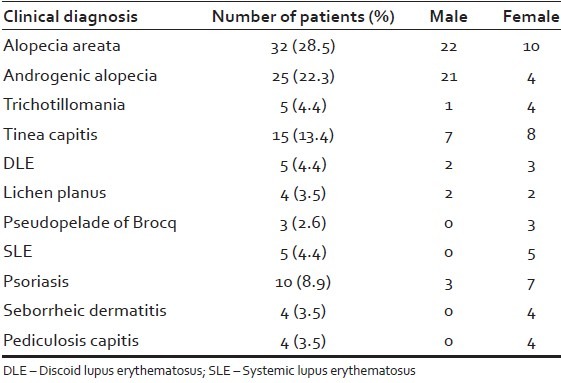
The demographic profile shows that the maximum number of patients documented in alopecia areata [Table 1].
Table 1.
Demographic profile
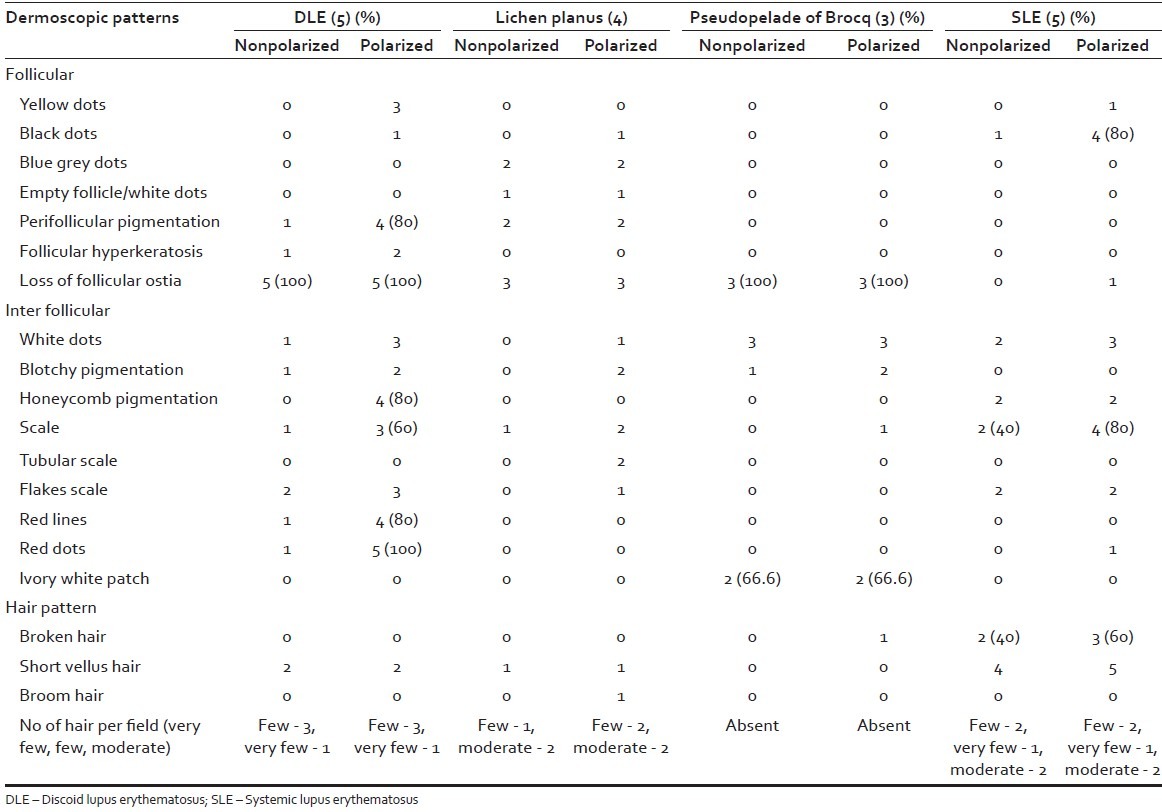
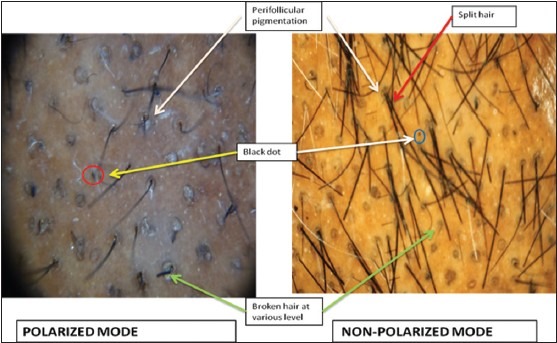
These disorders were classified for differentiation purpose broadly into nonscarring alopecia, scarring alopecia and scaling disorders [Tables 2–4].
Table 2.
Nonscarring alopecia (number of patients=77)
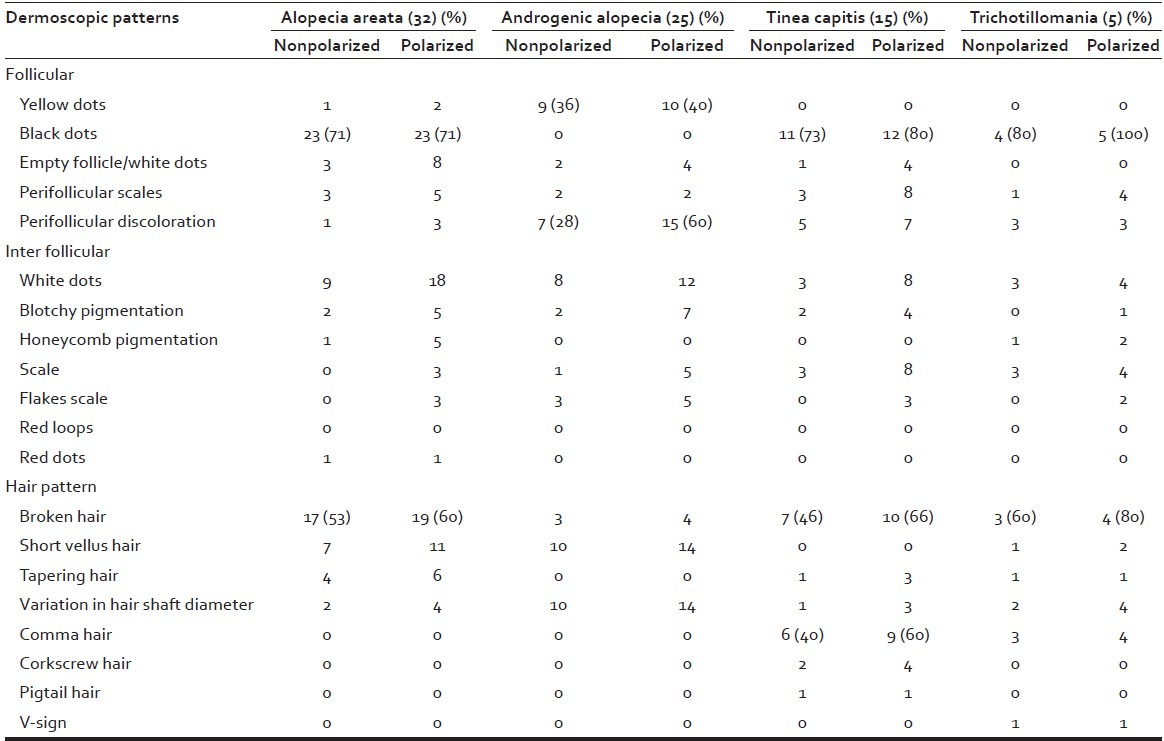
Table 4.
Scaling disorders (number of patients=18)
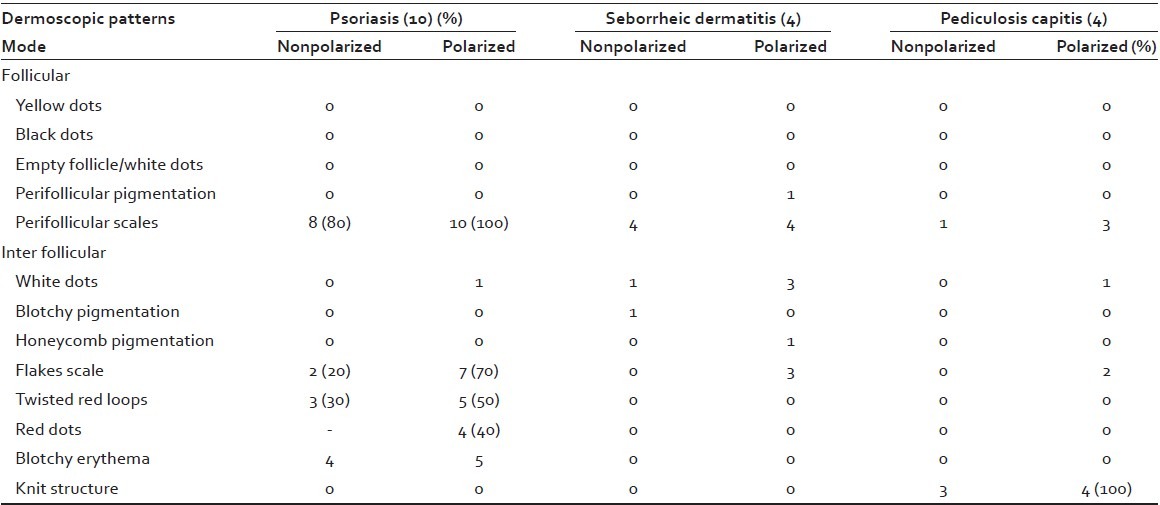
Table 3.
Scarring alopecia (number of patients=17)
The first statistical analysis table [Table 5] is a comparison of the two dermoscope that is nonpolarized and polarized mode and their finding for a particular pattern by observing the specificity, sensitivity, positive predictive value (PPV), likelihood ratio (LR) for each dermoscopic pattern.
Table 5.
Statistical analysis (nonpolarized mode)
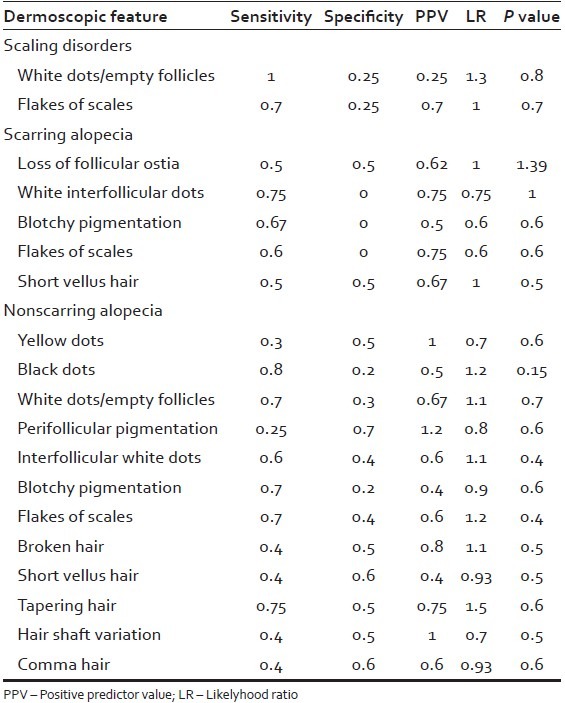
Since two dermoscopes were compared the one with the maximum findings that are polarized (noncontact) mode dermoscope was considered as the golden standard, and the comparison was carried out for the nonpolarized dermoscope.
Follicular features
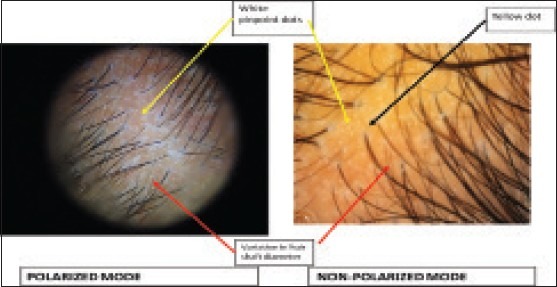
When we consider only follicular features we see that in nonscarring alopecia yellow dots were observed in patients of alopecia areata (6%) and androgenetic alopecia (40%) with a greater appreciation in the polarized mode. Other features like perifollicular scaling in tinea capitis, perifollicular discoloration in androgenetic alopecia were also better observed in polarized mode.
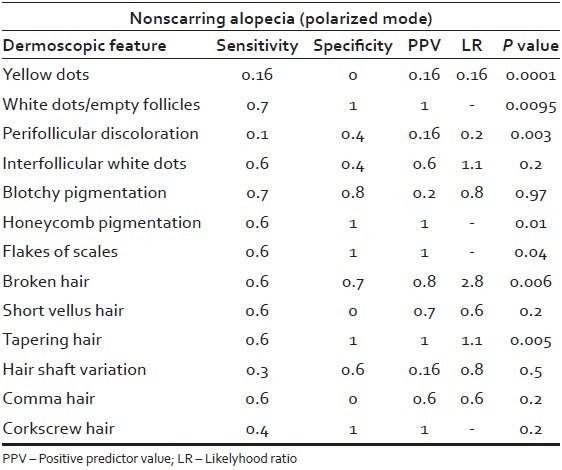
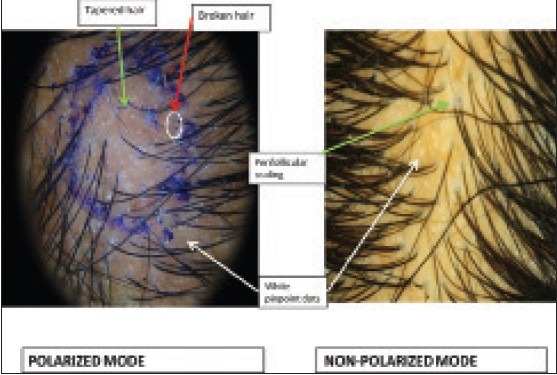
Black dots had greater sensitivity and diagnostic value (LR > 1) for the contact mode that is they were better appreciated in contact mode, but were not statistically correlated. They were seen in alopecia areata (71.8%), tinea capitis (73%) and trichotillomania (100%) patients.
When we consider scarring alopecia certain distinctive follicular features like lack of follicular ostia was present in most of the four conditions, a feature well-documented in polarized mode.
Interfollicular features
A very significant association was also appreciated for perifollicular pigmentation seen mostly in androgenetic alopecia (60%) and white pinpoint interfollicular dots in both alopecia areata (56%) and androgenetic alopecia (40%) patients.
White pinpoint dots (empty follicle), interfollicular white dots, flakes of scales, broken hair and tapering hair showed positive diagnostic correlation with the contact dermoscope with a likelihood ratio of >1.
While considering scarring alopecia many of the interfollicular features like blue grey dots, reticular pigmentation and tubular scaling of lichen planopilaris along with vascular patterns like red dots, red lines along with yellow dots resembling follicular keratosis in discoid lupus erythematosus (DLE) were all better seen in the polarized mode.
In scaling disorders the main diagnostic patterns are the flakes of interfollicular scales, vascular red dots and red loops both of which were better seen in the polarized mode. No significant hair shaft patterns were appreciated in these scaling disorders. As observed in scaling disorders the greatest sensitivity for the detection of white dots/empty follicle along with a likelihood ratio of >1.
None of the dermoscopic features of the contact (nonpolarized) mode showed any statistical significance when compared with the polarized mode.
Hair patterns
Considering hair patterns in nonscarring alopecia like broken hair in alopecia areata, tinea capitis and trichotillomania along with comma hair in tinea capitis were better visualized in the polarized mode. Hair shaft diameter variation, a diagnostic pattern of androgenetic alopecia was also better visualized in the polarized mode.
While we consider scarring alopecia into consideration broken hair, a variable feature seen in patients of systemic lupus erythematosus (SLE) and was better appreciated in polarized mode. Broom hair, an isolated finding in was seen in singe patient of lichen planopilaris.
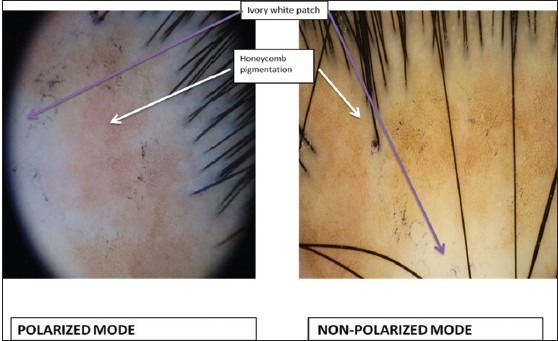
When just alone the polarized mode was evaluated [Table 6] we observed P value for nonscarring alopecia we observed statistically significant association for two patterns namely honeycomb pigmentation in alopecia areata and flakes of interfollicular scaling in tinea capitis.
Table 6.
Statistical analysis for polarized mode in nonscarring alopecia
An extremely high significant relationship was found for observation of yellow dots which were majorly seen in androgenetic alopecia.
A statistically very significant association was observed for tapered hair in alopecia areata and broken hair feature both alopecia areata and tinea capitis.
Honeycomb pigmentation, flakes of interfollicular scales, tapered hair and corkscrew hair all showed high specificity and PPV that is were diagnosed much specifically with the polarized dermoscope.
DISCUSSION
The spectrum of dermoscopy has received considerable interest in the last decade. Its use in hair and scalp disorders has been only used recently. Most conventional studies on dermoscopy in hair disorders have either been on contact and noncontact dermoscopy. In our study, we used both the modes for studying the 11 conditions. For the convenience, these conditions were broadly classified as nonscarring alopecia, scarring alopecia and scaling disorders.
Nonscarring alopecia
There were four conditions included in this category namely alopecia areata, androgenetic alopecia, trichotillomania and tinea capitis.
Follicular features
Yellow dots were the most conspicuous findings observed in patients of androgenetic alopecia and alopecia areata. They are considered a sensitive marker for alopecia areata. According to Tosti and Duque-Estrada yellow dots were specific findings for alopecia areata in 95% Europeans, 60% Asians and vary according to skin types.[2] We noticed yellow dots in only 6% patients of alopecia areata. When we talk about androgenetic alopecia, in different studies yellow dots were observed in 66%, 30.5%, 10% and 7% of cases.[3] We observed yellow dots in 40% of our androgenetic alopecia patients, thus corresponding to various studies. Other hallmark features for alopecia areata included tapered hair, black dots and broken hair [Figure 1] which can also be observed to a degree in trichotillomania and tinea capitis. Black dots were better observed in contact mode. Perifollicular and interfollicular scaling was characteristic finding in patients of tinea capitis than other nonscarring hair loss.
Figure 1.
Alopecia areata - Note that black dots and broken hair better visualized in non-polarized mode
Interfollicular features
Tapered hair (exclamation mark hair) were found to more degree in cases of alopecia areata and few in tinea capitis, also, they were better documented on polarized mode. Perifollicular discoloration (peripilar sign) was observed in patients of androgenetic alopecia, tinea capitis and trichotillomania. It represented perifollicular inflammation and was seen in more number in androgenetic alopecia[3] (15-20 hair/field) as compared to tinea capitis and trichotillomania.
Both the follicular and interfollicular features were better appreciated in the polarized mode.
Hair patterns
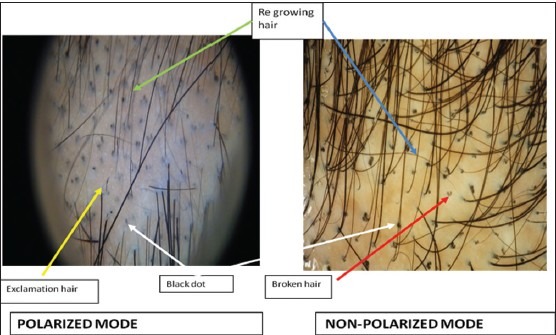
Broken hair were found to be numerous in alopecia areata and to a lesser extent in tinea capitis and trichotillomania. According to Tosti broken hair was the most specific finding in trichotillomania.[4] In our study too broken hair shaft at various level was the most conspicuous finding observed in trichotillomania [Figure 2]. It was detected equally well in both modes but more distinctly visualised in the nonpolarized mode.
Figure 2.
Trichotillomania - Note that broken hair and black dots better visualized in nonpolarized mode
Increased vellus hair (miniaturization) that is, reduction in length, pigmentation and diameter was seen in 40% of androgenetic alopecia patients [Figure 3]. According to Laccharreire et al. hair diameter was most accurate parameter for miniaturization.[3]
Figure 3.
Androgenetic alopecia - Note that hair shaft variation better visualized in polarized mode
Variation in hair shaft diameter was found to observed more specifically in cases of androgenetic alopecia although other conditions did show some degree of vellus hair.
In tinea capitis distinctive dermoscopic markers include black dots, broken hair and comma hair [Figure 4]. We observed these features in 80%, 66% and 60% patients respectively. Slowinska et al. reported comma hair to be a distinctive marker for tinea capitis, followed by broken and black dots (dystrophic hair).[5] Comma hair, corkscrew hair and pigtail hair[6] were all observed only in patients of tinea capitis, thus forming specific features. While comma hair was found equally well in polarized and nonpolarized mode, corkscrew hair and pigtail hair were better observed in nonpolarized mode.
Figure 4.
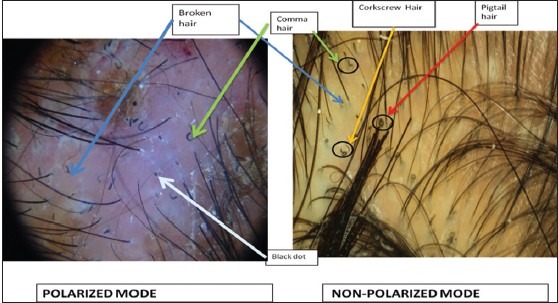
Tinea capitis - Note that the scaling is better seen in polarized mode while pigtail hair, corkscrew hair are visualized only in nonpolarized mode
In general for nonscarring alopecia, we observed that most distinctive features for each disorder were better visualized by the polarized mode than the nonpolarized mode.
Scarring alopecia
In his group four entities were studied namely DLE, lichen planopilaris, pseudopelade of Brocq and SLE.
Follicular features
White patch is corresponding to the absence of follicular ostia forms a hallmark for diagnosing alopecia of scarring origin.[4] All the conditions included in scarring alopecia had this feature. The diagnostic point of the patch of pseudopelade is classic ivory (snow) white color which was seen in all patients. In DLE the patch is whitish brown. The patch in lichen planopilaris and SLE are nonspecific and may vary according to the stages of the disease. These findings were better observed in polarized mode.
Interfollicular features
The dermoscopic distinctive clincher for DLE includes yellow dots, red dots and red lines.[7] According to Tosti et al. red dots and yellow dots are specific findings in DLE. Red dots were found in all patients in our study [Figure 5]. Red dots form a good prognostic indicator and indicate possible hair growth by Tosti et al.[8] The yellow dots observed in DLE are larger in size and represent follicular plugging. Both of these changes were better appreciated in polarized mode.
Figure 5.
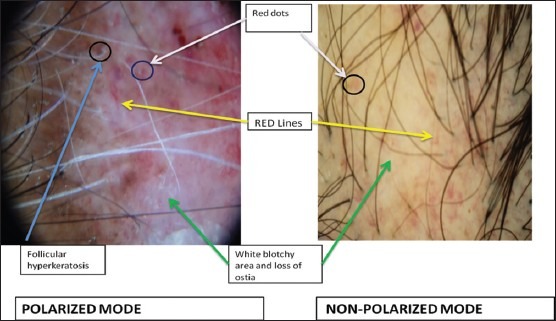
Discoid lupus erythematosus - Vascular structures like red dots and red loops are better appreciated in polarized mode
In lichen planopilaris [Figure 6] we observed violaceous white patch that is, loss of follicular ostia in majority of patients (3 out of 4). Blue grey dots were seen in 50% patients. Reticulated white pigment network could be appreciated better in noncontact mode. Bruna Duque Estrada et al. reported targetoid pattern of pigmentation in comparison to the haphazard pigmentation of DLE.[9] We feel that white pigment network may correspond clinically with Wickham's striae.
Figure 6.
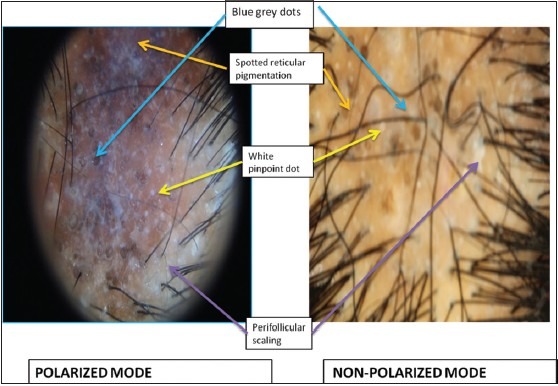
Lichen planopilaris - Note that blue grey dots and spotted reticular pigmentation are better seen in polarized mode
Another interesting finding in lichen planopilaris is tubular scaling which can helpful to differentiate it from DLE. The scales are entangling hair shaft up to 2-3 mm above scalp surface described as tubular scaling phenomenon. Thus, the noteworthy points to be seen in lichen planopilaris include blue grey dots, reticular white pigment network and tubular cast. None of the other scarring conditions included showed them. Furthermore, they were better appreciated in polarized mode.
Hair patterns
The number of hair is characteristically reduced in scarring alopecia and may range from total absent hair in pseudopelade of Brocq [Figure 7] to few hair loss in DLE, lichen planopilaris and SLE.
Figure 7.
Pseudopelade of Brocq - Dermoscopic features equally well documented in both modes
In our own observational finding, broken hair were found to be more observed in patients with SLE, which may correspond to lupus hair [Figure 8]. This finding was better documented in polarized mode.
Figure 8.
Systemic lupus erythematosus - Note that broken hair were better visualized in polarized mode
Scaling disorders
Regarding scaling disorders, the most important differential considered, were the psoriasis and seborrheic dermatitis.
The most distinctive clincher for dermoscopic feature of psoriasis includes presence of perifollicular scales and red loops.[4] Deeper vasculature structures are better visualized in the polarized light.[10] Although red loops were not observed in our study, red dot was observed in 50% of patients [Figure 9].
Figure 9.
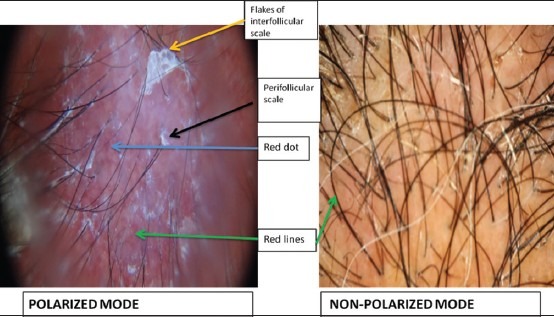
Psoriasis - Note the absence of scaling and less appreciation of vascular structures in nonpolarized mode
Seborrheic dermatitis on the other hand shows presence of whitish-yellow scales as a distinctive feature. Also, although arborizing vessels were not found in our study they form a good differentiating point from the red loops in psoriasis [Figure 10].
Figure 10.
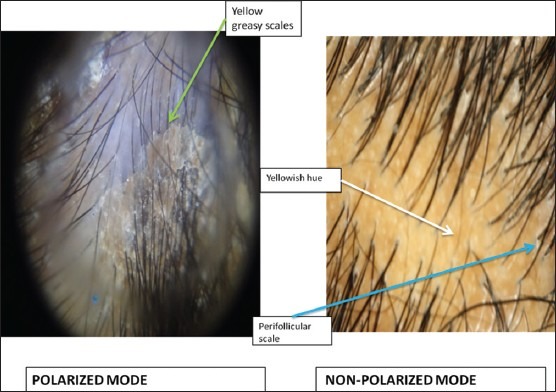
Seborrheic dermatitis - Note that greasy yellow scales better visualized in polarized mode
The knit structure in pediculosis capitis,[11] was also better documented in polarized mode [Figure 11].
Figure 11.
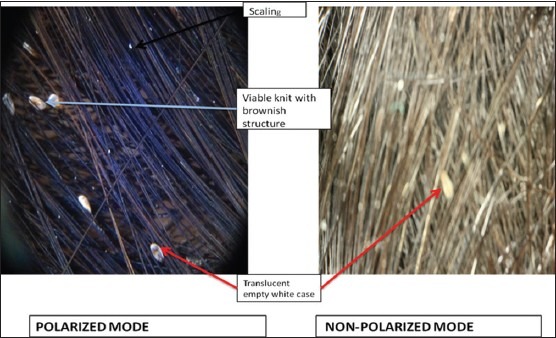
Pediculosis capitis - Knit structure is better visualized in polarized mode
Limitations observed in the study irregular sample size between disease groups and slight blurring of the nonpolarized (contact) images due to instability of the dermoscope, while taking image.
CONCLUSION
In our study, nonscarring and scaling disorders were better appreciated with the polarized mode. Certain features of scarring alopecia like red dots, reticular pigmentation were also better appreciated in polarized mode. We appreciated dermoscopic features like red dots, red lines; perifollicular scaling which are missed by nonpolarized mode can be diagnosed with certainty with polarized mode except black dots, broken hair which was much better appreciated by nonpolarized mode. Hence, we can conclude here with the saying that polarized mode holds a slight advantage over the nonpolarized mode in our study. Trichoscopy improves diagnostic accuracy and may contribute in understanding the pathogenesis of hair disorders. It thus may serve as an important diagnostic connecting tool between clinical diagnosis and histopathology.
Footnotes
Source of Support: Department of Dermatology, Venereology and Leprosy, Government Medical College, Bhavnagar
Conflict of Interest: None declared.
REFERENCES
- 1.Rudnicka L, Olszewska M, Majsterek M, Czuwara J, Slowinska M. Presence and future of dermoscopy. Expert Rev Dermatol. 2006;1:769. [Google Scholar]
- 2.Tosti A, Duque-Estrada B. Dermoscopy in hair and scalp disorders. J Egypt Women Dermatol Soc. 2010;7:1. [Google Scholar]
- 3.de Lacharrière O, Deloche C, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Hair diameter diversity: A clinical sign reflecting the follicle miniaturization. Arch Dermatol. 2001;137:641–6. [PubMed] [Google Scholar]
- 4.Tosti A. Atlas: Dermoscopy of hair and scalp disorders: Pathological and clinical correlations. Inform Healthc. 2008:43–7. [Google Scholar]
- 5.Slowinska M, Rudnicka L, Schwartz RA, Kowalska-Oledzka E, Rakowska A, Sicinska J, et al. Comma hairs: A dermatoscopic marker for tinea capitis: A rapid diagnostic method. J Am Acad Dermatol. 2008;59:S77–9. doi: 10.1016/j.jaad.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Rudnicka L, Rakowska A, Olszewska M, Slowinska M, Czuwara J, Rusek M, et al. Atlas of Trichoscopy. London: Springer-Verlag©; 2012. Hair shafts; p. 11. [Google Scholar]
- 7.Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5:82–8. doi: 10.3315/jdcr.2011.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tosti A, Torres F, Misciali C, Vincenzi C, Starace M, Miteva M, et al. Follicular red dots: A novel dermoscopic pattern observed in scalp discoid lupus erythematosus. Arch Dermatol. 2009;145:1406–9. doi: 10.1001/archdermatol.2009.277. [DOI] [PubMed] [Google Scholar]
- 9.Abraham LS, Piñeiro-Maceira J, Duque-Estrada B, Barcaui CB, Sodré CT. Pinpoint white dots in the scalp: Dermoscopic and histopathologic correlation. J Am Acad Dermatol. 2010;63:721–2. doi: 10.1016/j.jaad.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Pan Y, Gareau DS, Scope A, Rajadhyaksha M, Mullani NA, Marghoob AA. Polarized and nonpolarized dermoscopy: The explanation for the observed differences. Arch Dermatol. 2008;144:828–9. doi: 10.1001/archderm.144.6.828. [DOI] [PubMed] [Google Scholar]
- 11.Zalaudek I, Giacomel J, Cabo H, Di Stefani A, Ferrara G, Hofmann-Wellenhof R, et al. Entodermoscopy: A new tool for diagnosing skin infections and infestations. Dermatology. 2008;216:14–23. doi: 10.1159/000109353. [DOI] [PubMed] [Google Scholar]


