Abstract
Background This research compares the outcomes of percutaneous technique and open surgical peritoneal dialysis catheter placement in children.
Methods: In this randomized controlled trial, between 2010 and 2011,a total of 35 pediatric uremic patients were enrolled and randomized into two study groups. Follow up data included duration of operation (minute), duration of hospitalization (days) and onset time of peritoneal dialysis. Complications were considered as mechanical and infectious.
Results: The percutaneous procedure was significantly faster than the open surgical technique (9.5 ± 1.81 versus 27.00 ± 2.61 minutes, p= 0.0001). The onset of dialysis was earlier in percutaneous insertion. There were no cases of hollow viscous perforation, early peritonitis and exit site infection at the 3rd, 7th, and 14th day in both groups. Complications in open surgical group were include wrapped omentum in 4 (23.5%), catheter malposition in 3 (17.6%),delayed exit site infection in 2 (11.7%), Incisional hernia in 1 (5.8%)and hemoperitoneum in 2 (11.7%)cases. Complications in percutaneous insertion group were include catheter malposition and wrapped omentum each in one case.
Conclusion: Percutaneous method with secure insertion of the catheter reduced the rate of some complications. Although they were not statistically significant, this technique reduces the time of hospitalization and operation without need to general anesthesia. The onset of dialysis was earlier significantly. Trial registry code: IRCT2013091514670N1
Keywords: Surgical Procedures, Peritoneal dialysis, Catheters, Complications
Introduction
Ambulatory peritoneal dialysis is a simple and effective method for chronic renal replacement therapy in children (1,2). The advantage of this method includes simplicity, lower costs, patient independence and better patient satisfaction (3,4). Disadvantages include leak age, catheter related infections, hernia and mechanical out flow obstruction and catheter tip migration (2,5,6). Insertion procedures for peritoneal dialysis catheter (PDC) have shifted toward minimally invasive techniques, recently. Open technique is used more frequently which requires laparotomy (7-9).
Peritoneal dialysis catheters can be inserted percutaneously by a general surgeon to provide a simple, safe and fast peritoneal access. Beigi et al have showed that the implantation of the catheter by percutaneous technique was safe and easy and PDC was inserted with a low complication rate. This technique is performed successfully with local anesthesia and light sedation without any need for general anesthesia (10).
Therefore we hypothesized that percutaneous PDC insertion can provide the reliable and safe peritoneal access and may achieve the better outcome.
Methods
This randomized clinical trial study was performed in the department of pediatric nephrology and vascular surgery at Alzahra university hospital, Isfahan, Iran between 2010 and 2011. Informed consent was obtained from the parents of children taking part in our study. Ethical approval for this study was obtained from Isfahan University of Medical Sciences Research Ethics Committee prior to the launch of the study. This study is registered with the Iranian Registry of Clinical Trials, IRCT 2013091514670N1. A total of 35 pediatric uremic patients were enrolled in this study and randomized into two study groups by random allocation software.
Collected perioperative and follow up data of this study included age, Gender , body mass index (BMI ) history of hemodialysis, primary disease, creatinin (Cr), duration of operation (minute) and duration of hospitalization (day).
In our center, open placement of the PDC is the common procedure for most pediatric patients and general anesthesia is the preferred option. A left 3-4cm paramedian incision is made approximately 1-2cm superior to the umbilicus. A small opening is made in the fascia and peritoneum. Then using a stiff guide wire the tip of catheter is passed toward the pelvic cavity .The catheter is brought through a subcutaneous tunnel to the exit site in the left lower quadrant. Finally the fascia and the rectus sheet was repaired with vicryl and the skin was closed with nylon stiches.
For the percutaneous insertion, the patient was placed in the supine position. The abdomen was prepped and draped. Then under local anesthesia with lidocaine 2% up to 5 mg/kg installation and light sedation with intravenous injection of ketamine (0.5 mg/kg) and midazolam (1-2 mg/kg), 1 cm transverse incision was made on the skin, just below the umbilicus. Linea Alba was sutured by vicryl and pulled. Veress atraumatic laparoscopic needle was inserted in peritoneal cavity through linea Alba. Normal saline (10 cc/kg) was infused in the abdomen to create the artificial ascites. A guide wire was inserted through the needle and the needle was removed. A dilator with a sheet was inserted over the guide wire. Then the dilator and guide wire was removed and the PD catheter with rigid guide was advanced through the sheet and directed toward the pelvis. The rigid guide was withdrawn and then both parts of sheet were divided and removed. Then a subcutaneous tunnel was made 3-4 cm caudally to the left lower quadrant, thereafter in all cases, with plain radiography we ensured the pelvic positioning of the catheter.
PDC related complications included catheter out flow obstruction, leakage, hemoperitoneum, hollow viscous perforation, incisional site hernia, exit site infection and peritonitis.
Inclusion criteria included male and female patients below 15 years of age who will be receiving peritoneal dialysis and have family support. Patients will be excluded if there is a history of prior major abdominal surgery, ventral or inguinal hernia or BMI ≥35 kg/m2.
Eighteen PDCs were placed percutaneously (P group) and 17 were inserted surgically (S group). Outcomes were recorded for two months following the insertion of the catheters.
Statistical Analysis
All data were analyzed using statistical program SPSS Ver. 17. Fisher exact tests, student – t, Mann Whitney u test and Chi – square were used for analysis. P values less than 0.05 were considered as significant.
Results
Patient characteristics and clinical details are summarized in table 1. The total of 35 catheters was inserted successfully without any postoperative mortality. The percutaneous procedure was significantly faster than the open surgical technique (9.5 ±1.81 minutes versus 27.00 ±2.61, p= 0.0001). Complications of both percutaneous and surgical procedures included incisional hernia, leakage from insertion site, hollow viscous perforation, catheter malposition, Hemoperitoneum, exit site infection and out flow failure of catheter.
Table 1. Characteristics and clinical details of study population .
| Patients characteristic | Total (n=35) |
Percutaneous group (n=18) |
Surgical group (n=17) |
p |
| Male, n (%) | 21(60%) | 9(50%) | 12(70.5%) | 0.214 |
| Age (years) | 6.58 ±4.82 | 6.77 ±4.87 | 6.38 ±4.91 | 0.91 |
| BMI (kg/m2) | 15.85 ±1.25 | 16.8 ±1.31 | 14.8 ±1.33 | 0.32 |
| History of hemodialysis | 4(11.42%) | 3(16.66%) | 1(5.88%) | 0.316 |
| Plasma Cr (mg/dl) | 5.10 ±2.19 | 5.23 ±2.00 | 4.96 ±2.43 | 0.595 |
| Primary disease | ||||
| Congenital n (%) | 11(31.4) | 4(22.2 ) | 7(41.1) | 0.531 |
| Hydronephrosis n (%) | 2(5.7) | 1(5.5) | 1(5.8) | 0.781 |
| Reflux n (%) | 3(8.5) | 2(11.1) | 1(5.8) | 0.581 |
| Hypertension n (%) | 5(4.2) | 4(22.2) | 1(5.8) | 0.217 |
| Nephrotic syndrome n (%) | 4(11.4) | 3(16.6) | 1(5.8) | 0.316 |
| Others n (%) | 10(28.5) | 4(22.2) | 6(35.2) | 0.561 |
| Duration of operation (min) | 18.54±8.9 | 9.5 ±1.81 | 27.00 ±2.71 | 0.0001 |
| Onset of dialysis (day) | 6.4±1.9 | 3.1 ±1.1 | 10.2 ±2.1 | 0.0001 |
Incisional hernia was seen in one patient in open surgical group. The total of 2 cases (11.7%) in group S was complicated with hemoperitoneum. There were no cases of hollow viscous perforation, early peritonitis and exit site infection at the 3rd, 7th, 14th day in both groups.
Two cases (11.7%) in group S were complicated by exit site infection at the 30th and 60th day of follow up. (p= 0.296)
Catheter malposition was seen in 4 patients (3 (17.6%) in S group and 1 (5.5%) in P group). In our study, the total of 5 patients (14.2%) complicated by wrapped omentum and they needed omentectomy (4 (23.5%) in S group and 1 (5.5%) in P group. Onset of dialysis was 3rd and 10th day of insertion in P and S group respectively (p<0.0001). Outcomes of the two methods are summarized in Fig. 1.
Fig. 1 .
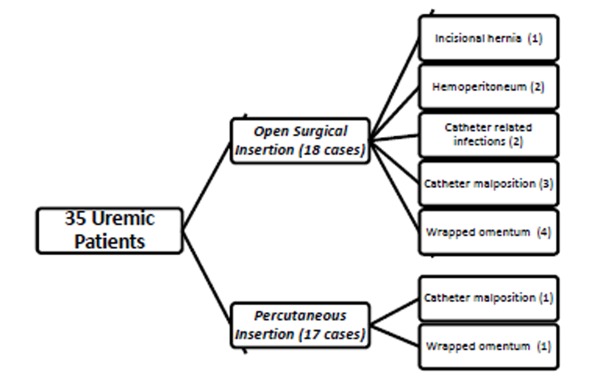
Comparison of the complications related to surgical and percutaneous techniques
Discussion
Beigi et al compared the outcomes of 34 percutaneous PD catheter placements in adults.
There was no incisional hernia and hollow viscous perforation. Duration of operation was significantly lower in percutaneous insertion technique than open surgical method.
Hemoperitoneum and out flow failure was more frequent in surgical insertion group.
Duration of hospitalization was same in both groups (approximately 3 days) .And in percutaneous group all PDCs were inserted without general anesthesia (10). In our series two cases (11.7%) were complicated by in incisional hernia in S group. In P group all catheters were placed with local anesthesia and light sedation. In addition, the duration of hospitalization was longer in surgical group. Also out flow failure was more frequent in S group significantly (p<0.0001).
Varughese et al suggested that the percutaneous technique is extremely simple and reduces the time of hospitalization. There was no fluid leakage from insertion site. And one patient complicated with hollow viscous injury (11). In this study the period of hospitalization was longer is S group, and there was no case of fluid leakage in percutaneous group.
Ozener et al reported that the rate of catheter related complications was the same in surgical and percutaneous techniques. This study suggested that there was statistically significant difference between open surgical and percutaneous procedure (12).
Tiong et al reported that, approximately one third of percutaneously inserted PD catheters complicated with wound infection and catheter out flow failure. Also Duration of procedure was prolonged (13,14). In our series the percutaneous technique is simple, fast and safe method with better out comes in comparison with surgical method.
Dwarakanathan et al showed that the onset of peritoneal dialysis with 7 days delay of open surgical insertion time is safe with low complications. In this randomized study the meantime of starting peritoneal dialysis was 10th day of catheter insertion in S group versus 3rd in P group (p<0.0001)
Conclusion
In summary the percutaneous method with secure insertion of the catheter reduced the rate of some complications. Although they were not statistically significant, this technique reduces the time of hospitalization and operation without need to general anesthesia.
Acknowledgments
The authors want to greatly thank vice chancellery of research of Isfahan University of Medical Science for excellent supports.
Cite this article as: Merrikhi A, Raji Asadabadi H, Beigi A.A, Marashi S.M, Ghaheri H, Nasiri Zarch Z. Comparison of percutaneous versus open surgical techniques for placement of peritoneal dialysis catheter in children: A randomized clinical trial. Med J Islam Repub Iran 2014 (1 June). Vol. 28:38
References
- 1.Mortazavi F, Maleki M. Management and outcome of children with end-stage renal disease in northwest Iran. Indian J Nephrol. 2012;22(2):94–7. doi: 10.4103/0971-4065.97113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jwo SC, Chen KS, Lin YY. Video –assisted laparoscopic procedures in peritoneal dialysis. Surg Endos. 2003;17(10):1666–70. doi: 10.1007/s00464-003-8106-0. [DOI] [PubMed] [Google Scholar]
- 3.Bullmaster JR, Miller SF, Finley RK, Jones LM. Surgical aspects of the Tenckhoff peritoneal dialysis catheter A 7 year experience. Am J surg. 1985;149(3):339–42. doi: 10.1016/s0002-9610(85)80103-3. [DOI] [PubMed] [Google Scholar]
- 4.Cronen PW, Moss JP, Simpson T, Rao M, Cowles L. Tenckhoff catheter placement: surgical aspects. Am surg. 1985;51(11):627–9. [PubMed] [Google Scholar]
- 5.Fleisher AG, Kimmelstiel FM, Lattes CG, Miller RE. Surgical complications of peritoneal dialysis catheters. Am J surg. 1985;149(6):726–9. doi: 10.1016/s0002-9610(85)80174-4. [DOI] [PubMed] [Google Scholar]
- 6.James LW, Kelly R. Acute abdominal emergencies in patients on long-term ambulatory peritoneal dialysis. Can J surg. 1993;36(6):522–4. [PubMed] [Google Scholar]
- 7.Blessing WD Jr, Ross JM, Kennedy CI, Richardson WS. Laparoscopic assisted peritoneal dialysis catheter placement, an improvement on the single trocar technique. Am Surg. 2005;71(12):1042–6. [PubMed] [Google Scholar]
- 8.Crabtree JH, Fishman A. Videolaparoscopic implantation of long-term peritoneal dialysis catheters. Surg Endosc. 1999;13(2):186–190. doi: 10.1007/s004649900936. [DOI] [PubMed] [Google Scholar]
- 9.Crabtee JH, Fishman A. A laparoscopic approach under local anesthesia for peritoneal dialysis access. Perit Dial Int. 2000;20(6):757–65. [PubMed] [Google Scholar]
- 10.Atapour A, Raji-Asadabadi H, Karimi S, Eslami A, Beigi AA. Comparing the outcomes of open surgical procedure and percutaneously peritoneal dialysis catheter (PDC) insertion using laparoscopic needle: A two month follow-up study. J Res Med Sci. 2011;16(4):463–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Varughese S, Sundaram M, Basu G, Tamilarasi V, John GT. Percutaneous continuous ambulatory peritoneal dialysis (CAPD) catheter insertion – a preferred option for developing countries. Trop Doct. 2010;40(2):104–5. doi: 10.1258/td.2010.090370. [DOI] [PubMed] [Google Scholar]
- 12.Ozener C, Bihorac A, Akoglu E. Technical survival of CAPD catheters: complication between percutaneous and conventional surgical placement techniques. Nephrol Dial transplant. 2001;16(9):1893–9. doi: 10.1093/ndt/16.9.1893. [DOI] [PubMed] [Google Scholar]
- 13.Mellotte GJ, Ho CA, Morgan SH, Bending MR, Eisinger AJ. Peritoneal dialysis catheter: a comparison between percutaneous and conventional surgical placement techniques. Nephrol Dial transplant. 1993;8(7):626–30. [PubMed] [Google Scholar]
- 14.Ranganathan D, Baer R, Fassett RG, Williams N, Han T. et al. Randomized controlled trial to determine the appropriate time to initiate peritoneal dialysis after insertion of catheter to minimize complications (Timely PD study) BMC Nephrol. 2010;11:11. doi: 10.1186/1471-2369-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


