Abstract
Objectives
To examine the impact of telephone reinforcement (TR) on predictors of physical activity (PA) maintenance in older adults with osteoarthritis.
Methods
Mixed effects modeling was conducted of data from a randomized PA trial that used negotiated maintenance contracts, supplemented by TR, to test impact of TR on barriers, decisional balance, and stage of change at multiple points in time.
Results
Participants who were referred to a PA program and received TR improved the most in barriers and decisional balance. Participants who negotiated a tailored maintenance contract but did not receive TR improved the most in stage.
Conclusions
TR appears to positively affect perceptions around engagement, whereas negotiation positively impacts PA behavior. Further research should examine the effectiveness of specific PA maintenance strategies.
Keywords: physical activity, older adults, transtheoretical model, stages of change
Osteoarthritis (OA) is the most prevalent type of arthritis and a leading cause of functional impairment among older adults in the US.1–4 An estimated 26.9 million adults have OA, including 12.4 million adults aged 65 and older.5,6 Approximately 44% of adults with doctor-diagnosed arthritis report no leisure-time physical activity (PA),7 and older adults are more likely to be inactive than middle-aged adults.8 This high rate of inactivity, coupled with the increase in the older adult population, underscores the need for programs that promote initiation, adherence, and maintenance of PA in persons with OA.
Promoting PA initiation and maintenance among older adults is challenging. PA programs often fail to recruit older adults who need exercise most, and those who do take part in programs tend to revert to sedentary behaviors after program completion.9 Studies frequently do not offer clear descriptions of how theoretical components are operationalized in interventions.10 Few studies specifically explain methods applied during interventions to improve PA participation.11 Most PA interventions have demonstrated reduced PA participation over time, indicating a critical need to develop effective strategies that foster long-term maintenance of PA.9–12 Telephone reinforcement (TR) for PA is usually conducted as a stand-alone intervention that is not part of a PA program, and comparatively few studies have examined the use of TR to bolster the effects of an earlier intervention. Three studies that have used TR as an adjunct to PA have found improvement in energy expenditure, blood pressure, heart rate, depressive symptoms, physical functioning, quality of life, and exercise participation.13–15 Together, these results indicate that TR may be an effective method for bolstering the effects of PA programs.
A systematic review (N=25 studies) of telephone-based interventions that targeted both PA and dietary behaviors of adults found that 52% of studies reported the number of calls received (dose), and 56% reported the average call length, but only 8% examined the impact of dose on outcomes.16 Although 48% of studies described interviewer training, few (12%) described programs that were tested for efficacy and disseminated to, and implemented in community settings. The current study contributes to this literature by reporting the impact of tapered TR over 16 months on 3 behavioral predictors of PA maintenance: barriers, decisional balance, and stage of change (SOC). Our unique study design enabled us to examine the main effects of follow-up assignment17 as well as additive effects of tapered TR.
To the best of our knowledge, this study is one of the first to describe strategies for promoting PA applied during TR among older adults with OA over 18 months. Messier et al18 conducted an 18-month clinical trial - the “Arthritis, Diet, and Activity Promotion Trial” (ADAPT), which examined the impact of exercise and diet among obese and overweight older adults with knee OA. They randomized participants into a dietary intervention, an exercise intervention, both exercise and diet, and healthy lifestyle control. Participants who entered maintenance in the dietary intervention participated in a meeting or call which occurred successively every 2 weeks. Participants who transitioned to exercising at home received calls every other week during the initial 2 months, every 3 weeks during the next 2 months, and once a month until the end of the study. The diet and exercise group received both programs. The control group received calls once a month during months 4–6, tapering during months 7–18 to every other month. However, behavioral strategies used during calls were not described. They found that the combination of diet and exercise benefited pain, functioning and mobility more than each intervention on its own.18 Findings also indicated that offering a choice of location for PA and promoting initial attendance boosts future attendance.19 Messier et al20,21 implemented a second 18-month clinical trial to assess how weight loss influences disease progression among obese and overweight older adults with knee OA - the “Intensive Diet and Exercise for Arthritis (IDEA) Trial.” Regular calls were also a part of this protocol for those exercising at home, but call content was not described in detail. They found that persons in the combined diet and exercise group and diet group had better OA outcomes than the exercise group.20,21
TR for PA is different for older adults with OA compared to other subgroups of older adults because discussions focus on OA management and how to engage in an active lifestyle, despite symptoms such as pain and stiffness that are associated with the condition.
Theoretical Framework
The 3 primary outcomes for this study were selected because they are key components of the Transtheoretical Model (TTM) which provided the theoretical framework for the study. TTM is a social-cognitive-based model developed by Prochaska et al22,23 to explain health behavior change as a process that progresses through stages, from pre-contemplation to action. Stage progression is determined by perception of barriers and decisional balance. The concept of decisional balance was developed by Janis and Mann20 as part of their decision-making model.25 Two decisional balance constructs, pros and cons of behavior change, were later incorporated into TTM.23,25 For the purpose of this paper, the pros and cons of behavior change will be referred to as decisional balance. Decisional balance is one of the processes of change in TTM,23 insofar as the balance between pros and cons of behavior change differs by stage.25 TR applies constructs from this framework to support behavior maintenance. TR strategies include assessing confidence and motivation, developing ways to overcome obstacles, and maximizing opportunities to engage in PA while reinforcing success and progress.
Barriers
Barriers to exercise adherence among older adults include poor health and symptoms, such as pain, as well as limited availability of parks, sidewalks, and fitness centers, unsafe neighbor -hood, lack of physician recommendation, minimal knowledge about the impact of PA on health, and PA experience.26 Stiggelbout et al27 examined factors associated with PA program maintenance among older adults. They found that non-smoking, married females who were employed and younger in age with high self-efficacy and positive attitudes about PA had high intent to continue to exercise. Those with little to no gaps in activity, positive perception of program quality, and high exercise intent, positive attitude about PA, and minimal risk situations at baseline predicted actual PA maintenance.
Decisional Balance
Although some studies have examined decisional balance for PA among older adults, none have focused on those with OA. A qualitative study by O’Brien Cousins28 found that active participants engaged in a similar amount of negative self-talk about PA as less active participants. However, active participants were more capable of balancing each problem with positive thinking based on successful experience with exercise and benefits received from engaging in exercise in the past.
Guillot et al29 evaluated decisional balance ratings among cardiac and pulmonary rehabilitation patients and found that both pros and cons increased as participants approached the end of rehabilitation. They postulated that cons increased because participants were trying to determine how to continue post-rehabilitation exercise and concluded that expectation of future barriers can have adverse influence on current ratings.
Stage of Change
Research indicates that SOC accurately detects exercise behavior change over time.30,31 Older adults in action and maintenance report significantly more moderate-to-vigorous PA behavior compared to those in lower stages. Active seniors also classify themselves at higher stages than less active older adults.31–35 Most studies demonstrate short-term benefits of stage-matched interventions, but results are not maintained over time.36 Thus, PA maintenance strategies require further development, and their application also must be examined. The current paper addresses this gap by examining the impact of TR as a booster to PA maintenance in a randomized trial.
METHODS
Participants
The study sample consisted of 486 community-dwelling older adults with lower extremity OA who were recruited to participate in the evidence-based Fit and Strong! program through targeted mailings, flyers, media announcements, and presentations at events for older adults. Eligible study participants were 60 years of age or older, did not participate in an aerobic exercise program regularly, had current OA symptoms, well-controlled or no diabetes, and a score of 7 or more correct items on the Short Portable Mental Status Questionnaire.37
Instruments: Outcome Measures
Participants in all 4 study groups were assessed on the following measures of behavioral change at baseline, 2, 6, 12, and 18 months.
Barriers to exercise
This 23-item measure asks participants to rate on a scale of 1 to 5, the degree to which each barrier made it difficult to exercise regularly in the past 6 months.38 A Cronbach’s α = .902 was found for this measure in this study sample.
Decisional balance
The 16-item Decisional Balance Inventory39,40 asks participants to rate how strongly they agree/disagree with positive and negative statements about exercise, using a Likert scale that ranges from 1 (strongly disagree) to 5 (strongly agree). A Cronbach’s α = .762 was found for this measure in this study sample.
Stage of change
The 5-item Marcus Exercise Stage of Change measure uses 3 response categories: Yes (1), No (2), and Not Applicable (3) to classify participants within one of 5 stages based on frequency of engagement in PA. This ordinal measure asks participants about level of exercise participation and classifies them into the mutually exclusive categories of precontemplation, contemplation, preparation, action or maintenance. This scale also displays good reliability, with a κ index of .78.31,35,41,42
Procedure
We conducted secondary data analyses of data from the “Maintenance of Exercise Adherence among Older Adults with Osteoarthritis” Trial funded by National Institute on Aging (Grant # R01 AG23424).17,43 The main effects of this trial have been reported previously and included PA maintenance (long-term PA participation) as a primary outcome.17 This follow-up study examined change over time in behavioral measures described above that are associated with PA maintenance.
All study participants participated in Fit and Strong! which meets 3 times per week for 8 weeks. Each program session includes 60 minutes of stretching/flexibility, low-impact aerobics, strengthening, and balance exercise, followed by 30 minutes of manual-based, group problem-solving/health education for managing OA with PA. Arthritis severity was determined by rheumatologist exams conducted during the first 2 weeks of the program. The American Rheumatism Association (ARA) Functional Class Classification was used to categorize arthritis-specific functioning into 4 levels of increasing severity.44–46
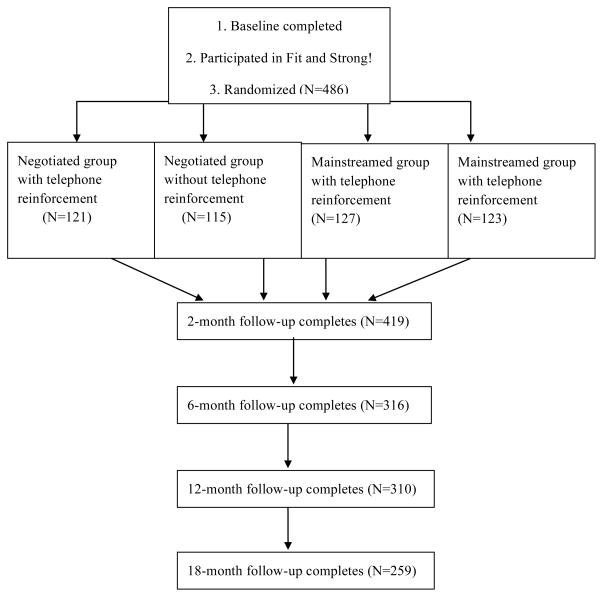
In week 6 of Fit and Strong!, participants met individually with their instructor to develop negotiated follow-up exercise maintenance plans for post-program PA maintenance. Because the impact of the negotiated contract was unknown, the main trial sought to answer that question by randomizing participants in week 6 to the customary negotiated contract follow-up condition or to a mainstreamed follow-up condition. Participants in the mainstreamed group were referred to an ongoing best-practice, multiple-component PA program held at the same facility as Fit and Strong!. Further, because the potential impact of TR as a booster to maintenance of PA in this group was also unknown, the 2 study groups were further divided randomly into persons who received TR after the program ended versus those who did not. Thus, during week 6, participants were randomized to: (1) negotiated follow-up maintenance plan with TR (N-TR); (2) negotiated follow-up without TR (N-noTR); (3) mainstreamed to an ongoing PA program with TR (M-TR); and (4) mainstreamed follow-up without TR (M-noTR) (Figure 1).
Figure 1.
Randomization and Measurement
TR was hypothesized to boost PA maintenance after the intervention ended.17 The application of TR strategies tailored to each stage was expected to promote movement to higher stages and bolster PA maintenance in both negotiated and mainstreamed group participants who received it. Both the negotiated follow-up contracts and mainstreaming participants to an ongoing, on-site PA class were expected to promote PA maintenance. However, the negotiated contract was expected to have stronger effects on maintenance than mainstreaming because negotiation enabled participants to develop individually tailored, customized maintenance plans.17
Participants who were randomized to receive TR completed regular phone interviews with study staff. The protocol specified making bi-weekly phone calls during months 3–6 after the completion of Fit and Strong!, followed by monthly calls during months 7–18.
Intervention
Negotiated group
Individual beliefs mediate the development of a successful PA plan, which is an interactive process that is therapeutic and includes “mutual inquiry, problem-solving, and negotiation between” instructor and participant.47 Cress et al48 found that the development of contracts to promote PA among older adults is a best-practice for PA programs and recommended tailoring exercise to meet individual needs, which should include balance, flexibility, aerobics, and strengthening. Persons in the negotiated treatment group of this study developed individualized, negotiated follow-up adherence contracts with their instructor during week 6 of Fit and Strong!. The purpose of the contract was to create an individualized plan for PA maintenance upon completion of Fit and Strong!. The contract process reviewed participants’ preferences, capability, and access to PA opportunities in their respective environments. The contract required participants to articulate strategies for handling relapse and barriers to exercise. During contract development, participants chose the time of day, location, mode, and type of PA in which they would engage regularly. The instructor and participant worked together to identify types and duration of stretching, aerobic, and strengthening activities that would be performed at specific times of the week in specific, realistic locations. The contract required participants to engage in one hour of PA or 20 minutes each of stretching, aerobic, and strengthening activities per day for a minimum of 3 days per week. The instructor evaluated participant preferences, offered relevant information/resources, and assisted participants to develop achievable, realistic PA goals. TR counselors reviewed the contract and continued to review and revise goals and action plans with negotiated group participants after the intervention ended.
Mainstreamed group
Mainstreamed participants did not develop negotiated maintenance contracts but were referred instead to an on-going PA program during week 6 of Fit and Strong!. The program was a best-practice, multiple-component PA program offered at the same facility as Fit and Strong! and was expected to enable participants to maintain participation in group, facility-based exercise. Participants in the negotiated group were hypothesized to have better outcomes than participants in the mainstreamed group because negotiated participants developed individually tailored exercise contracts.
TR
Participants in both TR groups were scheduled to receive 20 calls during months 3 to 18. The protocol specified bi-weekly calls during months 3 to 6, tapering to once a month during months 7 to 18. Calls were conducted by trained Master of Public Health students (N=4) or by the Master’s level-prepared study staff members (N=2). All study staff members were trained in TTM, arthritis management strategies, evaluation of PA participation, type, intensity, frequency, and duration, as well as goal-setting, problem-solving techniques, exercise programming and resources, monitoring progress, and reactivation and maintenance strategies. Both negotiated and mainstreamed TR interview strategies applied theoretical components of TTM. Calls sought to increase motivation and confidence, recognize and overcome PA barriers, maximize facilitators for exercise, and initiate, increase, and maintain PA.
Phone counselors for both study groups reviewed each participant’s previous interview before conducting the current interview as a reminder of the participant’s history and issues. Counselors asked participants to rate their motivation and confidence in meeting their exercise plan on a scale of 1(no confidence or motivation) to 10 (high confidence or motivation). Counselors then asked participants about barriers and facilitators of exercise and ways to overcome barriers. If participants had difficulty thinking of ways to overcome barriers, counselors offered suggestions. For instance, if weather was a barrier, the counselor would say: “Many people report weather as a barrier to exercise; some methods that have worked for them include doing Fit and Strong! exercises indoors with music, cleaning the house, or going to an indoor mall to walk. Do you think these options would work for you, and how would you incorporate this new activity into your day?” The counselor also asked participants about exercise opportunities and what worked for them: “Has there ever been an instance where you faced the same barrier but exercised anyway? What was unique about the situation that helped you move forward with exercising?” If the participant was still having difficulty coming up with a strategy to overcome a barrier, the counselor was instructed to ask the participant for more information: “What is it about the barrier that makes it difficult to come up with a strategy? What strategies did you try in the past that did not work? Why do you think the strategies did not work?” The participant could be predisposed to failure by having high expectations for exercise, exercising at an inconvenient time/location, or other reasons. Counselors probed to uncover issues that could engage participants to problem-solve and identify unique solutions to challenges encountered.
Among the common barriers counselors reviewed included such things as experiencing arthritis pain or stiffness, finding a convenient location for exercise, and having a busy schedule. Counselors asked participants to report whether each barrier applied to them, and if so, how much the barrier kept them from exercising or reduced their level of exercise. All participants were asked to report type, frequency, duration, and intensity of stretching/flexibility, aerobic, and strengthening exercise. For example, participants might describe a group-based program in which they were involved or exercises completed at home. The calls also monitored participant PA maintenance and problem-solved ways to maintain or reactivate PA. If participants indicated that they had reduced their activity or had stopped exercise, counselors would ask participants about feasible ways to increase participation, such as engaging in short episodes of activity at home over the course of each day.
Independent Variables
Primary independent variables for this study were TR receipt vs no TR receipt, maintenance treatment group (negotiated vs mainstreamed), and total number of TR calls (TR dose). TR dose was defined as the number of TR calls received or the number of completed TR interviews/sessions and was a continuous variable.
Covariates
Covariates were demographic, health, and disease characteristics. Demographics included age, sex, race/ethnicity, educational status, and income level. Health characteristics included arthritis functional class44–46 and BMI. Disease characteristics were obtained using a self-report disease inventory from the GERI-AIMS49 that inquires about the presence or absence of 19 common chronic conditions.
Statistical Analysis
This study tested the following hypotheses:
Hypothesis 1
Participants who received TR in both negotiated and mainstreamed treatment groups (N-TR and M-TR) will have significantly higher positive movement on these measures at 2, 6, 12, and 18-months than participants in both of these groups who did not receive TR (N-noTR and M-noTR). Participants in the negotiated group who received TR (N-TR) will show the greatest benefit.
Hypothesis 2
Participants who received more calls (TR dose) in both negotiated and mainstreamed treatment groups (N-TR and M-TR) will perform better on these measures at 2, 6, 12, and 18-months than participants in both of these groups who received fewer calls. This hypothesis tests the main effect of TR dose.
Statistical analyses were conducted using SPSS, SAS, and Microsoft Excel. Logistic regression analysis was conducted to test whether attrition from measurement at 2, 6, 12, and 18-months was a function of random assignment. The M-noTR group was chosen as the reference category because this group received the least intensive treatment.
Longitudinal data analyses were conducted using mixed-effects regression models (MRM).50 MRM determined whether a differential change occurred in each outcome as a function of receipt of TR, maintenance treatment group, and TR dose. Covariates were included in the models to examine their influence on outcomes.
RESULTS
Study Sample
The total study sample (N=486) was 87% female, with a mean age of 71, (range: 59 to 91 years). Study participants were 51% African American, 35% non-Hispanic White, 7% Hispanic/Latino, 3% Asian or Pacific Islander, 1% Native American or Alaskan Native, and 2% Other. The majority had an education level of high school or more and annual incomes under $20,000. Most participants were categorized as arthritis functional class II (73%), indicating mild impairment.44–46 A substantial majority of participants were overweight or obese (82%). Arthritis (96%), high blood pressure (65%), vision problems (30%), and diabetes (24%) were the most frequently reported chronic conditions. No statistically significant differences were found among any of the 4 groups on demographic, health, or disease characteristics at baseline.
Attrition from Treatment: TR
Of 248 participants randomized to receive TR, 121 were assigned to the negotiated group and 127 to the mainstreamed group. Both groups were scheduled to receive 20 calls during months 3–18, including 8 calls during months 3–6 and 12 calls during months 7–18. During months 3–6, an average of 4 of 8 possible sessions was completed for the negotiated group (50% of the intended dose). During the same time frame, a mean of 3 sessions was completed for the mainstreamed group, representing 38% of the intended dose. The mean dose during months 7–18 for the negotiated group was 58%, compared to 50% for the mainstreamed group during the same time frame. Participants who refused TR were dropped from TR but could continue with measurement. During months 3–18, 21% of N-TR group participants and 20% of M-TR group participants refused TR, showing little difference by group. Primary reasons for refusal included unable to contact after several attempts (58%), refused calls (24%), no time (8%), health (8%), and caregiving (2%).
Measurement Retention
The percentage of participants who completed measurement decreased over time, from 86% at 2 months, to 65% at 6 months, 64% at 12 months, and 53% at 18 months (Figure 1). Participants lost to follow-up included persons who dropped out of the study or those who did not complete measurement at specific points in time. Logistic regression analysis tested whether the probability of response at each measurement point in time was a function of random assignment and found no statistically significant difference in response when comparing each of the remaining 3 randomized groups to the reference group, indicating that probability of response did not differ significantly by study group.
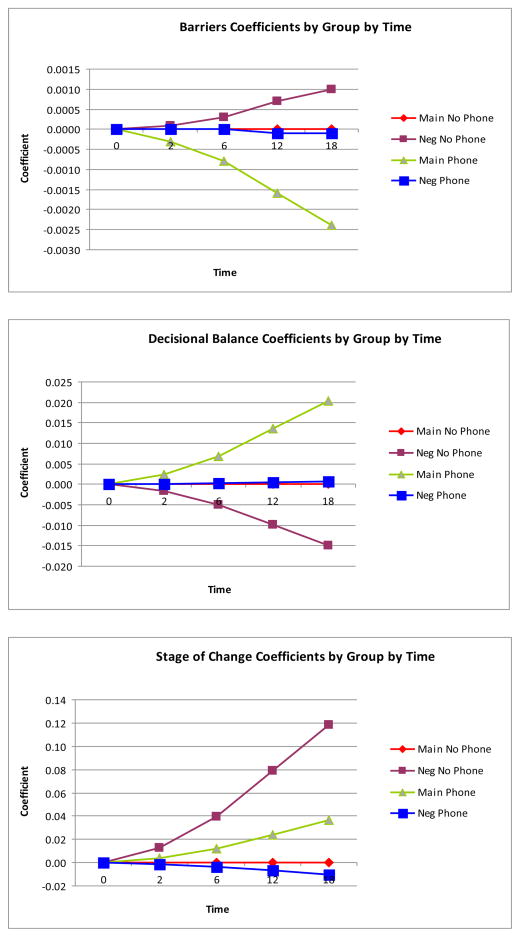
Barriers
Regression analysis (Table 1) found that the interaction of TR condition by maintenance treatment group-by-time (b = .05, p = .04) was statistically significant coefficients by group-by-time (Figure 2) indicates that M-TR participants reported fewer barriers over time. N-TR and M-noTR participants showed little change on this measure over time; however, participants in the N-noTR group reported more barriers over time. TR dose did not have a statistically significant .03, p = .24). In addition to these findings, men (b = −.26, p = .03) and participants with more education (b = −.10, p = .01) reported significantly fewer barriers. Finally, high BMI (b = .12, p = .02) and presence of diabetes (b = .19, p = .045) were related to a significant increase in barriers.
Table 1.
Longitudinal Regression Model for Outcome: Barriers
| Effect | b | se | t | p |
|---|---|---|---|---|
| Intercept | 2.82 | .59 | 4.79 | <.0001 |
| TR dose | .03 | .03 | 1.19 | .24 |
| TR Condition (Phone or No phone reinforcement) | −.09 | .11 | −.83 | .41 |
| Maintenance Treatment Arm (Negotiated-Mainstreamed) | .04 | .11 | .35 | .73 |
| Timepoint (baseline,2,6,12,18 months) | .00 | .01 | .12 | .90 |
| Sex | −.26 | .11 | −2.27 | .03 |
| Education | −.10 | .04 | −2.84 | .01 |
| Race | −.09 | .17 | −.54 | .59 |
| Income | −.03 | .02 | −1.22 | .23 |
| Age | .00 | .01 | −.47 | .64 |
| Arthritis functional class | .02 | .08 | .29 | .77 |
| Body mass index (BMI) | .12 | .05 | 2.32 | .02 |
| Arthritis | −.11 | .15 | −.78 | .44 |
| High blood pressure | .11 | .08 | 1.29 | .20 |
| Vision problems | .00 | .06 | .07 | .95 |
| Diabetes | .19 | .09 | 2.03 | .05 |
| Interactions | ||||
| TR Condition* Maintenance Treatment Arm | .01 | .02 | .09 | .93 |
| TR Condition * Timepoint | −.03 | .02 | −1.40 | .16 |
| Maintenance Treatment Arm * Timepoint | −.04 | .16 | −2.71 | .01 |
| TR Condition * Maintenance Treatment Arm * Timepoint | .05 | .02 | 2.05 | .04 |
| χ2 | 118.13 | <.0001 | ||
| Model degrees of freedom | 2 | |||
| Covariance Parameter Estimates | b | se | z | p |
| UN (Intercept,Intercept) | .326000 | .043800 | 7.440000 | <.0001 |
| UN (Timepoint, Intercept) | .000919 | .003689 | .250000 | .803300 |
| UN (Timepoint, Timepoint) | 7.56E-20 | |||
| ID | .229500 | .020940 | 10.960000 | <.0001 |
Figure 2.
Coefficient Plots
Decisional Balance
Regression analysis (Table 2) found that the interaction of TR condition by maintenance treatment group-by-time (b = −.06, p = .02) was statistically significant. Plotting the coefficients by group-by-time (Figure 2) shows that scores improved over time among M-TR participants. M-noTR and N-TR participants showed little change over time, whereas scores for N-noTR participants again declined. TR dose did not have a statistically significant on decisional balance (b = −.04, p = .15). However, a strong, significant, positive relationship was again seen between education and decisional balance (b = .24, p = .0001), indicating that participants with more education scored higher on this measure. In contrast, participants with high blood pressure (b = −.29, p = .01) and those with diabetes (b = −.31, p = .02) scored significantly lower on decisional balance compared to those without these conditions.
Table 2.
Longitudinal Regression Model for Outcome: Decisional Balance
| Effect | b | se | t | p |
|---|---|---|---|---|
| Intercept | 2.09 | .84 | 2.48 | .01 |
| TR dose | −.04 | .03 | −1.43 | .15 |
| TR Condition (Phone or No phone reinforcement) | −.04 | .16 | −.25 | .80 |
| Maintenance Treatment Arm (Negotiated-Mainstreamed) | .03 | .16 | .18 | .86 |
| Timepoint (baseline,2,6,12,18 months) | −.03 | .01 | −2.19 | .03 |
| Sex | .20 | .17 | 1.23 | .22 |
| Education | .24 | .05 | 4.49 | <.0001 |
| Race | .20 | .23 | .84 | .40 |
| Income | −.03 | .03 | −1.01 | .31 |
| Age | −.01 | .01 | −1.03 | .31 |
| Arthritis functional class | −.14 | .12 | −1.12 | .26 |
| Body mass index (BMI) | .06 | .07 | .85 | .39 |
| Arthritis | .18 | .21 | .87 | .38 |
| High blood pressure | −.29 | .11 | −2.52 | .01 |
| Vision problems | −.06 | .08 | −.67 | .50 |
| Diabetes | −.31 | .13 | −2.36 | .02 |
| Interactions | ||||
| TR Condition* Maintenance Treatment Arm | −.08 | .23 | −.37 | .72 |
| TR Condition * Timepoint | .08 | .03 | 2.92 | .00 |
| Maintenance Treatment Arm * Timepoint | .04 | .02 | 2.29 | .02 |
| TR Condition * Maintenance Treatment Arm * Timepoint | −.06 | .03 | −2.35 | .02 |
| χ2 | 200.18 | <.0001 | ||
| Model degrees of freedom | 2 | |||
| Covariance Parameter Estimates | b | se | z | p |
| UN (Intercept,Intercept) | .805400 | .092100 | 8.740000 | <.0001 |
| UN (Timepoint, Intercept) | .005509 | .007243 | .760000 | .446900 |
| UN (Timepoint, Timepoint) | .000195 | .000662 | .290000 | .384000 |
| ID | .446200 | .041140 | 10.850000 | <.0001 |
Stage of Change
Regression analysis (Table 3) found that the interaction of TR condition by maintenance treatment group-by-time (b = −.27, p = .01) was statistically significant. The plot of coefficients (Figure 2) depicting the relationship among TR condition, maintenance treatment group, and time indicated that participants in the N-noTR group showed the most improvement in stage, followed by participants in the M-TR group. In contrast, participants in M-noTR and N-TR groups showed little change over time. TR dose was not statistically significant for SOC (b = .04, p = .71). Only high BMI was significantly associated with lower SOC (b = −.41, p = .01).
Table 3.
Longitudinal Regression Model for Outcome: Stage of Change
| Effect | b | se | t | p |
|---|---|---|---|---|
| Intercept Stage 2 | 1.43 | 1.73 | .82 | .41 |
| Intercept Stage 3 | 6.19 | 1.84 | 3.36 | .00 |
| Intercept Stage 4 | 3.29 | 1.74 | 1.90 | .06 |
| Intercept Stage 5 | −.02 | 1.73 | −.01 | .99 |
| TR dose | .04 | .10 | .38 | .71 |
| TR Condition (Phone or No phone reinforcement) | −.09 | .33 | −.26 | .80 |
| Maintenance Treatment Arm (Negotiated-Mainstreamed) | −.28 | .33 | −.85 | .40 |
| Timepoint (baseline,2,6,12,18 months) | −.02 | .07 | −.33 | .74 |
| Sex | .33 | .33 | 1.02 | .31 |
| Education | .07 | .11 | .70 | .49 |
| Race | .17 | .47 | .36 | .72 |
| Income | −.04 | .08 | −.55 | .58 |
| Age | .02 | .02 | 1.16 | .25 |
| Arthritis functional class | −.43 | .24 | −1.85 | .07 |
| Body mass index (BMI) | −.41 | .16 | −2.65 | .01 |
| Arthritis | −.20 | .51 | −.40 | .69 |
| High blood pressure | .13 | .24 | .55 | .58 |
| Vision problems | .02 | .22 | .11 | .91 |
| Diabetes | −.02 | .27 | −.08 | .94 |
| Interactions | ||||
| TR Condition* Maintenance Treatment Arm | .41 | .48 | .87 | .39 |
| TR Condition * Timepoint | .16 | .08 | 1.93 | .06a |
| Maintenance Treatment Arm * Timepoint | .18 | .07 | 2.46 | .02 |
| TR Condition * Maintenance Treatment Arm * Timepoint | −.27 | .10 | −2.77 | .01 |
| Log likelihood | 10,655.30b | |||
| Iterations | 32 | |||
| Covariance Parameter Estimates | b | se | ||
| Intercept | 1.412300 | .315800 | ||
| Timepoint | .003918 | .005793 | ||
Note.
Not significant (borderline)
Convergence criteria satisfied
DISCUSSION
Little is known about behavioral factors that impact PA maintenance among older adults in general, and even less is known about their impact among diverse subgroups of older adults, including those with OA.9–12 Participants in this study were primarily older women from diverse racial/ ethnic backgrounds. Study results indicate that the M-TR group showed the most improvement in perception of PA barriers and decisional balance, whereas the N-noTR showed the most improvement in PA stage over time.
Barriers
Across TR recipient groups, the mainstreamed group showed more reduction in barriers over time than the negotiated group, contrary to our hypothesis. M-TR participants did not have an opportunity to develop a tailored PA contract during Fit and Strong!. Therefore, they may have valued and/or benefited more from TR than N-TR participants. In contrast, N-noTR participants showed an increase in barriers over time. Because the latter group also showed the highest maintenance of PA (SOC), it could be that participants in this group encountered more barriers as they exercised but managed to surmount them. TR dose did not affect perceived barriers. Appropriate TR dose may need to be individually prescribed to reflect environmental, social, behavioral, or biological factors.
Sex and education were statistically significant covariates in this analysis. Men reported fewer barriers than women, consistent with findings that older women have positive attitudes about PA, but are less likely to engage in exercise due to certain barriers.51 Participants with more education reported fewer barriers than people with less education, consistent with the fact that low educational level is a well-established correlate of sedentary behavior.52 In contrast, participants with high BMI reported more barriers than those with lower BMI. Again, perceived overweight status is a known PA barrier for both men and women.53,54 Participants with diabetes also reported more barriers compared to those without diabetes. Negative feelings about weight and symptoms, such as pain and fatigue among overweight participants with diabetes, constitute a primary barrier to exercise participation.55
Decisional Balance
Across TR recipients, those in the negotiated group were predicted to perform better on decisional balance than counterparts in the mainstreamed group. However, the reverse was true. The reason for this finding might be similar to that reported for the barriers measure. Participants in the mainstreamed group did not have the opportunity to develop the PA contract with their instructor; therefore, they may have valued and/or benefited more from the TR calls than participants in the negotiated group. Again, the N-noTR group had the lowest decisional balance scores over time but scored best with respect to maintenance (SOC). This finding also may indicate that maintaining exercise is an ongoing struggle, leading to a more balanced view of pros and cons. Similar to the barriers measure, TR dose did not significantly influence decisional balance, suggesting the need to develop criteria for determining appropriate dose.
Increased education also was related to improved decisional balance; high blood pressure and diabetes were related to poor decisional balance. No literature could be found that has examined the impact of co-morbid conditions on decisional balance for PA among older adults with OA. This is an important gap because persons with arthritis who have cardiovascular disease or diabetes are less likely than persons with arthritis who do not have these conditions to engage in physician-prescribed exercise.56,57 This finding underscores a need to examine ways to promote PA engagement and maintenance among persons with multiple chronic conditions.
Stage of Change
The N-noTR group showed the greatest improvement in stage compared to the other study groups, contrary to what was hypothesized. Paradoxically, as already noted, the same group showed the most increase in barriers and decline in decisional balance over time. It could be that N-noTR participants implemented their contracts in the absence of TR; barriers became more apparent, but they managed to surmount them.
Taken as a whole, the main findings for all 3 outcomes suggest that TR positively impacts perception of PA (barriers and decisional balance). However, participation in a negotiated contract appears to operate differently and may promote actual PA behavior change, as indicated by improvement in stage. These findings suggest that TR helps people change/maintain positive perceptions of PA, whereas, the negotiated contract helps people adopt and maintain a physically active lifestyle.
Limitations
Limitations for this study include attrition from TR and post-test measurement. With respect to receipt of TR, participants in the negotiated group completed 53% of calls, compared to 43% for the mainstreamed group, but retention in TR was roughly similar. Two-thirds (66%) of participants in the N-TR group and 70% of those in the M-TR group remained in TR through its intended duration. Participants in the M-TR group were somewhat more likely to remain in TR but completed fewer calls on average compared to those in the N-TR group. This finding suggests that the 2 groups may differ on certain characteristics not associated with group assignment, or it may indicate that the M-TR group valued the calls more. The latter interpretation is consistent with their improvement on 2 of the 3 study outcomes.
Measurement retention decreased over time from 86% at 2 months to 53% at 18 months. However, results showed that the probability of response at 2, 6, 12, or 18 months past baseline was not a function of group assignment. Although TR dose was included in regression analyses to examine impact on outcomes, it was not statistically significant in any of the models, indicating that number of calls received did not substantially influence outcomes. This finding may suggest that other environmental, social, behavioral, or biological factors might have impacted outcomes more than TR itself. Future research should explore how these factors influence PA behavior, and also, examine how they might confound the relationship between call dose and outcome.
Finally, our study sample was overwhelmingly female, indicating the need to develop and implement recruitment strategies which target older men.
Summary and Conclusions
Findings from this study offer insight into the exercise maintenance behavior of older adults with OA, a population that is dramatically increasing in size, but has received minimal attention with respect to this particular PA research topic. The main findings suggest that addition of TR as a mainte -nance strategy to short-term PA interventions that do not include a negotiated contract for follow-up may bolster positive perceptions of PA but does not appear to impact actual maintenance of the behavior. In contrast, providing an opportunity to develop a tailored, negotiated follow-up contract seems to improve actual maintenance of PA. Thus, the negotiated contract simultaneously appears to be more effective and less expensive to implement.
The secondary findings indicate that future studies should examine the use of specific TR strategies to determine their effectiveness with sub-groups of older adults. From an implementation and economic perspective, it is important to identify the minimal, effective call dose to promote PA maintenance. The appropriate dose may vary by cognitive and personality factors, health and disease characteristics, demographics, and environmental factors. Evaluation of commonly reported barriers by people who have risk factors for sedentary behavior along with successful strategies used to overcome barriers can contribute to the development of methods to promote their exercise maintenance. Examining the exercise goals and plans of those who successfully maintain their exercise behavior may provide effective maintenance strategies.
Further research also should assess the directional/causal relationship of primary outcomes from this study with one another and their impact on PA participation over time to improve understanding of the long-term PA behavior of study participants. These more sophisticated analyses are needed to examine causation between change in perception and behavior change.
Finally, these results provide a strong basis to review methods used to implement short-term, facility-based PA interventions. To date, standard operating procedures in many exercise programs have been to advise participants to use their own resources to put together a follow-up program of their own devising - a “cold handoff” at best. Results of this study call into question the sustainability of effects produced by such interventions, highlight the negative consequence that can result from lack of resources and planning allocated to maintenance, and underscore the need to incorporate strategies like a tailored, negotiated contract that appears to promote both PA adoption and maintenance over time, into short-term PA programs going forward.
Acknowledgments
This work was supported by the National Institute on Aging (grant number R01 AG23424). We would like to thank the organizations, participants, faculty, and staff involved in this study. We would also like to recognize the software developed by Michael Berbaum, PhD, which was applied to conduct stratification and randomization.
Footnotes
Human Subjects Statement
This study was approved by the University of Illinois at Chicago Office for the Protection of Research Subjects, IRB Protocol #: 2003-0663.
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
References
- 1.Brault MW, Hootman J, Helmick CG, et al. Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58(16):421–426. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2003–2005. MMWR Morb Mortal Wkly Rep. 2006;55(40):1089–1092. [PubMed] [Google Scholar]
- 3.Dunlop DD, Hughes SL, Manheim LM. Disabilities in activities of daily living. Patterns of change and a hierarchy of disability. Am J Public Health. 1997;87:378–383. doi: 10.2105/ajph.87.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunlop DD, Hughes SL, Edelman P, et al. Impact of joint impairment on disability and disability-specific domains at four years. J Clin Epidemiol. 1998;51(12):1253–1261. doi: 10.1016/s0895-4356(98)00128-0. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. [Accessed November 27, 2013];Arthritis types: osteoarthritis. 2011 Available at: http://www.cdc.gov/arthritis/basics/osteoarthritis.htm.
- 6.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis, National Health Interview Survey, 2002. Am J Prev Med. 2006;30(5):385–393. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality and Centers for Disease Control and Prevention. [Accessed November 27, 2013];Physical activity and older Americans: benefits and strategies. 2002 Available at http://www.ahrq.gov/legacy/ppip/activity.htm.
- 9.van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22(2):120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 10.Conn VS, Minor MA, Burks KJ, et al. Integrative review of physical activity intervention research with aging adults. J Am Geriatr Soc. 2003;51(8):1159–1168. doi: 10.1046/j.1532-5415.2003.51365.x. [DOI] [PubMed] [Google Scholar]
- 11.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults: a critical review and recommendations. Am J Prev Med. 1998;15(4):316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 12.Focht BC. Effectiveness of exercise interventions in reducing pain symptoms among older adults with knee osteoarthritis: a review. J Aging Phys Act. 2006;14(2):212–235. doi: 10.1123/japa.14.2.212. [DOI] [PubMed] [Google Scholar]
- 13.Albright CL, Pruitt L, Castro C, et al. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Ann Behav Med. 2005;30(3):191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- 14.Piette JD, Richardson C, Himle J, et al. A randomized trial of telephonic counseling plus walking for depressed diabetes patients. Med Care. 2011;49(7):641–648. doi: 10.1097/MLR.0b013e318215d0c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yates BC, Anderson T, Hertzog M, et al. Effectiveness of follow-up booster sessions in improving physical status after cardiac rehabilitation: health, behavioral, and clinical outcomes. Appl Nurs Res. 2005;18(1):59–62. doi: 10.1016/j.apnr.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 16.Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Health Behav. 2012;42(1):81–88. doi: 10.1016/j.amepre.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 17.Hughes SL, Seymour RB, Campbell RT, et al. Fit and Strong!: bolstering maintenance to physical activity among older adults with lower-extremity osteoarthritis. Am J Health Behav. 2010;34(6):750–763. doi: 10.5993/ajhb.34.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50(5):1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 19.van Gool CH, Penninx BWJH, Kempen GIJM, et al. Determinants of high and low attendance to diet and exercise interventions among overweight and obese older adults: results from the arthritis, diet, and activity promotion trial. Contemp Clin Trials. 2006;27(3):227–237. doi: 10.1016/j.cct.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Messier SP, Legault C, Mihalko S, et al. The intensive diet and exercise for arthritis (IDEA) trial: design and rationale. BMC Musculoskelet Disord. 2009;10(93):1–14. doi: 10.1186/1471-2474-10-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Messier SP, Legault C, Mihalko S, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–1273. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 23.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 24.Janis IL, Mann L. Decision Making: A Psychological Analysis of Conflict, Choice, and Commitment. New York, NY: Free Press; 1977. [Google Scholar]
- 25.Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- 26.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39(5):1056–1061. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Stiggelbout M, Hopman-Rock M, Crone M, et al. Predicting older adults’ maintenance in exercise participation using an integrated social psychological model. Health Educ Res. 2006;21(1):1–14. doi: 10.1093/her/cyh037. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien Cousins S. A self-referent thinking model: how older adults may talk themselves out of being physically active. Health Promot Pract. 2003;4(4):439–448. doi: 10.1177/1524839903255417. [DOI] [PubMed] [Google Scholar]
- 29.Guillot J, Kilpatrick M, Hebert E, Hollander D. Applying the transtheoretical model to exercise adherence in clinical settings. American Journal of Health Studies. 2004;19(1):1–10. [Google Scholar]
- 30.Marshall SJ, Biddle SJ. The transtheoretical model of behavior change: a meta-analysis of applications to physical activity and exercise. Ann Behav Med. 2001;23(4):229–246. doi: 10.1207/S15324796ABM2304_2. [DOI] [PubMed] [Google Scholar]
- 31.Nigg CR. Physical Activity Assessment Issues in Population Based Interventions: A Stage Approach. In: Welk GJ, editor. Physical Activity Assessments for Health-related Research. Champaign, IL: Human Kinetics; 2002. pp. 227–239. [Google Scholar]
- 32.Barké CR, Nicholas PR. Physical activity in older adults: the stages of change. J Appl Gerontol. 1990;9(2):216–223. [Google Scholar]
- 33.Gorely T, Gordon S. An examination of the transtheoretical model and exercise behavior in older adults. J Sport Exerc Psychol. 1995;17(3):312–324. [Google Scholar]
- 34.Hellman EA. Use of the stages of change in exercise adherence model among older adults with a cardiac diagnosis. J Cardiopulm Rehabil. 1997;17(3):145–155. doi: 10.1097/00008483-199705000-00001. [DOI] [PubMed] [Google Scholar]
- 35.Marcus BH, Simkin LR. The stages of exercise behavior. J Sports Med Phys Fitness. 1993;33(1):83–88. [PubMed] [Google Scholar]
- 36.Spencer L, Adams TB, Malone S, et al. Applying the transtheoretical model to exercise: a systematic and comprehensive review of the literature. Health Promot Pract. 2006;7(4):428–443. doi: 10.1177/1524839905278900. [DOI] [PubMed] [Google Scholar]
- 37.Kahn RL, Goldfarb AI, Pollack M, Peck A. Brief objective measures for the determination of mental status in the aged. Am J Psychiatry. 1960;117:326–328. doi: 10.1176/ajp.117.4.326. [DOI] [PubMed] [Google Scholar]
- 38.Wing RR, Jeffery RW, Burton LR, et al. Change in waist-hip ratio with weight loss and its association with change in cardiovascular risk factors. Am J Clin Nutr. 1992;55(6):1086–1092. doi: 10.1093/ajcn/55.6.1086. [DOI] [PubMed] [Google Scholar]
- 39.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision-making for exercise. Health Psychol. 1992;11(4):257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 40.Marcus B, Bock B, Pinto B, et al. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20(3):174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 41.Cox KL, Gorely TJ, Puddey IB, et al. Exercise behaviour change in 40 to 65-year-old women: the SWEAT study (sedentary women exercise adherence trial) Br J Health Psychol. 2003;8(Pt. 4):477–495. doi: 10.1348/135910703770238329. [DOI] [PubMed] [Google Scholar]
- 42.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 43.Seymour RB, Hughes SL, Campbell RT, et al. Comparison of two methods of conducting Fit and Strong! Arthritis Care Res. 2009;61(7):876–884. doi: 10.1002/art.24517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 45.Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 46.ARA Glossary Committee, American Rheumatism Association. Dictionary of the Rheumatic Diseases: Vol. 1. Signs and Symptoms. New York, NY: Contact Associates International; 1982. [Google Scholar]
- 47.Jensen GM, Lorish CD. Promoting patient cooperation with exercise programs: linking research, theory, and practice. Arthritis Care Res. 1994;7(4):181–189. doi: 10.1002/art.1790070405. [DOI] [PubMed] [Google Scholar]
- 48.Cress ME, Buchner DM, Prohaska T, et al. Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act. 2005;13(1):61–74. doi: 10.1123/japa.13.1.61. [DOI] [PubMed] [Google Scholar]
- 49.Hughes SL, Edelman P, Chang RW, et al. The GERI-AIMS. Reliability and validity of the arthritis impact measurement scales adapted for elderly respondents. Arthritis Rheum. 1991;34(7):856–865. doi: 10.1002/art.1780340711. [DOI] [PubMed] [Google Scholar]
- 50.Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, NJ: Wiley-Interscience; 2006. [Google Scholar]
- 51.Lee C. Factors related to the adoption of exercise among older women. J Behav Med. 1993;16(3):323–334. doi: 10.1007/BF00844763. [DOI] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention. State Behavioral Risk Factor Surveillance System Coordinators. Prevalence of sedentary lifestyle -- behavioral risk factor surveillance system, United States, 1991. MMWR Morb Mortal Wkly Rep. 1993;42(29):576–579. [PubMed] [Google Scholar]
- 53.Atlantis E, Barnes EH, Ball K. Weight status and perception barriers to healthy physical activity and diet behavior. Int J Obes. 2008;32(2):343–352. doi: 10.1038/sj.ijo.0803707. [DOI] [PubMed] [Google Scholar]
- 54.Gallagher KI, Jakicic JM, Napolitano MA, Marcus BH. Psychosocial factors related to physical activity and weight loss in overweight women. Med Sci Sports Exerc. 2006;38(5):971–980. doi: 10.1249/01.mss.0000218137.25970.c6. [DOI] [PubMed] [Google Scholar]
- 55.Korkiakangas EE, Alahuhta MA, Laitinen JH. Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int. 2009;24(4):416–427. doi: 10.1093/heapro/dap031. [DOI] [PubMed] [Google Scholar]
- 56.Bolen J, Hootman J, Helmick CG, et al. Arthritis as a potential barrier to physical activity among adults with diabetes -- United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep. 2008;57(18):486–489. [PubMed] [Google Scholar]
- 57.Bolen J, Murphy L, Greenlund K, et al. Arthritis as a potential barrier to physical activity among adults with heart disease -- United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep. 2009;58(7):165–169. [PubMed] [Google Scholar]