Abstract
Objective
Examine sources, predictors, and child outcomes associated with NICU-related stress for mothers of infants born very preterm (VPT).
Study Design
Participants were 133 mothers of VPT infants admitted to a regional level-III NICU. At term equivalent, mothers completed the Parental Stressor Scale: NICU and were interviewed about their psychological wellbeing and family circumstances. Infant clinical data were also collected. At corrected age 4, 49 children were assessed for cognition, language, and socio-emotional development.
Result
Mothers reported moderate to low stress, with parental role alteration considered most stressful and parent-staff communications least stressful. Predictors of overall stress included maternal educational underachievement, stressful life events, postnatal depression, and infant unsettled-irregular behavior. NICU-related stress was associated with child anxiety and poorer language development.
Conclusion
Parental wellbeing is an important focus of care in the neonatal setting. Strategies are needed to optimize early engagement and reduce stress levels to assist improved child outcomes.
Keywords: Maternal Mental Health, NICU, Outcomes, Social Risk, Stress, Very Preterm
The Neonatal Intensive Care Unit (NICU) is an equipment and staff intensive environment where infants born very preterm (VPT) are exposed to invasive clinical procedures, frequent handling, and high levels of visual and auditory stimulation. Parents of these infants also are subject to psychological distress related to their infant's health and survival, risks of disability, family disruption, as well as physical and emotional features of the NICU environment.1, 2 Efforts to address the psychological needs of parents and families have tended to lag behind medical efforts to improve infant health and survival,3 despite evidence that parental factors such as maternal mental health, parenting, and family cohesion make an important independent contribution to the long-term developmental outcomes of VPT infants.4, 5, 6, 7
Research concerned with the wellbeing of women giving birth to a VPT infant show that these mothers tend to experience more severe psychological distress than mothers of healthy full-term infants.8, 9 However, several issues require further research and clarification. First, there is a need to better understand the specific aspects of the NICU experience that parents find stressful so as to target these in family-based intervention efforts. A recent review of 14 studies found that, in general, parents of high-risk neonates experience a sense of loss of control around caretaking and parenting responsibilities.10 But comparatively little attention has been given to the NICU experiences of parents of infants born VPT, with findings remaining somewhat unclear.2 Early studies described the experiences of small selected samples of predominantly North American parents recruited in the late 80s and early 90s.2 More recent studies have focused largely on intervention-based outcomes or on parental stress perceptions after hospital discharge.2, 8
A second issue of concern is the identification of factors that may place some mothers at an increased risk of experiencing high levels of stress. Findings to date suggest that maternal stress may be influenced by a range of factors spanning infant, maternal, and family social background characteristics.2 These include the severity of infant illness,1, 11 pregnancy planning and previous pregnancy loss,1 maternal trait anxiety and mental health history,11, 12 exposure to other stressful life events,13 maternal education,14 and family socioeconomic status.15 Identification of key factors that place mothers of VPT infants at an increased risk of adverse stress reactions will help assist staff to better recognize and meet the clinical needs of these potentially at-risk mothers and infants.
A final issue concerns the extent to which high levels of maternal stress in the NICU are associated with increased neurodevelopmental risks for their VPT infant. This is important since many family-based interventions in the NICU focus on reducing parental stress on the premise that this will lead to improved child outcomes. Yet there is currently no evidence to support a direct and prospective link between maternal NICU-related stress levels and longer-term child outcomes in this high-risk population.
Accordingly, the specific aims of this paper were as follows.
To describe sources of stress in the NICU for mothers of infants born VPT.
To identify infant, maternal, and family social background factors that may place mothers of VPT infants at an increased risk of high levels of stress in the NICU.
To examine links between the extent of maternal stress in the NICU and child developmental outcomes at corrected age 4 years.
METHODS
Sample
The sample consisted of 133 mothers whose infants were born VPT (≤32 weeks gestation) and admitted consecutively to the level-III NICU at Christchurch Women's Hospital in New Zealand from December 1999 to May 2004. This unit is the sole provider of neonatal intensive care services for the region. Exclusion criteria included infant died before discharge, congenital anomaly, non-English speaking mother, or family lived outside the region. Of those eligible to participate (N=157), 85% agreed. Table 1 describes the infant neonatal, maternal, and family social background characteristics of the sample.
Table 1.
Infant, Maternal, and Social Background Characteristics of the Sample (N=133)
| Characteristic | |
|---|---|
| Infant characteristic | |
| Gestational age at birth, M ± SD, weeks | 27.6 ± 2.4 |
| Birth weight, M ± SD, grams | 1046.2 ± 323.3 |
| Male sex, % | 50.4 |
| Twin birth, % | 29.3 |
| Oxygen therapy at 36 weeks, % | 37.6 |
| Postnatal dexamethasone use, % | 6.9 |
| Necrotizing enterocolitis, % | 1.5 |
| Patent ductus arteriosus, % | 36.1 |
| Retinopathy of prematurity, % | 33.8 |
| Confirmed sepsis, % | 22.6 |
| Maternal characteristic | |
| Maternal age, M ± SD, years | 30.6 ± 5.2 |
| Low educationa, % | 28.6 |
| Minority ethnicity, % | 15.0 |
| Single parenthood, % | 10.5 |
| Social background characteristic | |
| Family socioeconomic statusb | |
| Professional/managerial, % | 28.6 |
| Technical/skilled, % | 48.1 |
| Semiskilled/unskilled/unemployed, % | 23.3 |
Defined as not a high school graduate.
Assessed using the Elley-Irving Socioeconomic Index (Elley & Irving, 2003).
Procedure
At infant term equivalent age (40 weeks gestation) or hospital discharge, whichever came first, all study mothers were interviewed by a trained research nurse about their obstetric history, previous life stress, NICU experiences, psychological wellbeing, family circumstances and initial parenting experiences. To avoid bias, this interviewer did not work in the NICU. Extensive infant medical data were also collected from birth to discharge. At corrected age 4 years (± 2 weeks), a subsample of 49 children enrolled in a longitudinal MRI cohort study16, 17 completed an evaluation of their general cognitive ability, language development, and emotional and behavioral adjustment. The Regional Health and Disability Ethics Committee approved all procedures and written informed consent was obtained from all parents.
Measures
Maternal Perceptions of Stress in the NICU
The Parental Stressor Scale: NICU (PSS: NICU) assessed mothers perceived parental stress within the NICU.18 The PSS: NICU consists of 46 items, which form four subscales assessing stress related to infant appearance and behavior (19 items), parental relationship and communication with staff (11 items), parental role alteration (11 items), and sights and sounds in the NICU (5 items). For this study, the Metric-II scoring procedure was used to provide an overall mean stress score for each subscale ranging from 1 (not stressful) to 5 (extremely stressful). The PSS: NICU has good concurrent and predictive validity, and is internally consistent with Cronbach alphas ranging from .73 to .94.11, 18, 19
Infant, Maternal, and Family Social Background Predictors of Maternal Stress in the NICU
Based on previous research and theory, a variety of infant, maternal, and psychosocial factors were examined as potential predictors of maternal NICU-related stress. These measures are described below. Infant Clinical Characteristics included gestational age at birth, birth weight, and a composite neonatal illness index (scaled 0–6) derived by allocating a score of one for each of the following conditions: confirmed sepsis; necrotizing enterocolitis; oxygen therapy at 36 weeks; patent ductus arteriosus; postnatal dexamethasone use; and retinopathy of prematurity.
Neonatal Behavior and Maternal Confidence
The Mother and Baby Scales (MABS) is a 36-item parent report measure of infant alertness, negative emotionality, and maternal caretaking confidence.20 Items were rated on a 6-point Likert scale from 0 (not at all) to 5 (very much/often) to form three subscales: 1) lack of caretaking confidence; 2) infant unsettled-irregular behavior; and 3) infant alertness-responsiveness. Reliability coefficients are good ranging from .83 to .93.20
Maternal Psychological Wellbeing
The 10-item Edinburgh Postnatal Depression Scale (EPDS) measured maternal psychological wellbeing.21 This scale assessed the extent to which mothers experienced depressive symptoms during pregnancy (antenatal subscale) and in the postpartum period (postnatal subscale). Consistent with diagnostic criteria, questions focus on activity and motivation levels, eating and sleeping patterns, as well as on rumination. The EPDS is internally consistent and valid, detecting postnatal depression in 86% of cases. It also correlates highly with standardized psychiatric interview methods.22
Stressful Life Events
An adapted version of the 36-item Social Readjustment Rating Scale provided a measure of stressful life events in the last 12 months, e.g. job loss, death of family member.23 Items were rated on a Likert scale ranging from 1 (not stressful) to 4 (extremely stressful). If no stressful event was experienced, an item was coded 0. The number of stressful life events reported in the past year was summed to provide an overall stressful life events score.
Family Socioeconomic Status
The Elley and Irving Socioeconomic Index provided a measure of family socioeconomic status.24 This scale is derived from New Zealand census data and ranks families into six socioeconomic categories based on median income and education levels associated with occupations nationally. Categories range from 1 (professional) to 6 (unskilled), with a score of 7 used when neither parent was employed.
Child Developmental Outcomes (Age 4 Years)
At corrected age 4 years, children's general cognitive ability was assessed using a short form of the revised Wechsler Preschool and Primary Scales of Intelligence (WPPSI-R).25 Language development was assessed using the preschool version of the Clinical Evaluation of Language Fundamentals (CELF-P).26 Finally, child emotional and behavioral adjustment was assessed using the parent reported Strengths and Difficulties Questionnaire (SDQ).27 This assessment protocol has been described in detail previously.17
RESULTS
Maternal Perceptions of Stress in the NICU
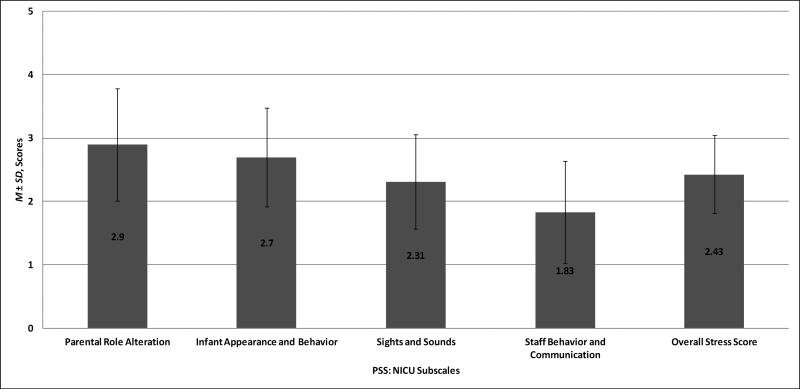
Figure 1 describes the distribution of PSS: NICU subscale scores for all mothers of infants born VPT. Results show that, on average, mothers reported the highest levels of stress in relation to their perceived loss of parental role (M=2.90) and their infants appearance and behavior (M=2.70). Mean ratings suggest these aspects of the NICU experience were moderately stressful for mothers (i.e. ratings close to 3 on a scale of 1 to 5). Least stressful were issues related to staff behavior and communication (M=1.83). Mothers’ mean overall stress scores were within the low to moderately stressful range (M=2.43).
Figure 1.
Sources of maternal stress in the NICU.
Of the 10 items from the highest ranking subscale, Parental Role Alteration, Table 2 shows that the item rated most stressful by mothers was “being separated from my baby”, with this perceived as very stressful (M=4.04). Next most stressful was “feeling helpless and unable to protect my baby from pain and painful procedures” (M=3.83) and “feeling helpless about how to help my baby during this time” (M=3.41).
Table 2.
PSS: NICU Parental Role Alteration Subscale Individual item Scores
| PSS: NICU Parental Role Alteration Subscale Item | Score, M ± SD |
|---|---|
| Being separated from my baby | 4.04 ± 1.08 |
| Feeling helpless and unable to protect my baby from pain and painful procedures | 3.83 ± 1.20 |
| Feeling helpless about how to help my baby during this time | 3.41 ± 1.39 |
| Not being able to hold my baby when I want | 3.34 ± 1.45 |
| Not feeding my baby myself | 2.99 ± 1.33 |
| Not being able to share my baby with other family members | 2.70 ± 1.36 |
| Not being able to care for my baby myself | 2.47 ± 1.48 |
| Being afraid of touching or holding my baby | 2.33 ± 1.39 |
| Feeling staff is closer to my baby than I am | 2.23 ± 1.44 |
| Sometimes forgetting what my baby looks like | 1.61 ± 1.15 |
Infant, Maternal, and Family Social Background Factors Associated with Maternal Stress in the NICU
Table 3 shows the associations between maternal levels of overall stress in the NICU and a range of infant, maternal, and social background factors. Mothers were stratified into three groups based on the degree of stress reported. These groups were: low stress (≤50th percentile); moderate stress (51st–85th percentile); and high stress (>85th percentile). The use of different cut-points and alternative classifications all produced results that were consistent with those presented in Table 3.
Table 3.
Infant, Maternal, and Social Background Factors Associated with Overall Maternal Stress in the NICU
| Characteristic | Extent of Maternal Stress in the NICU |
F/χ2 | p | ||
|---|---|---|---|---|---|
| Low (N=67) | Moderate (N=46) | High (N=20) | |||
| Infant characteristic | |||||
| Gestational age at birth, M ± SD, weeks | 27.4 ± 2.3 | 28.0 ± 2.3 | 27.2 ± 2.8 | 0.08 | .78 |
| Birth weight, M ± SD, grams | 1042.6 ± 300.9 | 1088.6 ± 331.4 | 960.5 ± 373.7 | 1.0 | .32 |
| Male sex, % | 50.7 | 47.8 | 55.0 | 0.03 | .87 |
| Twin birth, % | 34.3 | 19.6 | 35.0 | 0.34 | .56 |
| Neonatal illness indexa, M ± SD | 1.4 ± 1.4 | 1.2 ± 1.5 | 2.0 ± 1.8 | 2.44 | .12 |
| MABS unsettled-irregular score, M ± SD | 7.7 ± 5.2 | 9.3 ± 5.9 | 11.8 ± 6.5 | 7.98 | .005 |
| MABS alertness-responsive score, M ± SD | 11.3 ± 2.6 | 11.0 ± 3.3 | 12.4 ± 2.5 | 2.42 | .12 |
| Maternal characteristic | |||||
| Maternal age, M ± SD, years | 31.4 ± 4.5 | 29.8 ± 4.7 | 29.7 ± 7.9 | 1.72 | .19 |
| Low educationb, % | 22.4 | 28.3 | 50.0 | 4.91 | .03 |
| Minority ethnicity, % | 11.9 | 15.2 | 25.0 | 1.83 | .19 |
| Single parenthood, % | 7.5 | 10.9 | 20.0 | 2.33 | .17 |
| EPDS antenatal depression score, M ± SD | 7.5 ± 3.9 | 8.8 ± 4.5 | 9.2 ± 5.0 | 2.48 | .12 |
| EPDS postnatal depression score, M ± SD | 6.5 ± 4.1 | 8.8 ± 4.5 | 10.4 ± 4.7 | 12.91 | < .001 |
| MABS lack of confidence score, M ± SD | 5.2 ± 4.0 | 7.6 ± 4.1 | 8.7 ± 5.2 | 10.23 | .002 |
| Total stressful life events, M ± SD | 4.2 ± 3.3 | 5.0 ± 3.3 | 7.6 ± 4.3 | 14.66 | < .001 |
| Social background characteristic | |||||
| Low family socioeconomic statusc, % | 26.9 | 8.7 | 45.0 | 0.06 | .80 |
Sum of risk of confirmed sepsis, necrotizing enterocolitis, oxygen therapy at 36 weeks, patent ductus arteriosus, postnatal dexamethasone use, and retinopathy of prematurity.
Defined as not a high school graduate.
Defined as semiskilled/unskilled/unemployed as assessed using the Elley-Irving Socioeconomic Index (Elley & Irving, 2003).
With respect to infant neonatal characteristics, a linear association was found between maternal reports of infant unsettled-irregular behavior at term equivalent and mothers’ levels of NICU-related stress (p=.005). Mothers in the high stress group had infants with MABS unsettled-irregular behavior scores that were 1.3–1.5 times higher than infants whose mothers were in the low and moderate stress groups. No other infant neonatal characteristics, including the more common clinical conditions associated with increased care needs and morbidity (e.g. lower gestational age and birth weight), were associated with higher maternal stress in the NICU.
In terms of maternal and family social background characteristics, lower maternal education (p=.03), higher levels of maternal postnatal depressive symptoms (p<.001), lower levels of parenting confidence (p=.002), and other previous life stressors (p<.001) were associated with higher levels of NICU-related stress. Of note, half of the mothers in the high stress group had not graduated from high school.
Predictors of Maternal Stress in the NICU
To identify which of the infant, maternal, and family social background factors made an independent contribution to the prediction of maternal stress in the NICU environment, a linear regression model was constructed with the total PSS: NICU score as the dependent variable. Forward and backward variable selection procedures were used to determine the best-fitting and most parsimonious model. The influence of infant clinical factors on parental stress perceptions were examined both individually and as a composite measure of neonatal risk (as described in the methods). Table 4 shows that the number of stressful life events in the last year (p=.01), lower maternal education (p=.06), higher maternal postnatal depressive symptoms (p=.001), and higher levels of infant unsettled-irregular behavior (p=.04) independently predicted overall maternal NICU-related stress, explaining 21.2% of the variance.
Table 4.
Final Fitted Regression Model for Prediction of Maternal Stress in the NICU
| Characteristic | Overall Maternal Stress |
Parental Role Alteration Stress |
||||
|---|---|---|---|---|---|---|
| B ± SE | β | p | B ± SE | β | p | |
| Infant characteristic | ||||||
| MABS unsettled-irregular score | 0.02 ± 0.01 | 0.17 | .04 | - | - | - |
| Maternal characteristic | ||||||
| EPDS postnatal depression score | 0.04 ± 0.01 | 0.28 | .001 | 0.05 ± 0.02 | 0.27 | .001 |
| Total stressful life events | 0.04 ± 0.01 | 0.21 | .01 | 0.04 ± 0.02 | 0.18 | .03 |
| Maternal education | −0.06 ± 0.03 | −0.15 | .06 | −0.14 ± 0.04 | −0.26 | .002 |
Note. B = Unstandardized Regression Coefficient; SE = Standard Error; β = Standardized Regression Coefficient.
A similar regression analysis was conducted with the PSS: NICU Parental Role Alteration score as the dependent variable. As shown in Table 4, higher maternal postnatal depression symptoms (p=.001), lower maternal education (p=.002), and the number of stressful life events in the last year (p=.03) each emerged as independent predictors of maternal stress associated with the loss of parental role. Jointly these variables accounted for 18.4% of the variance.
Maternal Stress in the NICU and Child Developmental Outcomes at Age 4 Years
Relations between the extent of maternal stress in the NICU and children's longer-term developmental outcomes were examined in a subsample (N=49) of study infants followed to corrected age 4 years. With the exception of twin births (p=.009) and maternal education (p=.02), no significant differences were found between this subsample and the total sample on any of the infant, maternal or family social background characteristics listed in Table 1. Infants with follow-up data were characterized by higher rates of twin births (43% vs. 21%) and lower rates of maternal high-school completion (41% vs. 20%).
As shown in Table 5, significant correlations were found between the extent of overall and parental role alteration stress at NICU discharge and later child language development and emotional symptoms. Children whose mothers experienced high levels of stress during their NICU stay were more likely to have lower scores on the CELF-P receptive (r=−.28 – −.31; p≤.04) and total language scales (r=−.25 – −.29; p≤.05) and higher scores on the emotional symptoms scale of the SDQ (r=.24–.28; p≤.05). These associations persisted after statistical control for maternal education, postnatal depression symptoms, and the number of other stressful life events in the year prior to childbirth.
Table 5.
Correlations between Maternal Stress in NICU and Child Developmental Outcomes at Age 4 years
| Child Developmental Outcomes (N=49) | Maternal PSS: NICU Score |
|||
|---|---|---|---|---|
| Overall Stress |
Parental Role Alteration Stress |
|||
| r | pa | r | pa | |
| Cognitive ability | ||||
| WPPSI-R total IQ score | −.06 | .35 | −.21 | .07 |
| Language developmentb | ||||
| CELF-P receptive language score | −.28 | .04 | −.31 | .02 |
| CELF-P expressive language score | −.17 | .14 | −.19 | .11 |
| CELF-P total language score | −.25 | .05 | −.29 | .03 |
| Emotional and behavioral adjustment | ||||
| SDQ emotional symptoms score | .28 | .03 | .24 | .05 |
| SDQ conduct problems score | .003 | .49 | −.06 | .33 |
| SDQ inattention/hyperactivity score | .004 | .49 | −.14 | .17 |
| SDQ peer relationship problems score | .13 | .19 | .14 | .17 |
| SDQ prosocial behavior score | −.07 | .32 | −.07 | .32 |
| SDQ overall behavioral difficulties score | .12 | .21 | .02 | .44 |
Significance testing for 1-tailed test.
Excludes 6 cases.
DISCUSSION
This study examined maternal perceptions of stress in the NICU after the birth of a VPT infant. Of specific interests were the sources of stress for mothers, the factors that placed mothers at risk of high NICU-related stress, and the influence of stress on the longer-term child outcomes. Methodological strengths of this study included the unselected nature of our regionally representative sample, high sample recruitment, and the use of well-validated measures of maternal psychological wellbeing, parenting confidence, and child outcomes. Key findings and their clinical implications are discussed below.
Overall, at term equivalent, mothers reported moderate levels of stress associated with their VPT infant's NICU hospitalization. The most stressful aspect of the NICU experience was their perceived loss of parental role and in particular being separated from their infant and feeling helpless and unable to protect their infant from pain and painful procedures. This is in line with previous research showing that irrespective of the time of parent report (within 5 days of admission, at discharge, 3 years later)12, 15, 28 or study design (qualitative vs. quantitative),1, 12, 15, 29 mothers of VPT born infants report the loss of their own role in the care of their infant as a primary source of NICU-related stress. This is important as intervention strategies tend to concentrate on reducing stress exposures for the infant patient,30, 31, 32, 33 but do not often address factors associated with parental and family stress that may potentially impede parental engagement and preparedness for parenting their baby at home.
Pregnancy is a time of both physical and psychological adjustment for parents, including the development and intensification of attachment to their new infant. This is a gradual process, such that by the end of nine months of pregnancy, parents develop a sense of readiness for their infant's birth and parenting.34 For parents of a preterm infant, this process is abruptly shortened, often leaving them with feelings of loss, grief, and anxiety alongside a desire to protect and care for their infant. Findings from this study highlight the need to care for the infant and parent as a family unit, and to actively involve parents in decision making and care of their infant so as to help mitigate feelings of powerlessness and avoidance which could potentially interfere with parental engagement, NICU visitation, and the formation of a secure parent-infant attachment.
The second study aim was to identify the infant, maternal, and family factors that place mothers at increased risk of high NICU stress to assist the delivery of individualized care. Unexpectedly, infant clinical characteristics such as extreme prematurity, birth weight, and severity of illness (examined as both individually and as a cumulative measure) were not related to the severity of mother's NICU-related stress. The only infant factor found to be important was the parent's perception of their infant's behavior, with mothers whose infants were characterized by high levels of unsettled and irritable behavior reporting more stress. These findings are consistent with mainstream attachment and early mother-infant interaction studies of typically developing and other high-risk groups and highlight the importance of creating opportunities for positive mother-infant interaction in the NICU.
Several other maternal and family factors were also associated with maternal stress. Mothers characterized by lower levels of educational achievement, stressful life events in the past year, and increased symptoms of early postnatal depression were at increased risk of high levels of NICU-related stress. Other studies have also linked low maternal education, family socioeconomic adversity, and early motherhood with increased stress.2, 11, 15, 32 Although the direction of the relationship between maternal mental health and NICU stress is unclear, results do indicate that those mothers who are most vulnerable to becoming distressed during their infant's NICU hospitalization are also facing significant challenges and stressors in their personal lives which are likely to impact not only their capacity to deal with their infant's high-risk birth, but also their own and infant's psychological wellbeing over time.
Preliminary analyses also suggest that higher levels of maternal stress in the NICU were associated with modest decreases in child receptive language and increases in child emotional adjustment problems four years following hospital discharge. These associations unlikely reflect low parent visitation since previous research based on our NICU population reveal high levels of maternal visitation (43 ± 16 hours per week) relative to other units.35 Mainstream developmental studies show that elevated maternal stress and anxiety, especially when persistent, can increase infant tendencies to anxiety and internalizing difficulties as well as having an adverse impact on mother-child relations that can further lead to increased parent-child anxiety.36, 37 Parents subject to high levels of stress and symptoms of depression are also less likely to interact with their infant, thus providing fewer opportunities for language development. 38, 39 There is also evidence that children with language delay may be at an increased risk of emotional and behavioral regulation difficulties and vice-versa. Irrespective of the nature of these relationships, current findings suggest the need for further studies examining the longer-term consequences of high levels of maternal NICU-related stress on parent-infant relations and child developmental outcomes in larger samples.
These findings have a number of implications for intervention efforts aimed at improving the psychological wellbeing of mothers of VPT infants. Screening mothers of high-risk newborns for post-traumatic stress, mental health problems and/or psychosocial adversity is likely to be an important first step in identifying those families who might benefit from additional support during their infant's NICU stay and as they transition home. Also, given that parental role alteration appears to be a major source of stress for many mothers, systematic efforts should be made by the neonatal clinical care team to include mothers and fathers in the care of their infant. Strategies such as Kangaroo Care and the use of audio-recorded maternal speech that have been shown to have clinical benefits for infants are also likely to be important in fostering a parent's sense of control and competence in tending to their infant. In addition, new interventions such as the Family Nature Intervention, which involve encouraging mother-infant sensory calming interaction inside and out of the isolette, show promise.40 Parental guidance on reading infant cues and demonstrating techniques for managing infant unsettled-irregular behavior at the bedside may not only ensure that mothers gain parenting confidence and an awareness of their important role in their child's life, but may also help to de-escalate stress. Closer to, and/or after discharge, parenting or mother-infant play groups focused on understanding the cues and behaviors of the preterm neonate may also be beneficial. Finally and importantly, findings also showed that maternal stress levels vary considerably according to the individual background characteristics of the mother and her infant, emphasizing the importance of individualized care.
Finally, several limitations should be acknowledged in the interpretation of study findings. First, maternal NICU-related stress was measured using self-report. It may be helpful in future studies to supplement these with biochemical measures of stress and also to potentially monitor stress over time rather than at a single retrospective time point. Second, the direction of the relationship between maternal mental health and severity of NICU stress remains unclear. Nonetheless findings do suggest that high levels of NICU stress place VPT infants at increased developmental risk over and above the effects of antenatal and postnatal depression. Third, detailed information about maternal complications during pregnancy or the severity of infant illness at the time of interview was not available. Therefore the extent to which these factors may also have contributed to mother's stress in the NICU could not be assessed.
In conclusion, this study shows that mothers experience varying degrees of stress related to their infants hospitalization in the NICU and that some mothers appear to be more vulnerable than others. Importantly, loss of parental role was perceived as the most stressful aspect of their infant's NICU hospitalization. Findings emphasize the need for routine screening of mothers of VPT infants for psychological wellbeing and psychosocial adversity during the postpartum period. To optimize mothers’ engagement in infant care, parental attachment, and a successful transition to home/follow-up care, it is recommended that parents are involved in infant care as much as possible and are fully informed about their infant's clinical needs and behavioral responses. Finally and importantly, this study highlights the need for further follow-up research to monitor the impact of maternal stress in the NICU and post-discharge on longer-term mother-infant adjustment and child developmental outcomes, particularly socio-emotional and language development.
ACKNOWLEDGEMENTS
Funding Source: Supported by grants from the Neurological Foundation of New Zealand (reference number: 0012/PG; 022/PG), the Health Research Council of New Zealand (reference number: 03/196), the Lottery Grants Board of New Zealand (reference number: AP84691), and the Washington University Intellectual and Developmental Disabilities Research Center (reference number: NIH/NICHD P30 HD062171).
Financial Disclosure: None of the authors have any financial relationship relevant to this study disclose.
Special thanks to Dr. Alessandra Raudino for her biostatistical advice and also to Michelle Davey, Jacqueline Ware, and Dr. Kelly Hood for their assistance with data collection. Most importantly, we would like to thank the families who supported and generously gave their time, free of charge, to the study.
Footnotes
Conflict of Interest: None of the authors have any conflict of interest relevant to this study to disclose.
REFERENCES
- 1.Holditch-Davis D, Miles MS. Mothers' stories about their experiences in the neonatal intensive care unit. Neonatal Netw. 2000;19(3):13–21. doi: 10.1891/0730-0832.19.3.13. [DOI] [PubMed] [Google Scholar]
- 2.Schappin R, Wijnroks L, Uniken Venema MM, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS One. 2013;8(2):e54992. doi: 10.1371/journal.pone.0054992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aucott S, Donohue PK, Atkins E, Allen MC. Neurodevelopmental care in the NICU. Ment Retard Dev Disabil Res Rev. 2002;8(4):298–308. doi: 10.1002/mrdd.10040. [DOI] [PubMed] [Google Scholar]
- 4.Clark CA, Woodward LJ, Horwood LJ, Moor S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: biological and social influences. Child Dev. 2008;79(5):1444–1462. doi: 10.1111/j.1467-8624.2008.01198.x. [DOI] [PubMed] [Google Scholar]
- 5.Frye RE, Malmberg B, Swank P, Smith K, Landry S. Preterm birth and maternal responsiveness during childhood are associated with brain morphology in adolescence. J Int Neuropsychol Soc. 2010;16(5):784–794. doi: 10.1017/S1355617710000585. [DOI] [PubMed] [Google Scholar]
- 6.Poehlmann J, Fiese BH. Parent-infant interaction as a mediator of the relation between neonatal risk status and 12-month cognitive development. Infant Behav Dev. 2001;24(2):171–188. [Google Scholar]
- 7.Treyvaud K, Anderson VA, Lee KJ, Woodward LJ, Newnham C, Inder TE, et al. Parental mental health and early social-emotional development of children born very preterm. J Pediatr Psychol. 2010;35(7):768–777. doi: 10.1093/jpepsy/jsp109. [DOI] [PubMed] [Google Scholar]
- 8.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kersting A, Dorsch M, Wesselmann U, Lüdorff K, Witthaut J, Ohrmann P, et al. Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. J Psychosom Res. 2004;57(5):473–476. doi: 10.1016/j.jpsychores.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Obeidat HM, Bond EA, Callister LC. The Parental Experience of Having an Infant in the Newborn Intensive Care Unit. J Perinat Educ. 2009;18(3):23–29. doi: 10.1624/105812409X461199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shields-Poë D, Pinelli J. Variables associated with parental stress in neonatal intensive care units. Neonatal Netw. 1997;16(1):29–37. [PubMed] [Google Scholar]
- 12.Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs. 1991;2(2):346–354. doi: 10.4037/15597768-1991-2022. [DOI] [PubMed] [Google Scholar]
- 13.Doering LV, Moser DK, Dracup K. Correlates of anxiety, hostility, depression, and psychosocial adjustment in parents of NICU infants. Neonatal Netw. 2000;19(5):15–23. doi: 10.1891/0730-0832.19.5.15. [DOI] [PubMed] [Google Scholar]
- 14.Cronin CM, Shapiro CR, Casiro OG, Cheang MS. The impact of very low-birth-weight infants on the family is long lasting. A matched control study. Arch Pediatr Adolesc Med. 1995;149(2):151–158. doi: 10.1001/archpedi.1995.02170140033005. [DOI] [PubMed] [Google Scholar]
- 15.Montirosso R, Provenzi L, Calciolari G, Borgatti R, Group N-AS Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 2012;101(2):136–142. doi: 10.1111/j.1651-2227.2011.02440.x. [DOI] [PubMed] [Google Scholar]
- 16.Woodward LJ, Clark CA, Bora S, Inder TE. Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PLoS One. 2012;7(12):e51879. doi: 10.1371/journal.pone.0051879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woodward LJ, Moor S, Hood KM, Champion PR, Foster-Cohen S, Inder TE, et al. Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch Dis Child Fetal Neonatal Ed. 2009;94(5):F339–344. doi: 10.1136/adc.2008.146282. [DOI] [PubMed] [Google Scholar]
- 18.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152. [PubMed] [Google Scholar]
- 19.Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49(6):608–615. doi: 10.1111/j.1365-2648.2004.03336.x. [DOI] [PubMed] [Google Scholar]
- 20.Brazelton TB, Nugent JK. Neonatal Behavioral Assessment Scale. 3rd edn. Vol. 137. Mac Keith Press; London: 1995. 3rd edn. [Google Scholar]
- 21.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 22.Navarro P, Ascaso C, Garcia-Esteve L, Aguado J, Torres A, Martín-Santos R. Postnatal psychiatric morbidity: a validation study of the GHQ-12 and the EPDS as screening tools. Gen Hosp Psychiatry. 2007;29(1):1–7. doi: 10.1016/j.genhosppsych.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 24.Elley WB, Irving JC. The Elley-Irving Socio-Economic Index: 2001 census revision. New Zeal J Educ Stud. 2003;38:3–17. [Google Scholar]
- 25.Wechsler Preschool and Primary Scale of Intelligence-Revised. The Psychological Corporation; San Antonio, TX: 1989. [Google Scholar]
- 26.Wiig EH, Secord W, Semel E. Clinical Evaluation of Language Fundamentals–Preschool: Examiner's Manual. The Psychological Corporation; New York: 1992. [Google Scholar]
- 27.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 28.Wereszczak J, Miles MS, Holditch-Davis D. Maternal recall of the neonatal intensive care unit. Neonatal Netw. 1997;16(4):33–40. [PubMed] [Google Scholar]
- 29.Affonso DD, Hurst I, Mayberry LJ, Haller L, Yost K, Lynch ME. Stressors reported by mothers of hospitalized premature infants. Neonatal Netw. 1992;11(6):63–70. [PubMed] [Google Scholar]
- 30.van der Pal SM, Maguire CM, le Cessie S, Wit JM, Walther FJ, Bruil J. Parental experiences during the first period at the neonatal unit after two developmental care interventions. Acta Paediatr. 2007;96(11):1611–1616. doi: 10.1111/j.1651-2227.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 31.Fleisher BE, VandenBerg K, Constantinou J, Heller C, Benitz WE, Johnson A, et al. Individualized developmental care for very-low-birth-weight premature infants. Clin Pediatr (Phila) 1995;34(10):523–529. doi: 10.1177/000992289503401003. [DOI] [PubMed] [Google Scholar]
- 32.Turan T, Başbakkal Z, Ozbek S. Effect of nursing interventions on stressors of parents of premature infants in neonatal intensive care unit. J Clin Nurs. 2008;17(21):2856–2866. doi: 10.1111/j.1365-2702.2008.02307.x. [DOI] [PubMed] [Google Scholar]
- 33.Als H, Gilkerson L, Duffy FH, McAnulty GB, Buehler DM, Vandenberg K, et al. A three-center, randomized, controlled trial of individualized developmental care for very low birth weight preterm infants: medical, neurodevelopmental, parenting, and caregiving effects. J Dev Behav Pediatr. 2003;24(6):399–408. doi: 10.1097/00004703-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Brazelton T, Cramer B. The earliest relationship: Parents, infants and the drama of early attachment. Karnac books; 2012. [Google Scholar]
- 35.Ichijima E, Kirk R, Hornblow A. Parental support in neonatal intensive care units: a cross-cultural comparison between New Zealand and Japan. J Pediatr Nurs. 2011;26(3):206–215. doi: 10.1016/j.pedn.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 36.Apter-Levy Y, Feldman M, Vakart A, Ebstein RP, Feldman R. Impact of maternal depression across the first 6 years of life on the child's mental health, social engagement, and empathy: The moderating role of oxytocin. Am J Psychiatry. 2013;170(10):1161–1168. doi: 10.1176/appi.ajp.2013.12121597. [DOI] [PubMed] [Google Scholar]
- 37.Giallo R, Cooklin A, Wade C, D'Esposito F, Nicholson JM. Maternal postnatal mental health and later emotional-behavioural development of children: the mediating role of parenting behaviour. Child Care Health Dev. 2013 doi: 10.1111/cch.12028. [DOI] [PubMed] [Google Scholar]
- 38.Topol D, Girard N, St Pierre L, Tucker R, Vohr B. The effects of maternal stress and child language ability on behavioral outcomes of children with congenital hearing loss at 18-24months. Early Hum Dev. 2011;87(12):807–811. doi: 10.1016/j.earlhumdev.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 39.Quittner AL, Barker DH, Cruz I, Snell C, Grimley ME, Botteri M, et al. Parenting Stress among Parents of Deaf and Hearing Children: Associations with Language Delays and Behavior Problems. Parent Sci Pract. 2010;10(2):136–155. doi: 10.1080/15295190903212851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Welch MG, Hofer MA, Brunelli SA, Stark RI, Andrews HF, Austin J, et al. Family nurture intervention (FNI): methods and treatment protocol of a randomized controlled trial in the NICU. BMC Pediatr. 2012;12:14. doi: 10.1186/1471-2431-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]