Abstract
Objectives:
To explore the role that virtual reality training might play in the learning curve of laparoscopic varicocelectomy.
Methods:
A total of 1326 laparoscopic varicocelectomy cases performed by 16 participants from July 2005 to June 2012 were retrospectively analyzed. The participants were divided into 2 groups: group A was trained by laparoscopic trainer boxes; group B was trained by a virtual reality training course preoperatively. The operation time curves were drafted, and the learning, improving, and platform stages were divided and statistically confirmed. The operation time and number of cases in the learning and improving stages of both groups were compared. Testicular artery sparing failure and postoperative hydroceles rate were statistically analyzed for the confirmation of the learning curve.
Results:
The learning curve of laparoscopic varicocelectomy was 15 cases, and with 14 cases more, it came into the platform stage. The number of cases for the learning stages of both groups showed no statistical difference (P = .49), but the operation time of group B for the learning stage was less than that of group A (P < .00001). The number of cases of group B for the improving stage was significantly less than that of group A (P = .005), but the operation time of both groups in the improving stage showed no difference (P = .30). The difference of testicular artery sparing failure rates among these 3 stages was proved significant (P < .0001), the postoperative hydroceles rate showed no statistical difference (P = .60).
Conclusions:
The virtual reality training shortened the operation time in the learning stage and hastened the trainees' steps in the improving stage, but did not shorten the learning curve as expected to.
Keywords: Laparoscopic varicocelectomy, Learning curve, Varicocele, Virtual reality training
INTRODUCTION
Laparoscopic varicocelectomy was first introduced as an efficient treatment for male infertility in 1992.1–4 Within more than 2 decades, this laparoscopic procedure has evolved into superior techniques such as robot-assisted,5 lymphatic sparing,6 and single-port7 laparoscopic varicocelectomies. Recent published articles have been focused on issues such as laparoscopic varicocelectomy for adolescents,8 comparison of the outcomes of different varicocelectomy techniques,9 observation,10 and prevention11 of the postoperative hydroceles. Though early literatures argued the importance of a learning curve in laparoscopic procedures12,13 and the important training role the laparoscopic varicocelectomy might play in the future urologic laparoscopic procedures,14 the learning curve of laparoscopic varicocelectomy still remained unclear. Thus, we retrospectively analyzed 1326 cases of laparoscopic varicocelectomy performed by 16 participants from July 2005 to June 2012, through which the learning curve of laparoscopic varicocelectomy was demonstrated and statistically confirmed by strong support of the large sample size. Interestingly, during these analyses, we discovered that virtual reality training for the participants played an unexpected role in the learning curve of laparoscopic varicocelectomy.
MATERIALS AND METHODS
Participants and Preoperative Training
Sixteen participants were recruited in this study, all of them were male residents (postgraduate years 3 and 4), and laparoscopic varicocelectomy was the first laparoscopic procedure they performed independently. In the preoperative training courses, 8 participants trained in our center from July 2005 to September 2008, accomplished a 5-step (hand-eye coordination, clipping, disk cutting, knots tying, and suturing on catheter) 4 week (1 hour daily) training course using the self-contained laparoscopic trainer boxes. Eight participants trained in our center from October 2008 to June 2012, accomplished a 4-step (eye-hand coordination, object placement, clipping, and cutting) 4 week (1 hour daily) virtual reality (VR) training course, using Simbionix LAP Mentor (Cleveland, Ohio), which has been serving clinical training since October 2008. In data collecting and statistical analyses, the clinical data of 8 participants trained by the laparoscopic trainer boxes were defined as group A, and the other 8 participants trained by the VR training course were defined as group B.
Operative Procedures
All cases of laparoscopic varicocelectomy were performed by the testicular artery sparing technique.15,16 All tissues except the testicular artery were ligated and divided using sutures and scissors but not titanium clips or LigaSure device (Covidien, Mansfield, Massachusetts), considering the cost-effectiveness (Figure 1).
Figure 1.
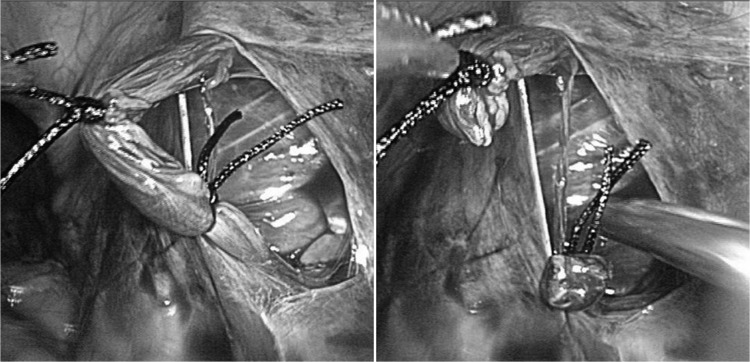
The testicular artery was dissociated and confirmed, and the suture ligations were done. Then the rest of the tissues of spermatic cord were divided and the testicular artery was well preserved.
Data Collection
All clinical data of the laparoscopic varicocelectomy cases from July 2005 to June 2012 were collected from the electronic medical records database. All bilateral procedures were included, unilateral procedures were excluded, and all procedures were consecutively performed as described in the preceding sections by the participants from their first case. The clinical data of operation time (interval from skin incision to skin closure), bleeding complications, artery sparing failure rate, postoperative hydrocele rate, testicular atrophy rate, and recurrence rate were collected and calculated. Based on our previous study,17 operation time was used as the key parameter for demonstrating the learning curve, and the operation time of all cases, was first extracted from the data pool into an Excel spreadsheet (Microsoft, Seattle, Washington) to illustrate the learning curves. The first 12 months' follow-up data were extracted and the sample size and number of participants were considered.
Learning Curve and Statistical Analyses
The learning curve of laparoscopic varicocelectomy was confirmed through 3 steps. The operation time curve of each participant was first drafted by Excel and 3 stages of operation time curves were observed and divided by the steep decline points, from which stages 1 to 3 were named as the learning stage, improving stage, and platform stage, respectively. Then the statistical analyses were performed to confirm the differences of operation time among these 3 stages. The differences of artery sparing failure rate and hydrocele rate among these 3 stages were evaluated the by additional statistical analyses, which then finally confirmed the learning curve of laparoscopic varicocelectomy.
Statistical analyses were performed using Stata 12.0 software (StataCorp, College Station, Texas). Data were evaluated by the t test, Cochran-Mantel-Haenszel (CMH) test, and Pearson χ2 test. P < .05 was considered significant in all analyses.
RESULTS
Parameters and Complications
The clinical data of 1326 bilateral laparoscopic varicocelectomy cases were finally collected, in which the first 12 months' follow-up data of 932 cases qualified for these analyses. The operation time of all cases, 85 artery sparing failure cases, and 76 postoperative hydrocele cases were recorded and statistically analyzed as parameters for the learning curve. Three postoperative blood transfusion cases (0.32%) due to the umbilical trocar wound bleeding, 5 postoperative single side testicular atrophy cases (0.54%) due to the testicular artery sparing failure, and 15 left side recurrence cases (1.61%) performed by 11 different participants were recorded, but they were not statistically analyzed because of the limited number.
Operation Time Curve
In the operation time curve of participant 1, as Figure 2 shows, 2 sharp decreasing points (the 12th case and the 27th case) were marked and demonstrated how these 3 stages divided. By the same method, Figure 3 demonstrated operation time curves of all participants in both groups, from which the learning stage, improving stage, and platform stage were clearly drafted and statistically proved (P < .05). Table 1 lists the exact number in the 3 stages for each participant. Statistical analyses confirmed the average number of learning stage cases was 15.06, and with the average of 14.44 cases more, the learning curve went into platform stages.
Figure 2.
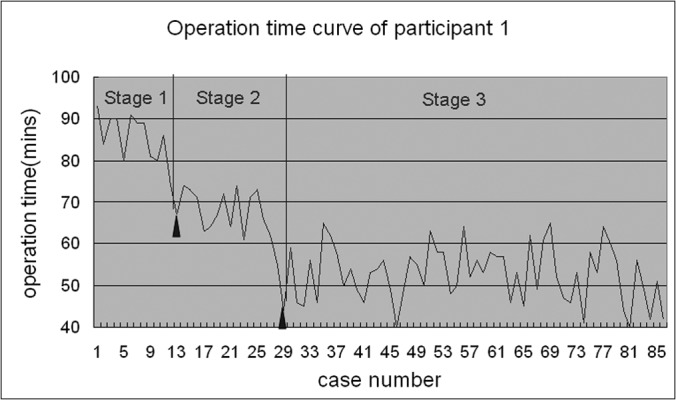
This operation time curve of participant 1 clearly showed 2 sharp decline points (triangles ▴ point to the 12th case and the 27th case), which divided the learning, improving, and platform stages, which were later proved by statistical analyses.
Figure 3.
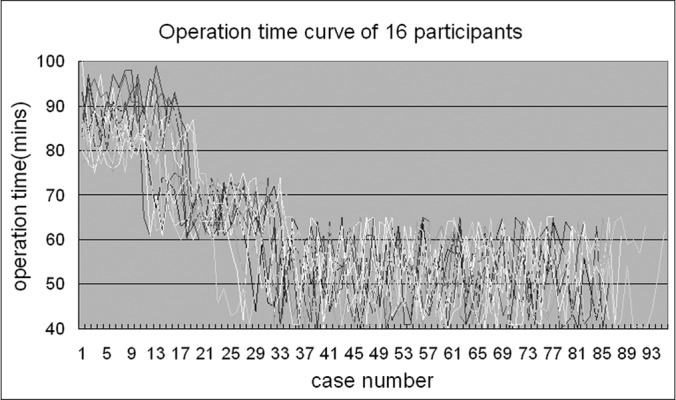
These curves were drafted by all operation time data for the 16 participants of both groups, which visually showed there were 3 stages in the curves, not 2 stages as was previously thought.
Table 1.
The Number of Cases for the Learning, Improving, and Platform Stages of Each Participant
| Participants | Performed Cases | Learning Stage | Improving Stage | Platform Stage |
|---|---|---|---|---|
| 1 | 86 | 11 | 16 | 59 |
| 2 | 72 | 16 | 16 | 40 |
| 3 | 77 | 14 | 16 | 47 |
| 4 | 92 | 13 | 18 | 61 |
| 5 | 82 | 10 | 17 | 55 |
| 6 | 81 | 18 | 15 | 48 |
| 7 | 75 | 17 | 14 | 44 |
| 8 | 87 | 17 | 15 | 55 |
| 9 | 84 | 14 | 11 | 59 |
| 10 | 75 | 19 | 15 | 41 |
| 11 | 88 | 19 | 14 | 55 |
| 12 | 86 | 11 | 12 | 63 |
| 13 | 73 | 14 | 12 | 47 |
| 14 | 87 | 19 | 16 | 52 |
| 15 | 86 | 17 | 14 | 55 |
| 16 | 95 | 12 | 10 | 73 |
| Total:1326 | Average:15.06 ± 3.09 | Average:14.44 ± 2.22 |
As Table 2 shows, in the learning stage, the operation time of group B was statistically shorter than that of group A (P < .00001), but the number of cases for the learning stages of both groups was not significantly different (P = .49). However, in the improving stage, the difference of operation time in both groups was no more significant (P = .29), though the participants in group B had experienced fewer cases than did those in group A in the improving stages (P = .005). When the participants in both groups went into the platform stages, the operation time and the number of cases were not statistically different (P = .27 and 0.32, respectively).
Table 2.
The Comparison of Average Operation Time and Number of Cases for Groups A and B in Learning and Improving Stages
| Group | Learning Stage |
Improving Stage |
||||||
|---|---|---|---|---|---|---|---|---|
| Operation Time, min |
Cases, n |
Operation Time, min |
Cases, n |
|||||
| A | B | A | B | A | B | A | B | |
| 86.6 | 83.1 | 11 | 14 | 68.5 | 69.4 | 16 | 11 | |
| 88.6 | 83.2 | 16 | 19 | 67.7 | 66.5 | 16 | 15 | |
| 88.7 | 82.6 | 14 | 19 | 65.1 | 69.1 | 16 | 14 | |
| 86.5 | 80.2 | 13 | 11 | 68.8 | 68.5 | 18 | 12 | |
| 88.3 | 82.5 | 10 | 14 | 66.9 | 68 | 17 | 12 | |
| 90.8 | 81.6 | 18 | 19 | 65.4 | 66.4 | 15 | 16 | |
| 90.9 | 79.9 | 17 | 17 | 68.2 | 68.5 | 14 | 14 | |
| 88.7 | 81.3 | 17 | 12 | 65.7 | 66.1 | 15 | 10 | |
| Average | 88.6 ± 1.6 | 81.8 ± 1.3 | 14.5 ± 2.9 | 15.6 ± 3.3 | 67.04 ± 1.48 | 67.81 ± 1.29 | 15.88 ± 1.25 | 13 ± 2.07 |
| p Value | <0.00001 | 0.4852 | 0.2967 | 0.0046 | ||||
Testicular Artery Sparing Failure Rate
Table 3 lists the testicular artery sparing failure number and rate in the learning, improving, and platform stages. Statistical analyses showed significant difference of testicular artery sparing failure rate among these 3 stages (P < .0001), which directly proved the validity of the learning curve concluded by operation time. Further statistical analyses did not find any difference of testicular artery sparing failure rate between groups A and B in any of these 3 stages (P = .46, .58, and .52, respectively).
Table 3.
The Testicular Artery Sparing Failure Number and Rate in the Learning, Improving, and Platform Stages
| Learning Stage |
Improving Stage |
Platform Stage |
Total |
|||||
|---|---|---|---|---|---|---|---|---|
| Failures, n | Spared, n | Failures, n | Spared, n | Failures, n | Spared, n | Failures, n | Spared, n | |
| Group A | 18 | 98 | 10 | 117 | 13 | 396 | 41 | 611 |
| Group B | 21 | 104 | 8 | 96 | 15 | 430 | 44 | 630 |
| Total | 39 | 202 | 18 | 213 | 28 | 826 | 85 | 1241 |
| Failure rate, % | 16.18 | 7.79 | 3.28 | 6.41 | ||||
Postoperative Hydroceles Rate
Table 4 shows postoperative hydroceles number and rate in the learning, improving, and platform stages, which gradually decreased from 9.69% to 9.09% to 7.47%. Statistical analyses showed no significant difference of postoperative hydroceles rate among these 3 stages (P = .60), nor between groups A and B in any of these 3 stages (P = .49, .60, and .51, respectively).
Table 4.
The Postoperative Hydroceles Number and Rate in the Learning, Improving, and Platform Stages
| Learning Stage | Improving Stage | Platform Stage | Total | |
|---|---|---|---|---|
| Group A | 9/87 | 9/105 | 17/234 | 35 |
| Group B | 10/109 | 7/82 | 24/315 | 41 |
| Total | 19/196 | 16/187 | 41/549 | 76/932 |
| Hydrocele rate, % | 9.69 | 9.09 | 7.47 | 8.15 |
DISCUSSION
Laparoscopic varicocelectomy has been accepted as a safe and cost-effective technique for the treatment of varicocele,18 which is one of the most common causes of male infertility.19 Nowadays, this technique has been updated to various fashion styles, as we described earlier. Almost all advantages and disadvantages of this technique have been researched and reported.20 However, the learning curve of this simple laparoscopic varicocelectomy is still not clearly declared with convincing data, even it has been performed for >20 years around the world. Curiously, the learning curve study now seems to be in an awkward situation; urologists prefer reporting the learning curve of senior laparoscopic procedures, such as robot-assisted laparoscopic radical prostatectomy21 or laparoscopic pyeloplasty22 with a few participants and limited cases. Laparoscopic varicocelectomy procedure, containing and requesting precise incision, ligation, or even suture under the laparoscope, would play a very important role in training future laparoscopic urologists. The trainer boxes or virtual reality simulators would never simulate the individualized situation encountered in the real procedures, so would only ease the learning courses. So the learning curve data of this procedure is essential for all the trainees or novice surgeons. With the accumulation of cases in the last 7 years, this study retrospectively analyzed 1326 laparoscopic varicocelectomy cases with the initial purpose of demonstrating the exact learning curve of this technique.
In the study design, we supposed the learning curve of laparoscopic varicocelectomy would be a curve gradually decreasing into a platform. However, when the operation time data of a participant drafted, as Figure 2 shows, 2 steep decreasing points were observed, and the data were divided into 3 stages. By statistical analyses, the difference of operation time under the learning, improving, and platform stages was confirmed. With more caution, the operation time curves of all 16 participants were drafted and analyzed by same methods, and the 3 stages could be visualized this time too.
With further statistical analyses on testicular artery sparing failure rate and postoperative hydroceles rate, the validity of the learning curve was confirmed; the average number of cases for these 16 participants under the learning stages was 15. As far as we know, the learning curve of laparoscopic varicocelectomy has never been reported with such a large number of cases and participants.
During the data collection and statistical analyses, the variety of the number of cases and operation time of different participants for the learning curve was noticed, and the reason was initially explained as the differences of participants' “surgical talent.” However, when the participants' preoperational basic laparoscopic training courses were retrospectively rechecked, we found some of them were trained by a standard training course using the VR simulator, whereas others were trained by self-contained laparoscopic trainer boxes. Thus, we expanded the enrollment list and the data pool, from which the operational data of 16 participants were finally extracted, grouped, and compared by the difference of preoperative training courses.
As the data in Table 2 shows, the number of cases for the learning stage showed no statistical difference between these 2 groups, but the average operation time of group B was significantly shorter than that of group A. Then further analyses were made in the improving stages of both groups, which interestingly showed that the participants in group B experienced fewer cases than those in group A before they went into the platform stages, but the average operation time in the improving stage of both groups was not statistically different. So the standard VR simulator training courses did help the trainees by decreasing their operation time in the learning stage and speeding up their improving stage of the laparoscopic varicocelectomy, but the VR simulator training did not shorten the learning curve as we expected.
Actually, ligation of spermatic cord tissues was a time-consuming procedure. Ligation under the laparoscope could hardly be simulated by the VR training courses even with the help of force feedback system, but was well trained by the laparoscopic trainer boxes. Therefore, these results complemented the common sense that VR training would be inherently better than laparoscopic training boxes only in given circumstances. Each training method has its own advantages.
In this study, operation time was the key parameter for demonstrating the learning curve, and testicular artery sparing failure, as another parameter, proved its validity. Postoperative hydroceles rate, though analyzed with sufficient cases provided by follow-up data, only showed a gradually decreased trend, but was not statistically significant in these 3 stages, suggesting the postoperative hydroceles rate would be affected by >1 factor (follow-up data bias, individual skills, and testicular artery sparing technique itself would be others). Further discussion would be beyond the focus of this study.
CONCLUSIONS
By retrospective analyses of 1326 laparoscopic varicocelectomy cases performed by 16 participants, this study clearly demonstrated the learning curve of this technique was 15 cases. More interestingly, the participants trained by VR simulator experienced less mean operation time in the learning stages and fewer cases in the improving stages comparing with those who trained by self-contained laparoscopic trainer boxes. But the VR simulator training did not shorten the learning curve as we expected it to.
Contributor Information
Zheng Wang, Minimally Invasive Urology Center, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
Yuhua Ni, Department of Healthcare, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
Yinan Zhang, Minimally Invasive Urology Center, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
Xunbo Jin, Minimally Invasive Urology Center, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
Qinghua Xia, Minimally Invasive Urology Center, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
Hanbo Wang, Minimally Invasive Urology Center, Provincial Hospital Affiliated to Shandong University, Jinan, Shandong Province, China..
References:
- 1. Hagood PG, Mehan DJ, Worischeck JH, Andrus CH, Parra RO. Laparoscopic varicocelectomy: preliminary report of a new technique. J Urol. 1992;147(1):73–76 [DOI] [PubMed] [Google Scholar]
- 2. Matsuda T, Horii Y, Higashi S, Oishi K, Takeuchi H, Yoshida O. Laparoscopic varicocelectomy: a simple technique for clip ligation of the spermatic vessels. J Urol. 1992;147(3):636–638 [DOI] [PubMed] [Google Scholar]
- 3. Winfield HN, Donovan JF. Laparoscopic varicocelectomy. Semin Urol. 1992;10(3):152–160 [PubMed] [Google Scholar]
- 4. Mehan DJ, Andrus CH, Parra RO. Simultaneous laparoscopic varicocelectomy and removal of an intrascrotal atrophic testicle. Surg Laparosc Endosc. 1992;2(4):327–331 [PubMed] [Google Scholar]
- 5. Corcione F, Esposito C, Cuccurullo D, et al. Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc. 2005;19(1):117–119 [DOI] [PubMed] [Google Scholar]
- 6. Kocvara R, Dvorácek J, Sedlácek J, Díte Z, Novák K. Lymphatic sparing laparoscopic varicocelectomy: a microsurgical repair. J Urol. 2005;173(5):1751–1754 [DOI] [PubMed] [Google Scholar]
- 7. Kaouk JH, Palmer JS. Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int. 2008;102(1):97–99 [DOI] [PubMed] [Google Scholar]
- 8. Waalkes R, Manea IF, Nijman JM. Varicocele in adolescents: a review and guideline for the daily practice. Arch Esp Urol. 2012;65(10):859–871 [PubMed] [Google Scholar]
- 9. Sun HB, Liu Y, Yan MB, Li ZD, Gui XG. Comparing three different surgical techniques used in adult bilateral varicocele. Asian J Endosc Surg. 2012;5(1):12–16 [DOI] [PubMed] [Google Scholar]
- 10. Nees SN, Glassberg KI. Observations on hydroceles following adolescent varicocelectomy. J Urol. 2011;186(6):2402–2407 [DOI] [PubMed] [Google Scholar]
- 11. Chiarenza SF, Giurin I, Costa L, et al. Blue patent lymphography prevents hydrocele after laparoscopic varicocelectomy: 10 years of experience. J Laparoendosc Adv Surg Tech A. 2012;22(9):930–933 [DOI] [PubMed] [Google Scholar]
- 12. Soulie M, Seguin P, Richeux L, et al. Urological complications of laparoscopic surgery: experience with 350 procedures at a single center. J Urol. 2001;165(6 Pt 1):1960–1963 [PubMed] [Google Scholar]
- 13. Janetschek G, Marberger M. Laparoscopic surgery in urology. Curr Opin Urol. 2000;10(4):351–357 [DOI] [PubMed] [Google Scholar]
- 14. Salas Cabrera R, Ramírez Torres C, Sagué Larrea J, Laurencio Mena A. Laparoscopic varicocelectomy in the adult patient [in Spanish]. Arch Esp Urol. 2008;61(7):815–818 [DOI] [PubMed] [Google Scholar]
- 15. Cohen RC. Laparoscopic varicocelectomy with preservation of the testicular artery in adolescents. J Pediatr Surg. 2001;36(2):394–396 [DOI] [PubMed] [Google Scholar]
- 16. Tu D, Glassberg KI. Laparoscopic varicocelectomy. BJU Int. 2010;106(7):1094–1104 [DOI] [PubMed] [Google Scholar]
- 17. Zhang YN, Xia QH, Wang Z. The learning curve of laparoscopic varicocele ligation. J Urol Clin. 2011;3:15–17 [Google Scholar]
- 18. Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011;108(7):1157–1172 [DOI] [PubMed] [Google Scholar]
- 19. Chan P. Management options of varicoceles. Indian J Urol. 2011;27(1):65–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ding H, Tian J, Du W, Zhang L, Wang H, Wang Z. Open non-microsurgical, laparoscopic or open microsurgical varicocelectomy for male infertility: a meta-analysis of randomized controlled trials. BJU Int. 2012;110(10):1536–1542 [DOI] [PubMed] [Google Scholar]
- 21. Ploussard G, Salomon L, Parier B, Abbou CC, de la Taille A. Extraperitoneal robot-assisted laparoscopic radical prostatectomy: a single-center experience beyond the learning curve. World J Urol. 2013;31(3):447–453 [DOI] [PubMed] [Google Scholar]
- 22. Zhu H, Shen C, Li X, et al. Laparoscopic pyeloplasty: a comparison between the transperitoneal and retroperitoneal approach during the learning curve. Urol Int. 2013;90(2):130–135 [DOI] [PubMed] [Google Scholar]


