Abstract
Background and Objectives:
Mesh fixation during laparoscopic totally extraperitoneal repair is thought to be necessary to prevent recurrence. However, mesh fixation may increase postoperative chronic pain. This study aimed to describe the experience of a single surgeon at our institution performing this operation.
Methods:
We performed a retrospective review of the medical records of all patients who underwent bilateral laparoscopic totally extraperitoneal repair without mesh fixation for inguinal hernia from January 2005 to December 2011. Demographic, operative, and postoperative data were obtained for analysis.
Results:
A total of 343 patients underwent simultaneous bilateral laparoscopic totally extraperitoneal repair of 686 primary and recurrent inguinal hernias from January 2005 to December 2011. The mean operative time was 33 minutes. One patient was converted to an open approach (0.3%), and 1 patient had intraoperative bladder injury. Postoperative hematoma/seroma occurred in 5 patients (1.5%), wound infection in 1 (0.3%), hematuria in 2 (0.6%), and acute myocardial infarction in 1 (0.3%). Chronic pain developed postoperatively in 9 patients (2.6%); 3 of them underwent re-exploration. All patients were discharged home a few hours after surgery except for 3 patients. Among the 686 hernia repairs, there were a total of 20 recurrences (2.9%) in 18 patients (5.2%). Two patients had bilateral recurrences, whereas 16 had unilateral recurrences. Twelve of the recurrences occurred after 1 year (60%). Fourteen recurrences occurred among direct hernias (70%).
Conclusion:
Compared with the literature, our patients had fewer intraoperative and postoperative complications, less chronic pain, and no increase in operative time or length of hospital stay but had a slight increase in recurrence rate.
Keywords: Bilateral, Laparoscopic, TEP, Mesh fixation
INTRODUCTION
Inguinal hernia repair is one of the most common procedures in the field of general surgery. Various methods for inguinal hernia repair have been described. Tension-free repair is the procedure type of choice because of its low recurrence rate.1 Tension-free repair procedures can be roughly categorized into 2 groups based on the approach: laparoscopic and open anterior. The main indications for the laparoscopic approach are bilateral and recurrent inguinal hernias.2 Despite the fact that recent trials3–5 and meta-analyses6,7 have confirmed that laparoscopic inguinal hernia repair is at least comparable with open surgery in overall outcome and may even be superior in terms of recovery, this procedure has yet to gain acceptance worldwide. Which technique is superior remains debatable. The debate centers on costs, the steep learning curve, possible major complications, and the need for general anesthesia.
Laparoscopic hernia repair can be performed by either a total extraperitoneal (TEP) approach or transabdominal preperitoneal approach. TEP repair is gaining popularity because many surgeons have become wary of the potential complications when entering the peritoneal cavity using the transabdominal approach. TEP repair has shown favorable short-term results with regard to reduced postoperative stay, decreased postoperative pain, and earlier return to physical activity in comparison with open mesh repairs.8 Postoperative groin pain is still a concern in approximately one fifth of patients after TEP repair.9–11 Though generally mild and nonlimiting, it can be severe in a small percentage of patients who may seek help from chronic pain specialists and have significant occupational difficulties.12
The common practice of using staples or tacks to fixate mesh to the groin has been implicated as a possible cause of postoperative pain based on numerous reports of new groin pain that is well localized, corresponds with the location of fixation tacks, and is ameliorated by their removal.13 On the other hand, there is an entrenched belief within the surgical community that mesh fixation is a vital step in the repair to reduce the risk of mesh folding or migration that could lead to early hernia recurrence. In this study we describe the experience of a single surgeon at our institution performing bilateral laparoscopic TEP repair without mesh fixation with regard to operative time, length of hospital stay, and intraoperative and postoperative complications, particularly chronic pain and recurrence.
METHODS
With the approval of the Kaiser Permanente Institutional Review Board, we performed a retrospective analysis of the medical records of all patients who underwent bilateral laparoscopic TEP repair without mesh fixation at our institution by a single staff surgeon (F.Y.) for inguinal hernia from January 2005 to December 2011. Patient demographic characteristics (age, sex, and race), body mass index (BMI), American Society of Anesthesiologists physical status class, hernia types, indication for surgery, operative time, other surgical procedures performed during the operation, intraoperative complications and postoperative complications including chronic pain, hospital length of stay, and recurrence were all collected retrospectively from patient electronic medical records and the computerized operating room database.
Laparoscopic repair is offered to all patients with no contraindications to general anesthesia who present with recurrent or bilateral inguinal hernia. All operations were elective. A combined hernia was defined as any 2 or more hernia types combined on one side. The operative time was defined as the time from skin incision to skin closure. The length of hospital stay was defined as the total number of nights spent in the hospital after the operation. Chronic pain was defined as continuous pain for >3 months after inguinal hernia repair, the period regarded as the normal tissue-healing time. All patients were contacted by telephone 1 week after surgery. Patients with complaints or indications of a suspected recurrence were asked to return to the clinic and were followed up regularly at the outpatient clinic. We used the last recorded follow-up data for our statistical analysis.
Surgical Technique
Surgery was performed with the patient under general anesthesia by the standard 3-port operative technique. The senior author was present as the lead surgeon in all cases. A single dose of a first-generation cephalosporin was used for prophylaxis. To create the preperitoneal space, a 12-mm skin incision is made below the umbilicus, and it is carried down to the anterior rectus sheath. The anterior rectus sheath is identified, and then a small horizontal incision is made on the anterior rectus sheath on the side of the larger hernia. By use of a small blunt hook, the fibers of the rectus abdominis muscle are retracted laterally, exposing the posterior layer of the rectus sheath. A channel between the rectus muscle and the posterior rectus sheath is created by inserting a space maker with advancement toward the pubic tubercle. A dissecting balloon is then inserted, inflated under direct vision, and removed. The preperitoneal space is insufflated with carbon dioxide. Pressure is maintained at 12 to 15 mm Hg by continuous insufflation of carbon dioxide. The preperitoneal space is then entered by a 0°, 10-mm telescope. Two 5-mm ports are inserted under direct vision, one at 2 cm above the symphysis pubis in the midline and the other at the midline between the previous 2 ports. Blunt dissection of the hernia sac is performed, exposing the spermatic cord/round ligament and all inguinofemoral hernia orifices. Dissection of the contralateral side is performed through the ipsilateral access, with no need to place further trocars. To avoid adhesions, peritoneal holes that occur intraoperatively are closed endoscopically. After dissection of the inguinal region, reduction of the hernia sac, and parietalization of the spermatic cord have been completed, two 15×10–cm polyester meshes are inserted and used to cover all potential hernia orifices on both sides with 1 to 2 cm of overlap in the midline above the pubic symphysis. At our institution, polyester mesh is available in 1 size (15×10 cm); however, the mesh is trimmed when needed (usually in smaller patients). The meshes are left without any form of fixation. The patients are transferred to the recovery room and are observed for a few hours before being discharged home.
RESULTS
From January 2005 to December 2011, a total of 343 patients underwent bilateral laparoscopic TEP repair of 686 primary and recurrent inguinal hernias performed by a single staff surgeon at our institution. The median follow-up period was 49 months (range, 6–88 months). The mean patient age was 52 years (range, 17–87 years). Male patients were predominant (96%). Most patients were white (65%). The American Society of Anesthesiologists physical status class was 1 in 26% of patients, 2 in 71%, and 3 in 3%. On the basis of BMI classification, 30% of patients had a normal body weight, 46% were overweight, and 24% were obese (Table 1).
Table 1.
Demographic Characteristics
| Data | |
|---|---|
| No. of patients | 343 |
| No. of hernias | 686 |
| Age [mean (range)] (y) | 52 (17–87) |
| Sex [n (%)] | |
| Male | 330 (96%) |
| Female | 13 (4%) |
| Race [n (%)] | |
| White | 223 (65%) |
| Black | 20 (6%) |
| Hispanic | 60 (17%) |
| Asian | 19 (6%) |
| Other/unknown | 21 (6%) |
| Mean ASAa class | 2 |
| ASA class [n (%)] | |
| 1 | 88 (26%) |
| 2 | 243 (71%) |
| 3 | 12 (3%) |
| Mean BMI | 27.4 |
| BMI [n (%)] | |
| <25 | 98 (29%) |
| 25–30 | 166 (48%) |
| 30–35 | 61 (18%) |
| >35 | 18 (5%) |
ASA = American Society of Anesthesiologists.
Perioperative data are summarized in Table 2. The indication for bilateral TEP repair was the presence of a bilateral primary hernia in 81% of patients, unilateral recurrent hernia in 13%, and bilateral recurrent hernia in 6%. A direct hernia was the predominant type of hernia (60%). Of the remaining hernias, 20% were indirect, 2% were femoral, and 18% were combined. The mean operative time was 33 minutes (range, 17–102 minutes). Other surgical procedures performed along with inguinal hernia repair were umbilical hernia repair in 72 patients (20%), neurectomy in 1 (0.3%), bilateral vasectomy in 4 (1.2%), and lipoma excision in 2 (0.6%). Another patient with a known history of an undescended testicle underwent orchiectomy after the undescended testicle was found in the hernia sac. Regarding intraoperative complications, only 1 patient had intraoperative bladder injury (0.3%) and 1 patient (0.3%) was converted to an open approach because of contracted mesh that extended into the preperitoneal space and was not able to be removed laparoscopically. All patients were discharged on the same day of the surgery except for 3 patients who were admitted to the hospital postoperatively. In the first patient dizziness and syncope developed postoperatively, and further workup showed acute myocardial infarction. The second patient was noted to have blood in the urine intraoperatively, likely due to traumatic urinary catheter insertion, and was discharged the next day after bladder irrigation. The last patient was admitted for 1 night and was discharged home the next day, but we could not identify the reason for the admission from the medical records.
Table 2.
Perioperative Data
| Data | |
|---|---|
| Indication for surgery [n (%)] | |
| Bilateral primary hernia | 278 (81%) |
| Unilateral recurrent herniaa | 45 (13%) |
| Bilateral recurrent hernia | 20 (6%) |
| Type of hernia [n (%)] | |
| Direct | 424 (60%) |
| Indirect | 136 (20%) |
| Femoral | 20 (2%) |
| Combined | 129 (18%) |
| Operative time [mean (range)] (min) | 33 (17–102) |
| Other procedures [n (%)] | |
| UHRb | 72 (20%) |
| Neurectomy | 1 (0.3%) |
| Bilateral vasectomy | 4 (1.2%) |
| Orchiectomy | 1 (0.3%) |
| Lipoma excision | 2 (0.6%) |
| Intraoperative complications | 1 (0.3%) |
| Bladder injury | 1 |
| Bowel injury | 0 |
| Vascular injury | 0 |
| Conversion to open [n (%)] | 1 (0.3%) |
| Length of stay [mean (range)] (d) | 0 (0–1) |
| Length of stay [n (%)] | |
| 0 d | 340 (99%) |
| 1 d | 3 (1%) |
A bilateral repair was performed because a contralateral hernia was incidentally discovered intraoperatively.
UHR = umbilical hernia repair.
The incidence of postoperative complications is reported in Table 3. Hematoma/seroma developed in 5 patients (1.5%). Postoperative wound infection occurred in only 1 patient (0.3%). Hematuria developed postoperatively in 2 patients (0.6%) (1 due to traumatic urinary catheter insertion and 1 due to intraoperative bladder injury). Postoperative acute myocardial infarction occurred in 1 patient (0.3%). Chronic pain and a burning sensation in the inguinal area after surgery were reported by 9 patients (2.6%). Three of them underwent re-exploration and either mesh removal (1 patient) or neurectomy (2 patients). Finally, among the 686 repairs, there were a total of 20 recurrences (2.9%) in 18 patients (5.2%). Two patients had bilateral recurrences, and 16 had unilateral recurrences. Of the recurrences, 25% (n=5) occurred in the first 6 months after surgery, 15% (n=3) occurred between 6 months and 1 year, 35% (n=7) occurred between 1 and 2 years, and 25% (n=5) occurred after 2 years. Seventy percent of the recurrences (n=14) occurred among direct hernias, 15% (n=3) among indirect hernias, 5% (n=1) among femoral hernias, and 10% (n=2) among combined hernias (Figure 1).
Table 3.
Postoperative Complications
| n (%) | |
|---|---|
| Hematoma/seroma | 5 (1.5%) |
| Wound infection | 1 (0.3%) |
| Hematuria | 2 (0.6%) |
| Myocardial infarction | 1 (0.3%) |
| Chronic pain | 9 (2.6%) |
| Reoperation | 3 |
| No reoperation | 6 |
| Recurrence | 18 (5.2%) |
| Site of recurrence | |
| Unilateral | 16 |
| Bilateral | 2 |
| Time to recurrence | |
| <6 mo | 5 (25%) |
| 6 mo to 1 y | 3 (15%) |
| 1–2 y | 7 (35%) |
| 2 y | 5 (25%) |
| Total | 20 (100%) |
Figure 1.
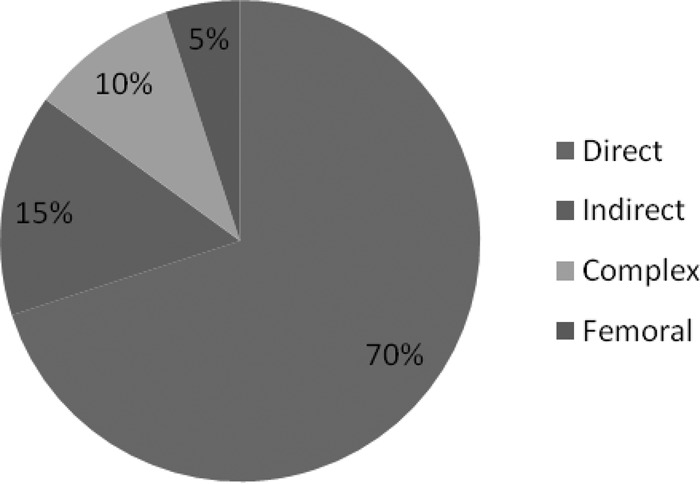
Recurrence rate by type of repaired hernia.
DISCUSSION
We have described the experience of a single surgeon performing bilateral laparoscopic TEP repair of 686 primary and recurrent inguinal hernias without mesh fixation in a series of 343 consecutive patients at our institution over a 6-year period. In comparison with the available literature about laparoscopic TEP repair,9–11,14–26 our patients had fewer intraoperative and postoperative complications, less chronic pain, and no increase in operative time or length of hospital stay but did have a slight increase in recurrence rate.
The indication for bilateral TEP repair was either the presence of a bilateral primary hernia, bilateral recurrent hernia, or unilateral recurrent hernia. Among patients with a preoperative diagnosis of unilateral recurrent hernia, bilateral repair was performed because a contralateral hernia was incidentally discovered intraoperatively. In this study about 13% of the patients were taken to the operating room with a preoperative diagnosis of unilateral recurrent hernia, were found to have an undiagnosed contralateral hernia intraoperatively, and eventually underwent bilateral repair. Diagnosing a potentially existing but preoperatively undiagnosed hernia is a clear advantage of laparoscopic repair. Bochkarev et al27 found unknown hernias on the contralateral side in 22% of patients in their study.
Data on the duration of surgery using the laparoscopic TEP repair technique vary in the literature. Several factors must be taken into account when comparing operative time, including the use of mesh fixation, the nature of the hernia (primary vs recurrent), the site of the hernia (unilateral vs bilateral), and the complexity of the hernia (simple vs combined). In a randomized controlled trial (RCT) of laparoscopic TEP repair with and without mesh fixation in 40 patients, the mean operative time was 66 minutes in the mesh fixation group and 61 minutes in the group with no fixation.14 Laparoscopic TEP repair of recurrent hernias is usually challenging because of tissue scarring and distorted anatomy that often require longer and more careful dissection. In a prospective study of 19 patients with recurrent unilateral inguinal hernias who underwent laparoscopic TEP repair, Jang et al15 reported a mean operative time of 100 minutes. Similarly, the complexity of the hernia affects the operative time because more time is needed for identification and reduction of all hernia contents safely and effectively. Obesity is another factor that has been considered a relative contraindication for laparoscopic inguinal hernia repair because it negatively affects the quality of dissection and the visualization of defects and hence results in a longer operative time and higher risk of recurrence.16 Consistent with our findings, Choi and Hur17 reported a mean operative time of 33 minutes in 112 patients who underwent bilateral laparoscopic TEP repair. However, no information was reported on whether mesh fixation was used. Considering the relatively large proportion of our patients who were either overweight or obese and given that almost one-fifth of them had recurrent or combined hernias, performing bilateral TEP repair did not increase the operative time in our study. Although nonfixation of mesh should logically reduce the operative time, it must also be noted that additional procedures such as umbilical hernia repair, neurectomy, bilateral vasectomy, orchiectomy, and lipoma excision were performed in more than one-fifth of the patients. The length of hospital stay was also examined as a proxy for resource utilization and cost. Generally speaking, performing bilateral repair should lead to higher incidences of pain and urinary retention postoperatively and thus a longer hospital stay. However, the fact that bilateral hernias were repaired through the same ports, with no additional ports placed, may explain why the length of hospital stay in this study was similar to or even shorter than that reported in the literature.17,18
Our rates of intraoperative bladder injury and conversion to an open approach were lower than those previously reported in the literature. Overall, major intraoperative complications are rarely seen in laparoscopic inguinal hernia surgery. Studies on laparoscopic repair report intraoperative bowel injury in 0% to 0.3% of cases and damage to major vessels at rates of 0% to 0.11%.19–21 No bowel injury or iliac vessel injury occurred among our patients. A more common intraoperative complication encountered with TEP and transabdominal preperitoneal repair, but readily managed endoscopically, is injury to the bladder. The one intraoperative bladder injury that occurred in our study was retroperitoneal and was not identified intraoperatively. Instead, hematuria developed while the patient was in the recovery room, and the diagnosis was made based on the computed tomography scan and cystogram. The patient was treated conservatively with urinary catheter drainage for 2 weeks. The patient did well, and the urinary catheter was removed with no problems. Although the operation was straightforward and uneventful in this patient, we do believe that this complication was related to surgery, likely a trocar-related injury.
Previous studies of TEP repair with mesh fixation reported postoperative hematoma/seroma rates of 4% to 8%.19–22 The lower rates in our study may be explained by nonfixation of mesh. Garg et al23 reported that patients with mesh fixation had a significantly higher incidence of seroma and hematoma formation (9.8%) than patients without mesh fixation (1.7%) (P<.001). A possible explanation is irritation of the peritoneum by the metallic tacks, leading to more serum formation. In addition, compartmentalization of the preperitoneal space by mesh fixation may lead to a delayed resolution of physiological serous collection in the dissected space, with later presentation of seroma.
The incidence of chronic pain in the literature ranges from 9% to 22% in patients after laparoscopic TEP repair with mesh fixation.9–11 Several RCTs were conducted to evaluate the incidence of chronic pain after laparoscopic TEP repair with and without mesh fixation.16,24,25 However, data from those studies are conflicting. An RCT by Taylor et al24 not only found that mesh fixation was associated with a higher incidence of chronic pain but also found an association between the number of fixation tacks used and the incidence of pain. In contrast, Koch et al14 in their RCT reported that elimination of mesh fixation during laparoscopic TEP repair significantly reduced the use of postoperative narcotic analgesia but did not reduce postoperative pain. In another RCT Ferzli et al25 reported no difference in the incidence of postoperative pain between the two groups. The incidence of postoperative chronic pain in our study is much lower than that reported in the literature. Among the 9 patients who had chronic pain postoperatively, only 3 had pain severe enough that they underwent re-exploration; the rest had mild pain that responded to physical therapy and nonoperative measures. It is reasonable to conclude that postoperative chronic pain is less likely to develop in patients who undergo TEP repair without mesh fixation; moreover, even when chronic pain does develop in such patients, their pain will be mild and unlikely to necessitate re-exploration.
Compared with data from previous reports,17–20 our recurrence rate is relatively higher. Possible explanations include the relatively longer follow-up in this study compared with previous studies. In our study 40% of the recurrences occurred within 1 year after surgery, whereas 60% were identified after the first year. In addition, the fact that almost 20% of our patients had recurrent hernias before surgery may have increased their risk of recurrence after TEP repair. The higher BMI observed in our patients may have contributed to this as well. The argument of whether using or not using mesh fixation will affect recurrence rates is an ongoing issue. In the early years of laparoscopic hernia repairs, strong fixation seemed to be the most important factor in the prevention of recurrence. With the increasing size of mesh and true macroporous materials now being used, the belief in strength has become less important and has given way to the concern that chronic pain is possibly caused by fixation. The controversy of fixation or nonfixation of mesh is currently under scrutiny. There are reports of excellent results with meshes that are not fixed,14,24,25 as well as some alarming reports showing an increased risk of recurrence.26 However, most of those studies were limited by a short follow-up time, which may not catch recurrences that occur later, as we showed in our study.
The dilemma of chronic pain after laparoscopic inguinal hernia repair using metallic tacks to fixate mesh has encouraged the development and use of alternative methods of fixation that avoid the use of such tacks, including fibrin glues, acrylate adhesives, and absorbable tacks. Patients appear to report less pain than with permanent fixation in some studies.28–30 However, these alternate forms of fixation have their own disadvantages including high cost and/or difficulty of use. Although those studies were limited by the short duration of follow-up, they were not able to show any statistically significant difference in the risk of hernia recurrence between the two methods of fixation. Considering the fact that 70% of our recurrences occurred among direct hernias, we recently adopted a policy of selective use of mesh fixation in patients with this type of hernia, especially when the defect is diffuse or too large, and we do use absorbable tacks in such cases.
Nonfixation of mesh is also cost-effective. Although we did not perform a cost analysis, previous studies have shown a significant reduction in cost when the mesh is not fixed.24 Ferzli et al25 showed that nonfixation of mesh resulted in savings of $120 per operation. The two groups in their study were similar in terms of sex ratio, operative times, conversion rates, recurrent hernias, and bilateral hernias repaired.
Some study limitations are worth mentioning. The retrospective collection of data is limited by the accuracy and completeness of the medical records. Lack of active follow-up is another issue. Lack of data on patients who had their complications and/or recurrences treated at other institutions is a concern. Our results are from a single medical center and from a single surgeon's experience; this might not reflect other institutions' or groups' practices.
In conclusion, laparoscopic TEP repair with no mesh fixation is safe and feasible for bilateral primary and recurrent inguinal hernias. Compared with the literature, our patients had fewer intraoperative and postoperative complications, less chronic pain, and no increase in operative time or length of hospital stay but did have a slight increase in recurrence rate. Nonfixation of mesh may decrease the incidence and severity of postoperative chronic pain, but this might be at the expense of an increase in the risk of recurrence. Selective use of mesh fixation for diffuse and large direct defects may be considered. Further prospective randomized trials with long-term follow-up will be needed for more insight.
Contributor Information
Ahmed Dehal, Department of General Surgery, Kaiser Permanente, Fontana, California..
Brandon Woodward, Department of General Surgery, Kaiser Permanente, Fontana, California..
Samir Johna, Department of General Surgery, Kaiser Permanente, Fontana, California..
Frank Yamanishi, Department of General Surgery, Kaiser Permanente, Fontana, California..
References:
- 1. Wara P, Bay-Nielsen M, Juul P, Bendix J, Kehlet H. Prospective nationwide analysis of laparoscopic versus Lichtenstein repair of inguinal hernia. Br J Surg. 2005;92:1277–1281 [DOI] [PubMed] [Google Scholar]
- 2. Grant AM, Scott NW, O'Dwyer PJ, MRC Laparoscopic Groin Hernia Trial Group. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg. 2004;91:1570–1574 [DOI] [PubMed] [Google Scholar]
- 3. Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A. Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc. 2004;18:518–522 [DOI] [PubMed] [Google Scholar]
- 4. McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trial lists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003. (1):CD001785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Memom MA, Cooper NJ, Memon B, Memon MI, Abrams KR. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. 2003;90:1479–1492 [DOI] [PubMed] [Google Scholar]
- 6. Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg. 2009;249:33–38 [DOI] [PubMed] [Google Scholar]
- 7. Carter J, Duh Q. Laparoscopic repair of inguinal hernias. World J Surg. 2011;35:1519–1525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kuhry E, van Veen R, Langeveld H, Steyerberg E, Jeekel J, Bonjer H. Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc. 2007;21:161–166 [DOI] [PubMed] [Google Scholar]
- 9. Kumar S, Wilson RG, Nixon SJ, Macintyre IM. Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg. 2002;89:1476–1479 [DOI] [PubMed] [Google Scholar]
- 10. Taylor C, Wilson T. Long-term results of laparoscopic totally extraperitoneal inguinal herniorrhaphy ANZ J Surg. 2005;75:637–639 [DOI] [PubMed] [Google Scholar]
- 11. Lau H, Patil NG, Yuen WK, Lee F. Prevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc. 2003;17:1620–1623 [DOI] [PubMed] [Google Scholar]
- 12. Hindmarsh AC, Cheong E, Lewis MP, Rhodes M. Attendance at a pain clinic with severe chronic pain after open and laparoscopic inguinal hernia repairs. Br J Surg. 2003;90:1152–1154 [DOI] [PubMed] [Google Scholar]
- 13. Wong J, Anvari M. Treatment of inguinodynia after laparoscopic herniorrhaphy: a combined laparoscopic and fluoroscopic approach to the removal of helical tackers. Surg Laparosc Endosc Percutan Tech. 2001;11:148–151 [PubMed] [Google Scholar]
- 14. Koch CA, Greenlee SM, Larson DR, Harrington JR, Farley DR. Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS. 2006;10:457–460 [PMC free article] [PubMed] [Google Scholar]
- 15. Jang IS, Lee SM, Kim JH, Kim BS, Choi SI. Clinical usefulness of laparoscopic total extraperitoneal hernia repair for recurrent inguinal hernia. J Korean Surg Soc. 2011;10:313–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kukleta JF. Causes of recurrence in laparoscopic inguinal hernia repair. J Minim Access Surg. 2006;2:187–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Choi YY, Hur KY. Simultaneous laparoscopic totally extraperitoneal repair of bilateral inguinal hernia: review of 1 surgeon experiences. Surg Laparosc Endosc Percutan Tech. 2011;21:264–266 [DOI] [PubMed] [Google Scholar]
- 18. Dulucq JL, Wintringer P, Mahajna A. Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3,100 hernia repairs over 15 years. Surg Endosc. 2009;23:482–486 [DOI] [PubMed] [Google Scholar]
- 19. Schultz C, Baca I, Gotzen V. Laparoscopic inguinal hernia repair. Surg Endosc. 2001;15:582–584 [DOI] [PubMed] [Google Scholar]
- 20. Sayad P, Hallak A, Ferzli G. Laparoscopic herniorrhaphy: review of complications and recurrence. J Laparoendosc Adv Surg Tech. 1998;8:3–10 [DOI] [PubMed] [Google Scholar]
- 21. Ramshaw B, Shuler FW, Jones HB, et al. Laparoscopic inguinal hernia repair. Surg Endosc. 2001;15:50–54 [DOI] [PubMed] [Google Scholar]
- 22. Liem MSL, van der Graaf Y, van Steensel CJ, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med. 1997;336:1541–1547 [DOI] [PubMed] [Google Scholar]
- 23. Garg P, Rajagopal M, Varghese V, Ismail M. Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1,692 hernias. Surg Endosc. 2009;23:1241–1245 [DOI] [PubMed] [Google Scholar]
- 24. Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S. Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomized clinical trial. Surg Endosc. 2008;22:757–762 [DOI] [PubMed] [Google Scholar]
- 25. Ferzli GS, Frezza EE, Pecoraro AM, Jr, Ahern KD. Prospective randomized study of stapled vs. unstapled mesh in laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg. 1999;188:461–465 [DOI] [PubMed] [Google Scholar]
- 26. Knook MT, Weidema WF, Stassen LP, van Steensel CJ. Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc. 1999;13:507–511 [DOI] [PubMed] [Google Scholar]
- 27. Bochkarev V, Ringley C, Vitamvas M, Oleynikov D. Bilateral laparoscopic hernia repair in patients with occult contralateral inguinal defects. Surg Endosc. 2007;21:734–736 [DOI] [PubMed] [Google Scholar]
- 28. Schwab R, Willms A, Kroger A, Becker HP. Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia 2006;10(3):272–277 [DOI] [PubMed] [Google Scholar]
- 29. Lau H. Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg. 2005;242(5):670–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Topart P, Vandenbroucke F, Lozac'h P. Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc. 2005;19(5):724–727 [DOI] [PubMed] [Google Scholar]


