Abstract
Background and Objectives:
Transumbilical single-incision laparoscopic surgery (SILS) is gaining in popularity as a minimally invasive technique. The reduced pain and superior cosmetic appearance it affords make it attractive to many patients. For this study, we focused on SILS, analyzing the outcomes of transumbilical single-incision laparoscopic liver resection (SILLR) achieved at our institution between January 2010 and February 2013.
Patients and Methods:
Pre- and postoperative data from 17 patients subjected to transumbilical SILLR for various hepatic lesions (8 hemangiomas, 2 hepatocellular carcinomas, 2 metastases, 2 calculi of left intrahepatic duct, and 3 adenomas) were assessed. Altogether, eight wedge resections, seven left lateral lobectomies, a combination wedge resection/left lateral lobectomy, and a proximal left hemihepatectomy segmentectomy were performed, as well as four simultaneous laparoscopic cholecystectomies. In each instance, three ports were installed through an umbilical incision. Once vessels and bleeding were controlled, the lesion(s) were resected with 5-mm margins of normal liver. Resected tissues were then bagged and withdrawn through the umbilical incision. The follow-up period lasted for a minimum of 6 months.
Results:
All 17 patients were successfully treated through a single umbilical incision. The procedures required 55 to 185 minutes to complete, with blood loss of 30 to 830 mL. Subjects regained bowel activity 0.8 to 2.3 days postoperatively and were discharged after 3 to 10 days. There were few complications (23.5%), limited to pleural effusion, wound infection, and incisional hernia.
Conclusions:
Transumbilical SILLR is challenging to perform through conventional laparoscopic instrumentation. The risk of bleeding and technical difficulties is high for lesions of the posterosuperior hepatic segment. Surgical candidates should be carefully selected to optimize the benefits of this technique.
Keywords: Laparoscopy, Single-incision surgery, Hepatectomy
INTRODUCTION
Laparoscopic hepatectomy (LH) is an emerging technique that is rarely performed outside of specialized institutions. Because of its inherent technical challenges, the risk of serious complications (such as hemorrhage and gas embolism) is considerable, and the suitability of LH for treatment of malignant lesions has been questioned. Although few large studies have been conclusive, and results are not easily reproducible in diverse settings, some noteworthy efforts to date demonstrate the feasibility and safety of LH in controlled environments.1–4 Current consensus at least concedes its superiority to open surgery in terms of intraoperative blood loss, pain control, hospital stay, resumption of oral intake, and complication rates.2,3
Single-incision laparoscopic liver resection (SILLR) is more challenging than conventional multi-incisional laparoscopic surgery. Posterosuperior lesions in particular are far from reach and are close to major blood vessels, making them especially difficult targets with a heightened procedural risk. Thus an appropriate experience level and command of the required procedures are mandatory.
This report details our SILLR technique (using conventional instrumentation) and our initial experience with SILLR of localized hepatic lesions in a select group of patients.
METHODS
Patient Selection and Surgical Indications
A total of 17 patients (age range, 32–71 y; males, 8; females, 9) presenting with focal hepatic lesions (8 hemangiomas, 2 hepatocellular carcinomas, 2 metastases [colon cancer], 2 calculi of left intrahepatic duct, and 3 adenomas) were selected for single-incision LH. The patients were retrospectively reviewed from a prospective database of laparoscopic hepatectomy. All patients provided complete informed consent regarding the nature of the surgical procedure and the risks involved before consents were obtained. The study was performed under institutional review board approval.
Conversion to multiport laparoscopic surgery or open surgery was grounds for exclusion. Procedures performed were as follows: eight wedge resections, seven left lateral lobectomies, one combination left lateral lobectomy/S8 wedge resection of two lesions, and one proximal left hemihepatectomy segmentectomy.
The inclusion criteria specified patients undergoing SILLR of malignant tumor <5.0 cm in diameter located in segments II or III, or those smaller than 2.5 cm in diameter located at the surface of the liver in segments IV, V, VI, or VIII; and patients with benign tumors <10 cm in diameter located in segments II or III, or those <5.0 cm in diameter located at the surface of the liver in segments IV, V, VI, or VIII. Resection of tumors located in the right lobe and the posterior and superior liver segments (VII, IV posterior, and I) are excluded. No prophylactic antibiotics were administered to the patients, and antiinflammatory therapy was stopped within one week in all patients, with no complications of postoperative infection.
Surgical Technique
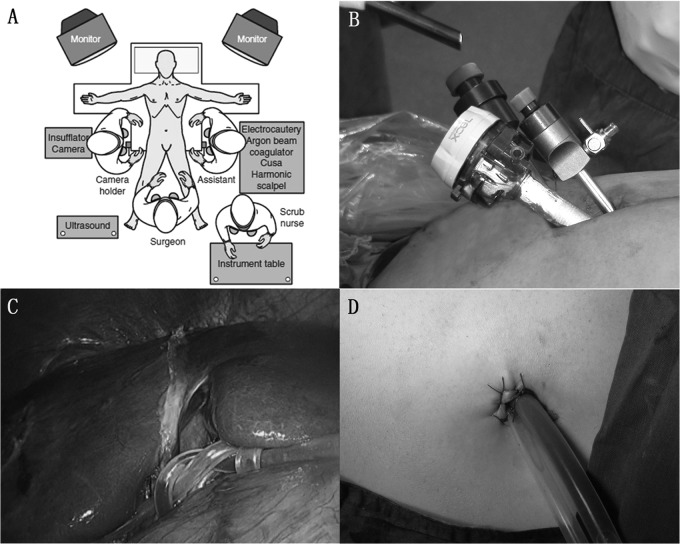
Each patient was placed in the supine position with legs apart. Under general anesthesia, the abdominal skin was cleaned and draped aseptically (Figure 1[A]). Once a pneumoperitoneum was induced (using the Veress needle technique), a 10-mm trocar was inserted through a 20-mm vertical intraumbilical incision. The abdominal cavity was then examined, and each lesion was localized through visual inspection or intraoperative ultrasonography. At this point, adjusting the operating table to a 30-degree reverse Trendelenburg position allows the intestines to gravitate downward, enabling better hepatic exposure. Next, skin and subcutis were retracted, creating an opening sufficient for 5-mm and 12-mm trocar insertions (Xcel B12LT; Ethicon Endo-Surgery Inc, Cincinnati, Ohio) in an inverted triangular formation (Figure 1[B]).
Figure 1.
A, Patient position; B, three ports placed in an inverted triangular formation; C, Pringle maneuver; D, drainage from the umbilicus.
Electrocautery (at least 5 mm from lesions, sometimes done using the Pringle maneuver [Figure 1[C]]) was used to mark the liver capsule for harmonic scalpel incision. Vascular and biliary supplies to lesions were ligated (applying Hem-o-lok clips proximal to the liver parenchyma and titanium clips distally) and divided with a harmonic scalpel. Smaller vessels were simply coagulated and divided without clipping. Bleeding sites were packed with dry gauze, and raw surfaces were covered with absorbable hemostatic gauze (Surgicel, Ethicon) as needed. Although difficult to accomplish in this setting, active bleeding spots were sutured with absorbable ligatures. Resected tissues were collected in a plastic bag that was withdrawn through the umbilical incision (extended to ∼50 mm) (Figure 2). Finally, a drainage tube was placed over the operative site and left protruding from the abdomen through the umbilical incision (Figure 1[D]). The umbilical incision was closed in two layers, with a purse string left through the peritoneal layer and subcutaneous tissue around the drain for later closure when the drain tube was removed.
Figure 2.
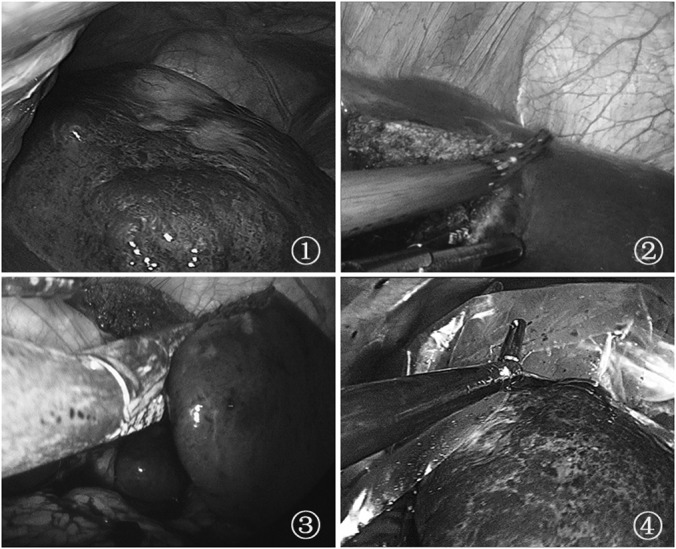
1, Positioning of the tumor; 2, liver incision via a harmonic scalpel; 3, use of an Endo-GIA stapler to resect the liver; 4, bagging the specimen.
RESULTS
Between January 2010 and February 2013, 17 consecutive patients at our institution underwent SILLR for focal hepatic lesions, and all procedures were successful. The range of patient follow-up was 6 to 42 months. Patient demographics, indications for resection, and tumor characteristics are summarized in Table 1. Altogether, eight wedge resections (including one S5 subcapsular hemangioma resection with synchronous cholecystectomy), seven left lateral lobectomies, one combination left lateral lobectomy/S8 wedge resection (for colon cancer liver metastasis), and one proximal left hemihepatectomy segmentectomy (patient 12, Figure 3) were performed (Table 1). None of the procedures required conversion to conventional laparoscopic hepatectomy or open surgery.
Table 1.
SILLR Cohort: Demographics and Interventions
| Patient No. | Age (y) | Gender | Lesion Type | Location | Size (cm) | Intervention |
|---|---|---|---|---|---|---|
| 40 | Male | Hepatic hemangioma and gallbladder polyp | S2, S3 | 5.4 × 4.1 | Single-incision LH left lateral lobectomy and cholecystectomy | |
| 2 | 56 | Male | Hepatic hemangioma | S5, S6 | 7.6 × 6.3 | Single-incision LH S5, S6 wedge resection and cholecystectomy |
| 3 | 61 | Male | Colon cancer and liver metastases | S2, S3 | 4.7 × 3.9 | Single-incision LH left lateral lobectomy and S8 wedge resection |
| 2.5 × 1.5 | ||||||
| 4 | 46 | Female | Left lateral lobe giant hemangioma | S2, S3 | 10.5 × 9.5 | Single-incision LH left lateral lobectomy |
| 5 | 50 | Female | Hepatic hemangioma | S2, S3 | 9.0 × 6.0 | Single-incision LH left lateral lobectomy |
| 6 | 60 | Male | Hepatic hemangioma | S2 | 4.5 × 4.0 | Single-incision LH S2 wedge resection |
| 7 | 50 | Female | Hepatocellular carcinoma (HCC) well-differentiated | S2, S3 | 3.3 × 2.6 | Single-incision LH S2 wedge resection |
| 8 | 35 | Female | Hepatic hemangioma | S2, S3 | 7.0 × 5.0 | Single-incision LH left lateral lobectomy |
| 9 | 34 | Female | Hepatic focal nodular hyperplasia (FNH) | S5, S6 | 6.2 × 4.0 | Single-incision LH S5 wedge resection |
| 10 | 56 | Female | Hepatic hemangioma | S2, S3 | 4.8 × 4.6 | Single-incision LH S2 wedge resection |
| 11 | 64 | Male | Hepatocellular carcinoma (HCC) well-differentiated | S8 | 3.0 × 2.5 | Single-incision LH S8 wedge resection |
| 12 | 48 | Male | Cholecystolithiasis and calculus of left intrahepatic duct | S2, S3 | — | Single-incision laparoscopic proximal left hemihepatectomy segmentectomy and cholecystectomy |
| 13 | 37 | Female | Liver adenoma | S4 | 4.0 × 3.0 | Single-incision LH S4 wedge resection |
| 14 | 32 | Female | Liver adenoma | S2, S3 | 10.0 × 8.0 | Single-incision LH left lateral lobectomy |
| 15 | 60 | Female | Hepatic hemangioma | S2, S3 | 5.0 × 3.0 | Single-incision LH left lateral lobectomy |
| 16 | 71 | Male | Cholecystolithiasis and calculus of intrahepatic duct | S2, S3 | — | Single-incision LH left lateral lobectomy |
| 17 | 58 | Male | Colon cancer and liver metastases | S5 | 2.0 × 2.0 | Single-incision LH S5 wedge resection and right colectomy |
LH, laparoscopic hepatectomy.
Figure 3.

Resected liver showing calculus of the intrahepatic duct and abscess formation.
For this cohort, the median operating time was 117.94 ± 49.21 minutes (range, 55–185), and median blood loss was 256.47 ± 236.51 mL (range, 30–830). Patients were discharged from the hospital 3 to 10 days after surgery (median, 7.65 ± 1.66) and resumed normal diets after 18 to 55 hours (median, 39.82 ± 10.93). Two patients later died (16 and 18 months postoperatively) as a result of multiple liver metastases (Table 2).
Table 2.
Patient Outcomes Post-SILLR
| Patient No. | Blood Loss (mL) | Operating Time (min) | Hospital Stay (d) | Days to Oral Intake (h) | Mortalitya | Postoperative Pain >5 d/Pain Scoreb (VAS) | |
|---|---|---|---|---|---|---|---|
| 1 | 120 | 155 | 7 | 40 | Alive | No/3 | |
| 2 | 830 | 175 | 8 | 44 | Alive | No/4 | |
| 3 | 800 | 185 | 10 | 48 | Expired 16 months postoperatively | Yes/6 | |
| 4 | 210 | 180 | 7 | 50 | Alive | No/4 | |
| 5 | 130 | 130 | 7 | 36 | Alive | No/2 | |
| 6 | 290 | 70 | 8 | 24 | Alive | No/3 | |
| 7 | 480 | 160 | 10 | 30 | Expired 18 months postoperatively | No/4 | |
| 8 | 220 | 115 | 8 | 48 | Alive | No/3 | |
| 9 | 200 | 115 | 6 | 45 | Alive | Yes/5 | |
| 10 | 310 | 85 | 7 | 51 | Alive | No/2 | |
| 11 | 180 | 55 | 8 | 55 | Alive with multiple metastases | No/3 | |
| 12 | 90 | 180 | 10 | 40 | Alive | No/5 | |
| 13 | 140 | 90 | 8 | 48 | Alive | No/4 | |
| 14 | 200 | 140 | 8 | 46 | Alive | No/3 | |
| 15 | 30 | 50 | 3 | 18 | Alive | No/2 | |
| 16 | 50 | 65 | 8 | 28 | Alive | No/2 | |
| 17 | 80 | 55 | 7 | 26 | Alive with no metastases | No/4 | |
| Total (N = 17) Percentage | Average | 256.47 ± 236.51 | 117.94 ± 49.21 | 7.65 ± 1.66 | 39.82 ± 10.93 | 11.76% | 11.76% |
VAS, visual analog scale.
Follow-up range was 6 to 42 months.
Highest recorded postoperative pain score.
The overall complication rate of 23.5% was attributable to two pleural effusions, one wound infection, and one incisional hernia. No other complications (eg, hematoma or abscess requiring drainage, upper gastrointestinal bleeding, bile duct obstruction, or bile leakage) were encountered (Table 3).
Table 3.
Complications
| Patient No. | Pleural Effusion | Incisional Infection | Incisional Hernia | Hematoma Requiring Drainage, Abscess Requiring Drainage, Abdominal Infection | Upper GI Bleeding, Bile Duct Obstruction, Bile Leak | Overall Complication |
|---|---|---|---|---|---|---|
| 1 | No | No | No | No | No | 0 |
| 2 | No | No | No | No | No | 0 |
| 3 | No | No | No | No | No | 0 |
| 4 | No | Yes | No | No | No | 1 |
| 5 | No | No | No | No | No | 0 |
| 6 | No | No | No | No | No | 0 |
| 7 | No | No | No | No | No | 0 |
| 8 | No | No | No | No | No | 0 |
| 9 | No | No | Yes | No | No | 1 |
| 10 | No | No | No | No | No | 0 |
| 11 | No | No | No | No | No | 0 |
| 12 | No | Yes | No | No | No | 1 |
| 13 | No | No | No | No | No | 0 |
| 14 | No | No | No | No | No | 0 |
| 15 | Yes | No | No | No | No | 1 |
| 16 | No | No | No | No | No | 0 |
| 17 | No | No | No | No | No | 0 |
| Total (N = 17)/percentage | 1/5.88% | 2/11.76% | 1/5.88% | 0/0.00% | 0/0.00% | 4/23.53% |
GI, gastrointestinal.
DISCUSSION
Single incision laparoscopic resection of lesions in the left lateral liver (segments II-III) or anterior and inferior liver segments (IV anterior, V, and VI) are most favorable because minimal mobilization of the liver is necessary. In our center, laparoscopic left lateral sectionectomy (resection of segments II and III) is now considered a routine approach for tumors localized in the left lateral lobe. Alternatively, resection of tumors located in the right lobe and the posterior and superior liver segments (VII, IV posterior, and I) is technically more demanding and should be approached with caution are not included in our study.
We placed a single drainage tube at the operative site, which exited the abdomen through the umbilical incision. The umbilical incision was closed in two layers, with a purse string left through the peritoneal layer and subcutaneous tissue around the drain for later closure when the drain tube was removed. The tube was used for observation of hemorrhage, but there was no complication of postoperative hemorrhage that occurred in our study; thus we are considering eliminating the drainage step for the no active bleeding patients in our next study.
SILS is technically more challenging than conventional laparoscopic surgery because of the limited operative field and a two-instrument restriction. Resection of deep-seated lesions, of which the view is obstructed, is especially problematic and risky. However, given the judicious use of tourniquets, hook electrocautery, ultrasonic scalpels, coagulation, LigaSure (Covidien, Mansfield, Massachusetts), absorbable clips, Endo-GIA staplers (Covidien), ligatures, and surgical/biological glues, bleeding can be controlled effectively. Endo-GIA staplers should be used to divide large vessels and bile ducts, followed by suturing cut edges with absorbable ligature as needed.
The advantages of SILS include a hidden (so-called “no scar”) incision for better cosmetic results, minimization of secondary abdominal injury, milder postoperative pain, quicker recovery, earlier resumption of normal activities, and shortened hospital stays, all of which have a very positive impact on patient rehabilitation.
In this cohort, three hepatic hemangiomas were resected from a single patient (maximum diameter, 8 cm). In two patients with hemangiomas, cholecystectomy was added to the SILLR procedures. All wounds healed well postoperatively and patient satisfaction was high.
The evolution of LH has been comparatively slow, primarily because surgeons are fearful of hemorrhage from the rich hepatic blood supply, and there is a general dearth of proper laparoscopic equipment. Furthermore, the use of carbon dioxide for pneumoperitoneum induction may promote gas embolism of the hepatic vein, a complication that carries the risks of considerable morbidity and/or mortality. The liver is a rather large organ as well, making it difficult to locate and resect deep-seated lesions that are obscured by the diaphragm or that are dangerously close to vena cava.
In recent years, >100 cases of minimally invasive liver surgery have appeared in various medical journals,1,3 Chinese and foreign,3–5 indicating that this approach is increasingly seen as viable by the surgical community. Cumulative experience and gradual modernization of operative techniques are contributing greatly to the resolution of major technical difficulties and risk reduction. In time, minimally invasive surgery of the liver thus promises to become much safer.
Contributor Information
Shuodong Wu, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Xiao-Peng Yu, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Yu Tian, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Ernest Amos Siwo, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Yongnan Li, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Hong Yu, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Dianbo Yao, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
Chao Lv, Department of Minimally Invasive Surgery, Shengjing Hospital of China Medical University, Shenyang, China..
References:
- 1. Sasaki A, Nitta H, Otsuka K, et al. Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg. 2009;96:274–279 [DOI] [PubMed] [Google Scholar]
- 2. Azagra JS, Goergen M, Gilbart E, Jacobs D. Laparoscopic anatomical (hepatic) left lateral segmentectomy–technical aspects. Surg Endosc. 1996;10:758–761 [DOI] [PubMed] [Google Scholar]
- 3. Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144:143–147 [DOI] [PubMed] [Google Scholar]
- 4. Fors D, Eiriksson K, Arvidsson D, Rubertsson S. Gas embolism during laparoscopic liver resection in a pig model: frequency and severity Br J Surg. 2010;105:282–288 [DOI] [PubMed] [Google Scholar]
- 5. Hu MG, Zhao GD, Xu DB, Liu R. Transumbilical single-incision laparoscopic hepatectomy: an initial report. Chinese Med J. 2011;124(5):787–789 [PubMed] [Google Scholar]