Abstract
Objective
To report a novel mutation in the gene EIF2B3 responsible for a late-onset form of vanishing white matter disease.
Design
Case report.
Setting
University teaching hospital.
Patient
A 29-year-old pregnant woman with a history of premature ovarian failure and hemiplegic migraines presented with a 10-week history of progressive confusion and headaches. Magnetic resonance imaging of the brain revealed a diffuse leukoencephalopathy.
Results
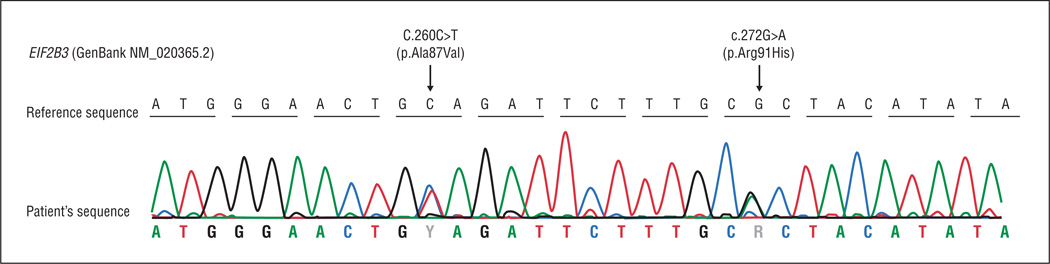
Sequencing of the exons and intron boundaries of EIF2B3 uncovered 2 missense mutations: c.260C>T (p.Ala87Val) and c.272G>A (p.Arg91His). To our knowledge, the latter missense mutation has never been previously reported.
Conclusion
This is the second report of adult-onset vanishing white matter disease due to mutations in EIF2B3 and the first report of the c.272G>A (p.Arg91His) missense mutation.
Vanishing white matter disease (VWM; OMIM 603896),1 also called childhood ataxia with central hypomyelination, is one of the most common leukodystrophies.2 It is an autosomal recessive leukoencephalopathy with typical onset in the pediatric age group. It is estimated that adulthood-onset VWM represents 15% of cases.3 The classic phenotype is characterized by an onset between the first and fifth years of life, with prominent cerebellar ataxia and spasticity. The disease is typically slowly progressive with episodes of neurological deterioration classically triggered by stressful events (eg, fever, infections, mild head trauma, or even fright).1,4 The evolution of the disease is highly variable, from patients dying within 1 to 5 years of disease onset to a much slower progression.5
Patients with the adult-onset form of the disorder typically have a milder and more insidious clinical course characterized by behavioral changes, dementia, and seizures.6,7 A few cases have presented with complicated migraines.8,9 The typical stress-related acute neurological deteriorations are less frequent in adult-onset cases.3 Ovarian failure is frequently reported in women with VWM and can precede the neurological symptoms,10,11 leading to the name ovarioleukodystrophy.10,12 Interestingly, gene mutations in EIF2B1, EIF2B2, EIF2B3, EIF2B4, and EIF2B5 are extremely rare among subjects with premature ovarian failure.13
Neuroradiological findings of VWM are specific.1,14 Brain magnetic resonance imaging typically shows diffuse and symmetric white matter hyperintensities on T2-weighted imaging, with possible sparing of the U fibers, the outer rim of the corpus callosum, the anterior commissure, and the internal capsule.15 The cerebral white matter typically progresses to cystic degeneration and rarefaction, best visualized in fluid-attenuated inversion recovery or proton density sequences.1 The cerebellar and brainstem white matter can be affected as well, but no cystic degeneration has been reported.1,6 Magnetic resonance spectroscopy may show a global reduction of all metabolites.16,17
Mutations in any of the 5 genes encoding the eukaryotic translation initiation factor 2B (EIF2B1-EIF2B5) are responsible for the disease.18,19 Patients usually have a compound heterozygous status.20 Mutations in EIF2B5 are the most common, accounting for approximately 60% to 70% of all cases of VWM.19,20 The Arg113His mutation is the most frequent18 and is usually associated with the adult-onset form.21
We report an atypical case of adult-onset VWM carrying a novel mutation in EIF2B3 (GenBank NM_020365.2).
REPORT OF A CASE
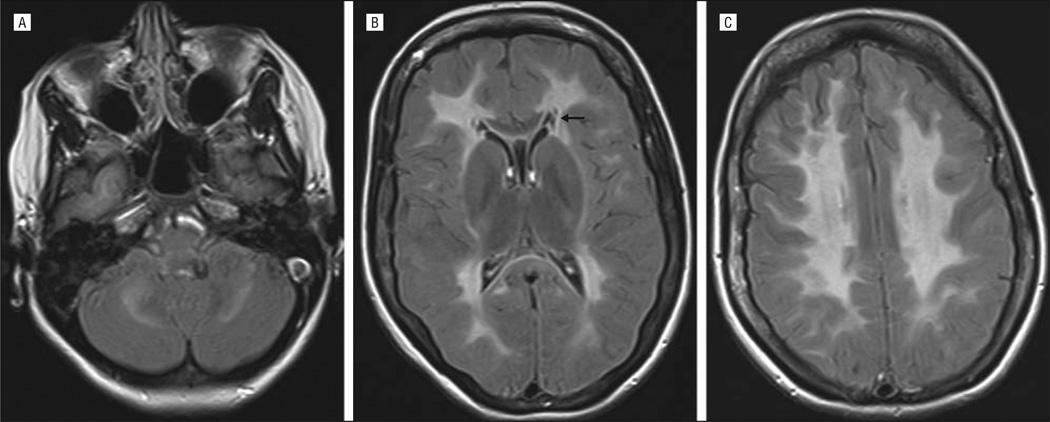
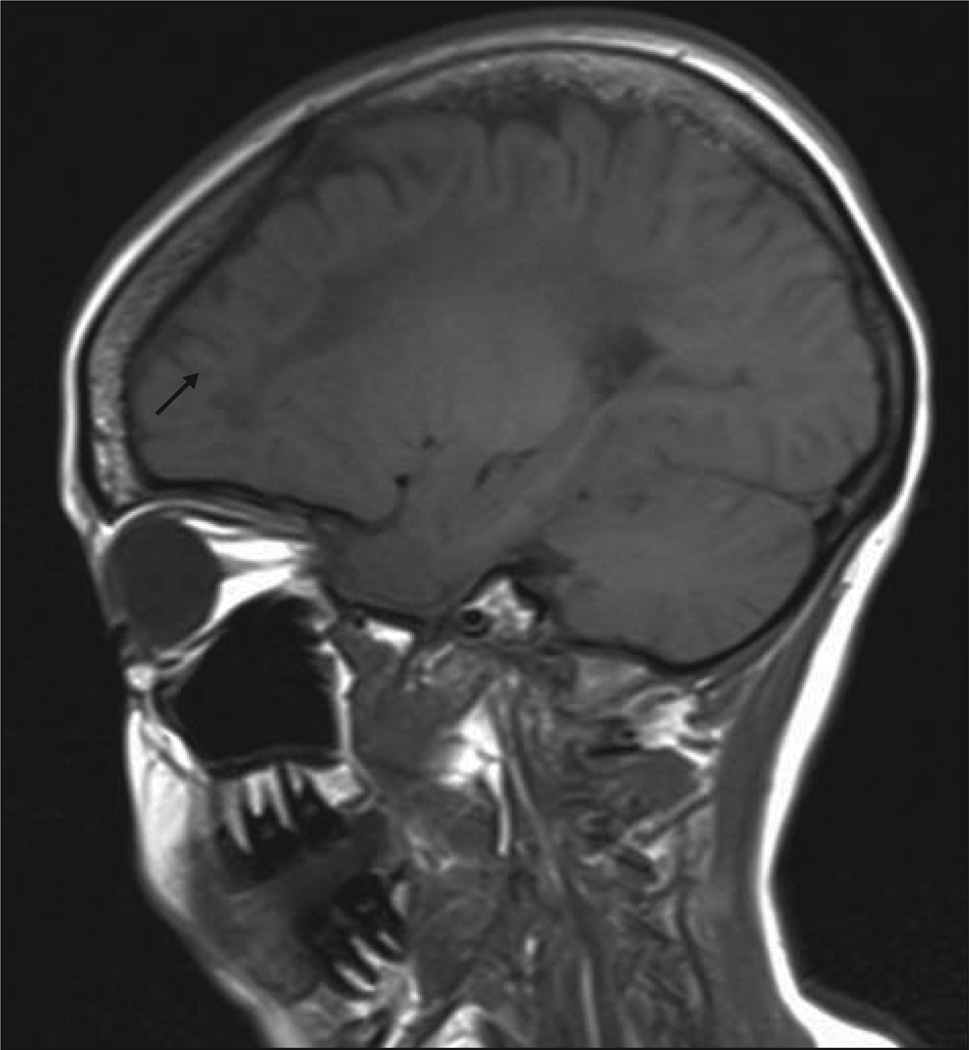
This patient was first seen by our neurogenetics team at age 29 years for an acute episode of migraine, fever, and encephalopathy. She had been pregnant for 10 weeks at the time and had constant headache with intermittent left hemibody paresthesias, aphasia, nausea, and vomiting since the beginning of her pregnancy. The patient was the second daughter of nonconsanguineous French Canadian parents. The family history was unremarkable. Her medical history was significant for hemiplegic migraines since age 20 years as well as secondary amenorrhea and premature ovarian failure. Magnetic resonance imaging of the brain performed at age 21 years revealed a diffuse leukoencephalopathy; magnetic resonance spectroscopy showed a reduction of all metabolites. The investigations performed at the time did not uncover the cause of her leukoencephalopathy. On arrival to the emergency department, the degree of her encephalopathy limited the neurological examination. Laboratory investigations failed to show any abnormality except mild leukocytosis. Electroencephalography revealed a slow background without epileptic abnormality. During the course of her admission, the patient’s encephalopathy subsided and, as she became more collaborative, mild cerebellar signs were noted. In the following month, she gradually improved but did not recover completely; she remained with impaired cognitive status and behavioral disturbances. Magnetic resonance imaging of the brain confirmed the known diffuse and symmetric cerebral and cerebellar white matter abnormalities, with hyperintense signal on T2-weighted images (Figure 1) and hypointense signal on T1-weighted images (Figure 2). Small cystic areas were seen bilaterally at the frontal horns on a fluid-attenuated inversion recovery sequence (Figure 1B). Otherwise, there was no evidence of white matter rarefaction or cystic degeneration.
Figure 1.
Axial fluid-attenuated inversion recovery magnetic resonance images. A, Symmetric involvement is noted at the level of the cerebellar white matter. B, Diffuse and symmetric leukodystrophy is evident; the U fibers, the outer rim of the corpus callosum, and the internal capsule are relatively spared. Small areas of cystic degeneration (arrow) are noted bilaterally in the periventricular white matter. The typical widespread white matter rarefaction is lacking. C, Diffuse and symmetric white matter involvement is noted at the level of the centrum semiovale.
Figure 2.
Sagittal T1-weighted magnetic resonance image shows the diffuse and homogeneous white matter hypointense signal in the deep cerebral white matter, relatively sparing the U fibers (arrow).
On the basis of the clinical features, the history of ovarian failure, and the magnetic resonance imaging pattern, adult-onset VWM was suspected. Genetic testing for the 5 EIF2B genes was performed (PreventionGenetics) and uncovered 2 mutations in EIF2B3: c.260C>T (p.Ala87Val) and c.272G>A (p.Arg91His) (Figure 3). To our knowledge, the second mutation in exon 3 has never been reported but is thought to be pathogenic because it leads to an amino acid substitution (p.Arg91His) in a highly conserved region across species and is predicted to be probably damaging by the experimental program Polymorphism Phenotyping version 2.22
Figure 3.
Genomic sequence chromatograms of the 2 missense mutations in exon 3 of EIF2B3: the known c.260C>T mutation and the novel c.272G>A mutation.
COMMENT
This is the second report of adult-onset VWM with mutations in EIF2B3.23 Mutations in EIF2B3 are thought to account for approximately 4% to 7% of all VWM cases.20,24 We report a novel missense mutation in this gene in an adult-onset case. Wu et al25 reported that mutations in EIF2B3 account for 20% of the Chinese pediatric cases, raising the hypothesis that mutations in this gene may be more prevalent than previously thought, particularly in the Chinese population, although this was a small patient sample. Moreover, they identified 2 novel missense mutations in the gene: c.140G>A in exon 2 and c.1037T>C in exon 9, the latter being a common mutation present in 4 of 5 patients. Until recently, mutations in EIF2B3 have never been reported in patients with adult-onset VMW or ovarioleukodystrophy.10,11,18 A recent article23 reports a new homozygous mutation (c.80T>A) in EIF2B3 resulting in the substitution of leucine by glutamine (p.Leu27Gln) in an adult-onset case of VWM and ovarian failure. Our case is thus the second report of late-onset VWM and ovarian failure due to mutations in EIF2B3.
Some clinical features in our patient are of particular interest. The hemiplegic migraine as the presenting neurological sign has been rarely reported in VWM.8,9 In a case of pediatric-onset VWM reported by Ramaswamy et al8 in 2006, episodes of periodic hemiparesis and headache were described in the course of the disease. Ramaswamy and colleagues discussed the fact that the episodes of hemiplegia and headaches could fulfill the criteria for hemiplegic migraines. They emphasized that in both conditions, the episodes can be triggered by stressful events.8 This was also observed in our patient; in fact, the patient, who has had hemiplegic migraines for years, experienced an exacerbation of her migraines culminating in an encephalopathy in the context of her acute febrile disease and pregnancy.
The known correlation between the age at onset of the neurological deterioration and the severity of ovarian failure26 was observed in our case; despite the previous diagnosis of early menopause, the patient became pregnant unexpectedly without any hormone replacement therapy or in vitro fertilization. This event can be explained only by considering residual ovarian functionality.
The trigger event for the rapid deterioration in our patient is not completely established, but the role of the pregnancy should be taken into account. Another case of rapid neurological deterioration was described in a patient who had undergone in vitro fertilization and had been pregnant for 4 weeks.27 The important physical and psychological changes occurring in the first trimester as well as in the last weeks of gestation, especially the labor, may be considered potentially stressful events.27 Both the case reported by Peter et al27 and our case had a history of leukoencephalopathy and premature ovarian failure when the acute neurological deterioration occurred during pregnancy, suggesting the diagnosis of VWM.
In conclusion, our patient is the second adult-onset case of VWM with mutations in EIF2B3 reported in the literature and the first, to our knowledge, with the c.272G>A (p.Arg91His) missense mutation in exon 3. Hemiplegic migraines are an unusual but possible presenting manifestation of this disorder, and it is important to consider the diagnosis of adult-onset VWM disease in patients with leukoencephalopathy and premature ovarian failure with or without neurological deterioration.
Acknowledgments
Funding/Support: Dr La Piana has received a fellowship grant from the Montreal Neurological Institute. Dr Vanderver has received support from the American Academy of Neurology Foundation. Dr van der Knaap is supported by TOP grant 9120.6002 from the Dutch Organisation for Scientific Research (ZonMw) and grant 2008029 WO from the Dr W. M. Phelps Foundation. Drs Brais and Bernard have received research funds from the Fondation des Leucodystrophies and the European Leukodystrophy Foundation. Dr Bernard has received fellowship grants from the Fonds de Recherche en Santé du Québec.
Additional Contributions: We thank the patient for her participation in this study and Luc Marchand, MD, FRCPC, for referring the patient. Prevention Genetics performed the genetic testing and provided the color chromatogram of the 2 mutations.
Footnotes
Author Contributions: Study concept and design: Brais and Bernard. Acquisition of data: Vanderver, Roux, and Brais. Analysis and interpretation of data: La Piana, Vanderver, van der Knaap, and Tampieri. Drafting of the manuscript: La Piana. Critical revision of the manuscript for important intellectual content: Vanderver, van der Knaap, Roux, Tampieri, Brais, and Bernard. Administrative, technical, and material support: Vanderver. Study supervision: Brais and Bernard.
Financial Disclosure: None reported.
REFERENCES
- 1.van der Knaap MS, Barth PG, Gabreëls FJ, et al. A new leukoencephalopathy with vanishing white matter. Neurology. 1997;48(4):845–855. doi: 10.1212/wnl.48.4.845. [DOI] [PubMed] [Google Scholar]
- 2.van der Knaap MS, Breiter SN, Naidu S, Hart AAM, Valk J. Defining and categorizing leukoencephalopathies of unknown origin:MRimaging approach. Radiology. 1999;213(1):121–133. doi: 10.1148/radiology.213.1.r99se01121. [DOI] [PubMed] [Google Scholar]
- 3.Labauge P, Horzinski L, Ayrignac X, et al. Natural history of adult-onset eIF2Brelated disorders: a multi-centric survey of 16 cases. Brain. 2009;132(pt 8):2161–2169. doi: 10.1093/brain/awp171. [DOI] [PubMed] [Google Scholar]
- 4.Schiffmann R, Fogli A, Van der Knaap MS, Boespflug-Tanguy O. Childhood ataxia with central nervous system hypomyelination/vanishing white matter. In: Pagon RA, Bird TD, Dolan CR, et al., editors. Gene Reviews. Seattle: University of Washington; 1993. [Google Scholar]
- 5.van der Knaap MS, Pronk JC, Scheper GC. Vanishing white matter disease. Lancet Neurol. 2006;5(5):413–423. doi: 10.1016/S1474-4422(06)70440-9. [DOI] [PubMed] [Google Scholar]
- 6.van der Knaap MS, Kamphorst W, Barth PG, Kraaijeveld CL, Gut E, Valk J. Phenotypic variation in leukoencephalopathy with vanishing white matter. Neurology. 1998;51(2):540–547. doi: 10.1212/wnl.51.2.540. [DOI] [PubMed] [Google Scholar]
- 7.Prass K, Brück W, Schröder NW, et al. Adult-onset leukoencephalopathy with vanishing white matter presenting with dementia. Ann Neurol. 2001;50(5):665–668. doi: 10.1002/ana.1259. [DOI] [PubMed] [Google Scholar]
- 8.Ramaswamy V, Chan AK, Kolski HK. Vanishing white matter disease with periodic (paroxysmal) hemiparesis. Pediatr Neurol. 2006;35(1):65–68. doi: 10.1016/j.pediatrneurol.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 9.van der Knaap MS, Bugiani M, Boor I, Proud CG, Scheper GC. Vanishing white matter. In: Valle D, Beaud AL, Vogelstein B, et al., editors. Metabolic and Molecular Bases of Inherited Disease. New York, NY: McGraw-Hill; 2010. [Google Scholar]
- 10.Fogli A, Rodriguez D, Eymard-Pierre E, et al. Ovarian failure related to eukaryotic initiation factor 2B mutations. Am J Hum Genet. 2003;72(6):1544–1550. doi: 10.1086/375404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathis S, Scheper GC, Baumann N, et al. The ovarioleukodystrophy. Clin Neurol Neurosurg. 2008;110(10):1035–1037. doi: 10.1016/j.clineuro.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Schiffmann R, Tedeschi G, Kinkel RP, et al. Leukodystrophy in patients with ovarian dysgenesis. Ann Neurol. 1997;41(5):654–661. doi: 10.1002/ana.410410515. [DOI] [PubMed] [Google Scholar]
- 13.Fogli A, Gauthier-Barichard F, Schiffmann R, et al. Screening for known mutations in EIF2B genes in a large panel of patients with premature ovarian failure. BMC Womens Health. 2004;4(1):8. doi: 10.1186/1472-6874-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaczorowska M, Kuczynski D, Jurkiewicz E, Scheper GC, van der Knaap MS, Jozwiak S. Acute fright induces onset of symptoms in vanishing white matter disease: case report. Eur J Paediatr Neurol. 2006;10(4):192–193. doi: 10.1016/j.ejpn.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 15.van der Knaap M, Valk J. Magnetic Resonance of Myelination and Myelin Disorders. 3rd ed. Heidelberg, Germany: Springer-Verlag; 2005. [Google Scholar]
- 16.Tedeschi G, Schiffmann R, Barton NW, et al. Proton magnetic resonance spectroscopic imaging in childhood ataxia with diffuse central nervous system hypomyelination. Neurology. 1995;45(8):1526–1532. doi: 10.1212/wnl.45.8.1526. [DOI] [PubMed] [Google Scholar]
- 17.Dreha-Kulaczewski SF, Dechent P, Finsterbusch J, et al. Early reduction of total N-acetyl-aspartate-compounds in patients with classical vanishing white matter disease: a long-term follow-up MRS study. Pediatr Res. 2008;63(4):444–449. doi: 10.1203/01.pdr.0000304934.90198.25. [DOI] [PubMed] [Google Scholar]
- 18.Leegwater PA, Vermeulen G, Könst AA, et al. Subunits of the translation initiation factor eIF2B are mutant in leukoencephalopathy with vanishing white matter. Nat Genet. 2001;29(4):383–388. doi: 10.1038/ng764. [DOI] [PubMed] [Google Scholar]
- 19.van der Lei HD, van Berkel CG, van Wieringen WN, et al. Genotype-phenotype correlation in vanishing white matter disease. Neurology. 2010;75(17):1555–1559. doi: 10.1212/WNL.0b013e3181f962ae. [DOI] [PubMed] [Google Scholar]
- 20.Fogli A, Schiffmann R, Bertini E, et al. The effect of genotype on the natural history of eIF2B-related leukodystrophies. Neurology. 2004;62(9):1509–1517. doi: 10.1212/01.wnl.0000123259.67815.db. [DOI] [PubMed] [Google Scholar]
- 21.van der Knaap MS, Leegwater PA, van Berkel CG, et al. Arg113His mutation in eIF2Bepsilon as cause of leukoencephalopathy in adults. Neurology. 2004;62(9):1598–1600. doi: 10.1212/01.wnl.0000123118.86746.fc. [DOI] [PubMed] [Google Scholar]
- 22.Adzhubei IA, Schmidt S, Peshkin L, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7(4):248–249. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsukawa T, Wang X, Liu R, et al. Adult-onset leukoencephalopathies with vanishing white matter with novel missense mutations in EIF2B2, EIF2B3, and EIF2B5. Neurogenetics. 2011;12(3):259–261. doi: 10.1007/s10048-011-0284-7. [DOI] [PubMed] [Google Scholar]
- 24.Maletkovic J, Schiffmann R, Gorospe JR, et al. Genetic and clinical heterogeneity in eIF2B-related disorder. J Child Neurol. 2008;23(2):205–215. doi: 10.1177/0883073807308705. [DOI] [PubMed] [Google Scholar]
- 25.Wu Y, Pan Y, Du L, et al. Identification of novel EIF2B mutations in Chinese patients with vanishing white matter disease. J Hum Genet. 2009;54(2):74–77. doi: 10.1038/jhg.2008.10. [DOI] [PubMed] [Google Scholar]
- 26.Fogli A, Boespflug-Tanguy O. The large spectrum of eIF2B-related diseases. Biochem Soc Trans. 2006;34(pt 1):22–29. doi: 10.1042/BST20060022. [DOI] [PubMed] [Google Scholar]
- 27.Peter L, Niel F, Catenoix H, et al. Acute neurological deterioration in ovarioleukodystrophy related to EIF2B mutations: pregnancy with oocyte donation is a potentially precipitating factor. Eur J Neurol. 2008;15(1):94–97. doi: 10.1111/j.1468-1331.2007.01999.x. [DOI] [PubMed] [Google Scholar]