Introduction
Adequate screening for identifying individuals at risk of developing cardiovascular disease (CVD) is important because vascular disorders are a preventable cause of morbidity and mortality worldwide. Furthermore, the lifetime risk of developing CVD is high (an estimated 66% for men and >50% for women) and often the first symptom of disease is a sudden death, thereby occurring without an opportunity for intervention.1–3 Conventional risk factors aggregated as risk scores (such as the National Heart, Lung, and Blood Institute report on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults [Adult Treatment Panel III, based on the Framingham risk score]) have shown to predict the 10-year risk of developing coronary heart disease (CHD) in most individuals,4, 5 and the predictive capability of these risk factors extends over a 30–year time horizon.6 However, established risk scores may underestimate CVD risk in some individuals.7 In addition, it is also recognized now that even among those with an optimal risk factor profile at age 55 years, the residual lifetime risk of CVD remains substantial (40% in men and 30% in women).3 These observations have motivated the search for additional risk factors (including imaging tests that detect subclinical atherosclerosis) that can enhance the predictive utility of conventional risk factors.
The underestimation of CVD risk may be especially evident in people with a family history of premature CVD.8–10 Independent of established risk factors, a positive family history has been associated with a greater prevalence of subclinical atherosclerosis (such as an increased coronary artery calcium [CAC] score, obtained by coronary computerized tomography [CCT]).11, 12 Estimation of the CAC score is, therefore, currently considered a valuable supplement to the Framingham Risk Score for the assessment of CVD risk in individuals with a familial history of premature vascular disease11, 12 and among patients classified as having an intermediate 10-year risk of coronary heart disease (CHD) based on Framingham Risk Score.13, 14
Undoubtedly, biomarkers (including imaging tests such as CCT) may aid the risk-stratification of asymptomatic people at risk of developing CVD. Yet, several criteria must be satisfied before any such biomarker can be incorporated into clinical practice at primary care settings. Table 1 summarizes the American Heart Association guidelines for the evaluation of biomarkers for screening for CVD risk.15 A comprehensive evaluation of which criteria are met by a putative screening biomarker assumes specific importance when a candidate test is expensive or not easily obtained (as it is in the case of imaging tests). The present article focuses on the clinical utility of CAC scores derived by CCT (as the prototype imaging test) because it is the most commonly used and best studied imaging modality that is used for screening asymptomatic individuals in the community. To put the discussion into a clinical context, we present 2 clinical cases in Table 2, which should serve as an appetizer for reflection. The 2 examples reflect relevant scenarios where CCT testing is appropriate according to guidelines, but where the interpretation of CAC scores may be challenging.
Table 1.
Principles for evaluation of a new biomarker, as suggested by Hlatky et al.15 in 2009 AHA guidelines of evaluation of a new biomarker.
|
Table 2.
Two illustrative cases.
| Mrs. X is a 48-year old African American lady who is overweight (body mass index of 29 kg/m2), has a slightly pro-atherogenic lipid profile with a high-density lipoprotein cholesterol value of 42 mg/dL and a total cholesterol value of 235 mg/dL, and a normal blood glucose. She has a normal estimated glomerular filtration rate and no microalbuminuria. Her mother suffered from an ischemic stroke at the age of 61 and her father died from myocardial infarction at the age of 55. She measured her blood pressure at home with an average value of 145/90 mmHg. The blood pressure in clinic is 150/95 mm Hg. She is a smoker and has a stressful life providing care for her two grandchildren aged 1 and 3 years two days a week, along with her fulltime night job at a convenience store. Because of her positive family history and adverse risk profile, her doctor refers her to CCT and her CAC score turns out to be zero. |
| Mr. Y is a 74-year old white man with an optimal lipid profile (HDL cholesterol 52 mg/dL and total cholesterol 195 mg/dL), normal blood pressure (120/80 mmHg), euglycemia, a normal estimated glomerular filtration rate with no microalbuminuria, and no family history of early-onset cardiovascular disease. He is a non-smoker and swims for 30 minutes 3x each week. Mr. Y has read in the newspaper about this new facility that provides CCT that provokes his interest and he seeks the test to find out his CAC score. His doctor, therefore, refers him to a CCT and the CAC score turns out to be >300. |
Based on the given information, the 10-year risk of developing coronary heart disease based on the Framingham Risk Score can be calculated elsewhere (http://cvdrisk.nhlbi.nih.gov/calculator.asp).
CAC score as an independent risk factor in asymptomatic individuals: Some Challenges
Data on Long-Term Outcomes
Several population-based cohort studies with a typical follow-up time of 3–5 years have consistently demonstrated that elevated CAC scores are associated with increased risk of new-onset CVD independent of standard risk factors and the Framingham Risk Score.16–23 However, there are very limited data available on CVD risk over a longer time horizon (such as 10-, 20- or 30-year risk of CVD).24 It seems likely that a high CAC score will continue to maintain a strong adverse prognostic value, but it is less clear if a CAC score of 0 will continue to maintain a strong favorable prognostic value over a longer time period. A CAC score of 0 is associated with a low risk of CVD during the subsequent 3–5 years and event rates may be as low as the event rates for those with a low Framingham Risk Score (<10% risk of coronary death or myocardial infarction within the next 10 years). The reported coronary death or myocardial infarction event rates were 11 of 1322 (0.8%) for those with a CAC score of 0 vs. 26 of 2230 (1.2%) for those with a Framingham Risk Score <10% during a mean follow-up of 5.0 years in the Heinz Nixdorf Recall Study.25 During a mean follow-up of 7 years corresponding numbers were 14 of 316 (4.4%) for those with a CAC score of 0 vs. 1 of 98 (1.0%) for those with a Framingham Risk Score <10% in the South Bay Heart Watch study. Moreover, during a follow-up of 7 years, 7 of 75 individuals (9.3%) with a CAC score of 0 but a Framingham Risk Score of ≥21 experienced an event in the South Bay Heart Watch study. Investigating a cohort of 442 individuals with a CAC score of 0 annually for 5 consecutive years, Min et al. reported that 106 patients (25.1%) converted to a CAC >0 during the study period, but that such a conversion was very uncommon before year 4 and escalated at the end of the study period.26 Additional studies are, therefore, clearly needed to establish the longer-term prognosis associated with a CAC score of 0.
Although not recommended in guidelines (for several reasons), one theoretical possibility to overcome the issue of limited follow-up time for currently available data could be to re-screen individuals at select time intervals, e.g., every 5 years to define management strategies. Longitudinal data indicate that individuals who have rapid increases in CAC scores over time are at markedly greater risk of CVD.24, 27 For example, 1 study showing that an increase of the CAC score >15% per year translated into a 17-fold increased risk of CHD, compared to those who did not have a progression in CAC scores.27 Recent data from the Multi-Ethnic Study of Atherosclerosis (MESA) confirm the prognostic significance of change in CAC.28 However, another recent study noted that progression of CAC score by >50 over a 5-year period was noted in only 2% of individuals.29 Thus, the use of changes in CAC scores is challenged by the limited variability over shorter periods of follow-up, relative to levels of other CVD risk factors.
Effect of Demographic Factors Including Race
It is unclear if the interpretation of CAC scores should be age- or ethnicity-specific. For example, it has been argued by Pletcher et al.30 that a CAC score of 50 may be unusually high for a 40-year-old woman without other CHD risk factors, but unusually low for a 70-year-old man with hypertension, and that the same CAC score, therefore, may affect risk assessment (post-test probability) in opposite directions for these two individuals. Likewise, the prevalence and possible prognostic importance of a high CAC score may vary by ethnicity. For instance, the MESA study reported that in women, whites had the highest CAC percentiles followed by the Chinese and blacks, whereas the Hispanics had the lowest percentiles of CAC scores. In men, the rank ordering of CAC scores was slightly different: whites had the highest percentiles followed by the Hispanics, with the lowest CAC scores being observed in blacks at the younger ages and in Chinese at the older ages.31 However, no differences in the prevalence of a CAC score >10 Agatston units were reported in asymptomatic whites versus blacks in the Dallas Heart Study.32 The prognostic importance of race in the risk assessment of CAC scores has not been firmly established yet, but data from the MESA study suggested that there were no significant race-related differences in the prognostic importance of a specific CAC score and that the predictive utility of CAC scores was independent of race.18, 33
Test-Retest Variability
The concept of reproducibility is important for all biomarkers, and CAC scores are no exception. Whereas earlier studies reported a high variability in repeat CCT scans to measure CAC, more recent studies have noted mean interscan variability of 15 to 20% with a median of 4 to 8%.34–36 Others have reported that variability of CAC scores is greatest in the low score range and least in the high score range.37 The interpretation of low CAC scores must, therefore, take into account variability in the measurements, especially when interpreting serial scans. The clinical consequences of such variability in CAC scores are not known. Specifically, it is not known if such variability will translate into individuals falling into different risk categories (e.g. CAC score of 0, 1–50, 51–100, 101–300, and >300) and, as a result, if such variability would impact treatment decisions.
Incremental Predictive Use of CAC Scores in a Primary Screening Program
To validate a new biomarker in the setting of screening of asymptomatic individuals, several metrics should be evaluated beyond measures of association (i.e., relative risks). These include a change in discrimination (c statistic), the net reclassification improvement (NRI), and the integrated discrimination improvement (IDI).15, 38 For the screening of asymptomatic individuals, there is evidence that CAC scores improve both the c statistic and the NRI. The MESA study demonstrated that CAC provided a net reclassification improvement of 25% (p<0.001) compared with a model including only the Framingham Risk Score, with 23% of those with events being reclassified to a high-risk category, and 13% of those without events being reclassified to a low-risk category when CAC scores were added to the multivariable model.22 These analyses were, however, limited to estimating the 5-year risk of CHD and excluded participants with diabetes mellitus.22 A more recent analysis of the MESA study with follow-up extended to 7.6 years yielded a much higher NRI of ≈66%.39 The Heinz Nixdorf Recall Study yielded a NRI of ≈31%.25 Similarly, data from the Rotterdam study of subjects >55 years showed an improved predictive capability of the 10-year risk of CHD by addition of CAC scores to the Framingham Risk Score. In total, 51% and 53% of the men and women were reclassified, with the greatest proportion of reclassifications in the intermediate risk group.19 C statistics were significantly improved from 0.72 to 0.76 and NRI was 14% (p < 0.01).19 The St. Francis Heart Study reported a NRI of ≈70% (as cited by Budoff).16, 40 These data indicate that CAC scores consistently improve model discrimination and NRI, yet the range of improvements in the latter varied widely between 14% (weak to intermediate) and 70% (strong),41 highlighting the need for additional studies.
A final concern related to newer biomarkers includes the risk of overestimating their predictive use. In this context, a recent review suggests substantial publication bias associated with most of the newer biomarkers, including measurements of CAC, underscoring the notion that published reports based on observational studies may overestimate their prognostic utility.42
Do Imaging Tests (Such as CAC Scoring) Translate Into a Change in Management and Better Clinical Outcomes in Asymptomatic Individuals?
When considering the value of a new biomarker as a supplement to conventional risk-prediction scores, we need to consider not only the ability for a new biomarker to reclassify CVD risk in patients, but we must evaluate whether the results of the biomarker test will affect treatment decisions and patient outcomes. Three potential benefits from a biomarker test have been suggested by Pletcher and Pignone.43 These include: (1) better patient understanding of the risk of disease, (2) healthier patient behavior, and (3) better clinical decisions. Studies regarding the impact of CCT on patient understanding and behavior are sparse. The Early Identification of Subclinical atherosclerosis by Noninvasive imaging Research (EISNER) prospective randomized trial assigned 2,137 volunteers to undergo vs. not to undergo CCT scanning (2:1) before risk factor counseling. The trial illustrated that those who were offered a CCT scan improved their risk factors more than those who did not undergo CCT.44 The improvements were further shown to be dose dependent with greater improvements in people with higher CAC scores.44 Other studies have failed to report changes in patient behavior upon being provided CAC score results.45–47 Whether CAC testing will translate into beneficial clinical outcomes is, therefore, yet to be determined, and currently data on hard endpoints from randomized trials (i.e., CCT vs. no CCT) are lacking.44 Also, of note, randomized trials of statins have reported clinical benefit without a change in CAC scores, suggesting that regression of CAC may not be a therapeutic target or a tool for monitoring benefits of treatment strategies (as opposed to other risk factors such as high blood pressure, or dyslipidemia).16, 48 It may be reasoned that this argument could be extended to standard risk scoring and biomarkers as well. In this context, a recent meta-analysis suggested that there may be a modest beneficial impact on lifestyle and prophylactic pharmacotherapy associated with the use of global risk scores, perhaps indicating that improving risk factors and patient behaviour with use of any tests is challenging in general.49
It is currently not well established whether the CAC scores modify treatment decisions for the individual people. For individuals with low 10-year risk of CHD, the likelihood of finding a CAC score >0 is so small that the tests are currently not recommended; further, prophylactic treatment is not recommended beyond lifestyle measures to maintain optimal levels of CVD risk factors.14 For people with high risk of CHD (i.e., ≥20% risk of developing CHD within the next 10 years) and possible for selected intermediate-risk individuals (i.e., 10–20% risk) non-pharmacological lifestyle management advice and appropriate pharmacological treatment (based on guidelines) should be offered irrespectively of their CAC status.50 More precisely, guidelines recommend consideration of aspirin treatment for all patients with a 10-year risk of CHD ≥10% without contraindications; statin treatment for those with dyslipidemia (threshold for initiation of treatment depends on risk factor burden with primary goal as follows: LDL-C <160 mg/dL if ≤1 risk factor is present; LDL-C <130 mg/dL if ≥2 risk factors are present and 10-year CHD risk is <20%; or LDL-C <100 mg/dL if ≥2 risk factors are present and 10-year CHD risk is ≥20% or if the patient has diabetes mellitus); and antihypertensive medications for those with hypertension.50 Thus, for most asymptomatic patients, CCT is unlikely to change clinical decision-making with the exception of patients with an intermediate risk who may be managed more aggressively if they have a high CAC score (although randomized clinical trial data are lacking to justify this strategy).
As for the example with Mrs. X and Mr. Y (Table 2), therapies would possible not be affected by CCT findings. Mrs. X had an estimated low risk of CHD based on the Framingham Risk Score (calculated risk 7%), but she had an adverse risk factor profiles including a positive family history of premature CVD, which in reality puts her at a higher risk than estimated by the Framingham Risk Score. Acknowledging this, current guidelines consider a CAC scan appropriate in such an individual.14 However, despite her burden of risk factors, the CAC score turned out to be 0. Based on the low CAC score, the question is whether Mrs. X should be treated less aggressively than if her CAC score was unknown. There is currently lack of data to answer this question, but perhaps a low CAC score should be considered an excellent opportunity for prevention of future CVD rather than declare her to be at lower risk than if her CAC score was unknown? Mr. Y is being classified as having an intermediate risk of CHD based on the Framingham Risk Score (calculated risk 14%) and, therefore, the indication for his CCT was appropriate according to the guidelines. Because his CAC score turned out to be high, the question is whether he should be treated more aggressively than if he had no CCT scan performed? The answer is probably not because current guidelines recommend consideration of aspirin use in all individuals at an intermediate or high 10-year risk of CHD.50 Because Mr. Y had an optimal lipid profile and blood pressure, other prophylactic medications are probably not indicated in his case beyond maintaining healthy lifestyle measures. It is, however, possible that, if his CAC score had turned out to be low aspirin could be omitted (but there are no randomized clinical trial data to support this strategy).
Follow-up Testing after CCT
Concerns have been raised that referral to stress test or coronary angiography after CCT might occur more often than is necessary and that the results from CAC scans may raise additional questions rather than provide easy answers in some cases.51, 52 Yet, the EISNER trial did not show a difference in downstream medical testing between those who did and did not undergo CAC scanning.44 Current guidelines state that stress myocardial perfusion imaging may be considered in asymptomatic individuals at high risk of coronary heart disease, such as those with a CAC score >400 (class IIb recommendation).53 When considering the risk of having significant stenosis based on CAC scores, it is critical to consider the sensitivity, specificity, positive and negative predictive values. The notion of positive predictive value is particularly important in the primary prevention setting. When the prevalence of a disease or a trait is low in the community, it is desirable to have a high specificity. This is because we want to avoid unnecessary anxiety associated with a false positive test, limit unnecessary treatment (and related side effects) and costs. When the setting is one of a high pretest probability (example, individuals with chest pain), we want to maximize sensitivity so as to avoid falsely reassuring someone with a negative test. Data on the sensitivity, specificity, positive, and negative predictive values of a CAC score below and above 0 for predicting coronary atherosclerosis and significant stenoses in asymptomatic people are sparse. Data from the MESA study indicated that a CAC score >0 was associated with a reasonable sensitivity (91%) but a low specificity of 51% and a very low positive predictive value of 2% for having significant stenoses creating the challenge of anxiety related to a false positive test (as cited by Budoff).33, 40 Ho et al.54 reported that the frequency of CT angiographic stenoses increased as CAC scores increased with a significant stenosis (>60% lesion) found in 7.9%, 8.3%, 14.5%, and 27.2% of those with CAC scores of 1 to 100, 101 to 400, 401 to 1,000, and >1,000, respectively. The extent to which individuals shown to have significant angiographic coronary stenosis are referred for invasive revascularizations downstream in a real-world clinical practice is not known. One caveat to be remembered when interpreting predictive values is that, unlike most screening tests in the case of CAC we are predicting events into the future. As such, predictive values of CAC testing may be sensitive to the duration of follow-up. Importantly, however, it is unclear if asymptomatic individuals with higher CAC scores should be referred for coronary angiography, given that there is currently little evidence to support revascularization of asymptomatic people.55
Cost-effectiveness of Imaging Tests
The economic evaluation of any screening or diagnostic test is complex, but a generally accepted measure in this context is the amount spent money on tests per quality-adjusted life years (QALY) gained. Because there are currently no data available that evaluate the improvements in long-term outcomes for screening with CCT, the cost-effectiveness of CCT is somewhat difficult to estimate. The economic value of CCT has, however, been evaluated both in young and middle-aged/older asymptomatic individuals. Using data from the Prospective Army Coronary Calcium (PACC) project of young volunteers recruited from the U.S. army (aged 40–50 years) Taylor et al.56 evaluated the cost-effectiveness of screening of young asymptomatic individuals with CCT.56 Based on the expected relative risk reduction associated with preventive medications and the numbers considered at pre-test risk, the authors estimated that adding CCT to the conventional Framingham risk score was associated with $11,500 to > $1,000,000 per QALY gained.56 One potential interpretation of these data is that in a group of low-risk individuals CCT screening may not be cost-effective. van Kempen et al.57 evaluated the cost-effectiveness associated with CCT screening based on data from the Rotterdam study of middle-aged and elderly individuals at intermediate risk of developing CVD. The study sample had a mean age of 70 and 74 years in men and women. The authors took into consideration economic costs of CCT, cost of preventive medications, benefits and risk of adverse effects of medications (e.g., bleedings with aspirin therapy), and cancer-related risk associated with CCT (see section below). They concluded that screening of intermediate risk patients (i.e., ≥10% risk of coronary heart disease within 10 years) is probably cost-effective in men but unlikely to be so in women (Figure 1).57 Two other recent studies have reported cost-savings associated with CAC screening.21, 44 Another interesting point of view from a public-health perspective illustrated in Figure 1 relates to the wide gap between current practice and current guidelines. If full adherence to the current guidelines would be reached in clinical practice, this would translate into a much larger gain in quality-adjusted life expectancy compared with the additional gain in quality-adjusted life expectancy associated with introduction of CCT beyond the full adherence to current guidelines. Perhaps these data therefore suggest that an improved focus on ‘getting with the guidelines’ may be an effective alternative to implementing CCT for CAC scoring.
Figure 1.
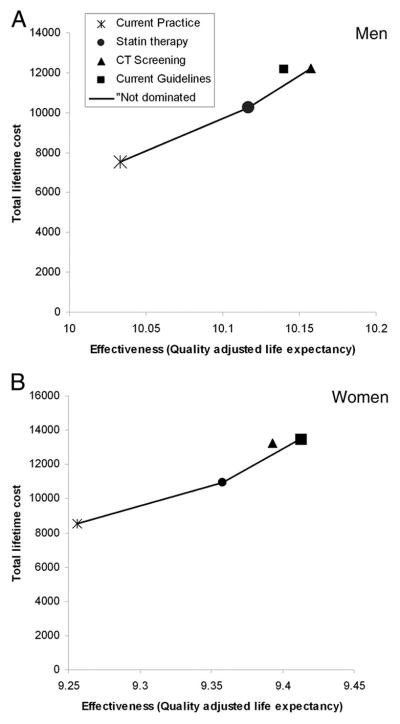
estimated cost-effectiveness associated with CCT screening of middle-age and elderly individuals at intermediate risk of developing CVD. Reprinted from van Kempen et al.57 with permission of the publisher. Copyright © 2011, Elsevier. Authorization for this adaption has been obtrained both from the owner of the copyright work and from the owner of copyright in the translation or adaption.
Other Concerns Associated with Use of CCT: Radiation Exposure and Risk of Incidental Findings Associated with Testing
When tests are performed on asymptomatic individuals, there is a hazard of incidental findings particularly with the use of imaging tests. If the indications for the tests are appropriate, the risk-benefit ratio is favorable. A retrospective review of 1356 individuals referred for CAC screening reported that 278 (20.5%) of the individuals had ≥1 non-cardiac finding on the scanning. Of these 57 (4.2%) individuals were recommended diagnostic CT follow-up.58 To our knowledge, the economic and psychosocial consequences associated with incidental findings in CCT scan screenings have not been adequately investigated.
When using CCT for screening, the risk of cancer induced by radiation exposure must be considered.59 The radiation exposure associated with a typical chest CT examination is ≈3x times the amount of annual natural background radiation exposure and is estimated to be 30x that received from a routine chest x-ray (estimated effective radiation doses are 3 mSv for CCT and 0.1 mSv for a posteroanterior and lateral chest x-ray). It has been suggested that as much as 1.5 to 2% of all cancers in the U.S. are currently attributable to CT scans, a number that has raised from 0.6% in 1996 and may be increasing further as a result of the increase in numbers of procedures performed.60 Although the amount of radiation for 1 scan is small, it will inevitably lead to a significant number of cancers, especially among younger patients and women (who are generally more susceptible to radiation compared with older men). Because the association between radiation and incidence of solid cancers seems to be cumulative, risks increase for each scan performed, arguing that in the setting of primary screening of asymptomatic individuals repetitive scans are inappropriate.61 In this context, it should be noted that more recent protocols have been reported to be associated with radiation exposure of <1 mSv to as low as 0.6 mSv (lower than mammography).62, 63 Clearly additional longitudinal data are warranted as experiences with these newer protocols accrue.
Other Concerns Associated with Use of CCT: That CAC Scores “Overrule” Clinical Risk Factors in Evaluation and Management
It may be argued that CAC scores should not be viewed as a risk factor but rather a marker of subclinical disease. Yet, even as a marker of subclinical disease, its presence (or absence) does not guarantee an adverse (or better) outcome. First, we do not know the long-term prognosis of a low CAC score; second, individuals with a low CAC score but high risk factor burden may still have a high CVD risk; and third, an elevated CAC score in individuals without other risk factors may not be associated with an adverse prognosis in all people, and may theoretically cause unnecessary anxiety and medical therapy (e.g., increased risks of bleeding with aggressive antiplatelet therapy). Of note, the predicted 7-year risk of coronary heart death or nonfatal myocardial infarction for a particular CAC score seemed to differ for the different categories of Framingham Risk Score in the South Bay Heart Watch study.20 As seen in Figure 2, individuals with a CAC score >300 but a Framingham Risk Score of <10% seem to have a much lower risk of suffering from an event than individuals with a CAC score of zero but a Framingham Risk Score of >20%. Thus, it seems important not to consider CAC scores as an absolute key for the future risk of developing overt cardiovascular disease, but rather as a clinical risk marker in line with the Framingham Risk Score.
Figure 2.
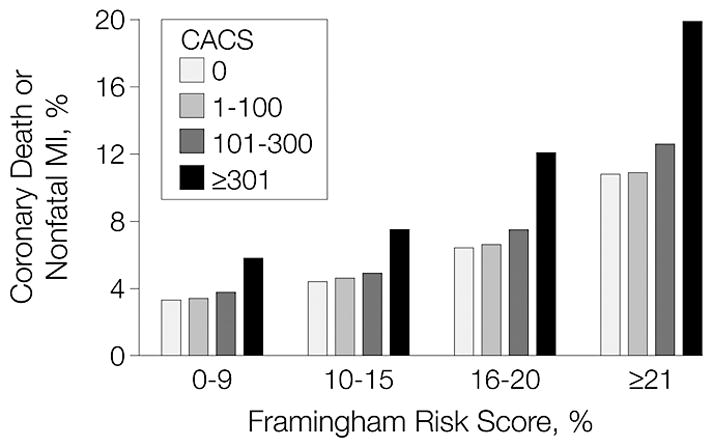
predicted 7-year risk of coronary heart death or nonfatal myocardial infarction for different combinations of coronary artery calcium (CAC) score and Framingham Risk Score in the South Bay Heart Watch study. Reprinted with permission from Greenland et al.20 Copyright © 2004, American Medical Association. Authorization for this adaption has been obtrained both from the owner of the copyright work and from the owner of copyright in the translation or adaption.
Conclusions
Whereas the use of imaging tests in people deemed to be at intermediate risk of coronary disease may be useful in some cases, the routine use of such tests in primary care settings is challenged by lack of data on long-term risk associated with CAC scores, and a lack of evidence that such screening results in a change in patient outcomes. The routine application of such testing in primary care settings is also challenged by the potential psychological burden associated with tests, incidental findings and their implications, radiation exposure (for select imaging tests) and associated cancer risks, and associated costs to the already-stressed health care systems.
Acknowledgments
Sources of Funding
This work was funded in part by N01-HC-25195. Dr. Andersson was supported by an independent research grant from the Danish agency for science, technology, and innovation (the Danish Medical Research Council, grant no. FSS - 11-120873).
Footnotes
Footnote appearing at page 1 in the published paper: “This article was submitted before the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults was released. Per these recent guidelines, Mr Y (Table 2) may meet indications for consideration for statin treatment”.
Conflicts of Interest Disclosures
None.
References
- 1.Fox CS, Pencina MJ, Wilson PW, Paynter NP, Vasan RS, D’Agostino RB., Sr Lifetime risk of cardiovascular disease among individuals with and without diabetes stratified by obesity status in the framingham heart study. Diabetes Care. 2008;31:1582–1584. doi: 10.2337/dc08-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. Jama. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: The framingham heart study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 5.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 6.Pencina MJ, D’Agostino RB, Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: The framingham heart study. Circulation. 2009;119:3078–3084. doi: 10.1161/CIRCULATIONAHA.108.816694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brindle P, Beswick A, Fahey T, Ebrahim S. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: A systematic review. Heart. 2006;92:1752–1759. doi: 10.1136/hrt.2006.087932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andresdottir MB, Sigurdsson G, Sigvaldason H, Gudnason V. Fifteen percent of myocardial infarctions and coronary revascularizations explained by family history unrelated to conventional risk factors. The reykjavik cohort study. Eur Heart J. 2002;23:1655–1663. doi: 10.1053/euhj.2002.3235. [DOI] [PubMed] [Google Scholar]
- 9.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: A prospective study of parents and offspring. Jama. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen M, Andersson C, Gerds TA, Andersen PK, Jensen TB, Kober L, Gislason G, Torp-Pedersen C. Familial clustering of myocardial infarction in first-degree relatives: A nationwide study. Eur Heart J. 2013;34:1198–1203. doi: 10.1093/eurheartj/ehs475. [DOI] [PubMed] [Google Scholar]
- 11.Nasir K, Michos ED, Rumberger JA, Braunstein JB, Post WS, Budoff MJ, Blumenthal RS. Coronary artery calcification and family history of premature coronary heart disease: Sibling history is more strongly associated than parental history. Circulation. 2004;110:2150–2156. doi: 10.1161/01.CIR.0000144464.11080.14. [DOI] [PubMed] [Google Scholar]
- 12.Parikh NI, Hwang SJ, Larson MG, Cupples LA, Fox CS, Manders ES, Murabito JM, Massaro JM, Hoffmann U, O’Donnell CJ. Parental occurrence of premature cardiovascular disease predicts increased coronary artery and abdominal aortic calcification in the framingham offspring and third generation cohorts. Circulation. 2007;116:1473–1481. doi: 10.1161/CIRCULATIONAHA.107.705202. [DOI] [PubMed] [Google Scholar]
- 13.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG, Lauer MS, Shaw LJ, Smith SC, Jr, Taylor AJ, Weintraub WS, Wenger NK, Jacobs AK, Anderson JL, Albert N, Buller CE, Creager MA, Ettinger SM, Guyton RA, Halperin JL, Hochman JS, Nishimura R, Ohman EM, Page RL, Stevenson WG, Tarkington LG, Yancy CW. 2010 accf/aha guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. J Am Coll Cardiol. 2010;56:e50–103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, Rubin GD, Kramer CM, Berman D, Brown A, Chaudhry FA, Cury RC, Desai MY, Einstein AJ, Gomes AS, Harrington R, Hoffmann U, Khare R, Lesser J, McGann C, Rosenberg A, Schwartz R, Shelton M, Smetana GW, Smith SC., Jr Accf/scct/acr/aha/ase/asnc/nasci/scai/scmr 2010 appropriate use criteria for cardiac computed tomography. A report of the american college of cardiology foundation appropriate use criteria task force, the society of cardiovascular computed tomography, the american college of radiology, the american heart association, the american society of echocardiography, the american society of nuclear cardiology, the north american society for cardiovascular imaging, the society for cardiovascular angiography and interventions, and the society for cardiovascular magnetic resonance. J Am Coll Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MS, Go AS, Harrell FE, Jr, Hong Y, Howard BV, Howard VJ, Hsue PY, Kramer CM, McConnell JP, Normand SL, O’Donnell CJ, Smith SC, Jr, Wilson PW American Heart Association Expert Panel on Subclinical Atherosclerotic D, Emerging Risk F, the Stroke C. Criteria for evaluation of novel markers of cardiovascular risk: A scientific statement from the american heart association. Circulation. 2009;119:2408–2416. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–1260. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 17.Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, O’Leary DH, Lima J, Blumenthal RS, Nasir K. Associations between c-reactive protein, coronary artery calcium, and cardiovascular events: Implications for the jupiter population from mesa, a population-based cohort study. Lancet. 2011;378:684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, Kondos G, Kronmal RA. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: Mesa (multi-ethnic study of atherosclerosis) J Am Coll Cardiol. 2009;53:345–352. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elias-Smale SE, Proenca RV, Koller MT, Kavousi M, van Rooij FJ, Hunink MG, Steyerberg EW, Hofman A, Oudkerk M, Witteman JC. Coronary calcium score improves classification of coronary heart disease risk in the elderly: The rotterdam study. J Am Coll Cardiol. 2010;56:1407–1414. doi: 10.1016/j.jacc.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 20.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with framingham score for risk prediction in asymptomatic individuals. Jama. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 21.LaMonte MJ, FitzGerald SJ, Church TS, Barlow CE, Radford NB, Levine BD, Pippin JJ, Gibbons LW, Blair SN, Nichaman MZ. Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. American journal of epidemiology. 2005;162:421–429. doi: 10.1093/aje/kwi228. [DOI] [PubMed] [Google Scholar]
- 22.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. Jama. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, Witteman JC. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112:572–577. doi: 10.1161/CIRCULATIONAHA.104.488916. [DOI] [PubMed] [Google Scholar]
- 24.McEvoy JW, Blaha MJ, Defilippis AP, Budoff MJ, Nasir K, Blumenthal RS, Jones SR. Coronary artery calcium progression: An important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56:1613–1622. doi: 10.1016/j.jacc.2010.06.038. [DOI] [PubMed] [Google Scholar]
- 25.Erbel R, Mohlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Gronemeyer D, Seibel R, Kalsch H, Brocker-Preuss M, Mann K, Siegrist J, Jockel KH Heinz Nixdorf Recall Study Investigative G. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: The heinz nixdorf recall study. J Am Coll Cardiol. 2010;56:1397–1406. doi: 10.1016/j.jacc.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 26.Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, Rozanski A, Callister TQ. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: What is the “warranty period” for remaining normal? J Am Coll Cardiol. 2010;55:1110–1117. doi: 10.1016/j.jacc.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 27.Budoff MJ, Lane KL, Bakhsheshi H, Mao S, Grassmann BO, Friedman BC, Brundage BH. Rates of progression of coronary calcium by electron beam tomography. Am J Cardiol. 2000;86:8–11. doi: 10.1016/s0002-9149(00)00820-1. [DOI] [PubMed] [Google Scholar]
- 28.Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, Detrano RC, Bild DE, Guerci AD, Liu K, Shea S, Szklo M, Post W, Lima J, Bertoni A, Wong ND. Progression of coronary calcium and incident coronary heart disease events: Mesa (multi-ethnic study of atherosclerosis) J Am Coll Cardiol. 2013;61:1231–1239. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gopal A, Nasir K, Liu ST, Flores FR, Chen L, Budoff MJ. Coronary calcium progression rates with a zero initial score by electron beam tomography. International journal of cardiology. 2007;117:227–231. doi: 10.1016/j.ijcard.2006.04.081. [DOI] [PubMed] [Google Scholar]
- 30.Pletcher MJ, Tice JA, Pignone M, McCulloch C, Callister TQ, Browner WS. What does my patient’s coronary artery calcium score mean? Combining information from the coronary artery calcium score with information from conventional risk factors to estimate coronary heart disease risk. BMC Med. 2004;2:31. doi: 10.1186/1741-7015-2-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: Results from the multi-ethnic study of atherosclerosis (mesa) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 32.Jain T, Peshock R, McGuire DK, Willett D, Yu Z, Vega GL, Guerra R, Hobbs HH, Grundy SM. African americans and caucasians have a similar prevalence of coronary calcium in the dallas heart study. J Am Coll Cardiol. 2004;44:1011–1017. doi: 10.1016/j.jacc.2004.05.069. [DOI] [PubMed] [Google Scholar]
- 33.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 34.Achenbach S, Ropers D, Mohlenkamp S, Schmermund A, Muschiol G, Groth J, Kusus M, Regenfus M, Daniel WG, Erbel R, Moshage W. Variability of repeated coronary artery calcium measurements by electron beam tomography. Am J Cardiol. 2001;87:210–213. A218. doi: 10.1016/s0002-9149(00)01319-9. [DOI] [PubMed] [Google Scholar]
- 35.Bielak LF, Sheedy PF, 2nd, Peyser PA. Coronary artery calcification measured at electron-beam ct: Agreement in dual scan runs and change over time. Radiology. 2001;218:224–229. doi: 10.1148/radiology.218.1.r01ja34224. [DOI] [PubMed] [Google Scholar]
- 36.Budoff MJ, McClelland RL, Chung H, Wong ND, Carr JJ, McNitt-Gray M, Blumenthal RS, Detrano RC. Reproducibility of coronary artery calcified plaque with cardiac 64-mdct: The multi-ethnic study of atherosclerosis. AJR Am J Roentgenol. 2009;192:613–617. doi: 10.2214/AJR.08.1242. [DOI] [PubMed] [Google Scholar]
- 37.Moser KW, O’Keefe JH, Jr, Bateman TM, McGhie IA. Coronary calcium screening in asymptomatic patients as a guide to risk factor modification and stress myocardial perfusion imaging. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology. 2003;10:590–598. doi: 10.1016/s1071-3581(03)00653-6. [DOI] [PubMed] [Google Scholar]
- 38.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: From area under the roc curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207-112. [DOI] [PubMed] [Google Scholar]
- 39.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, Carr JJ, Goff DC, Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. Jama. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Budoff MJ. Screening for ischemic heart disease with cardiac ct: Current recommendations. Scientifica. 2012;2012:12. doi: 10.6064/2012/812046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pencina MJ, D’Agostino RB, Pencina KM, Janssens AC, Greenland P. Interpreting incremental value of markers added to risk prediction models. American journal of epidemiology. 2012;176:473–481. doi: 10.1093/aje/kws207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tzoulaki I, Siontis KC, Evangelou E, Ioannidis JP. Bias in associations of emerging biomarkers with cardiovascular disease. JAMA Intern Med. 2013:1–8. doi: 10.1001/jamainternmed.2013.3018. [DOI] [PubMed] [Google Scholar]
- 43.Pletcher MJ, Pignone M. Evaluating the clinical utility of a biomarker: A review of methods for estimating health impact. Circulation. 2011;123:1116–1124. doi: 10.1161/CIRCULATIONAHA.110.943860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, Rana JS, Orakzai R, Hayes SW, Friedman JD, Thomson LE, Polk D, Min J, Budoff MJ, Berman DS. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the eisner (early identification of subclinical atherosclerosis by noninvasive imaging research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. doi: 10.1016/j.jacc.2011.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong ND, Detrano RC, Diamond G, Rezayat C, Mahmoudi R, Chong EC, Tang W, Puentes G, Kang X, Abrahamson D. Does coronary artery screening by electron beam computed tomography motivate potentially beneficial lifestyle behaviors? Am J Cardiol. 1996;78:1220–1223. doi: 10.1016/s0002-9149(96)00599-1. [DOI] [PubMed] [Google Scholar]
- 46.O’Malley PG, Feuerstein IM, Taylor AJ. Impact of electron beam tomography, with or without case management, on motivation, behavioral change, and cardiovascular risk profile: A randomized controlled trial. Jama. 2003;289:2215–2223. doi: 10.1001/jama.289.17.2215. [DOI] [PubMed] [Google Scholar]
- 47.O’Malley PG, Rupard EJ, Jones DL, Feuerstein I, Brazaitis M, Taylor AJ. Does the diagnosis of coronary calcification with electron beam computed tomography motivate behavioral change in smokers? Military medicine. 2002;167:211–214. [PubMed] [Google Scholar]
- 48.Schmermund A, Achenbach S, Budde T, Buziashvili Y, Forster A, Friedrich G, Henein M, Kerkhoff G, Knollmann F, Kukharchuk V, Lahiri A, Leischik R, Moshage W, Schartl M, Siffert W, Steinhagen-Thiessen E, Sinitsyn V, Vogt A, Wiedeking B, Erbel R. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: A multicenter, randomized, double-blind trial. Circulation. 2006;113:427–437. doi: 10.1161/CIRCULATIONAHA.105.568147. [DOI] [PubMed] [Google Scholar]
- 49.Sheridan SL, Crespo E. Does the routine use of global coronary heart disease risk scores translate into clinical benefits or harms? A systematic review of the literature. BMC health services research. 2008;8:60. doi: 10.1186/1472-6963-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, Franklin BA, Goldstein LB, Greenland P, Grundy SM, Hong Y, Miller NH, Lauer RM, Ockene IS, Sacco RL, Sallis JF, Jr, Smith SC, Jr, Stone NJ, Taubert KA. Aha guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: Consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American heart association science advisory and coordinating committee. Circulation. 2002;106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 51.Redberg R, Katz M, Grady D. Diagnostic tests: Another frontier for less is more: Or why talking to your patient is a safe and effective method of reassurance. Archives of internal medicine. 2011;171:619. doi: 10.1001/archinternmed.2010.465. [DOI] [PubMed] [Google Scholar]
- 52.Redberg RF. What is the prognostic value of a zero calcium score? J Am Coll Cardiol. 2010;55:635–636. doi: 10.1016/j.jacc.2009.08.076. [DOI] [PubMed] [Google Scholar]
- 53.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG, Lauer MS, Shaw LJ, Smith SC, Jr, Taylor AJ, Weintraub WS, Wenger NK, Jacobs AK, Smith SC, Jr, Anderson JL, Albert N, Buller CE, Creager MA, Ettinger SM, Guyton RA, Halperin JL, Hochman JS, Kushner FG, Nishimura R, Ohman EM, Page RL, Stevenson WG, Tarkington LG, Yancy CW American College of Cardiology F, American Heart A. 2010 accf/aha guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. J Am Coll Cardiol. 2010;56:e50–103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 54.Ho JS, Fitzgerald SJ, Stolfus LL, Wade WA, Reinhardt DB, Barlow CE, Cannaday JJ. Relation of a coronary artery calcium score higher than 400 to coronary stenoses detected using multidetector computed tomography and to traditional cardiovascular risk factors. Am J Cardiol. 2008;101:1444–1447. doi: 10.1016/j.amjcard.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 55.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. Accf/scai/sts/aats/aha/asnc/hfsa/scct 2012 appropriate use criteria for coronary revascularization focused update: A report of the american college of cardiology foundation appropriate use criteria task force, society for cardiovascular angiography and interventions, society of thoracic surgeons, american association for thoracic surgery, american heart association, american society of nuclear cardiology, and the society of cardiovascular computed tomography. J Am Coll Cardiol. 2012;59:857–881. doi: 10.1016/j.jacc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 56.Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: Mean three-year outcomes in the prospective army coronary calcium (pacc) project. J Am Coll Cardiol. 2005;46:807–814. doi: 10.1016/j.jacc.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 57.van Kempen BJ, Spronk S, Koller MT, Elias-Smale SE, Fleischmann KE, Ikram MA, Krestin GP, Hofman A, Witteman JC, Hunink MG. Comparative effectiveness and cost-effectiveness of computed tomography screening for coronary artery calcium in asymptomatic individuals. J Am Coll Cardiol. 2011;58:1690–1701. doi: 10.1016/j.jacc.2011.05.056. [DOI] [PubMed] [Google Scholar]
- 58.Schragin JG, Weissfeld JL, Edmundowicz D, Strollo DC, Fuhrman CR. Non-cardiac findings on coronary electron beam computed tomography scanning. J Thorac Imaging. 2004;19:82–86. doi: 10.1097/00005382-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Berrington de Gonzalez A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C. Projected cancer risks from computed tomographic scans performed in the united states in 2007. Archives of internal medicine. 2009;169:2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mettler FA, Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: A catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 61.Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950–1997. Radiat Res. 2003;160:381–407. doi: 10.1667/rr3049. [DOI] [PubMed] [Google Scholar]
- 62.deGoma EM, Karlsberg RP, Judelson DR, Budoff MJ. The underappreciated impact of heart disease. Women’s health issues: official publication of the Jacobs Institute of Women’s Health. 2010;20:299–303. doi: 10.1016/j.whi.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 63.Nakazato R, Dey D, Gutstein A, Le Meunier L, Cheng VY, Pimentel R, Paz W, Hayes SW, Thomson LE, Friedman JD, Berman DS. Coronary artery calcium scoring using a reduced tube voltage and radiation dose protocol with dual-source computed tomography. Journal of cardiovascular computed tomography. 2009;3:394–400. doi: 10.1016/j.jcct.2009.10.002. [DOI] [PubMed] [Google Scholar]


