Abstract
Background and aims: Exercise addiction receives substantial attention in the field of behavioral addictions. It is a unique form of addiction because in contrast to other addictive disorders it is carried out with major physical-effort and high energy expenditure. Methods: A critical literature review was performed. Results: The literature evaluation shows that most published accounts report the levels of risk for exercise addiction rather than actual cases or morbidities. The inconsistent prevalence of exercise addiction, ranging from 0.3% to 77.0%, reported in the literature may be ascribed to incomplete conceptual models for the morbidity. Current explanations of exercise addiction may suggest that the disorder is progressive from healthy to unhealthy exercise pattern. This approach drives research into the wrong direction. Discussion: An interactional model is offered accounting for the adoption, maintenance, and transformation of exercise behavior. The here proposed model has an idiosyncratic black-box containing the antecedents and characteristics that are unique to the individual, which cannot be researched via the nomothetic approach. Subjective aspects in the black-box interact with stressful life events that force the person to cope. The range of coping may be wide. Escape into exercise depends on personal (subjective) and situational (objective) factors, but the subjective components are inaccessible for a priori scholastic scrutiny. It is our view that currently only this dual interactional model may account for the fact that exercise addiction emerges suddenly and only in a few individuals from among those at high risk, estimated to be around 3.0% of the exercising population.
Keywords: dependence, exercise abuse, research, review, theory, transformation
INTRODUCTION
Exercise addiction within behavioral addictions
Currently three types of addictions are known in the scholastic literature: 1) substance or chemical addictions, 2) behavioral (non-chemical or non-pharmacological) addictions, and 3) food addictions (Egorov, 2013). Behavioral addictions are compulsive psychological and physiological urges for one or more specific behaviors. There is increased attention devoted to this group of morbidities by researchers in the field. A category of “Behavioral Addiction” is included into the new DSM-V (American Psychiatric Association, 2013). While there are many forms of behavioral addictions with wide range of consequences, the DSM-V category of behavioral addictions only includes gambling addiction. Internet addiction was also considered for inclusion into this category, but there was no consensus in the working group. Therefore, Internet addiction is only included in the manual's appendix to encourage further research. Exercise addiction, after over four decades of scholastic interest and research on the topic, is still left out from the DSM-V.
It is becoming increasingly more evident that people could become addicted to various behaviors. In addition to behavioral addiction to gambling recognized in the DSM-V (Parke & Griffiths, 2004), new forms of addictive behaviors have surfaced in the medical literature. Indeed, numerous individuals spend too much time at work (workaholism – Scottl, Moore & Miceli, 1997), or online (Internet addiction – Young, 1998). Some are too fond of shopping (shopping addiction – Krueger, 1988), watching television (addiction to television – Kubey & Csikszentmihalyi, 2002), overindulging in porn or sexual activity (sexual addiction – Carnes, 1983), or physical activity (exercise addiction – Szabo, 2010), or even tango dancing (dance addiction – Targhetta, Nalpas & Perney, 2013). While to date relatively little attention has been devoted to the understanding and treatment of these “imprisoning” behaviors, they should no longer be ignored. As pointed out by Martin and Petry (2005), non-chemical addictions may not only resemble, but they also share a common neurobiological mechanism with alcohol or drug addictions. Thus behavioral addictions are not only possible, but they are preponderant in the daily human life (Holden, 2001) – regardless of the recognition and/or consensus of the DSM-V working group – and may be more common than expected, because it is difficult to detect them as they very often blend into the normal spectrum of the daily human activities. Indeed, behavioral addictions are often as serious in their consequences as alcohol or drug addictions (Martin & Petry, 2005). A majority of non-pharmacological addictions are usually encountered within a family context and often seem to be fostered by family processes (J.Y. Yen, C.F. Yen, C.C. Chen, S.H. Chen & Ko, 2007). Therefore, family therapy is usually a first option in treating the variety of non-pharmacological addictions at individual-clinical (idiosyncratic cases), rather than group-research level.
There are several new attempts to classify behavioral addictions. Egorov (2007, 2013) offered a working classification of non-chemical forms of addictive behavior (Table 1). In this classification Glasser's (1976, 2012) concept of positive addiction has been incorporated in a context of mundane humane behaviors that under ordinary circumstances may make the individual stronger and happier. These behaviors, however, turn into negative addictions or psychopathology once they start to be abused to the point where they result in harm to both the affected individual and her/his social surroundings.
Table 1.
Working classification of non-chemical forms of addictive behavior (Egorov, 2007, 2013)
| Gambling addiction | Erotic addiction | Positive (or socially accepted) addictions (Glasser, 1976) | Technological addictions | Food addictions |
| Gambling and betting addictions | Love addiction | Workaholism or work addiction | Internet addiction1 | Overeating addiction |
| Sexual addiction | Exercise addiction2 | Mobile phone addiction | Starvation-diet related addiction | |
| Mixed love-sex, partner addiction | Shopping addiction (compulsive buying) | Television addiction | ||
| Pornography addiction | Religious addiction | |||
| Relationship addiction |
Internet addiction includes: Internet-gamblers, Internet-gamers, Internet-workaholics, Internet-sexaholics, Internet-erotaholics, Internet-shopaholics, Internet relationship and social networking addicts.
Exercise addiction does not include excessive exercise observed as symptom in eating disorders.
Physical exercise is one of the behaviors that benefits people both physically and mentally and, therefore, its regular practice may be beneficial and viewed by Glasser (2012) – and perhaps many others – as therapeutic. Recently, Glasser highlighted that in certain cases self-improving behaviors like exercise or meditation could become addictive and this form of addiction builds strength in the person and promotes a happier and healthier living. This is a view that in conjunction with the clinically diagnosed cases of exercise addiction (Griffiths, 1997) confers a paradoxical role for exercise behavior. Indeed, habitual or committed forms of exercise may be therapeutic, while loss of control renders the behavior pathogenic. In this analytical account the current models forwarded for exercise addiction are reconsidered. Then in an attempt to segregate risk assessment (nomothetic approach via questionnaire-screening) and clinical diagnosis of exercise addiction, an alternative interactional model is proposed for the better understanding of the exercise paradox.
EXERCISE ADDICTION
In the past decades several publications dealing with exercise addiction have emerged. Research into highly accustomed exercise started with a work that investigated the effects of exercise deprivation on sleep patterns (Baekeland, 1970). The author of the study faced great difficulties in recruiting highly committed athletes (exercising 5–6 days a week), who would be willing to give up their training for one month. In fact, eligible potential participants have refused to participate in the experiment even when they were offered cash reward. Baekeland was only able to recruit athletes who trained only 3–4 times a week. During the month of the deprivation, these participants reported negative psychological well-being, which surfaced as high level of anxiety, frequent night awakenings, and sexual tension.
Later the concept of addiction to exercise was first introduced by Sachs and Pargman (1984). The authors have used the term running addiction to describe the source of a set of withdrawal symptoms that surface during periods of running deprivation: anxiety, tension, irritability, muscle twitching, etc. However, earlier, Morgan (1979) also provided examples in which runners continued to run, despite the adverse circumstances (for example, various injuries), which should reduce or interrupt training. Diagnosed clinical cases of exercise addiction in all kinds of sports – martial arts, weight lifting, and body building – were only reported later (Griffiths, 1997; Hurst, Hale, Smith & Collins, 2000; Murphy, 1994). These clinical cases of exercise addiction are characterized by loss of control over the exercise behavior, which is performed as “obligation” rather than for enjoyment, and also have negative physical and psychosocial consequences for the individual. Symptoms include all components of addictive disorders: salience, withdrawal, mood modification, conflict, tolerance, and relapse (Szabo, 2010). In light of this definition pathogenic exercisers could be distinguished from the other high-volume exercisers, like athletes, who maintain control over their training, have a fixed schedule of training to also meet other life-obligations, and encounter no harmful or negative consequences as a result of their intensive training.
To avoid a conceptual confound, it should be mentioned that De Coverley Veale (1987) differentiated between primary and secondary exercise addiction. In this article only primary exercise addiction is considered because secondary exercise addiction is a symptom in a number of eating disorders including Anorexia Nervosa and Bulimia Nervosa (De Coverley Veale, 1987). In these disorders, excessive exercise is a means for caloric control and weight loss rather than for escape from a psychological hardship. Secondary exercise addiction as a symptom in eating disorders occurs in different “doses” in people affected by eating disorders. It was estimated that one third of anorectics may be affected (Crisp, Hsu, Harding & Hartshorn, 1980).
ESTIMATED PREVALENCE OF EXERCISE ADDICTION
Mass screening for exercise addiction takes place by using psychometrically validated questionnaires. Two instruments that prove to be similar in sensitivity and reliability (Mónok et al., 2012) are the Exercise Dependence Scale (EDS, 21 items; Hausenblas & Downs, 2002) and the Exercise Addiction Inventory (EAI, 6 items; Terry, Szabo & Griffiths, 2004). These scales do not convey exact – or accurate – information about the actual prevalence of exercise addictions since they are screening- rather than diagnosis-tools. Indeed, the estimates based on these questionnaires should be interpreted as symptomatic or at risk for exercise addiction as also noted be the developers of the tools (Hausenblas & Downs, 2002; Terry et al., 2004).
A number of inquiries were conducted on convenience samples of university students. Hausenblas and Downs (2002) reported that between 3.4% and 13.4% of their samples were at high risk for exercise addiction. The lower figure was also confirmed by Griffiths, Szabo and Terry (2005) who reported that 3.0% of university students could be at-risk of exercise addiction. Later Szabo and Griffiths (2007) confirmed that the prevalence of risk for exercise addiction is about 3.6% in the general exercising population, while the figure is nearly double (6.9%) in British Sport Science undergraduates. The study by Hausenblas and Downs (2002) was conducting by using the EDS, whereas the other two by using the EAI. Nevertheless, the two instruments yielded comparable results in American and British samples. Recently, in a Hungarian population-wide study (Mónok et al., 2012) the proportion of exercisers at-risk for addiction was 1.9% among exercisers and 0.3% in the general population as gauged with the EDS. However, the EAI yielded slightly higher figures, 3.2% in habitual exercisers and 0.5% in the general population. Mónok et al. (2012) attributed the discrepancy to a lack of an empirically established cut-off point for the EAI. In spite of the slight discrepancy between the EDS and EAI they appear to project a “close estimation” of the prevalence of risk for exercise addiction in committed exercisers (Sussman, Lisha & Griffiths, 2011a). Several investigations that used other instruments than the EDS and EAI in the scrutiny of the risk for exercise addiction have found exaggerated or unlikely figures for the morbidity, as summarized in Table 2.
Table 2. Prevalence of exercise addiction according to extant reports in the scholastic literature.
| Year | Author(s) | Sample studied | Measure(s) used | Prevalence (%) |
|---|---|---|---|---|
| 1995 | Thornton & Scott | Runners | Commitment to Running Scale (CRS – Carmack & Martens, 1979) | 77% |
| 1998 | Slay et al. | Runners | Obligatory Running Questionnaire (Blumenthal, O'Toole & Chang, 1985) | 26.2% of male runners, 25% of female runners |
| 2000 | Bamber, Cockerill & Carroll | Mixed exercisers and university students | Exercise Dependence Questionnaire (EDQ – Ogden, Veale & Summers, 1997) | 14.8% and 9% also suffering of eating disorders |
| 2002 | Ackard, Brehm & Steffen | Female university exercisers | Obligatory Exercise Questionnaire (Pasman & Thompson, 1988) | 8.0% |
| 2002 | Blaydon & Lindner | Triathletes | EDQ | 30.4% primary and 20.6% secondary exercise addiction |
| 2002 | Hausenblas & Downs | University students | Exercise Dependence Scale (EDS – Hausenblas & Downs, 2002) | 3.4% and 13.4% in two studies |
| 2004 | Downs, Hausenblas & Nigg | University students | EDS-Revised (EDS-R – Downs et al., 2004) | 3.6% and 5.0% in two studies |
| 2005 | Griffiths et al. | University students | Exercise Addiction Inventory (EAI – Terry et al., 2004) | 3.0% |
| 2007 | Allegre, Therme & Griffiths | Ultra-marathoners | EDS-R (French) | 3.2% |
| 2007 | Szabo & Griffiths | Habitual exercisers and Sport Science students | Exercise Addiction Inventory (EAI – Terry et al., 2004) | 3.6% in habitual exercisers, 6.9% in Sport Science undergraduates |
| 2007 | Youngman | Triathletes | EAI | 19.9% |
| 2008 | Lejoyeux, Avril, Richoux,Embouazza & Nivoli | Fitness centre attendees | Interview and own questionnaire | 42% |
| 2009 | Modolo et al. (cf. Modolo et al., 2011) | Various amateur athletes | Negative addiction Scale (NAS – Hailey & Bailey, 1982) | 32% |
| 2010 | Smith, Wright & Winrow | Competitive runners | EDS and Running Addiction Scale (RAS – Chapman & De Castro, 1990) | 50% |
| 2011 | Grandi, Clementi, Guidi, Benassi & Tossani 2011 | Habitual exercisers | EDQ (Italian) | 40.5% |
| 2011 | Villella et al. | High school students | EAI (Italian) | 8.5% |
| 2012 | Costa, Cuzzocrea, Hausenblas, Larcan & Oliva | Fitness centre attendees | EDS-R (Italian) | 6.6% |
| 2012 | Lejoyeux, Guillot, Chalvin, Petit & Lequen | Fitness centre attendees | EAI (French) and own questionnaire | 29.6% |
| 2012 | McNamara & McCabe | Elite athletes | The Exercise Dependence and Elite Athletes Scale (EDEAS – McNamara & McCabe, 2013) | 34.8% |
| 2012 | Mónok et al. | Population-wide study | EDS and EAI (Hungarian) | 0.3% on EDS and 0.5% on EAI in general population; 1.9% on EDS and 3.2% on EAI in regular exercisers |
| 2013 | Lichtenstein, Christiansen, Bilenberg & Støving | Exercisers and soccer players | EAI (Danish) | 5.8% |
| 2013 | Menczel et al. | Fitness centre attendees | EDS & EAI (Hungarian) | 1.8% + 1.8% who exhibited both exercise addiction and eating disorders |
Although researchers have stressed that actual cases of exercise addiction are rare (Szabo, 2000; Veale, 1995) especially when compared to other addictions (Sussman et al., 2011b), figures of above 40% prevalence, published in the past five years, suggest that the psychopathology is not well understood among scholars. The diversity in instruments used, samples, and methods of inquiry – as well as some possible cross-cultural issues that were not addressed to date – may all contribute to the inconsistencies seen in Table 2. Further, as noted earlier, the questionnaire-based studies could only estimate the preponderance of the “at-risk” exercisers rather than actual clinical cases. Consequently, the latter may be even lower than the estimates based on the population-wide results reported recently (Mónok et al., 2012).
THEORETICAL MODELS FOR EXERCISE ADDICTION
The apparent lack of understanding of the exercise paradox, begs for sound theory-driven research. In his 2010 monograph, Szabo presented two specific models for exercise addiction and several models that try to explain the psychological beneficence of exercise, which in turn could be indirectly linked to exercise addiction. In the current paper only the specific models are dealt with. The Sympathetic Arousal Hypothesis (Thompson & Blanton, 1987) is physiological model suggesting how adaptation of the organisms to habitual exercise may lead to addiction. Briefly, adaptation to exercise lowers the body's sympathetic activity. Lower sympathetic activity at rest means lower level of arousal. This new baseline or resting level of arousal may not be adequate for various daily activities. It may be experienced as a lethargic or energy-lacking state. This feeling prompts the person to do something about it, or to increase her/his arousal. One means to do that is exercise. However, the effects of exercise in increasing arousal are only temporary and, therefore, more and more bouts of exercise may be needed to trigger an optimal state of arousal (Figure 1). Further, not only the frequency but also the volume of exercise may need to be increased due to training effect. Such an increase accounts for the tolerance in the addiction process. The main dilemma with this model is that sympathetic adaptation to exercise is universal, so it occurs in everyone, but only about 3% of the regular exercises may become addicted to the behavior (Sussman et al., 2011a).
Figure 1.
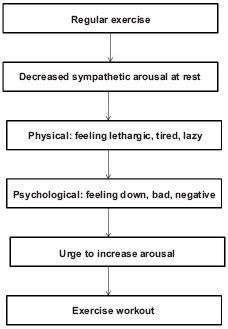
The Sympathetic Arousal Hypothesis
The second model presented by Szabo (2010) was the Cognitive Appraisal Hypothesis (Szabo, 1995). This model takes in consideration life-stress – that requires challenge beyond one's perceived resources – in the addiction model. Some (but it is unknown who) exercisers may try to escape from an ongoing or a sudden stress by resorting to exercise as the means of coping with stress. Once exercise is the coping method with stress, the person depends on it to function well. She/he believes that exercise is a healthy means of coping with stress based on information from scholastic and public information sources. Therefore, the person is using rationalization to explain the exaggerated amount of exercise that progressively takes a tool on other obligations and daily activities. However, when interference of exercise with other life-obligations forces the individual to reduce the amount of exercise, psychological hardship emerges in form of withdrawal symptoms. Loss of exercise also means the loss of the coping mechanism. Consequently, the exerciser loses control, which generates greater vulnerability to stress by further amplifying the negative feelings associated with the lack of exercise. The problem could be resolved only through resuming the previous pattern of exercise often at the expense of the other obligations in the daily life (Figure 2). While this model depicts exercise addiction as coping or escape, it only accounts for maintenance of addiction, but not its onset.
Figure 2.
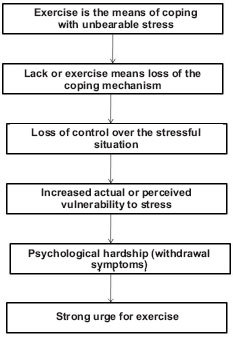
The Cognitive Appraisal Hypothesis
Based on: Thompson & Blanton (1987).
A “Four Phase” model for exercise addiction was proposed by Freimuth, Moniz and Kim (2011). The first phase is characterized by pleasurable activity while the behavior is under control. There are no major negative consequences in general, but muscles soreness or minor strains may occur. In phase two, the psychological beneficence of exercise is realized and the mood-modifying effects may be adopted for coping with hardship. Addiction is most likely to occur when exercise becomes the primary or the sole means of coping with stress. This part of the model may address the onset of exercise addiction, but it does not specify two key issues: 1) a distress must exist, whether progressively mounting or suddenly appearing, and 2) under what conditions or influences will exercise be adopted for coping with stress? The third phase is characterized by the rigid organization of daily obligations around exercise, negative consequences due to exaggerated exercise, and several forms of exercise either for replacing or complementing the habitual mode of exercise. Further, exercise is performed individually, rather than with friends, in a team, or during scheduled fitness classes. The fourth or the last stage encompasses the typical symptoms of fully manifested addiction like salience, tolerance, conflict, need for mood modification and the avoidance of withdrawal symptoms and relapse. While the model is appealing indeed, it does not account for the choice of coping mechanism, or who and why from among the exercise population will turn to this form of time and major energy requiring means of coping with adversity (Figure 3).
Figure 3.
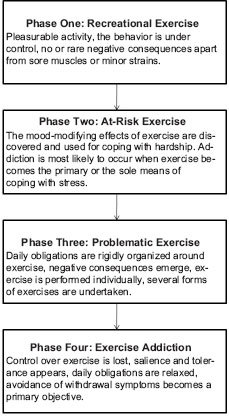
The “Four Phase” model for exercise addiction
Based on: Szabo (1995).
Based on: Freimuth, Moniz & Kim (2011).
A “Biopsychosocial” model for exercise addiction in elite athletes was also proposed recently (McNamara & McCabe, 2012). It is our view that overtraining and over commitment in elite athletes does not parallel the psychiatric cases of exercise addiction. In our opinion this model is questionable for at least two reasons: 1) Timing and availability; If behavioral addictions are means of escape from unbearable stress (Korolenko, 1991), the escape needs to happen when the pain dictates or the urge arises. Elite athletes have a training regimen that is scheduled for them, in group settings, and at directed intensity. These are not characteristics of exercise or any other behavioral or chemical addiction, because the compulsive urges that dominate the person's behavior – after she/he has lost control over the addictive behavior(s) – trigger craving for instant fulfillment. 2) The model has a biologically determined onset, like body mass index (BMI), given as example by the authors (McNamara & McCabe, 2012). If we consider deeply that most addictions are forms of escape from painful reality (Korolenko, 1991), then while biological factors affect psychology, the route of addiction(s) may be – most likely – of psychological origin. The “Biopsychosocial” model (Figure 4) states that exercise addiction has a biological factor (e.g. BMI) at its route of origin in the elite athletes. Social and psychological processes may interact to determine whether exercise addiction will occur or not. Freimuth et al. (2011) warned that intensive training, for long hours, and ambitious strivings to become the best of the best that characterizes successful elite athletes, should not be confused with symptoms of addiction in spite of the fact that there is overlap in the latter. This point of Freimuth et al. is fully endorsed for the two principal reasons discussed above.
Figure 4.
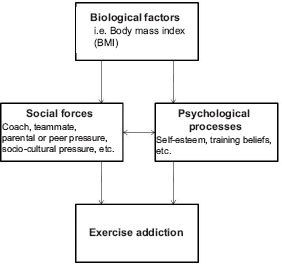
The “Biopsychosocial” model for exercise addiction in elite athletes
Based on: McNamara & McCabe (2012).
A theoretical model accentuating the possible role of interleukin six (IL-6) in exercise addiction has been proposed by Hamer and Karageorghis (2007). According to the model, an unidentified trigger causes IL-6 levels to rise and generate cytokine-induced sickness behavior that is linked to negative affect. In individuals affected by psychological hardship an elevated level of IL-6 could yield even more negative mental state. However, the IL-6 hypothesis may not account for the possibility that some individuals will resort to exercise while others may reach for chemical means of escape. The low prevalence of exercise addiction is ascribed to possible adaptations to exercise, whereas the lack of it may increase vulnerability to exercise addiction (Figure 5).
Figure 5.

The IL-6 Model for exercise addiction
Based on: Hamer & Karageorghis (2007).
Note: The dotted line reflects that inability to cope with exercise load my further increase IL-6 levels.
The review of the extant models that were specifically forwarded for the explanation of exercise addiction clearly reveals that there is inconsistency in the research perspectives from which this behavioral addiction is examined. Simply and perhaps crudely summarized, according to the Sympathetic Arousal Hypothesis most habitual exercisers may be affected by exercise addiction, a fact that is unlikely with a mean estimate of 3% (Sussman et al., 2011a); the Cognitive Appraisal Hypothesis accounts for exercise addiction only after the behavior has been adopted for coping with adversity, and cannot explain who/why chooses exercise as a means of coping; the “Four Phase” model is a hierarchical/developmental model, but again it does not address when and who would rely on the mood-moderating effects of exercise for coping and with specific (?) adversities or stress. The way the model may be interpreted is that all exercisers who discover the mood improving and other positive psychological results of exercise may become addicted while coping with stress; The “Biopsychosocial” model that was developed for elite athletes has unconvincing theoretical background in context of the freedom of choice to satisfy craving and urges inherent in addictions. Finally the IL-6 model may be an intermediary in the etiology of exercise addiction, but it cannot account neither for the trigger in raising IL-6 levels nor in exercise-related consequences, since according to the model some exercisers may be affected while others (with adaptation) may not. Therefore, a model accounting for the adaption, maintenance, and transformation of the behavior – and therefore addressing the exercise paradox – is needed for a consistent conceptualization and research framework in the understanding of exercise addiction as a clinical morbidity.
AN EXPANDED INTERACTIONAL MODEL FOR EXERCISE ADDICTION
A missing aspect of the existing models for exercise addiction is the determinant(s) of the choice of exercise as a means of escape from hardship. Here it is strongly stressed, that an interaction between personal values, social image, past exercise experience, and life situation jointly determine whether one will use exercise for coping or resort to other means of dealing with stress. The possible number of interactions between personal and situational factors is so large the each case is idiographic in a mindset resembling a secret “black-box”. The box could only be opened after diagnosis with the help of mental health professionals. Indeed, exercise addiction, unlike other chemical and/or behavioral addictions, has a unique characteristic not present in other addictions, which is the physical challenge or work. It was proposed, based on preliminary laboratory evidence, that exercise acts as cathartic-buffer for stress (Tsang & Szabo, 2003). Habitual exercisers when experiencing stress – knowing the mood improving effects of exercise from past experience (Freimuth et al., 2011) – may resort to exercise to cope with the challenge. However, not all exercisers will try to reduce the pain of a novel emotional hardship with exercise, but instead may resort to passive forms of escape behaviors or addiction(s). Therefore, a model taking into account the personal aspects interacting with social-environmental factors may be necessary for the better understanding of the genesis of exercise addiction in the affected individuals. Indeed, a positive relationship was established between exercise addiction risk-scores and trait anxiety (Coen & Ogles, 1993), perfectionism (Cook, 1996), and obsessive compulsiveness (Spano, 2001). Further, it was reported that neuroticism, extraversion, and agreeableness could predict symptoms of exercise addiction (Hausenblas & Giacobbi, 2004). Finally, gender (Cook, Hausenblas & Rossi, 2013) and sex role orientation (Rejeski, Best, Griffith & Kenney, 1987) may also have mediating roles. The large combination of subjective psychological factors interacting with situational variables may renders difficult if not impossible the scrutiny of exercise addiction from a nomothetic perspective.
The model presented in Figure 6 is an interactional model for exercise addiction. It is in line with the proposed PACE (Pragmatics, Attraction, Communication, Expectation) model for addictions in general (Sussman et al., 2011b). In the current model (Figure 6) a complex set of personal factors interact with a number of environmental – and/or situational – factors to determine the primary motive for exercise behavior. These motives diverge in two directions (Robbins & Joseph, 1985). A health (mental or physical) motivated individual, for example, may run for better or improved health (gain health) and/or to prevent ill health consequences like gaining weight, being lethargic, etc. Both incentives are therapeutic in nature. However, health motives could also have a mastery-orientation, like becoming stronger and lifting more weight (performance orientations), or concentrating better and being more productive at work. If better concentration would be the aim, a therapeutic-orientation would be established, but if the expected consequence of the better concentration (productivity) is the objective, then the mastery orientation is the driving force.
Figure 6.

An interactional model for the better understanding of the exercise paradox
The most important component of the here proposed model is the consideration of a suddenly emerging reaction, determined by a set of idiographic (i.e., personal and situational) interactions in the black-box to an ongoing and no longer bearable – or suddenly appearing – life stressor that causes psychological pain over which the individual has no control. This component accounts for the surmise that exercise addiction is not evolutionary, or slowly progressing, but rather revolutionary, or suddenly surfacing (Szabo, 2010). At the moment when the situation gets out of control, a person will “gravitate” towards a means of available coping in accord with the “Pragmatics” phase of the PACE model (Sussman et al., 2011b – see Figure 7). The choice is determined by conscious and subconscious interactions (in the black-box) between individual aspects, situational factors, and antecedents of exercise behavior, in accord with the “Attraction” component of the PACE model, in a similar way as the motivation for exercise is initially determined. Accordingly, even mastery-oriented exercisers may now shift focus to the therapeutic aspects of exercise and get more involved in it to get rid of the painful stress. This attentional cognition is also in line with the “Communication” factor in the PACE model in that experience, inter- and intrapersonal thought, beliefs and convictions will influence the escape path or the choice of the individual. For example, the lack of experience with alcohol, tobacco, or leisure drugs in conjunction with long exercise history and positive beliefs about exercise (media, social, health values) all interact with unique personal factors during the effort of coping. An already “therapeutic” exerciser in the model is more likely to chose exercise for coping. Then, also in agreement with the PACE model, the greater the expectation from exercise, the more unlikely that the exerciser will turn to other forms of addictions. Being a “positive addiction” it is much easier to hide behind exercise whilst maintaining one's reputation in the social environment, in contrast to other forms of addictions bearing a social stigma.
Figure 7.
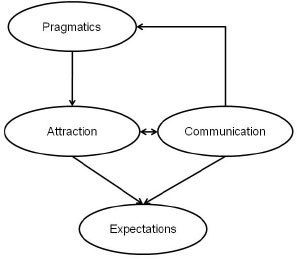
The PACE Model for addictions
Based on: Sussman et al. (2011b).
The PACE model was proposed for behavioral addictions in general (Sussman et al., 2011b). While the current model is in harmony with the PACE model, it is specific to exercise and highlights how orientation, experience and personal-situational interactions could all play mediating roles in the manifestation of exercise addiction. Past research long ago has revealed that addiction risk is higher in those who exercise for escaping the stress or changing their emotions, or physical appearance to improve self-esteem as compared to those who exercise for mastery reasons (Thornton & Scott, 1995). Indeed, Baker, Piper, McCarthy, Majeskie and Fiore (2004) proposed a model for drug addiction in which addictive behavior is sustained through negative reinforcement in an effort to avoid negative affect. Szabo (2010) also argued that exercise addiction is motivated by negative reinforcement. However, initial therapeutic orientation, like losing weight and/or gaining muscles, may – following fulfillment of the goal – turn into mastery orientation and be maintained within the spectrum of healthy exercise pattern. Then, as the bi-directional arrow (refer to Figure 6) indicates between the therapeutic-orientation and major life-stress (black), it is possible that through therapeutic exercising – without addiction – one could master the situation and re-establish a healthy pattern of exercise whilst coping with adversity in a healthy way.
A broken arrow (Figure 6) from mastery orientation to exercise addiction accounts for the unlikely and possibly rare occurrences when an athlete would jeopardize her/his health to stretch the personal limits. It must be stressed that the key reason beyond overtraining – which eventually will be unsuccessful due to strain, injury and staleness – could be traced to mental or psychological origins: 1) the athlete is unable to accept and to realize rationally a personal limit; 2) the athlete strives to beat own or past (other's) record at any cost or otherwise all the athletic career was meaningless, 3) pressure from a past failure, or an unpleasant experience, generates a psychological need to “prove” oneself at whatever cost. While these motivations could fuel exaggerated exercise behaviors, the route and path leading to the manifestations of the behavior is different from that of exercise addiction. In fact, the broken arrow may reflect instances of exaggerated training whilst chasing of dream (or illusion) that an athlete cannot give up. As such, it may be more closely defined as obsessive-compulsive behavior rather than addiction. It should be noted that addiction involves compulsion and dependence (Berczik et al., 2012) and the later may be absent in mastery situations, and therefore marked with a broken arrow.
CONCLUSION
Approaching half-century of research, exercise addiction is still not well understood. The spectrum of the reported preponderance ranging from 0.3% to 77% shows that there are theoretical and methodological barriers to research in this area. Indeed, nomothetic research could yield results about proneness or risk while actual clinical cases can only be examined through idiographic research. The existing models for exercise addiction are incomplete. A new more comprehensive interactional model, complementing the extant models, is offered with a view to the more homogeneous conceptualization of exercise addiction. Nevertheless, this dual interactional model has a subjective or idiosyncratic component, that interacts with objective situational elements, for which the nomothetic perspective and scholastic research may not account for. Therefore, the message of this paper is that researchers should clearly distinguish between risk for exercise addiction that may or may not end up in morbidity and actual clinical or psychiatric cases of exercise addiction. The scope of the model presented in here is to draw a line between risk and morbidity. The exercise addiction literature, apart from a few case studies, deals with estimates of risk that may never turn into actual morbidity.
Funding Statement
Funding sources: No financial support was received for this study.
References
- Ackard D. M, Brehm B. J, Steffen J. J. Exercise and eating disorders in college-aged women: Profiling excessive exercisers. Eating Disorders. 2002;10(1):31–47. doi: 10.1080/106402602753573540. [DOI] [PubMed] [Google Scholar]
- Allegre B, Therme P, Griffiths M. Individual factors and the context of physical activity in exercise dependence: A prospective study of “ultra-marathoners”. International Journal of Mental Health and Addiction. 2007;5(3):233–243. [Google Scholar]
- Diagnostic and statistical manual of mental health disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Publishing; American Psychiatric Association (2013). [Google Scholar]
- Baekeland F. Exercise deprivation: Sleep and psychological reactions. Archives of General Psychiatry. 1970;22(4):365–369. doi: 10.1001/archpsyc.1970.01740280077014. [DOI] [PubMed] [Google Scholar]
- Baker T. B, Piper M. E, McCarthy D. E, Majeskie M. R, Fiore M. C. Addiction motivation reformulated: An affective processing model of negative reinforcement. doi:10.1037/0033-295X.111. 1.33. Psychological Review. 2004;111(1):33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bamber D, Cockerill I. M, Carroll D. The pathological status of exercise dependence. British Journal of Sports Medicine. 2000;34(2):125–132. doi: 10.1136/bjsm.34.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berczik K, Szabo A, Griffiths M. D, Kurimay T, Kun B, Urbán R, Demetrovics Z. Exercise addiction: Symptoms, diagnosis, epidemiology, and etiology. Substance Use & Misuse. 2012;47(4):403–417. doi: 10.3109/10826084.2011.639120. [DOI] [PubMed] [Google Scholar]
- Blaydon M. J., Lindner K. J. Eating disorders and exercise dependence in triathletes. Eating Disorders. 2002;10:49–60. doi: 10.1080/106402602753573559. [DOI] [PubMed] [Google Scholar]
- Blumenthal J. A, O'Toole L. C, Chang J. L. Is running an analogue of anorexia nervosa? An empirical study of obligatory running and anorexia nervosa. Obstetrical & Gynecological Survey. 1985;40(2):94–95. [Google Scholar]
- Carmack M. A, Martens R. Measuring commitment to running: A survey of runner's attitudes and mental states. Journal of Sport Psychology. 1979;1:21–42. [Google Scholar]
- Carnes P. The sexual addiction. Minneapolis, MN: CompCare Publications; 1983. [Google Scholar]
- Chapman C. L, De Castro J. M. Running addiction: Measurement and associated psychological characteristics. The Journal of Sports Medicine and Physical Fitness. 1990;30:283–290. [PubMed] [Google Scholar]
- Coen S. P, Ogles B. M. Psychological characteristics of the obligatory runner: A critical examination of the anorexia analogue hypothesis. Journal of Sport & Exercise Psychology. 1993;15:338–354. [Google Scholar]
- Cook B, Hausenblas H. A, Rossi J. The moderating effect of gender on ideal-weight goals and exercise dependence symptoms. Journal of Behavioral Addictions. 2013;21:50–55. doi: 10.1556/JBA.1.2012.010. [DOI] [PubMed] [Google Scholar]
- Cook C. A. Unpublished master's thesis, University of Alberta, Alberta, Canada. (cf. Hausenblas & Giacobbi, 2004). The psychological correlates of exercise dependence in aerobics instructors. 1996 [Google Scholar]
- Costa S, Cuzzocrea F, Hausenblas H. A, Larcan R, Oliva P. Psychometric examination and factorial validity of the Exercise Dependence Scale-Revised in Italian exercisers. Journal of Behavioral Addictions. 2012;1(4):186–190. doi: 10.1556/JBA.1.2012.009. [DOI] [PubMed] [Google Scholar]
- Crisp A. H, Hsu L. K. G, Harding B, Hartshorn J. Clinical features of anorexia nervosa: A study of a consecutive series of 102 female patients. Journal of Psychosomatic Research. 1980;24:179–191. doi: 10.1016/0022-3999(80)90040-9. [DOI] [PubMed] [Google Scholar]
- De Coverley Veale D. M. W. Exercise dependence. British Journal of Addiction. 1987;82:735–740. doi: 10.1111/j.1360-0443.1987.tb01539.x. [DOI] [PubMed] [Google Scholar]
- Downs D. S, Hausenblas H. A, Nigg C. R. Factorial validity and psychometric examination of the exercise dependence scale-revised. Measurement in Physical Education and Exercise Science. 2004;8:183–201. [Google Scholar]
- Egorov A Y. Hexumuyeckue 3avucumocmu [Non-chemical addictions]. Sankt Petersburg, Izdatelstvo “Rech”. (in Russian) [Google Scholar]
- Egorov A. Y. New classification and psychopathology of nonchemical addictions. (Suppl. 1), 14. Abs. Journal of Behavioral Addictions. 2013;2 [Google Scholar]
- Freimuth M, Moniz S, Kim S. R. Clarifying exercise addiction: Differential diagnosis, co-occurring disorders, and phases of addiction. International Journal of Environmental Research and Public Health. 2011;8(10):4069–4081. doi: 10.3390/ijerph8104069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser W. Positive addiction. New York: Harper and Row; 1976. [Google Scholar]
- Glasser W. Promoting client strength through positive addiction. Canadian Journal of Counselling and Psychotherapy/Revue Canadienne de Counseling et de Psychothérapie. 2012;11(4):173–175. [Google Scholar]
- Grandi S, Clementi C, Guidi J, Benassi M, Tossani E. Personality characteristics and psychological distress associated with primary exercise dependence: An exploratory study. Psychiatry Research. 2011;189(2):270–275. doi: 10.1016/j.psychres.2011.02.025. [DOI] [PubMed] [Google Scholar]
- Griffiths M. D. Exercise addiction: A case study. Addiction Research & Theory. 1997;5(2):161–168. [Google Scholar]
- Griffiths M. D, Szabo A, Terry A. The exercise addiction inventory: A quick and easy screening tool for health practitioners. British Journal of Sports Medicine. 2005;39(6):e30. doi: 10.1136/bjsm.2004.017020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailey B. J, Bailey L. A. Negative addiction in runners: A quantitative approach. Journal of Sport Behavior. 1982;5:150–153. [Google Scholar]
- Hamer M, Karageorghis C. I. Psychobiological mechanisms of exercise dependence. Sports Medicine. 2007;37(6):477–484. doi: 10.2165/00007256-200737060-00002. [DOI] [PubMed] [Google Scholar]
- Hausenblas H. A, Downs S. D. How much is too much? The development and validation of the exercise dependence scale. Psychology and Health. 2002;17:387–404. [Google Scholar]
- Hausenblas H. A, Giacobbi P. R Jr. Relationship between exercise dependence symptoms and personality. Personality and Individual Differences. 2004;36(6):1265–1273. [Google Scholar]
- Holden C. ‘Behavioral addictions’: Do they exist? Science. 2001;294(5544):980–982. doi: 10.1126/science.294.5544.980. [DOI] [PubMed] [Google Scholar]
- Hurst R, Hale B, Smith D, Collins D. Exercise dependence, social physique anxiety, and social support in experienced and inexperienced bodybuilders and weightlifters. British Journal of Sports Medicine. 2000;34(6):431–435. doi: 10.1136/bjsm.34.6.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korolenko Ts P. Addiktivnoe povedenie& Ob]aq xarakteristika i zakonomernosti razvitiq [Addictive behavior. General characteristics and patterns of development.] (in Russian) Review of Psychiatry and Medical Psychology. 1991;1:8–15. [Google Scholar]
- Krueger D. W. On compulsive shopping and spending: A psychodynamic inquiry. American Journal of Psychotherapy. 1988;42(4):574–584. doi: 10.1176/appi.psychotherapy.1988.42.4.574. [DOI] [PubMed] [Google Scholar]
- Kubey R, Csikszentmihalyi M. Television addiction. Scientific American. 2002;286(2):74–81. doi: 10.1038/scientificamerican0202-74. [DOI] [PubMed] [Google Scholar]
- Lejoyeux M, Avril M, Richoux C, Embouazza H, Nivoli F. Prevalence of exercise dependence and other behavioral addictions among clients of a Parisian fitness room. Comprehensive Psychiatry. 2008;49(4):353–359. doi: 10.1016/j.comppsych.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Lejoyeux M, Guillot C, Chalvin F, Petit A, Lequen V. Exercise dependence among customers from a Parisian sport shop. Journal of Behavioral Addictions. 2012;1(1):28–34. doi: 10.1556/JBA.1.2012.1.3. [DOI] [PubMed] [Google Scholar]
- Lichtenstein M. B, Christiansen E, Bilenberg N, Støving R. K. Validation of the exercise addiction inventory in a Danish sport context. (in press – Early online, retrieved 08 May, 2013 from: doi:10.1111/j.1600-0838. 2012. 01515. x) Scandinavian Journal of Medicine & Science in Sports. 2013 doi: 10.1111/j.1600-0838.2012.01515.x. [DOI] [PubMed] [Google Scholar]
- Martin P. R, Petry N. M. Are non-substance-related addictions really addictions? The American Journal on Addictions. 2005;14(1):1–7. doi: 10.1080/10550490590899808. [DOI] [PubMed] [Google Scholar]
- McNamara J, McCabe M. P. Striving for success or addiction? Exercise dependence among elite Australian athletes. Journal of Sports Sciences. 2012;30(8):755–766. doi: 10.1080/02640414.2012.667879. [DOI] [PubMed] [Google Scholar]
- McNamara J, McCabe M. P. Development and validation of the Exercise Dependence and Elite Athletes Scale. (in press – Early online, retrieved 21 May, 2013. http://dx.doi.org/10.1016/j.peh. 2012.11.001) Performance Enhancement & Health. 2013 [Google Scholar]
- Menczel Z, Kovacs E, Farkas J, Magi A, Eisinger A, Kun B, Demetrovics Zs. Prevalence of exercise dependence and eating disorders among clients of fitness centres in Budapest. (Suppl. 1) Journal of Behavioral Addictions. 2013;2:23–24 Abs. [Google Scholar]
- Modolo V. B, Antunes H. K, Gimenez P. R, Santiago M. L, Tufik S, Mello M. T. D. Negative addiction to exercise: Are there differences between genders. Clinics (Sao Paulo) 2011;66(2):255–260. doi: 10.1590/S1807-59322011000200013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mónok K, Berczik K, Urbán R, Szabó A, Griffiths M. D, Farkas J, Magi A, Eisinger A, Kurimay T, Kökönyei G, Kun B, Paksi B, Demetrovics Z. Psychometric properties and concurrent validity of two exercise addiction measures: A population wide study in Hungary. Psychology of Sport and Exercise. 2012;13:739–746. [Google Scholar]
- Morgan W. P. Negative addiction in runners. The Physician and Sports Medicine. 1979;7:57–77. doi: 10.1080/00913847.1979.11948436. [DOI] [PubMed] [Google Scholar]
- Murphy M. H. Psychology in Sport. London: Taylor and Francis; 1994. Sport and drugs and runner's high (Psychophysiology). [Google Scholar]
- Ogden J, Veale D, Summers Z. The development and validation of the Exercise Dependence Questionnaire. Addiction Research & Theory. 1997;5(4):343–355. [Google Scholar]
- Parke J, Griffiths M. D. Gambling addiction and the evolution of the “near miss”. Addiction Research & Theory. 2004;12(5):407–411. [Google Scholar]
- Pasman L, Thompson J. K. Body image and eating disturbance in obligatory runners, obligatory weightlifters, and sedentary individuals. International Journal of Eating Disorders. 1988;7:759–777. [Google Scholar]
- Rejeski W. J, Best D. L, Griffith P, Kenney E. Sex-role orientation and the responses of men to exercise stress. Research Quarterly for Exercise and Sport. 1987;58(3):260–264. [Google Scholar]
- Robbins J. M, Joseph P. Experiencing exercise withdrawal: Possible consequences of therapeutic and mastery running. Journal of Sport Psychology. 1985;7:23–39. [Google Scholar]
- Sachs M. L, Pargman D. Running as therapy: An integrated approach. Lincoln, NE: University of Nebraska Press; 1984. Running addiction. In M. L. Sachs & G. W. Buffone (Eds.) pp. 231–252. [Google Scholar]
- Scottl K. S, Moore K. S, Miceli M. P. An exploration of the meaning and consequences of workaholism. Human Relations. 1997;50(3):287–314. [Google Scholar]
- Slay H. A, Hayaki J, Napolitano M. A, Brownell K. D. Motivations for running and eating attitudes in obligatory versus nonobligatory runners. International Journal of Eating Disorders. 1998;23(3):267–275. doi: 10.1002/(sici)1098-108x(199804)23:3<267::aid-eat4>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Smith D, Wright C, Winrow D. Exercise dependence and social physique anxiety in competitive and non-competitive runners. International Journal of Sport and Exercise Psychology. 2010;8(1):61–69. [Google Scholar]
- Spano L. The relationship between exercise and anxiety, obsessive-compulsiveness, and narcissism. Personality and Individual Differences. 2001;30(1):87–93. [Google Scholar]
- Sussman S, Lisha N, Griffiths M. D. Prevalence of the addictions: A problem of the majority or the minority? Evaluation & the Health Professions. 2011a;34(1):3–56. doi: 10.1177/0163278710380124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Leventhal A, Bluthenthal R. N, Freimuth M, Forster M, Ames S. L. A framework for the specificity of addictions. International Journal of Environmental Research and Public Health. 2011b;8:3399–3415. doi: 10.3390/ijerph8083399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo A. The impact of exercise deprivation on well-being of habitual exercisers. The Australian Journal of Science and Medicine in Sport. 1995;27:68–75. [PubMed] [Google Scholar]
- Szabo A. (Chapter 7. Physical activity and psychological well-being. London: Routledge; 2000. Physical activity as a source of psychological dysfunction. In S. J. H. Biddle, K. R. Fox & S. H. Boutcher (Eds.). pp. 130–195. [Google Scholar]
- Szabo A. Exercise addiction: A symptom or a disorder? New York: Nova Science Publishers Inc; 2010. [Google Scholar]
- Szabo A, Griffiths M. D. Exercise addiction in British sport science students. International Journal of Mental Health and Addiction. 2007;5(1):25–28. [Google Scholar]
- Targhetta R, Nalpas B, Perney P. Argentine tango: Another behavioral addiction? Journal of Behavioral Addictions. 2013;2(3):179–186. doi: 10.1556/JBA.2.2013.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry A, Szabo A, Griffiths M. D. The exercise addiction inventory: A new brief screening tool. Addiction Research and Theory. 2004;12:489–499. [Google Scholar]
- Thompson J. K, Blanton P. Energy conservation and exercise dependence: A sympathetic arousal hypothesis. Medicine and Science in Sports and Exercise. 1987;19:91–97. [PubMed] [Google Scholar]
- Thornton E. W, Scott S. E. Motivation in the committed runner: Correlations between self-report scales and behavior. Health Promotion International. 1995;10(3):177–184. [Google Scholar]
- Tsang T. C. E, Szabo A. Motivation for increased self-selected exercise intensity following psychological distress: Laboratory based evidence for catharsis. Journal of Psychosomatic Research. 2003;55(2):133. [Google Scholar]
- Veale D. Exercise addiction: Motivation for participation in sport and exercise. Leicester: The British Psychological Society; 1995. Does primary exercise dependence really exist? In J. Annett, B. Cripps & H. Steinberg (Eds.) pp. 1–5. [Google Scholar]
- Villella C, Martinotti G, Di Nicola M, Cassano M, La Torre G, Gliubizzi M. D, Messeri I, Petruccelli F, Bria P, Janiri L, Conte G. Behavioral addictions in adolescents and young adults: Results from a prevalence study. Journal of Gambling Studies. 2011;27(2):203–214. doi: 10.1007/s10899-010-9206-0. [DOI] [PubMed] [Google Scholar]
- Yen J. Y, Yen C. F, Chen C. C, Chen S. H, Ko C. H. Family factors of internet addiction and substance use experience in Taiwanese adolescents. CyberPsychology & Behavior. 2007;10(3):323–329. doi: 10.1089/cpb.2006.9948. [DOI] [PubMed] [Google Scholar]
- Young K. S. Internet addiction: The emergence of a new clinical disorder. CyberPsychology & Behavior. 3. 1998;1:237–244. [Google Scholar]
- Youngman J. D. http://scholarlyrepository.miami.edu/cgi/viewcontent.cgi?article =1011&context=oa_dissertations Risk for exercise addiction: A comparison of triathletes training for sprint-, olympic-, half-ironman-, and ironman-distance triathlons. Open Access Dissertations. Paper 12. Retrieved May 17, 2013. 2007 [Google Scholar]


