Abstract
Background
Self-medication with alcohol is frequently hypothesized to explain anxiety and alcohol dependence comorbidity. Yet, there is relatively little assessment of drinking to self-medicate anxiety and its association with the occurrence or persistence of alcohol dependence in population-based longitudinal samples, or associations within demographic and clinical subgroups.
Methods
Hypothesizing that self-medication of anxiety with alcohol is associated with the subsequent occurrence and persistence of alcohol dependence, we assessed these associations using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), and examined these associations within population subgroups. This nationally representative survey of the US population included 43,093 adults surveyed in 2001-2, and 34,653 re-interviewed in 2004-5. Logistic regression incorporating propensity score methods was used.
Results
Reports of drinking to self-medicate anxiety was associated with the subsequent occurrence (adjusted odds ratio (AOR)=5.71, 95% confidence interval (CI)=3.56-9.18, p<0.001) and persistence (AOR=6.25, CI=3.24-12.05, p<0.001) of alcohol dependence. The estimated proportion of the dependence cases attributable to self-medication drinking were 12.7% and 33.4% for incident and persistent dependence, respectively. Stratified analyses by age, sex, race-ethnicity, anxiety disorders and sub-threshold anxiety symptoms, quantity of alcohol consumption, history of treatment and family history of alcoholism showed few subgroup differences.
Conclusions
Individuals who report drinking to self-medicate anxiety are more likely to develop alcohol dependence, and the dependence is more likely to persist. There is little evidence for interaction by the population subgroups assessed. Self-medication drinking may be a useful target for prevention and intervention efforts aimed at reducing the occurrence of alcohol dependence.
Keywords: addiction, alcoholism, alcohol use disorder, anxiety disorder, epidemiology, generalized anxiety disorder, panic disorder, phobia
Introduction
Anxiety disorders are commonly found to co-occur with alcohol use disorders (AUD).1-12 The temporal relationship between the conditions may differ by anxiety subtype. Phobias tend to be temporally primary, whereas panic tends to be secondary to AUD.13-15 Some of the comorbidity has been thought to be related to substance-induced anxiety,8 emphasizing the need to distinguish comorbidity with independent anxiety disorders.1
Etiologic theories to explain the co-morbidity are frequently based on causal pathway models, in which anxiety results in AUD,16 or drinking problems cause anxiety.17;18 There may also exist a bidirectional relationship,15;19-21 or a common etiology such as a genetic vulnerability.22 A frequent explanation for the comorbidity with a primary anxiety disorder is that alcohol is used to self-medicate or alleviate anxiety symptoms.23 This hypothesis is supported by known neurochemical mechanisms of alcohol that affect the gamma-aminobutyric acid receptors in a manner that resembles the benzodiazepine class of medications. In addition, tension-reduction motives are positively associated with heavy drinking.24 Some investigators find little evidence that drinking reduces anxiety.25;26 For example, Himle and colleagues did not find an effect of alcohol dosing as compared with alcohol placebo on level of social phobic anxiety.26 Yet, Abrams and colleagues27 found a direct pharmacologic effect of alcohol on reducing social anxiety.
There has been a paucity of research assessing self-medication of anxiety with the occurrence of alcohol dependence, particularly using longitudinal population-based studies that minimize potential selection biases. Although recent evidence indicates that reports of drinking to self-medicate anxiety may increase the onset or persistence of AUD,28;29 there have been recent suggestions to examine abuse and dependence disorders separately.30 Because alcohol abuse has typically a weaker association with anxiety disorders,1;4 and may be influenced by social and cultural factors,30;31 we chose to examine the association of self-medication drinking with alcohol dependence alone. In addition, virtually no studies have assessed this association across subgroups of the population or utilized a statistical approach designed to estimate causal associations with observational data. In prior analyses of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) findings assessing self-medication of anxiety symptoms indicate cross-sectional relationships with psychopathology,32;33 and a recent longitudinal assessment provided evidence that self-medication is associated with incident and persistent alcohol and drug use disorders.28 The current analysis extends these findings by assessing the association of reports of drinking to self-medicate anxiety with the subsequent occurrence as well as persistence of alcohol dependence using propensity score methods34 that reduce potential selection bias and adjust for potential confounders. In addition, we explored these associations by specific population subgroups across age, sex and race-ethnicity strata. We further hypothesized that a history of treatment for anxiety differentially affects the association between drinking self-medication and alcohol dependence; specifically, that individuals in treatment are less likely to self-medicate anxiety as self-medication may suggest a failure to access treatment or the presence of refractory symptoms. We also explored the associations by family history of alcoholism to consider a potential for genetic vulnerability, as well as by consumption level to evaluate whether the association only occurred for heavier drinkers. Lastly, we assessed diagnostic categories to examine the self-medication association by specific anxiety disorders, and among individuals with sub-threshold symptoms.
Materials and Methods
Sample
The data for the analyses in this report come from the NESARC waves 1 and 2. The study design and sample characteristics have been previously described.1;35 In brief, the NESARC is a nationally representative survey of the United States population, which included residents of Hawaii and Alaska. The survey was conducted by the National Institute on Alcohol Abuse and Alcoholism, and face-to-face interviews were completed. The protocol included the oversampling of Blacks, Hispanics and young adults, ages 18 to 24 years, to obtain greater accuracy of estimates among racial and ethnic minority populations as well as among younger adults. The survey sample was weighted to provide nationally representative estimates and to adjust for the unequal probabilities of selection.
The first wave of the NESARC was completed between 2001 and 2002 and included a total of 43,093 adults, aged 18 years and older. Of these, 39,959 were eligible for wave 2 interviews. Ineligible respondents were those that were not interviewed because they were either deceased, deported, mentally or physically impaired or on active military duty at the time of the follow-up interview. A total of 34,653 of the eligible participants from wave 1 were successfully tracked and re-interviewed in the wave 2 survey between 2004 and 2005. The response rates for wave 1 and eligible wave 2 participants were 81% and 87%, respectively.
Separate analyses were completed to assess reports of drinking to self-medicate anxiety at baseline with three alcohol dependence outcomes: 1) the occurrence of alcohol dependence at follow-up, 2) the persistence of alcohol dependence, and 3) the incidence of alcohol dependence at follow-up. The study sample to assess the occurrence of alcohol dependence at follow-up was restricted to 1,567 NESARC participants with anxiety symptoms at baseline who reported alcohol use in their lifetime, were asked about drinking to self-medicate their anxiety symptoms at the baseline interview, and had been successfully re-interviewed at the wave 2 follow-up. In order to assess persistence of alcohol dependence, the study sample was further restrained to include only the 442 NESARC participants with a current or lifetime history of alcohol dependence at baseline. To assess incidence cases, we removed 208 baseline dependence cases leaving us with a analytic sample of 1,359.
Measures
Covariates that were assessed in the analyses were identified from the data gathered at the wave 1 interview. Substance use and psychiatric disorders were ascertained based on DSM-IV criteria using the NIAAA's Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version (AUDADIS-IV)36;37 -- a structured diagnostic interview designed for use by lay interviewers to derive diagnoses of lifetime and 12-month (current) substance use and psychiatric disorders. Individuals with anxiety disorders were those participants who met DSM-IV criteria within the 12-months prior to the baseline interview and included those with generalized anxiety disorder, panic disorder, social phobia and specific phobia. We also distinguished between individuals that met full diagnostic criteria for an anxiety disorder, and those with some but not all criteria, including the clinical significance criteria for any anxiety disorder (participants with sub-threshold anxiety symptoms). Because post traumatic stress disorder was not evaluated at the baseline NESARC survey, it was not included in these longitudinal assessments.
Other disorders adjusted for in the analyses included current or lifetime major depressive disorder, alcohol abuse and dependence, non-alcohol drug abuse and dependence (heroin, other narcotics, cocaine, stimulants, hallucinogens, and/or marijuana), nicotine dependence, and personality disorders measured at wave 1 or 2 (antisocial, narcissistic, histrionic, borderline, schizoid, schizotypal, paranoid, obsessive-compulsive, dependent, and/or avoidant).
Alcohol self-medication was assessed by asking if participants who had reported at least three anxiety symptoms in the six months prior to the baseline interview had ever drunk alcohol to calm down or help quiet their nerves when they felt tense, nervous, or worried. A follow-up question asked if this had occurred in the past year. The self-medication question was asked separately for each anxiety disorder after inquiring about the symptoms of that disorder. Information on treatment history for anxiety symptoms was identified by positive responses from survey queries concerning having ever sought treatment for anxiety symptoms from a counselor, therapist, doctor or other professional; if they had been hospitalized overnight or went to an emergency room, and/or if a doctor had ever prescribed medication for anxiety symptoms.
Additional characteristics included in the analyses were the following: sex, age (18-35, 36-49, and ≥50 years; 18-39 and ≥40 for the stratified analyses), race/ethnicity (non-Hispanic white, black, Hispanic, and other; and non-Hispanic white, and other for the stratified analyses), educational level (<12 years, and ≥12 years), past year consumption pattern (daily or nearly daily drinking vs. less than daily), and past year consumption level on drinking days (≥5 drinks/drinking day vs. <5 drinks/drinking day). Family history of alcoholism was assessed by report of first-degree relatives that were an “alcoholic or problem drinker”. Individual questions gathered information on specific first degree relatives (biological mother, father, sisters, brothers, and children).
Analyses
After exploratory data analyses to examine the frequency distributions of baseline characteristics associated with the occurrence and persistence of alcohol dependence, and with self-medication drinking, we completed initial and multiple logistic regression models. The logistic regression analyses were used to assess the strength of the associations between reports of drinking to self-medicate anxiety symptoms at baseline with the subsequent occurrence of alcohol dependence at follow-up. In these analyses, we held constant a history of lifetime alcohol dependence with or without abuse at baseline to account for prior history of dependence in all multivariable analyses (N=1567). We also completed analyses in which we focused on incident alcohol dependence, defined as the new onset of alcohol dependence at wave 2, excluding the 208 individuals with current or lifetime alcohol dependence at baseline (n=1359). In these latter analyses, we did not adjust for baseline dependence. Findings were similar to the results presented in this report. However, by excluding baseline dependence cases, power was reduced and inadequate to complete the stratified analyses within population subgroups. For the analyses to assess persistence of alcohol dependence, individuals with a history of 12-month or lifetime alcohol dependence with or without alcohol abuse at the baseline interview who also subsequently met criteria for alcohol dependence at follow-up were classified as having persistent alcohol dependence.
Potential confounding was constrained in these analyses via statistical adjustment in logistic regression models. In these models, we used propensity score methods,34 which have been widely applied in observational studies to estimate causal relationships and account for observed differences among the exposed and unexposed groups.29;38 Our exposed group comprised drinkers at baseline who reported using alcohol to self-medicate anxiety symptoms within the prior year. The non-exposed study participants were drinkers who reported no self-medication drinking.
The propensity score is defined as the conditional probability of being exposed (i.e., self-medicating) given a set of observed covariates. We used the propensity score as a method of adjustment for covariates in the logistic regression model in order to assess the association of self-medication drinking at baseline with the subsequent occurrence and persistence of alcohol dependence at follow-up. We estimated a propensity score using the observed background characteristics for each participant in the analytic sample. The background covariates were summarized into a single number, the propensity score, which represented the predicted probability of self-medicating anxiety symptoms with alcohol for each participant.
Once the propensity score was estimated, it was used in several different ways to assess the association between self-medication and alcohol dependence. Rosenbaum and Rubin34 identified three main ways to use the propensity score method. One is subclassification, which involves forming groups of individuals with similar propensity scores. A second is matching, in which a certain number of comparison individuals are selected for each exposed individual (often 1:1 matching). The third approach involves using the propensity score as a predictor variable in the regression model (with alcohol dependence as the outcome variable in our analyses), thereby holding constant covariates used in the estimation of the propensity score. The propensity score is calculated the same way but is applied differently with each method.38 In addition to including the propensity score as a predictor in the logistic regression analyses, we also applied each of the other two propensity score methods indicated above, involving subclassification, and 10:1 matching in separate analyses assessing drinking self-medication of anxiety symptoms with incident alcohol dependence. We found similar results for all methods. Because of reduced ability to achieve balance in the stratified analyses with the subclassification and matching methods, we completed our analyses by including the propensity score as a covariate in the regression analyses, with separate models for occurrence and persistence of alcohol dependence as the dependent variables.
The covariates used to estimate the propensity score included age, sex, race-ethnicity, educational level, lifetime history of alcohol dependence with or without alcohol abuse (not included in analyses to assess persistence of alcohol dependence or incident alcohol dependence), drinking pattern and consumption level, current history of an anxiety disorder (generalized anxiety, panic, social and specific phobia), major depressive disorder, non-alcohol substance use disorder, nicotine dependence, personality disorder, family history of alcoholism, and lifetime treatment for anxiety. To account for the complex survey design, Wave 2 survey weights were included as covariates in the estimated propensity score model.39 In order to test our hypotheses that the self-medication/alcohol dependence association would differ within subgroups of the population, we completed stratified analyses by sex, age, race-ethnicity, anxiety disorder diagnosis (as opposed to sub-threshold anxiety symptoms), weekly alcohol consumption level, and anxiety treatment history. All-way interaction terms for each stratified variable were included in our model to estimate the propensity scores.
The NESARC used a complex sampling design. Analyses used the svy routines of STATA 11.0 to take into account survey weights, clustering and stratification of the data. Population attributable fractions (PAF) were computed taking into account survey weights using the PUNAF program for STATA software.40
Results
Among those drinkers who reported anxiety symptoms at baseline and had been asked about self-medication with alcohol (n=1567), 188 individuals met criteria for alcohol dependence within the year prior to the wave 2 interview. Among those with a lifetime history of alcohol dependence at baseline (n=442), 136 individuals met criteria for persistent alcohol dependence at follow-up. In the initial bivariate analyses, individuals who met criteria for alcohol dependence at wave 2 as well as those with persistence of alcohol dependence were more likely to report having used alcohol to self-medicate their anxiety symptoms (Table 1). Men, younger adults, those who reported more frequent and heavier drinking, a family history of alcoholism and with a comorbid substance use disorder were more likely to have alcohol dependence at follow-up or have persistent dependence once dependence occurred. In addition, baseline major depression, panic disorder, specific phobia and personality disorder were associated with alcohol dependence at follow-up. Similar characteristics were related to the baseline report of alcohol self-medication of anxiety (Table 2).
Table 1.
Characteristics of NESARC participants with anxiety symptoms at the wave 1 (baseline) interview with the subsequent occurrence and persistence of alcohol dependence at the time of the follow-up interview (wave 2).
| Characteristics at baseline | Alcohol dependence at follow-up | Persistence of alcohol dependence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Absent | Present | Bivariate logistic regression analyses | Absent | Present | Bivariate logistic regression analyses | |||||||
|
| ||||||||||||
| N | % | N | % | OR (95% CI) | p | N | % | N | % | OR (95% CI) | p | |
|
|
|
|||||||||||
| Alcohol self-medication of anxiety: | ||||||||||||
| Absent | 1266 | 92.0 | 111 | 56.7 | 1.00 | <0.001 | 253 | 84.0 | 68 | 48.2 | 1.00 | |
| Present | 113 | 8.0 | 77 | 43.3 | 9.96 (6.47-15.32) | 53 | 16.0 | 68 | 51.8 | 6.45 (3.64-11.42) | <0.001 | |
|
|
|
|||||||||||
| Sex: | ||||||||||||
| Male | 418 | 34.8 | 102 | 54.5 | 1.00 | <0.001 | 139 | 51.7 | 79 | 58.3 | 1.00 | |
| Female | 961 | 65.2 | 86 | 45.5 | 0.40 (0.27-0.58) | 167 | 48.3 | 57 | 41.7 | 0.69 (0.42-1.14) | 0.144 | |
|
|
|
|||||||||||
| Age (years): | ||||||||||||
| 18-35 | 411 | 30.5 | 71 | 42.3 | 1.00 | 113 | 37.2 | 51 | 42.3 | 1.00 | ||
| 36-49 | 463 | 34.0 | 78 | 41.6 | 0.83 (0.53-1.30) | 0.412 | 110 | 35.0 | 58 | 44.1 | 0.99 (0.57-1.73) | 0.984 |
| 50+ | 505 | 35.5 | 39 | 16.1 | 0.30 (0.19-0.49) | <0.001 | 83 | 27.8 | 27 | 13.6 | 0.40 (0.22-0.72) | 0.003 |
|
|
|
|||||||||||
| Race/ethnicity: | ||||||||||||
| White | 1013 | 83.5 | 138 | 83.6 | 1.00 | 239 | 83.8 | 104 | 83.7 | 1.00 | ||
| Black | 180 | 7.3 | 26 | 8.8 | 1.17 (0.67-2.03) | 0.571 | 28 | 5.3 | 17 | 8.9 | 1.85 (0.81-4.24) | 0.141 |
| Hispanic/Other | 186 | 9.3 | 24 | 7.7 | 0.80 (0.431.49) | 0.480 | 39 | 10.9 | 15 | 7.4 | 0.68 (0.26-1.79) | 0.427 |
|
|
|
|||||||||||
| Education (years): | ||||||||||||
| <12 | 163 | 11.1 | 31 | 17.6 | 1.00 | 37 | 12.3 | 24 | 20.7 | 1.00 | ||
| ≥12 | 1216 | 88.9 | 157 | 82.4 | 0.59 (0.33-1.08) | 0.085 | 269 | 87.7 | 112 | 79.3 | 0.54 (0.24-1.20) | 0.128 |
|
|
|
|||||||||||
| Drinking patterna: | ||||||||||||
| <Daily | 1244 | 90.0 | 126 | 66.5 | 1.00 | 260 | 84.7 | 86 | 65.1 | 1.00 | ||
| Daily/nearly daily | 130 | 10.0 | 62 | 33.5 | 4.65 (3.09-6.97) | <0.001 | 46 | 15.3 | 50 | 34.9 | 3.01 (1.69-5.36) | <0.001 |
|
|
|
|||||||||||
| Drink levelb: | ||||||||||||
| <5 on drinking days | 1263 | 90.8 | 120 | 64.5 | 1.00 | 252 | 82.3 | 74 | 56.1 | 1.00 | ||
| ≥5 on drinking days | 113 | 9.2 | 66 | 35.5 | 7.19 (4.42-11.68) | <0.001 | 54 | 17.7 | 60 | 43.9 | 4.45 (2.50-7.92) | <0.001 |
|
|
|
|||||||||||
| Anxiety disorderc: | ||||||||||||
| GADd | 430 | 31.1 | 73 | 37.7 | 1.34 (0.90-2.00) | 0.139 | 110 | 34.5 | 57 | 39.7 | 1.21 (0.73-2.03) | 0.448 |
| Panic disorder | 102 | 7.2 | 25 | 13.6 | 1.94 (1.08-3.49) | 0.028 | 31 | 9.6 | 22 | 14.9 | 1.57 (0.77-3.22) | 0.209 |
| Social phobia | 175 | 13.3 | 40 | 17.7 | 1.40 (0.87-2.26) | 0.160 | 56 | 19.6 | 31 | 18.1 | 0.89 (0.46-1.73) | 0.723 |
| Specific phobia | 307 | 22.2 | 53 | 31.3 | 1.54 (1.02-2.33) | 0.038 | 78 | 26.1 | 41 | 33.5 | 1.36 (0.77-2.42) | 0.283 |
| Anxiety symptoms without full criteria | 708 | 50.9 | 79 | 39.1 | 0.61 (0.43-0.87) | 0.007 | 132 | 42.6 | 51 | 35.2 | 0.75 (0.47-1.19) | 0.221 |
|
|
|
|||||||||||
| Comorbidityc: | ||||||||||||
| Major depressive disorder | 419 | 29.9 | 68 | 36.5 | 1.34 (0.87-2.09) | 0.181 | 109 | 31.7 | 57 | 42.7 | 1.62 (0.95-2.75) | 0.077 |
| Personality disorderse | 593 | 43.8 | 118 | 64.3 | 2.32 (1.60-3.35) | <0.001 | 174 | 57.4 | 89 | 66.3 | 1.38 (0.88-2.18) | 0.158 |
| Non-alcohol drug use disorderf | 28 | 2.3 | 26 | 15.7 | 7.70 (3.39-17.52) | <0.001 | 17 | 6.0 | 25 | 20.7 | 3.69 (1.58-8.60) | 0.003 |
| Nicotine dependence | 430 | 31.6 | 118 | 66.0 | 4.32 (2.85-6.56) | <0.001 | 159 | 51.8 | 94 | 70.2 | 2.03 (1.20-3.46) | 0.010 |
|
|
|
|||||||||||
| Family history of alcoholism: | ||||||||||||
| Absent | 733 | 54.0 | 67 | 31.6 | 1.00 | 124 | 42.2 | 47 | 29.6 | 1.00 | ||
| Present | 646 | 46.0 | 121 | 68.4 | 2.70 (1.84-3.98) | <0.001 | 182 | 57.8 | 89 | 70.4 | 1.87 (1.13-3.09) | 0.016 |
|
|
|
|||||||||||
| Treatment of anxiety symptomsg: | ||||||||||||
| None | 673 | 48.5 | 93 | 46.6 | 1.00 | 144 | 51.2 | 68 | 46.4 | 1.00 | ||
| Any | 706 | 51.5 | 95 | 53.4 | 1.05 (0.71-1.54) | 0.808 | 162 | 48.8 | 68 | 53.6 | 1.14 (0.67-1.95) | 0.619 |
Indicates pattern of drinking in the past year. There is missing data for 5 participants for the sample to assess development of alcohol dependence.
Indicates the number of alcoholic drinks consumed on drinking days in the past year. There is missing data for 5 participants for the development sample, and missing data for 2 participants in the persistence sample.
Diagnostic categories are not mutually exclusive.
GAD, generalized anxiety disorder.
Includes antisocial, narcissistic, histrionic, borderline, schizoid, schizotypal, paranoid, obsessive-compulsive, dependent and avoidant personality disorders.
Includes lifetime history of abuse and/or dependence on non-alcohol substances: heroin, other opioids, cocaine, cannabis, stimulants, and/or hallucinogens.
Indicates any lifetime treatment history of anxiety symptoms including outpatient therapy, medication treatment and/or inpatient hospitalization.
Table 2.
Characteristics of NESARC participants with anxiety symptoms by report of self-medication with alcohol at the wave 1 (baseline) interview within the sample used to assess the subsequent occurrence of alcohol dependence (n=1567) at wave 2, and the persistence of alcohol dependence (n=442).
| Characteristics at baseline |
Sample to
Assess Alcohol Dependence at follow-up |
Sample to
Assess Persistence of Alcohol Dependence |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Alcohol self-medication at baseline | Bivariate logistic regression analyses | Alcohol self-medication at baseline | Bivariate logistic regression analyses | |||||||||
|
|
|
|||||||||||
| Absent | Present | Absent | Present | |||||||||
|
| ||||||||||||
| N | % | N | % | OR (95% CI) | p | N | % | N | % | OR (95% CI) | p | |
|
|
|
|||||||||||
| Sex: | ||||||||||||
| Male | 439 | 35.8 | 81 | 47.8 | 1.00 | 0.004 | 157 | 53.7 | 61 | 54.3 | 1.00 | |
| Female | 938 | 64.2 | 109 | 52.2 | 0.61 (0.43-0.85) | 164 | 46.3 | 60 | 45.7 | 0.98 (0.58-1.64) | 0.930 | |
|
|
|
|||||||||||
| Age (years): | ||||||||||||
| 18-35 | 399 | 29.5 | 83 | 49.4 | 1.00 | 111 | 35.2 | 53 | 48.6 | 1.00 | ||
| 36-49 | 474 | 35.3 | 67 | 32.3 | 0.54 (0.35-0.84) | 0.007 | 123 | 38.7 | 45 | 36.0 | 0.67 (0.38-1.20) | 0.175 |
| 50+ | 504 | 35.2 | 40 | 18.2 | 0.31 (0.19-0.49) | <0.001 | 87 | 26.2 | 23 | 15.4 | 0.43 (0.22-0.82) | 0.011 |
|
|
|
|||||||||||
| Race/ethnicity: | ||||||||||||
| White | 1014 | 84.2 | 137 | 78.6 | 1.00 | 256 | 87.3 | 87 | 74.4 | 1.00 | ||
| Black | 182 | 7.0 | 24 | 10.5 | 1.60 (0.94-2.73) | 0.081 | 30 | 4.3 | 15 | 12.1 | 3.29 (1.51-7.20) | 0.003 |
| Hispanic/Other | 181 | 8.8 | 29 | 10.9 | 1.32 (0.72-2.45) | 0.365 | 35 | 8.4 | 19 | 13.5 | 1.89 (0.78-4.61) | 0.157 |
|
|
|
|||||||||||
| Education (years): | ||||||||||||
| <12 | 165 | 11.1 | 29 | 18.1 | 1.00 | 39 | 12.0 | 22 | 23.1 | 1.00 | ||
| ≥12 | 1212 | 88.9 | 161 | 81.9 | 0.56 (0.31-1.02) | 0.058 | 282 | 88.0 | 99 | 76.9 | 0.45 (0.22-0.96) | 0.039 |
|
|
|
|||||||||||
| Drinking patterna: | ||||||||||||
| <Daily | 1240 | 89.7 | 130 | 67.7 | 1.00 | 278 | 87.2 | 68 | 55.1 | 1.00 | ||
| Daily/nearly daily | 132 | 10.3 | 60 | 32.3 | 4.15 (2.81-6.12) | <0.001 | 43 | 12.8 | 53 | 44.9 | 5.54 (3.10-9.89) | <0.001 |
|
|
|
|||||||||||
| Drink levelb: | ||||||||||||
| <5 on drinking days | 1260 | 90.8 | 123 | 64.0 | 1.00 | 261 | 81.3 | 65 | 54.3 | 1.00 | ||
| ≥5 on drinking days | 113 | 9.2 | 66 | 36.0 | 5.57 (3.52-8.80) | <0.001 | 59 | 18.7 | 55 | 45.7 | 3.66 (1.98-6.75) | <0.001 |
|
|
|
|||||||||||
| Anxiety disorderc: | ||||||||||||
| GADd | 391 | 28.6 | 112 | 55.7 | 3.14 (2.14-4.62) | <0.001 | 98 | 30.5 | 69 | 51.0 | 2.37 (1.37-4.11) | 0.003 |
| Panic disorder | 100 | 7.2 | 27 | 13.6 | 2.02 (1.13-3.61) | 0.018 | 32 | 9.4 | 21 | 16.2 | 1.86 (0.90-3.85) | 0.093 |
| Social phobia | 163 | 12.4 | 52 | 24.0 | 2.23 (1.47-3.37) | <0.001 | 50 | 15.7 | 37 | 28.0 | 2.09 (1.19-3.69) | 0.012 |
| Specific phobia | 296 | 22.1 | 64 | 32.6 | 1.70 (1.15-2.52) | 0.009 | 79 | 26.2 | 40 | 34.7 | 1.50 (0.86-2.61) | 0.149 |
| Anxiety symptoms without full criteria | 742 | 53.3 | 45 | 22.1 | 0.25 (0.16-0.37) | <0.001 | 154 | 46.7 | 29 | 23.2 | 0.34 (0.20-0.58) | <0.001 |
|
|
|
|||||||||||
| Comorbidityc: | ||||||||||||
| Major depressive disorder | 394 | 27.7 | 93 | 52.0 | 2.82 (1.90-4.20) | <0.001 | 102 | 27.8 | 64 | 54.8 | 3.14 (1.81-5.46) | <0.001 |
| Personality disorderse | 587 | 43.9 | 124 | 64.2 | 2.29 (1.59-3.30) | <0.001 | 174 | 55.1 | 89 | 73.8 | 2.30 (1.38-3.83) | 0.002 |
| Non-alcohol drug use disorderf | 24 | 2.3 | 30 | 16.2 | 8.13 (4.10-16.12) | <0.001 | 15 | 6.0 | 27 | 23.2 | 4.72 (2.12-10.49) | <0.001 |
| Nicotine dependence | 443 | 33.7 | 105 | 52.2 | 2.14 (1.46-3.16) | <0.001 | 172 | 55.7 | 81 | 63.4 | 1.38 (0.77-2.46) | 0.273 |
|
|
|
|||||||||||
| Family history of alcoholism: | ||||||||||||
| Absent | 721 | 53.3 | 79 | 36.2 | 1.00 | 124 | 40.5 | 47 | 31.8 | 1.00 | ||
| Present | 656 | 46.7 | 111 | 63.8 | 2.01 (1.36-2.95) | 0.001 | 197 | 59.5 | 74 | 68.2 | 1.46 (0.83-2.57) | 0.188 |
|
|
|
|||||||||||
| Treatment of anxiety symptomsg: | ||||||||||||
| None | 693 | 49.0 | 73 | 43.2 | 1.00 | 166 | 52.4 | 46 | 42.5 | 1.00 | ||
| Any | 684 | 51.0 | 117 | 56.8 | 1.26 (0.88-1.80) | 0.194 | 155 | 47.6 | 75 | 57.5 | 1.49 (0.89-2.49) | 0.128 |
Indicates pattern of drinking in the past year. There is missing data for 5 participants for the sample to assess development of alcohol dependence.
Indicates the number of alcoholic drinks consumed on drinking days in the past year. There is missing data for 5 participants for the development sample, and missing data for 2 participants in the persistence sample.
Diagnostic categories are not mutually exclusive.
GAD, generalized anxiety disorder.
Includes antisocial, narcissistic, histrionic, borderline, schizoid, schizotypal, paranoid, obsessive-compulsive, dependent and avoidant personality disorders.
Includes lifetime history of abuse and/or dependence on non-alcohol substances: heroin, other opioids, cocaine, cannabis, stimulants, and/or hallucinogens.
Indicates any lifetime treatment history of anxiety symptoms including outpatient therapy, medication treatment and/or inpatient hospitalization.
In our adjusted analyses, completed by including the propensity score as a covariate in the multivariate regression analyses, drinking self-medication of anxiety symptoms at baseline was associated with the subsequent occurrence of alcohol dependence at follow-up (adjusted odds ratio (AOR)=5.71, CI=3.56-9.18, p<0.001) and with the persistence of alcohol dependence (AOR=6.25, CI=3.24-12.05, p<0.001). In our analyses to assess self-medication with incident alcohol dependence after excluding baseline cases of alcohol dependence (n=1359), we had similar findings using three different approaches: propensity score adjustment (AOR=3.91, CI=2.05-7.49, p<0.001), 10 to 1 matching (AOR=4.41, CI=2.34-8.30, p<0.001, and subclassification (AOR=3.49, CI=1.17-10.38, p<0.025) (Table 3). However, sample size limitations precluded using this group for our exploratory stratified analyses described below, which were completed assessing occurrence of alcohol dependence at follow-up holding constant a history of lifetime dependence at baseline.
Table 3.
Use of different propensity score methods to assess the association of reports of drinking to self-medicate anxiety symptoms at baseline with the incidence of alcohol dependence at follow-up (wave 2, N=1359).
| Method | AORa | 95% CI | p-value |
|---|---|---|---|
| Logistic regression with propensity score adjustment | 3.91 | 2.05-7.49 | <0.0001 |
| Propensity score using matching (10:1) | 4.41 | 2.34-8.30 | <0.001 |
| Propensity score - subclassification | 3.49 | 1.17-10.38 | 0.025 |
Note: These analyses remove 208 baseline (wave 1) cases of alcohol dependence.
All analyses were adjusted for age, education, race/ethnicity, family history of alcoholism, alcohol abuse at wave 1, lifetime history of an anxiety disorder, major depression, nonalcohol substance use disorder, lifetime history of nicotine dependence, treatment history, and wave 2 survey weights. The matching model also adjusted for sex.
The population attributable fraction for drinking self-medication with development of alcohol dependence was calculated for the study sample assessing incident dependence at wave 2 after excluding baseline cases of alcohol dependence. In these analyses, the PAF was estimated to be 12.7% (CI=-1.1-24.6%) indicating that approximately 13% of incident cases of alcohol dependence among individuals with anxiety symptoms in our population potentially could be attributed to self-medication with alcohol. For the analyses involving persistence of dependence, the PAF was estimated to be 33.4% (CI=22.5-42.7%). Thus, an estimated one-third of the persistent cases of alcohol dependence among individuals with anxiety symptoms potentially could be attributed to their use of alcohol to self-medicate, cope with or relieve their anxiety.
In our exploratory examination of subgroups of drinkers with anxiety symptoms, we assessed the association of drinking self-medication with the subsequent occurrence and persistence of dependence by specific subgroup strata (Figures 1 and 2). We assessed subgroups by sex, age, race-ethnicity, history of treatment for anxiety symptoms, severity of symptoms (meeting full DSM criteria for an anxiety disorder, and those with sub-threshold symptoms), alcohol consumption level and family history of alcoholism. In these analyses, we found little evidence for interaction across these characteristics, with positive and strong associations for virtually all characteristics assessed and within all strata. Within related strata, AORs were not appreciably different, and confidence intervals overlapped. Smaller subgroup size within strata resulted in generally wide confidence limits. However, with few exceptions all associations met criteria for statistical significance.
Figure 1.
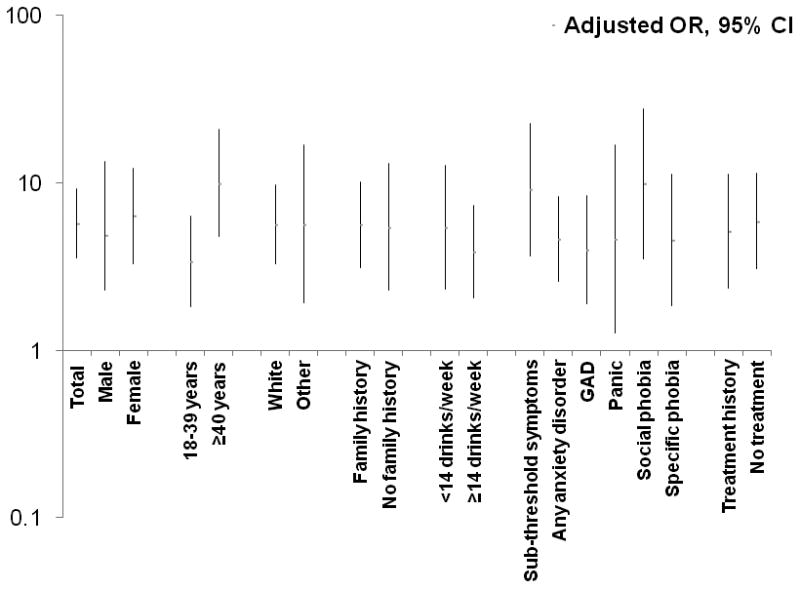
Multivariate analyses of the total sample and within strata of the association of baseline alcohol self-medication for anxiety symptoms with the subsequent occurrence of alcohol dependence at follow-up among NESARC participants using propensity score adjustmenta (n=1,567).
aAdjustment was completed by propensity scores of the probability of self-medication for anxiety symptoms. The covariates used to estimate the propensity score for the analyses of alcohol dependence development included age, sex, race-ethnicity, educational level, lifetime history of alcohol dependence with or without alcohol abuse, drinking pattern and consumption level on drinking days in the past year, current history of an anxiety disorder (generalized anxiety, panic, social and specific phobia), affective disorder (major depression, bipolar disorder, and dysthymia), non-alcohol substance use disorder, nicotine dependence, personality disorder, family history of alcoholism, and lifetime treatment for anxiety symptoms, wave 2 survey weights, and interaction terms for each variable stratified.
Figure 2.
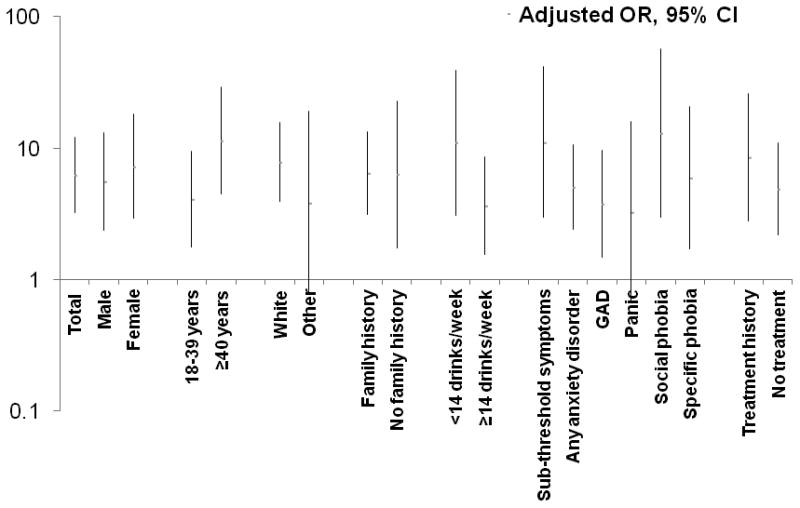
Multivariate analyses of the total sample and within strata of the association of baseline alcohol self-medication for anxiety symptoms with the persistence of alcohol dependence at follow-up among NESARC participants with a lifetime history of alcohol dependence using propensity score adjustmenta (n=442).
aAdjustment was completed by propensity scores of the probability of self-medication for anxiety symptoms. The covariates used to estimate the propensity score for the analyses of alcohol dependence persistence included age, sex, race-ethnicity, educational level, drinking pattern and consumption level on drinking days in the past year, current history of an anxiety disorder (generalized anxiety, panic, social and specific phobia), affective disorder (major depression, bipolar disorder, and dysthymia), non-alcohol substance use disorder, nicotine dependence, personality disorder, family history of alcoholism, and lifetime treatment for anxiety symptoms, wave 2 survey weights, and interaction terms for each variable stratified.
Discussion
Consistent with our a priori hypotheses, reports of drinking to self-medicate anxiety symptoms was associated with both the development and persistence of alcohol dependence in this population-based sample. These findings are consistent with earlier analyses of this dataset,28;41 but also extend the prior findings in several ways. First, although prior analyses from our research group found an association with alcohol dependence, there are limitations with the use of logistic regression to hold constant potential confounders.42;43 Using propensity score methods in this report increased our confidence that the associations found were less likely to be due to confounding. The propensity score methods aid in reducing selection bias, and in adjusting for multiple observed covariates. For example, one possible explanation for the relationship between self-medication drinking and alcohol dependence is that individuals who report self-medicating with alcohol are more likely to develop dependence because of a relatively higher and more frequent consumption pattern. However, even after adjustment for these and other confounding characteristics, we found a consistent association of self-medication with alcohol dependence. In supplementary analyses, we were also able to show that use of each of the other main types of propensity score methods yielded similar findings. Second, our current analyses extended prior findings by examining the potential risk for self-medication to increase chronicity or persistence of alcohol dependence. Although prior analyses have examined this association with alcohol abuse and dependence combined as an alcohol use disorder category,28 recent recommendations suggest the need to separate these conditions.30 Alcohol abuse has appreciably weaker associations with anxiety disorders,1;4 and may be influenced by social and cultural factors.30;31 The examination of self-medication drinking with persistence of alcohol dependence has not been assessed in prior longitudinal population-based samples. Using data from this general population sample reduces the potential selection biases that are likely to be present in an assessment of patients in a clinical setting. For example, we were able to assess whether treatment history would alter the self-medication/dependence association. Study participants both with and without a treatment history for their anxiety symptoms had strong positive associations of self-medication drinking with alcohol dependence. Third, in the current report, we were able to explore potential effect modification by specific sociodemographic, treatment, and comorbidity factors. However, no clear pattern of varying associations by sex, age, race-ethnicity, alcohol consumption level, family history of alcoholism, anxiety disorder diagnosis as opposed to sub-threshold symptoms, or treatment history were observed. Self-medication drinking was positively associated with dependence within each of these subgroups. Individuals with sub-threshold symptoms who self-medicate with alcohol as well as those who met full criteria for an anxiety diagnosis had strong associations with subsequent dependence. Although firm conclusions are not possible because of small subgroup sample sizes, individuals with sub-threshold symptoms had as strong or stronger association with alcohol dependence as compared with those who met full criteria for an anxiety disorder. However, those with sub-threshold symptoms are less likely to reach clinical attention and receive treatment for their anxiety.
Additional findings from our analyses indicate that within this sample of drinkers who report anxiety symptoms, a proportion of the cases of both newly developed as well as persistent dependence can be attributed to use of alcohol to relieve or cope with feelings of anxiety. We found that approximately 13% of new onset cases and 33% of persistent cases were potentially attributable to self-medication of anxiety symptoms with alcohol. This highlights the potential for prevention and early intervention efforts that may reduce the occurrence of alcohol dependence. Attention needs to be given to evaluation and treatment of both the anxiety symptoms as well as the subsequent consumption, particularly with the onset of problematic drinking.44;45 In addition, educational efforts among clinical populations may be necessary to minimize the use of alcohol as a method of relieving or treating anxiety; incorporating these efforts as a brief intervention may be possible.46
Several limitations in the analyses should be mentioned. First, although we were able to use propensity score methods to adjust for many potential confounding characteristics, residual confounding by unmeasured factors is still a possibility. For example, macrosocial factors related to available health care may still be viable explanations for the current findings and would need to be examined in future investigations. In addition, information on the frequency and quantity of self-medication drinking was not available. Second, because information for all the characteristics assessed was gathered by self-report, occurrences of reporting biases and misclassification, particularly for some characteristics such as family history and quantity and frequency of alcohol consumption are possible. Furthermore, it is plausible that some individuals underreport self-medication drinking. Participants have to be able to recognize and acknowledge this behavior. Yet, underreporting of self-medication drinking among participants with anxiety symptoms would likely attenuate the relationship between self-medication and dependence. This may indicate that our current findings underestimate the strength of the associations for drinking self-medication with alcohol dependence. Third, the stratified analyses should be considered as exploratory given the limitations in subgroup sample sizes. Furthermore, although associations within each stratum were typically strongly positive, the ability to assess statistical significance between related strata was reduced given the large standard errors. Fourth, our assessment of occurrence of alcohol dependence at wave 2 was based on individuals who met criteria for alcohol dependence within the prior year of follow-up, holding constant a history of alcohol dependence at baseline. Although our findings were similar after excluding alcohol dependence cases identified at wave 1, we were not able to use this sample for the stratified analyses because of limited power. Finally, because this was not an experience sampling approach as has been done previously to assess self-medication with alcohol,47 we were not able to adequately assess the temporal relationship between the experience of anxiety during an individual's day with the subsequent use of alcohol. Experience sampling would enhance our ability to more directly link anxiety symptoms with drinking behavior, but would not be readily feasible in a large cohort followed for the extended time necessary to observe transition to alcohol dependence.
Notwithstanding these limitations, the current findings extend prior work assessing self-medication of anxiety symptoms with the onset of alcohol dependence using methodology that helps to confirm this association. In addition, we present new findings related to the chronicity of alcohol dependence and begin an exploration of self-medication within subgroups of the population. The implication for potential prevention is highlighted by the proportion of cases of alcohol dependence among individuals with anxiety symptoms that can be attributed to self-medication behavior. This may be a useful target for intervention efforts that may aid in reducing the occurrence of alcohol dependence.
Acknowledgments
The analyses and preparation of this project were supported by grants from the National Institute on Alcohol Abuse and Alcoholism (AA016346), and the National Institute on Drug Abuse (DA030460). Preparation of this paper also was supported a National Institute on Alcohol Abuse and Alcoholism Research Supplement to Promote Diversity in Health-Related Research (R01AA010158-12S1 (AAHA)), and by grants from the Canadian Institutes of Health Research New Investigator Award (152348) and a Manitoba Health Research Council Chair award (JS). In the past 3 years, RM has received consultant fees from Lundbeck pharmaceuticals.
References
- 1.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Robins LN, Regier DA. Psychiatric disorders in America: The Epidemiologic Catchment Area Study. New York: The Free Press/MacMillan, Inc.; 1991. [Google Scholar]
- 3.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 4.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. The lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 5.Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. Am J Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- 6.Schneier FR, Martin NY, Leibowitz MR, et al. Alcohol abuse in social phobia. J Anxiety Disord. 1989;3:15–23. [Google Scholar]
- 7.Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM. Social phobia. Comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry. 1992;49:282–288. doi: 10.1001/archpsyc.1992.01820040034004. [DOI] [PubMed] [Google Scholar]
- 8.Schuckit MA, Hesselbrock V. Alcohol dependence and anxiety disorders: What is the Relationship? Am J Psychiatry. 1994;151:1723–1734. doi: 10.1176/ajp.151.12.1723. [DOI] [PubMed] [Google Scholar]
- 9.Pakriev S, Vasar V, Aluoja A, Shlik J. Prevalence of ICD-10 harmful use of alcohol and alcohol dependence among the rural population of Udmurtia. Alcohol Alcohol. 1998;33:255–264. doi: 10.1093/oxfordjournals.alcalc.a008389. [DOI] [PubMed] [Google Scholar]
- 10.Driessen M, Veltrup C, Wetterling T, John U, Dilling H. Axis I and Axis II comorbidity in alcohol dependence and the two types of alcoholism. Alcohol Clin Exp Res. 1998;22:77–86. [PubMed] [Google Scholar]
- 11.Crum RM, Pratt LA. Risk of heavy drinking and alcohol use disorders in social phobia: a prospective analysis. Am J Psychiatry. 2001;158:1693–1700. doi: 10.1176/appi.ajp.158.10.1693. [DOI] [PubMed] [Google Scholar]
- 12.Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. Am J Psychiatry. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- 13.Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the National Cormorbidity Survey. Arch Gen Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- 14.Swendsen JD, Merikangas KR, Canino GJ, Kessler RC, Rubio-Stipec M, Angst J. The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Compr Psychiatry. 1998;39:176–184. doi: 10.1016/s0010-440x(98)90058-x. [DOI] [PubMed] [Google Scholar]
- 15.Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry. 1998;34:24–28. [PubMed] [Google Scholar]
- 16.Kushner MG, Maurer E, Menary K, Thuras P. Vulnerability to the rapid (“telescoped”) development of alcohol dependence in individuals with anxiety disorder. J Stud Alcohol Drugs. 2011;72:1019–1027. doi: 10.15288/jsad.2011.72.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olgiati P, Liappas I, Malitas P, et al. Depression and social phobia secondary to alcohol dependence. Neuropsychobiology. 2007;56:111–118. doi: 10.1159/000112952. [DOI] [PubMed] [Google Scholar]
- 18.Carrigan MH, Randall CL. Self-medication in social phobia: a review of the alcohol literature. Addict Behav. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- 19.Schneier FR, Foose TE, Hasin DS, et al. Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2010;40:977–988. doi: 10.1017/S0033291709991231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cosci F, Schruers KR, Abrams K, Griez EJ. Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship. J Clin Psychiatry. 2007;68:874–880. doi: 10.4088/jcp.v68n0608. [DOI] [PubMed] [Google Scholar]
- 21.Flensborg-Madsen T, Mortensen EL, Knop J, Becker U, Sher L, Gronbaek M. Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: results from a Danish register-based study. Compr Psychiatry. 2009;50:307–314. doi: 10.1016/j.comppsych.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Merikangas KR, Stevens DE, Fenton B, et al. Co-morbidity and familial aggregation of alcoholism and anxiety disorders. Psychol Med. 1998;28:773–788. doi: 10.1017/s0033291798006941. [DOI] [PubMed] [Google Scholar]
- 23.Khantzian EJ. Self-regulation and self-medication factors in alcoholism and the addictions. Similarities and differences. Recent Dev Alcohol. 1990;8:255-71–255-271. [PubMed] [Google Scholar]
- 24.Rutledge PC, Sher KJ. Heavy drinking from the freshman year into early young adulthood: the roles of stress, tension-reduction drinking motives, gender and personality. J Stud Alcohol. 2001;62:457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- 25.Naftolowitz DF, Vaughn BV, Ranc J, Tancer ME. Response to alcohol in social phobia. Anxiety. 1994;1:96–99. doi: 10.1002/anxi.3070010209. [DOI] [PubMed] [Google Scholar]
- 26.Himle JA, Abelson JL, Haghightgou H, Hill EM, Nesse RM, Curtis GC. Effect of alcohol on social phobic anxiety. Am J Psychiatry. 1999;156:1237–1243. doi: 10.1176/ajp.156.8.1237. [DOI] [PubMed] [Google Scholar]
- 27.Abrams K, Kushner M, Medina KL, Voight A. The pharmacologic and expectancy effects of alcohol on social anxiety in individuals with social phobia. Drug Alcohol Depend. 2001;64:219–231. doi: 10.1016/s0376-8716(01)00125-9. [DOI] [PubMed] [Google Scholar]
- 28.Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch Gen Psychiatry. 2011;68:800–807. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- 29.Rosenbaum PR. Observational studies. 2nd. Springer; 2000. [Google Scholar]
- 30.Babor TF, Caetano R. The trouble with alcohol abuse: what are we trying to measure, diagnose, count and prevent? Addiction. 2008;103:1057–1059. doi: 10.1111/j.1360-0443.2008.02263.x. [DOI] [PubMed] [Google Scholar]
- 31.Keyes KM, Hasin DS. Socio-economic status and problem alcohol use: the positive relationship between income and the DSM-IV alcohol abuse diagnosis. Addiction. 2008;103:1120–1130. doi: 10.1111/j.1360-0443.2008.02218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robinson JA, Sareen J, Cox BJ, Bolton JM. Correlates of self-medication for anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Nerv Ment Dis. 2009;197:873–878. doi: 10.1097/NMD.0b013e3181c299c2. [DOI] [PubMed] [Google Scholar]
- 33.Robinson J, Sareen J, Cox BJ, Bolton J. Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. J Anxiety Disord. 2009;23:38–45. doi: 10.1016/j.janxdis.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–50. [Google Scholar]
- 35.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 37.Ruan WJ, Goldstein RB, Chou SP, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 39.Zanutto E, Lu B, Hornik R. Using propensity score subclassification for multiple treatment doses to evaluate a national antidrug media campaign. J Educ Behav Statistics. 2005;30:59–73. [Google Scholar]
- 40.Newson R. PUNAF: Stata module to compute population attributable fractions for cohort studies. [Accessed April 28, 2011]; at http://ideas.repec.org/c/boc/bocode/s457193.html.
- 41.Menary KR, Kushner MG, Maurer E, Thuras P. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. J Anxiety Disord. 2011;25:335–339. doi: 10.1016/j.janxdis.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010;13:273–277. doi: 10.1111/j.1524-4733.2009.00671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rubin DB. Propensity score methods. Am J Ophthalmol. 2010;149:7–9. doi: 10.1016/j.ajo.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 44.De Bernardo GL, Newcomb M, Toth A, Richey G, Mendoza R. Comorbid psychiatric and alcohol abuse/dependence disorders: psychosocial stress, abuse, and personal history factors of those in treatment. J Addict Dis. 2002;21:43–59. doi: 10.1300/J069v21n03_04. [DOI] [PubMed] [Google Scholar]
- 45.Goldsmith RJ, Garlapati V. Behavioral interventions for dual-diagnosis patients. Psychiatr Clin North Am. 2004;27:709–725. doi: 10.1016/j.psc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 46.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 47.Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: an experience sampling test of the self-medication hypothesis. J Abnorm Psychol. 2000;109:198–204. [PubMed] [Google Scholar]


