Abstract
SHANK genes code for scaffold proteins located at the post-synaptic density of glutamatergic synapses. In neurons, SHANK2 and SHANK3 have a positive effect on the induction and maturation of dendritic spines, whereas SHANK1 induces the enlargement of spine heads. Mutations in SHANK genes have been associated with autism spectrum disorders (ASD), but their prevalence and clinical relevance remain to be determined. Here, we performed a new screen and a meta-analysis of SHANK copy-number and coding-sequence variants in ASD. Copy-number variants were analyzed in 5,657 patients and 19,163 controls, coding-sequence variants were ascertained in 760 to 2,147 patients and 492 to 1,090 controls (depending on the gene), and, individuals carrying de novo or truncating SHANK mutations underwent an extensive clinical investigation. Copy-number variants and truncating mutations in SHANK genes were present in ∼1% of patients with ASD: mutations in SHANK1 were rare (0.04%) and present in males with normal IQ and autism; mutations in SHANK2 were present in 0.17% of patients with ASD and mild intellectual disability; mutations in SHANK3 were present in 0.69% of patients with ASD and up to 2.12% of the cases with moderate to profound intellectual disability. In summary, mutations of the SHANK genes were detected in the whole spectrum of autism with a gradient of severity in cognitive impairment. Given the rare frequency of SHANK1 and SHANK2 deleterious mutations, the clinical relevance of these genes remains to be ascertained. In contrast, the frequency and the penetrance of SHANK3 mutations in individuals with ASD and intellectual disability—more than 1 in 50—warrant its consideration for mutation screening in clinical practice.
Author Summary
Autism spectrum disorders (ASD) are a heterogeneous group of neurodevelopmental disorders. Mutations altering genes involved in the junction between brain cells have been repeatedly associated in ASD. For example, SHANK1, SHANK2 and SHANK3 emerged as one family of genes that are associated with ASD. However, little was known about the number of patients carrying these mutations and the clinical outcome. Here, we performed a new genetic screen of SHANK mutations and these results were analyzed in combination with those of the literature. In summary, SHANK mutations account for ∼1% of patients with ASD and were detected in the whole spectrum of autism with a gradient of severity in cognitive impairment: mutations in SHANK1 were rare (0.04%) and present in males with normal IQ and autism; mutations in SHANK2 were present in 0.17% of patients with ASD and mild intellectual disability; mutations in SHANK3 were present in 0.69% of patients with ASD and up to 2.12% of the cases with moderate to profound intellectual disability. Given the high frequency and impact of SHANK3 mutations in individuals with ASD and intellectual disability—more than 1 in 50—this gene should be screened for mutations in clinical practice.
Introduction
Autism spectrum disorders (ASD) are characterized by impairments in reciprocal social communication and stereotyped behaviors. There is strong evidence of the involvement of different forms of genetic variations in ASD [1], [2]. In particular, chromosomal rearrangements, rare de novo copy-number variants and de novo coding-sequence variants may account for more than 20% of the cases [1], [2]. These events have implicated more than 100 genes [3], but each gene or genomic alteration often accounts for less than 1% of the cases. Many of the genes associated with the disorder are involved in the development or functioning of neuronal circuits [4]. In particular, mutations in genes coding for synaptic cell adhesion molecules and scaffold proteins — such as neuroligins, neurexins and SHANK — have been repeatedly reported in individuals with ASD [5]–[10]. These proteins play a crucial role in the formation and stabilization of synapses [11], [12]. The synapse has therefore emerged as a common target for the different genetic mutations that affect chromatin remodeling, synaptic translation, formation and functioning [4].
Here, we focused on the three SHANK genes, which code for large synaptic scaffold proteins of the post-synaptic density [12]. Deletions, duplications and coding mutations in the SHANK genes have been recurrently reported in patients with ASD [6], [8]–[10], [13]–[20]. SHANK3 haploinsufficiency has been identified in more than 900 patients affected with chromosome 22q13 deletion syndrome, known as Phelan–McDermid syndrome [15]. The genomic rearrangements observed in these patients are diverse ranging from simple 22q13 deletions (72%), ring chromosomes (14%), unbalanced translocations (7%) to interstitial deletions (9%), all resulting in haploinsufficiency of the SHANK3 gene [21].
The majority of these patients have neonatal hypotonia, moderate to severe intellectual disability (ID), absent to severely delayed speech, and minor dysmorphic features [15]. In more than 80% of the cases, autism or autistic-like behavior is present [22]. De novo or truncating mutations in SHANK3 have also been observed in individuals with ASD [6], [13], [16], [17]. Few studies have explored SHANK1 and SHANK2 in ASD, but all have led to the conclusion that deleterious mutations in these genes contribute to the disorder [14], [18], [19].
Mice lacking any of the SHANK proteins display phenotypes relevant to ASD [23]. Shank1 knock-out mice show increased anxiety, decreased vocal communication, decreased locomotion and remarkably, enhanced working memory, but decreased long-term memory [24], [25]. Shank2 knock-out mice show hyperactivity, increased anxiety, repetitive grooming, and abnormalities in vocal and social behaviors [26], [27]. Shank3 knock-out mice show self-injurious repetitive grooming, and deficits in social interaction and communication [28]–[30].
While there is increasing evidence of an association between SHANK genes and ASD, SHANK mutations are considered to affect only a limited number of patients and as a consequence, these genes are not routinely sequenced in clinical practice. In addition, sequence gaps and annotation errors of SHANK2 and SHANK3 in the human genome assembly (hg19) have led to incorrect interpretations of sequencing results obtained in patients [15]. Finally, the clinical impact of the mutations in the SHANK genes is still largely unknown.
Our hypothesis was that mutations in SHANK genes might be more frequent in patients with ASD than previously suggested, and that each gene might be associated with specific clinical profiles. To conduct this study, we first corrected the reference sequence of SHANK2 and SHANK3 (Table S1, Figure S1 & S2 and Text S1: Supplementary Methods). We then analyzed a large number of individuals with ASD for SHANK copy-number variants and coding-sequence variants and combined these results with those reported in the literature. Finally, we performed an extended clinical investigation in all patients carrying de novo or truncating SHANK mutations.
Results
Cohorts used for the meta-analysis of SHANK mutations
We performed a meta-analysis of copy-number variants and coding sequence variants in all SHANK genes (Figure 1). This meta-analysis included the published data from 14 studies in addition to a new screening of SHANK copy-number variants and coding sequence variants. The number of individuals tested and the result of the meta-analysis are reported in the Table 1, Figures 2 and 3 and Table S2, S3, S4, S5, S6. In addition to the results from the literature, we performed a new copy-number variants analysis of 46 additional cases with ASD and 454 matched controls. We also performed a mutation screening of all SHANK1 exons in 743 independent individuals including 251 cases with ASD and 492 controls. Finally, we added 429 new independent cases with ASD and 80 new independent controls to our original screening of coding-sequence variants of SHANK3 [6]. When possible, the patients carrying truncating mutations altering SHANK genes underwent further clinical investigations (Table 2 & S7). The meta-analysis of the frequency of CNVs and coding-sequence variants altering SHANK genes in patients with ASD and in controls were also performed using IQ as a co-variable (Figure 4).
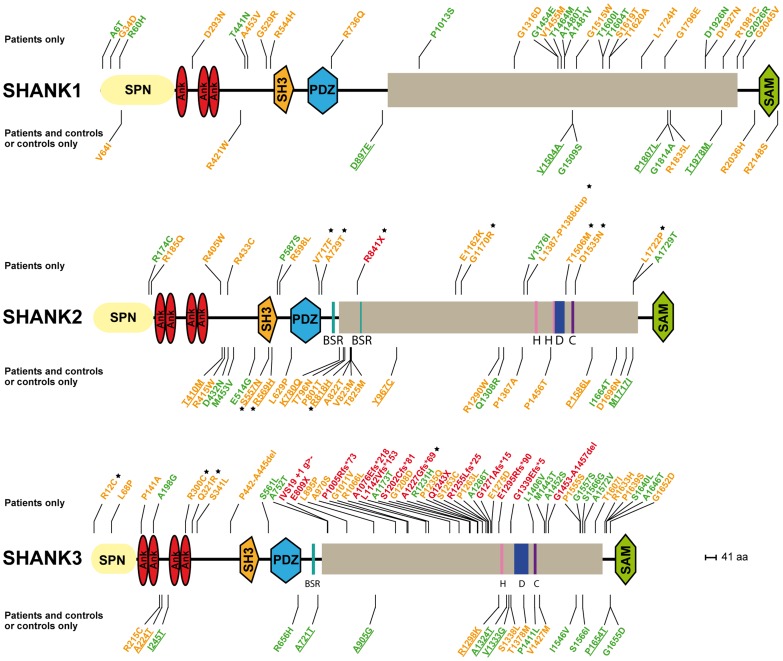
Figure 1. SHANK variants in patients with ASD and controls.
Coding-sequence variants identified only in patients with ASD (upper panel), shared by patients and controls (lower panel and underlined), and present only in controls (lower panel). Truncating variants are indicated in red. The variants predicted as deleterious or benign are indicated in orange and green, respectively. Coding-sequence variants with a proven in vitro functional impact are indicated with black stars. Conserved domains are represented in color: SPN (yellow), Ankyrin (red), SH3 (orange), PDZ (blue) and SAM (green).
Table 1. Prevalence of SHANK rare coding-sequence and copy-number variants in patients with ASD and controls.
| Number of studies | Number of reported carriers of rare SHANK variants | Prevalence of carriers of rare SHANK variants (%) | Fisher's exact test | Meta-analysis - Inverse variance method (FEM) | Meta-analysis - Inverse variance method (REM) | ||||||
| Total | ASD | Controls | ASD | Controls | Odds ratio | P-value | Odds ratio | P-value | Odds ratio | P-value | |
| SHANK1 | |||||||||||
| Coding-sequence variants a | 2b | ||||||||||
| All | 42/760 | 15/492 | 5.53 [4.01–7.4] | 3.05 [1.72–4.98] | 1.86 [1.00–3.65] | 0.051 | - | - | - | - | |
| Damaging missense | 24/760 | 5/492 | 3.16 [2.03–4.66] | 1.02 [0.33–2.36] | 3.17 [1.18–10.72] | 0.012 | - | - | - | - | |
| Truncating mutation | 0/760 | 0/492 | 0.00 [0–0.48] | 0.00 [0–0.75] | 0 [0-∞] | 1 | - | - | - | - | |
| Copy-number variants | 6 | 2/5 657 | 0/19 163 | 0.04 [0–0.13] | 0.00 [0–0.02] | ∞ [0.64-∞] | 0.052 | 2.73 [0.60–12.48] | 0.19 | 2.73 [0.60–12.48] | 0.19 |
| SHANK2 | |||||||||||
| Coding-sequence variants | 2 | ||||||||||
| All | 43/851 | 36/1 090 | 5.05 [3.68–6.75] | 3.30 [2.32–4.54] | 1.56 [0.97–2.52] | 0.064 | 1.44 [0.89–2.32] | 0.13 | 1.34 [0.56–3.22] | 0.51 | |
| Damaging missense | 39/851 | 29/1 090 | 4.58 [3.28–6.21] | 2.66 [1.79–3.8] | 1.76 [1.05–2.97] | 0.025 | 1.58 [0.94–2.66] | 0.082 | 1.46 [0.61–3.52] | 0.39 | |
| Truncating mutation | 1/851 | 0/1 090 | 0.12 [0–0.65] | 0.00 [0–0,34] | ∞ [0.033-∞] | 0.44 | 2.27 [0.21–24.56] | 0.49 | 2.27 [0.21–24.56] | 0.49 | |
| Copy-number variants | 6 | 3/5 657 | 0/19 163 | 0.05 [0.01–0.15] | 0.00 [0.02] | ∞ [1.40-∞] | 0.012 | 3.76 [0.87–16.25] | 0.076 | 3.76 [0.87–16.25] | 0.076 |
| SHANK3 | |||||||||||
| Coding-sequence variants | 5 | ||||||||||
| All | 72/2 147 | 29/1 031 | 3.35 [2.63–4.20] | 2.81 [1.89–4.01] | 1.20 [0.76–1.93] | 0.45 | 1.32 [0.79–2.20] | 0.29 | 1.42 [0.36–5.54] | 0.61 | |
| Damaging missense | 28/2 147 | 11/1 031 | 1.30 [0.87–1.88] | 1.07 [0.53–1.9] | 1.22[0.59–2.74] | 0.73 | 1.41 [0.65–3.07] | 0.38 | 1.42 [0.51–3.90] | 0.50 | |
| Truncating mutation | 11/2 147 | 0/1 031 | 0.51 [0.26–0.91] | 0.00 [0–0.36] | ∞ [1.21-∞] | 0.020 | 2.85 [0.41–19.96] | 0.29 | 2.85 [0.41–19.96] | 0.29 | |
| Copy-number variants | 6 | 10/5 657 | 2/19 163c | 0.18 [0.08–0.32] | 0.01 [0–0.04] | 16.96 [3.61–159.14] | 0.000016 | 4.05 [1.26–13.01] | 0.019 | 4.16 [1.09–15.81] | 0.036 |
All truncating SHANK variants were de novo (for three, the DNA of one parent was not available). In the damaging missense category, two SHANK3 (P141A & Q321R) were de novo.
For SHANK1, there are two studies (Sato et al. (2012) [19] and this study), but Sato et al. (2012) [19] did not screen for all SHANK1 exons in the controls. Therefore these controls were not included here.
The two SHANK3 deletions reported by Glessner et al. (2009) [34] in control subjects have not been validated and should be interpreted with caution. The frequencies of SHANK mutations have been calculated including only unrelated cases and controls. FEM, Fixed Effects Model; REM, Random Effects Model. After Bonferroni correction for 12 tests (significant threshold corrected α-value = 0.0042), only the SHANK3 copy-number variant association remains significant. The power achieved to observe the statistical difference between patients and controls for SHANK1 and SHANK2 damaging missense variants was 69% and 59%.
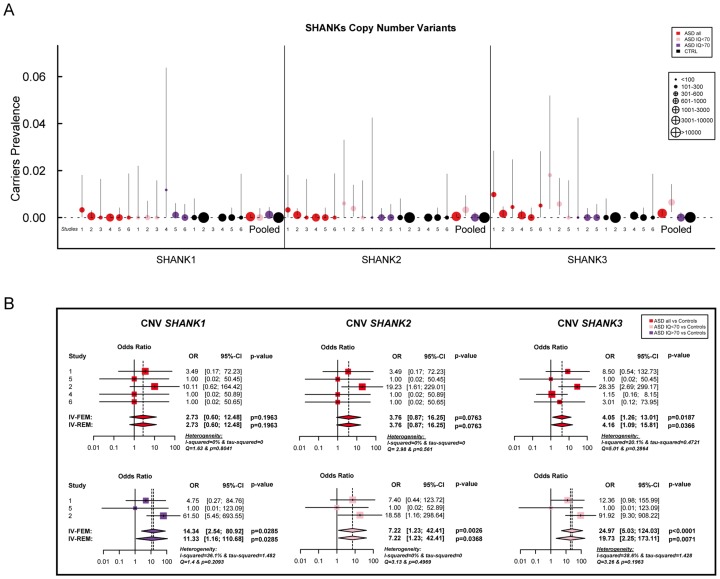
Figure 2. Prevalence and meta-analysis of copy number variant studies in ASD.
A. The prevalence and the confidence interval from a set of single copy number variant studies and the pooled prevalence and the confidence interval of the meta-analysis. The prevalence is indicated by circles in red, pink, purple and black for “ASD all” (all ASD patients), “ASD IQ<70” (patients with ID; IQ<70), “ASD IQ>70” (patients with IQ in the normal range), and “CTRL” (controls), respectively. The plotted circles are proportional to the corresponding sample size. B. Meta-analysis of the copy number variants altering SHANK genes. For each study, the Odds ratio and confidence interval are given. Each meta-analysis is calculated using inverse variance method for fixed (IV-FEM) and random effects (IV-REM). The statistics measuring heterogeneity (Q, I2 and Tau2) are indicated. The number under the scatter plot correspond to independent studies: 1 = “[The Paris cohort: this study+Durand et al. 2007 [6]; Sato et al. 2012 [19]; Leblond et al. 2012 [18]]”, 2 = “[Moessner et al. (2007) [13]; Marshall et al. (2008) [52]; Pinto et al. (2010) [8]; Berkel et al. (2010) [14]; Sato et al. (2012) [19]]”, 3 = “Bremer et al. (2010) [53]”, 4 = “Glessner et al. (2009) [34]”, 5 = “Sanders et al. (2011) [9]”, and 6 = “Sebat et al. (2007) [51]”. IV, Inverse Variance; FEM, Fixed Effect Method; REM, Random Effect Method; OR, Odds Ratio; CI, Confidence Interval; IQ, Intellectual Quotient; CNV, Copy Number Variant.
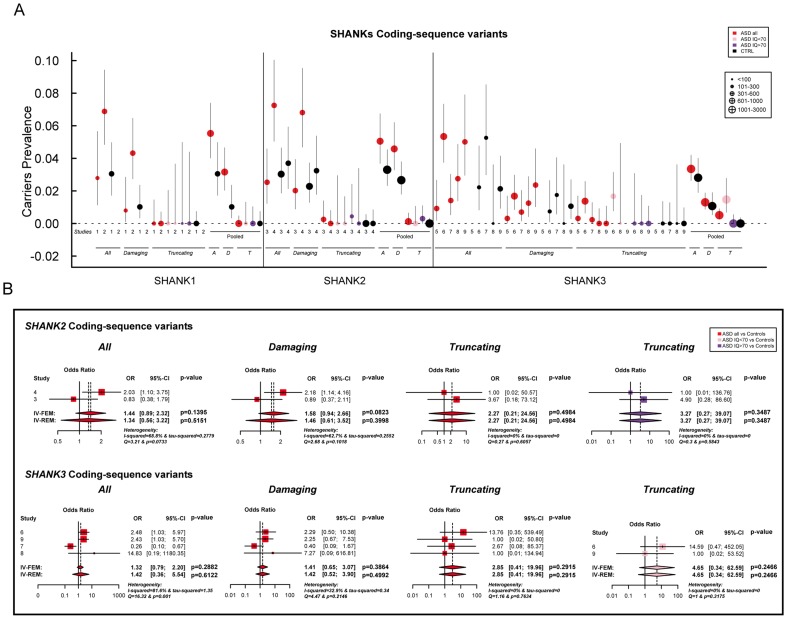
Figure 3. Prevalence and meta-analysis of coding-sequence variant studies in ASD.
A. The prevalence and the confidence interval from a set of single coding-sequence variant studies, and the pooled prevalence and the confidence interval of the meta-analysis. The prevalence is indicated by circles in red, pink, purple and black for “ASD all” (all ASD patients), “ASD IQ<70” (patients with ID; IQ<70), “ASD IQ>70” (patients with normal IQ), and “CTRL” (controls), respectively. Three categories are used to study the prevalence of coding-sequence variants in ASD and controls: all or “A” (all mutation), Damaging or “D” (damaging missense mutation; score obtained from polyphen-2), and Truncating or “T” (mutation altering SHANK protein). The plotted circles are proportional to the corresponding sample size. B. Meta-analysis of coding-sequence variant studies altering SHANK genes. For each study, the Odds ratio and confidence interval is given. Each meta-analysis is calculated using inverse variance method for fixed (IV-FEM) and random effects (IV-REM). The statistics measuring heterogeneity (Q, I2 and Tau2) are indicated. The number under the scatter plot correspond to independent studies: 1 = “This study”, 2 = “ Sato et al. (2012) [19]”, 3 = “Berkel et al. (2010) [14]”, 4 = “Leblond et al. (2012) [18]”, 5 = “Boccuto et al. (2012) [17]”, and 6 = “[This Study and Durand et al. 2007 [6]]”, 7 = “[Gauthier et al. (2009–2010) [16], [47]]”, 8 = “Moessner et al. (2007) [13]”, 9 = “Schaff et al. (2011) [35]”. IV, Inverse Variance; FEM, Fixed Effect Method; REM, Random Effect Method; OR, Odds Ratio; CI, Confidence Interval; IQ, Intellectual Quotient; CNV, Copy Number Variant.
Table 2. Clinical characteristics of the patients carrying de novo SHANK2 and SHANK3 mutations.
| Patients | ||||||
| SHANK2 | SK0217-003 | 6319_3 | AU038_3 | RDB_30769 | AUL_001 | Wischmeijer et al. 2010 |
| Pinto et al. 2010 | Pinto et al. 2010 | Leblond et al. 2012 | This study | This study | Wischmeijer et al. 2010 | |
| Sex | M | M | M | M | M | F |
| Mutation | CNV_del (66 kb) | CNV_del (68 kb) | CNV_del (421 kb) | CNV_del (1.8 Mb) | Translocation | CNV_del (3.4 Mb) |
| Loss of exon 6 & 7 | Loss of exon 14 & 15 | Loss of exon 5 to 16 | del_11q13.3q13.4 (all SHANK2 exons) | t(1;7;11)(p35;q33;q12)dn; breakpoint in SHANK2 (intron 14) | del_11q13.2q13.4 (all SHANK2 exons) | |
| De novo | De novo | De novo | De novo | De novo | De novo | |
| Diagnosis and cognitive development | Autism | Autism | Autism | Autism | Autism | Autism |
| Early DD (mild motor & language delay) | Early DD (mild motor & language delay) | Early DD (mild motor & language delay) | Global DD | Global DD | Global DD | |
| Mild ID/verbal | Mild ID/verbal | Mild ID/verbal | Severe ID/non verbal | Severe ID/non verbal | Severe ID/non verbal | |
| Neonatal hypotonia | Neonatal hypotonia | Neonatal hypotonia | ||||
| Dismorphic signs | Clinodactyly (5th fingers) | Large ears | Clinodactyly (5th fingers) | Clinodactyly (5th fingers) | Clinodactyly (5th fingers) | Deep-set eyes & epicanthus |
| Large ears | Pointed chin | Deep-set eyes | Deep-set eyes | Deep-set eyes & epicanthus | Long eyelashes & ptosis | |
| Long eyelashes | Wide nasal bridge | Large ears | Strabismus & ptosis | Large ears | Wide nasal bridge | |
| Wide nasal bridge | Retrognathia | Pointed chin | Large ears | Wide nasal bridge | Thin upper lip | |
| Retrognathia | Retrognathia | Long eyelashes | Retrognathia | |||
| Wide nasal bridge | Wide nasal bridge | Retrognathia | Clinodactyly (5th fingers) & syndactylia (2nd–3rd) | |||
| Thin upper lip | Thin upper lip | |||||
| Motor signs | Oral dyspraxia | Oral dyspraxia | Oral dyspraxia | Oral dyspraxia | ||
| Slight hypotonia | Slight hypotonia | Slight hypotonia | Slight hypotonia | |||
| Signs of cerebellar dysfunction (dysmetry & dysdiadochokinesis) | Signs of cerebellar dysfunction (dysmetry & dysdiadochokinesis) | Signs of cerebellar dysfunction (dysmetry & dysdiadochokinesis) | ||||
Mutations not present in the mother and father not tested (DNA unavailable). M, Male; F, Female; CNV, Copy Number Variant; del, deletion; CSV, Coding-Sequence Variant; DD, developmental delay; ID, intellectual disability; GTCS, Generalized Tonic-Clonic Seizures; AAO, Age at onset; y, years; SD, Standard Deviation.
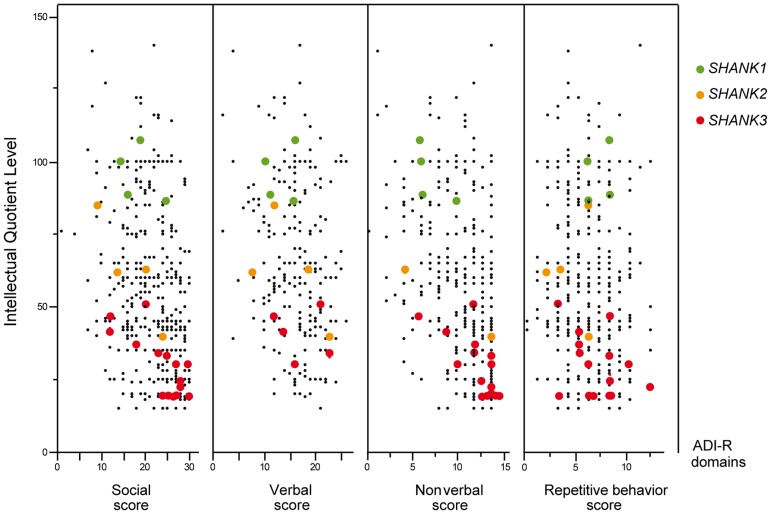
Figure 4. Scatter plots of the intellectual quotient and the Autism Diagnostic Interview-Revised (ADI-R) scores of the patients with ASD screened for SHANK1-3 mutations.
Mutations in SHANK1-3 are associated with a gradient of severity in cognitive impairment. SHANK1 mutations were reported in patients without ID (green dots). SHANK2 mutations were reported in patients with mild ID (orange dots). SHANK3 mutations were found in patients with moderate to severe deficit (red dots). Black dots correspond to the patients enrolled in the PARIS cohort screened for deleterious SHANK1-3 mutations (n = 498). In addition to the PARIS cohort [6], [8], [18], three patients with a SHANK1 deletion [19] and two patients with a SHANK2 deletion [14] were included in the scatter plot. A high score of the ADI-R is associated with a more severe profile. The threshold of the “Social”, “Verbal”, “Non-Verbal” and “Repetitive Behavior” Scores are 10, 8, 7 and 3, respectively.
SHANK1 in ASD
Altogether, our new screening of 306 patients with ASD and 454 controls and the previously published copy-number variants studies (Table S3 & S5) showed that deletions disrupting SHANK1 were detected in 0.04% (n = 2/5 657) of patients with ASD and were never found in 19 163 controls (Meta-analysis – Inverse variance method - fixed effect model P = 0.19, OR = 2.73, 95% CI = 0.60–12.48) (Table 1 and Figure 2). The two independent families with SHANK1 deletions were reported by Sato et al. (2012) [19]. A de novo deletion of 63.4 kb altering both the synaptotagmin-3 gene (SYT3) and SHANK1 was detected in a Swedish male with normal IQ and ASD [19]. An inherited exonic deletion of 63.8 kb altering both SHANK1 and CLEC11A segregated in a four-generation Canadian family in which male carriers—but not female carriers—have ASD [19]. No SHANK1 duplications were found.
We screened a sample of 251 patients and 492 controls for SHANK1 coding exons. As for the SHANK1 mutation screening by Sato et al. (2012), no de novo truncating mutation sequences were identified. Based on the two cohorts of 760 patients with ASD and 492 controls (Table 1, Figure 1 & 3, Tables S4, S5, S6, S7 & S9), rare inherited coding-sequence variants predicted as damaging were, however, more frequent in patients with ASD than in controls (3.16% in ASD, 1.02% in controls, Fisher's exact test two-sided, P = 0.012, OR = 3.17, 95% CI = 1.18–10.72). The rare variants observed in patients with ASD were not observed in an additional sample of 500 control chromosomes.
The 4 males with SHANK1 deletions were diagnosed with ASD and an IQ in the normal range (mean IQ = 107) and good verbal ability without significant language delay [19] (Figure 4). Interestingly, sex differences might modulate the phenotype since females carrying an inherited SHANK1 deletion exhibited anxiety and shyness, but did not fulfill criteria for ASD [19].
SHANK2 in ASD
SHANK2 deletions were found in 0.05% (n = 3/5 657) of patients with ASD, and never in controls (n = 0/19 163; Meta-analysis – Inverse variance method - fixed effect model, P = 0.076, OR = 3.76, 95% CI = 0.87–16.25) (Table 1, S3 & S5, and Figure 2). All deletions were de novo and disrupted coding exons. No SHANK2 duplications were reported. We identified two patients with a SHANK2 de novo deletion (Table 2). For patient AUL_001, the breakpoints were previously sequenced using whole genome sequencing [31] (Table 2, Figure S4 and Text S1). The second patient (RDB_30769) carried a de novo deletion of 1.8 Mb encompassing SHANK2. These two patients were not included in the calculation of the prevalence since they were not part of our cohort screened for copy-number variants. They were identified during clinical screening and the exact number of patients with ASD investigated was not available.
Based on the mutation screening of Berkel et al. (2010) and Leblond et al. (2012), the prevalence of truncating SHANK2 coding-sequence variants was 0.12% in patients with ASD (n = 1/851), and such variants were not found in any of the 1 090 controls (Figure 1 and 3, Table 1, Table S4, S5, S6, S7 & S10). This prevalence is similar to the one reported in the four large-scale studies in ASD using exome sequencing [32] (de novo or truncating SHANK2 mutation 1/965, 0.10%). Finally, we observed rare coding-sequence variants predicted as damaging in 4.58% of the patients with ASD compared with 2.66% of the controls (Fisher's exact test two-sided, P = 0.025, OR = 1.76, 95% CI = 1.05–2.97).
The individuals carrying a SHANK2 de novo deletion were diagnosed with autistic disorder or pervasive developmental disorder not otherwise specified (PDD-NOS) in combination with mild to moderate ID (mean IQ = 62±17) (Figure 4). They displayed early signs of developmental delay, mild motor delay and significant language delay. They also displayed minor signs of dysmorphism (broad nasal bridge, thin upper lip, pointed chin, clinodactyly) and abnormal neurological examination (Table 2). Specifically, cases 6319-3 and AU038-3 had mild axial hypotonia, oral dyspraxia and minor signs or cerebellar dysfunction (including dysmetry and dysdiadochokinesis). These clinical signs are unspecific, but were also reported in patients with ASD with more complex chromosomal rearrangements encompassing SHANK2 [33]. The individual carrying the de novo truncating mutation R841X (SK 0441-003) had a normal IQ and diagnosed with ASD without any developmental delays or dysmorphic features.
SHANK3 in ASD
In our screening of 306 patients with ASD, we identified one patient (AU029) carrying a de novo SHANK3 deletion of 1.5 Mb (Figure S4). Altogether, SHANK3 deletions were detected in 0.18% of patients with ASD (n = 10/5 657) and in 0.01% of controls (n = 2/19 163) (Meta-analysis – Inverse variance method - fixed effect model, P = 0.019, OR = 4.05, 95% CI = 1.26–13.01) (Figure 2, Figure S4, Table 1 and Table S3, S4, S5, S6, S7). Deletions of SHANK3 have not been reported in controls before, so the two deletions reported by Glessner et al. (2009) [34], which have not been validated, should be interpreted with great caution. In three families from France and Canada, the SHANK3 deletions originated from a balanced translocation present in a healthy parent [6], [13]. Interestingly, in two families, a sibling carried the reciprocal SHANK3 duplication. In the French family, the elder brother carrying the SHANK3 duplication was diagnosed with Asperger syndrome [6]. In the Canadian family, the elder sister carrying the SHANK3 duplication was diagnosed with attention-deficit/hyperactivity disorder (ADHD) and developmental delay [13]. In a screen of 160 additional patients with ASD and ID using Multiplex Ligation-dependent Probe Amplification (MLPA) analysis, we observed two patients carrying a de novo deletion altering SHANK3 (Figure S4 and Text S1: Supplementary Methods). For patient AUN_006, the deletion breakpoint is located within intron 8 of SHANK3 and leads to the loss of SHANK3 (exons 9 to 22), ACR and RABL2B. For the second patient AUN_007, the deletion covers the exon 22 of SHANK3 and exons 1 to 3 of ACR.
We screened 429 patients with ASD for all coding exons of SHANK3 and found 8 patients carrying heterozygous truncating mutations (Figure 1 and 3, Figure S5, Table 1, Table S4, S5, S6, S7 and Table S11), including 6 that appeared de novo in the probands. For the remaining two, the mothers were not carriers, but the DNA of the fathers were not available. When all mutation screenings were included, truncating SHANK3 coding-sequence variants were found in 0.51% of the patients (n = 11/2 147) and were not found in 1031 controls (meta-analysis – inverse variance method - fixed effect model, P = 0.29, OR = 2.85, 95% CI = 0.41–19.96) (Table 1, S5 & S11, and Figure 1 & 3) [6], [13], [16], [17], [35]. We observed an enrichment of truncating mutations in exon 21a of SHANK3. We therefore screened an additional sample of 138 cases with ASD for exon 21a and identified a novel de novo stop mutation (Q1243X) in one boy with autism and moderate ID (Table 2 & Figure S5).
Individuals with SHANK3 truncating mutations displayed autism with moderate to severe/profound ID (mean IQ: 31±8) (Figure 4). The individuals carrying SHANK3 deletions had also manifestations of the Phelan-McDermid syndrome [15]. For example, the boy carrying the L1142Vfs*153 mutation was non-verbal, showed a global developmental delay with neonatal hypotonia and typical dysmorphic features of Phelan-McDermid syndrome, including wide nasal bridge, pointed chin, deep-set eyes, flat mid-face, large ears, long eyelashes, bulbous nose, and high-arched palate (Table 2). He also developed generalized epilepsy at the age of 10 years, which was characterized by intolerance and resistance to variety of anticonvulsant medications. By contrast, the boy carrying the de novo truncating mutation S1202Cfs*81 was verbal and had moderate ID. Although reduced in quality by the opposition of the patient, the clinical examination was considered in the normal range with no significant dysmorphic features. Thus, the phenotypic variability of the Phelan-McDermid syndrome, which was considered to result from the wide range of deletion sizes, was also observed for individuals carrying SHANK3 de novo or truncating mutations.
Discussion
Mutations of the SHANK genes were detected in the whole spectrum of ASD with a gradient of severity in cognitive impairment. SHANK1 mutations were detected in individuals with ASD and normal IQ, SHANK2 mutations were found in cases with ASD and mild ID, and SHANK3 mutations were mainly found in individuals with ASD combined with moderate to severe ID. In the whole spectrum of ASD, we estimated that 0.04%, 0.17% and 0.69% of cases with ASD had heterozygous truncating mutations in SHANK1, SHANK2 or SHANK3, respectively (Table 1). Recent exome sequencing studies only reported one de novo SHANK2 mutation out of 965 patients [32], [36], [37] and no truncating coding-sequence variation within SHANK1 and SHANK3. In contrast, we report 0.51% of cases with ASD carrying truncating coding-sequence variations in SHANK3. This difference could be explained by the very low sequencing coverage of SHANK3 using whole-exome sequencing technology leading to a low power of detection of SHANK3 mutations. This coverage issue of SHANK3 was indeed observed by other groups [38]. Interestingly, regions with low coverage of SHANK3 correlate with high percentage of GC; and the majority of the mutations detected in our study were located in the exonic region of SHANK3 showing a very low coverage (Figure S3).
The prevalence of each SHANK mutations appeared to be different when the severity of cognitive impairment was considered (Figure 4, Table 3 and Table S6). This was particularly relevant for SHANK3 in individuals with ASD and ID. The prevalence of de novo or truncating SHANK3 mutations in these patients was 2.12% (copy-number variants: 6/917 patients with IQ<70; prevalence = 0.65%; coding-sequence variants: 9/611 patients with IQ<70; prevalence = 1.47%), 0% in patients with ASD without ID and 0.01% in controls. Our prevalence of SHANK3 deletions in patients with ASD and ID is similar to that reported by Cooper et al. (2011) in a large sample of 1 379 patients with autism and developmental delay (0.87%) [10]. Altogether, in addition to the large deletions observed in Phelan-McDermid syndrome, mutations of SHANK3 account for more than 1 out of 50 cases diagnosed with the combination of ASD and ID. Detection of such mutations should therefore be considered in clinical practice. This clinical screening should: (i) improve the quality of genetic counseling of ASD and ID for patients and their family relatives; (ii) increase our understanding of the clinical features associated with SHANK mutations together with the developmental trajectories of the patients [39], (ii) enable the development of a large number of independent induced pluripotent stem cells (iPSC) carrying SHANK mutations [40], (iii) set the ground for future large scale clinical trials targeting these synaptic defects [41].
Table 3. Summary of the SHANK protein functions and of the main findings obtained for patients with ASD.
| SHANK1 | SHANK2 | SHANK3 | ||
| DNA | chromosome | 19q13.3 | 11q13.3 | 22q13.3 |
| damaging mutations in Controls | 1.02% | 2.66% | 1.07% | |
| truncating mutations in Controls | 0% | 0% | 0% | |
| RNA & Proteins | mRNA localization in neurons | soma and dendrites (hippocampal & Purkinje cells) | soma and dendrites (Purkinje cells) | soma and dendrites (hippocampal neurons) |
| expression pattern | high in cortex | broad in brain (cerebellar Purkinje cells) | high in striatum (cerebellar granule cells) | |
| Synapses | localization | glutamatergic synapses | glutamatergic synapses | glutamatergic synapses |
| expression dynamics | 3rd Shank at the synapse | 1st Shank at the synapse | 2nd Shank at the synapse | |
| effect loss | decrease in GKAP & Homer | increase in NMDAR NR1 | decrease in NMDAR NR1 and AMPAR | |
| zinc dependence | independent | dependent | dependent | |
| Spines | effect of loss | decreased size of spine heads | decreased number of mature spines | decreased number of mature spines |
| effect of gain | increased number of mature spines | increased number of mature spines | ||
| effect of mutation in ASD | reduction of synaptic density affect spine induction & morphology | reduction of synaptic density affect spine induction & morphology | ||
| Synaptic currents | effect of loss | normal NMDA and AMPA | increase/decrease NMDA* | decrease NMDA and AMPA |
| Mouse behavior | social interactions | reduced | reduced | reduced |
| vocal behaviors | abnormal | abnormal | abnormal | |
| activity | reduced | increased | reduced | |
| stereotypies | increased | increased | ||
| learning | enhanced (but reduced memory) | reduced | reduced | |
| Truncating mutations | ASD | 0.04% | 0.17% | 0.69% |
| ASD (IQ>70) | 0.12% | 0.30% | 0% | |
| ASD (IQ≤70) | 0% | 0.33% | 2.12% | |
| IQ | ASD | 95±11 | 62±17 | 30±8 |
| Penetrance | males | high | high | high |
| females | incomplete | not reported | high |
The frequency of mutation in patients and control individuals was calculated from the total cohort (Table 1). The frequency of mutation in patients with normal IQ (IQ>70) and low IQ (IQ<70) were calculated for the patients with available IQ scores (copy-number variants for all SHANK: nASD with IQ>70 = 1 638 & nASD with IQ<70 = 917; SHANK1 coding-sequence variants: nASD with IQ>70 = 354 and nASD with IQ<70 = 278; SHANK2 coding-sequence variants: nASD with IQ>70 = 335 & nASD with IQ<70 = 344; SHANK3 coding-sequence variants: nASD with IQ>70 = 667 & nASD with IQ<70 = 611). The mean IQ and standard deviation was given only for patients carrying truncating or de novo mutations. The black star indicates that Schmeisser et al. (2012) [21] found an increase in NMDA currents, while Won et al. (2012) [22] found a decrease in NMDA currents in two independent SHANK2 knock-out mice.
Contrary to the de novo SHANK mutations, the role of the inherited sequence variants remains difficult to ascertain. Our study provides some insights regarding this issue. There is a trend for more SHANK1 (unadjusted P = 0.012) and SHANK2 (unadjusted P = 0.025) inherited deleterious mutations in patients with ASD than in controls (Table 1). However, these associations do not survive Bonferroni correction for multiple testing. Despite our meta-analysis that includes several mutations screening, we were underpowered to detect associations with low effect size (Table S12). The power to detect an odds ratio of 1.5 (two-sided) for SHANK1, SHANK2 and SHANK3 missense inherited damaging variants were 8%, 34% and 17%, respectively. Further studies with larger cohorts of patients stratified by IQ are therefore needed to achieve appropriate statistical power. Interestingly, in-frame deletions predicted to remove several amino acids in the SHANK2 and SHANK3 proteins were only detected in patients with ASD and their parents, never in controls. Previous functional studies have shown that inherited variants are associated with a statistically significant reduction in the density of synapses, although not as severe as the reduction caused by the de novo or truncating mutations [6], [18], [42]–[44]. Together, these genetic and functional data suggest that, although present in healthy parents, some inherited SHANK mutations might contribute to the development of ASD.
To date, only non-synonymous mutations in the known exons of the SHANK genes had been reported. However, all SHANK genes display several splicing isoforms and possibly some exons were not screened. In addition, other types of mutations such as synonymous mutations or variations in regulatory regions were rarely reported. In our cohort, we did not find synonymous mutations located at alternative splicing sites, but it is warranted that these variations should be reported in future screening.
It has been proposed that abnormal SHANK levels at the synapse might result in the mislocalization, de-clustering and/or functional impairment of several other crucial synaptic proteins such as cytoskeletal regulators and/or neurotransmitter receptors [12] (Table 3).
For SHANK1 mutations, it is expected that the number of dendrites and glutamatergic synapses will not be dramatically affected (if at all). SHANK1 mutations might rather lead to an immature neuronal network with a reduced number of large spine heads. Accordingly, male individuals carrying SHANK1 deletions do not present with language delay or ID and are diagnosed with normal IQ ASD or Asperger syndrome [19]. Interestingly, females who are carrier of a SHANK1 deletion seem to be protected against ASD suggesting that X-linked genes escaping the X-inactivation process and/or hormonal factors could buffer this type of synaptic alterations.
For SHANK2 and SHANK3 mutations, it is expected that affected neurons will have a reduced total number of dendritic spines and synapses. The reduction in mature glutamatergic synapses is expected to affect cognitive functions. Accordingly, most patients with SHANK2 and SHANK3 mutations have moderate to severe ID. Individuals with SHANK3 mutations are usually more severely affected than those carrying SHANK2 mutations. This difference in severity of cognitive impairment is in agreement with the observation that SHANK3 mutations are highly penetrant (to our knowledge only one validated SHANK3 deletion has been reported to be inherited from a mother with moderate ID [45]), while for SHANK2, additional genetic/epigenetic factors might be necessary to develop ASD [18], [19], [46].
In summary, our genetic and clinical findings provide additional support for considering SHANK mutations in a broad spectrum of patients with ASD. SHANK mutations are however not restricted to ASD. SHANK3 mutations have been identified in patients suffering from schizophrenia and bipolar disorder [45], [47]. More generally, other genes involved in the same synaptic pathway, including neurexin and neuroligin genes, appear to be associated with a variety of neuropsychiatric disorders [11]. Given the broad spectrum of disorders associated with this synaptic pathway, it is important to conduct fine-grained clinical investigations of patients in order to identify the factors that influence the clinical trajectory, clinical manifestations, and outcome of affected individuals [41].
Materials and Methods
Study samples for SHANK mutations in ASD
Mutation screening of the SHANK genes was performed in patients with ASD recruited by the PARIS (Paris Autism Research International Sibpair) study at specialized clinical neuropsychiatric centers located in France and Sweden (Table S2, S3, S4). Ethnicity of the patients and controls was ascertained using genetic data (Figure S6 and Text S1). The autism-spectrum diagnosis was based on the Autism Diagnostic Interview – Revised (ADI-R) [48] and for some of the patients, the Autism Diagnostic Observation Schedule (ADOS) [49]. In Sweden, in few cases, the Diagnostic Interview for Social and Communication Disorders (DISCO-10) [50] was used instead of the ADI-R. IQ was measured with an age-appropriate Weschler scale (WPPSI, Wechsler Preschool and Primary Scale of Intelligence; WISC, Wechsler Intelligence Scale for Children; or WASI, Wechsler Abbreviated Scale of Intelligence). For the most severe and/or non-verbal patients, the Raven's Standard Progressive Matrices were used to measure nonverbal IQ (NVIQ) and the Peabody Picture Vocabulary Test (PPVT-4th edition) to measured receptive vocabulary (RV). In addition, a physical exam was systematically performed to record specifically basic physical parameters (such as height, weight, cranial circumference), dysmorphic features and neurological symptoms. The patients used for the scatter plots of the intellectual quotient and the ADI-R scores, or for the clinical characteristics, or for the prevalence, are indicated in the Table S7.
Ethics statement
This study was approved by the local Institutional Review Board (IRB) and written informed consents were obtained from all participants of the study. For the patients who were unable to consent for themselves, a parent or legal guardian consented to the study on their behalf. The local IRB are the “Comité de Protection des Personnes” (Île-de-France Hôpital Pitié-Salpêtrière Paris, France); the “Comité de Protection des Personnes Sud Méditerrannée III” (centre hospitalier universitaire de Nîmes, France); the Sahlgrenska Academy Ethics committee (University of Gothenburg, Sweden); SickKids Research Ethics Board (Toronto, Ontario, Canada); Hamilton Integrated Research Ethic Board (HIREB) (Hamilton, Ontario, Canada) and Health Research Ethics Authority (HREA) (St. John's, Newfoundland, Canada).
SHANK copy-number and coding-sequence variants in ASD
SHANK copy-number variants were detected with the Illumina Human 1M-Duo BeadChip, and validated by quantitative PCR as previously described [8], [18]. For SHANK1 and SHANK2, the sequencing protocol was adapted from Leblond et al. (2012) [18] and Sato et al. (2012) [19] (Table S8). For SHANK3, because of its high GC content and the genomic sequence errors, several clinical and research centers could not screen exon 11 for mutations [13], [16]. We have now corrected the genomic sequence (Figure S2 and Text S1) and provided a new set of primers that successfully amplified and sequenced all SHANK3 exons. All SHANK primers and sequencing protocols are provided in Table S8.
To ascertain the frequency of SHANK mutations in ASD, we included all studies published before April 2012 reporting whole genome copy-number variant screening or SHANK mutation screening. We scanned the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed) with combinations of the following keywords: “Autis*”, “mutation*” “Shank*”, Prosap*, “copy number variants”. For SHANK copy-number variants, a total of 5 657 cases and 19 163 controls were included, representing 11 studies including this one (Table S3) [8], [9], [13], [14], [18], [19], [34], [35], [51]–[53]. In order to avoid biasing the estimation of the frequency of the copy-number variants, we only included studies that analyzed large numbers of individuals (>200 individuals) and used similar mutation screening procedures (for details see Table S3 and Text S1). To ensure that the cohorts were constituted of independent and unrelated cases and controls, we contacted the corresponding authors of each study. For example, the cohorts used in the following studies: Pinto et al. (2010), Moessner et al. (2007), Marshall et al. (2008), Berkel et al. (2010), and Sato et al. (2012) contained overlapping samples. The number of non-overlapping samples from these five studies was 1 866 patients with ASD and 15 122 controls, and the total number of non-overlapping samples used in the meta-analysis was 5 657 patients with ASD and 19 163 controls. For patients with ASD, only copy-number variants validated by an independent method were included in the analysis. For controls, the two SHANK3 deletions reported by Glessner et al. (2009) among 2 519 individuals, were not validated and thus should be regarded with caution.
For SHANK coding-sequence variants, 10 studies including this one were used (Table S4) [13], [14], [16]–[19], [35], [47]. For all variants, the hg19 coordinates are given. Because of the very low coverage of whole exome sequencing (Figure S3 and Text S1), we excluded mutation screening performed using this approach. Taken together, a total of 760–2 147 patients and 492–1 090 controls were included in the analysis (SHANK1: 760 patients and 492 controls; SHANK2: 851 patients and 1 090 controls; SHANK3: 2 147 patients and 1 031 controls).
Statistics
The significance of observed differences in copy-number and coding-sequence variants was determined by a two-sided Fisher's exact test on a two-by-two contingency table. We used Bonferroni correction for the multiple testing correction (ntest = 12, significant threshold corrected α-value = 0.05/12 = 0.0042). We used G*Power (v3.1, http://www.psycho.uniduesseldorf.de/abteilungen/aap/gpower3) to compute for each test the achieved statistical power (for a two-sided Fisher's exact test) and the power to detect an odd ratio from 1.5 to 3 (two-sided) (Table S12). Prevalence and confidence intervals of single studies were evaluated using Clopper and Pearson method [54]. Heterogeneity between studies was assessed by the Q, I2 and Tau2 statistics. The Q statistic is a chi-square test for heterogeneity, and the I2 and Tau2 are the proportion of observed variance in effect sizes across studies for fixed effect model and random effect model, respectively [55]. Zero total event studies (no events in both ASD and controls) were included [56]. The meta-analysis was performed using the classical inverse variance for both fixed effects model and random effects model. To avoid population stratification bias in the calculation of the odds ratio (OR), studies without a control group were excluded (i.e. Boccuto et al. 2012 and Bremer et al. 2012) (Figure 2, 3, and Table 1). If any contingency tables contained zero values, a continuity correction was applied to the relevant tables [57]. For all the calculations and illustrations the R statistical software, and “metafor” and “meta” packages were used.
Supporting Information
Genomic structure and phylogeny of SHANK family. A. Genomic structure of human SHANK genes. Conserved domains of protein interaction are represented in color: ANK (red), SH3 (orange), PDZ (blue) and SAM (green). Black stars identify the alternative spliced exons and turquoise stars the alternative spliced exons specifically retained in the human brain. Grey bars indicate CpGs islands and the arrows the different isoforms. The areas of the human genome with missing sequence are indicated by purple rectangles. B. Phylogenetic tree of SHANK proteins. SHANK1 was blasted with non-redundant protein sequence database and the tree was produced using the Neighbor joining method with a maximum of sequence difference = 0.85 and the Grishin Distance.
(TIF)
Genome errors covering SHANK3. A. Representation of the reference sequence and mRNA of SHANK3 in hg19 (http://genome.ucsc.edu/). Before the update of hg19 in March 2012, SHANK3 was supported by NM_001080420.1 carrying annotation and sequence errors. The false exon 11 was corrected in March 2012, but the real exon 11 still contained a wrong sequence with a gap. Using a combination of PCR and BLAST experiments, we corrected this sequence gb_JX122810. B. The clustalW2 alignment (http://www.ebi.ac.uk/Tools/msa/clustalw2/) shows the gap still present in hg19 and located in the 5′UTR and coding region of the exon 11 of SHANK3. JX122810 is the GenBank (http://www.ncbi.nlm.nih.gov/genbank/) accession number of the validated intron flanking and exon 11 sequences of NM_033517. E11, Exon 11; E12, Exon 12; gb, GenBank; hg, human genome; EST, Expressed Sequence Tag.
(TIF)
Read depth for SHANK genes using whole genome or exome sequencing. The average read depth of whole genome sequence from Complete Genomics (n = 54) and whole exome sequence from NHLBI GO Exome Sequencing Project – Exome Variant server (n = 3 510) are indicated in black and gray, respectively. The Y axis shows the average read number per nucleotide. On the X axis, the nucleotide positions are according to NM_016148 (SHANK1), NM_012309 (SHANK2), and NM_033517 (SHANK3) from NCBI37/hg19. The percentage of GC is calculated from sequences with size equal to 5 nucleotides. The arrows show the direction of the transcription. Truncating, deleterious and neutral coding-sequence variants are indicated in red, orange and green, respectively. Coding-sequence variants identified in ASD only, or in controls only, or in both ASD and controls are indicated by a star, a square or a circle, respectively. Avg, Average; ME, Multi-Ethnic; EA, European American; EVS, Exome Variant Server; CG, Complete Genomics.
(TIF)
Characterization of the de novo deletions of SHANK2 and SHANK3 identified in this study. A. A de novo deletion of 1.8 Mb including SHANK2 was identified in a patient with ASD (RDB_30769) using the HumanCytoSNP-12 Illumina array. FISH studies using the “RP11-102B19” probe covering SHANK2 showed one normal chromosome 11 with one green spot on 11q13, and the second chromosome 11 without the green signal. The parent's metaphase karyotype shows a green spot on both chromosomes 11. White arrows indicate the localization of the SHANK2 probe on chromosome 11. B. A de novo deletion of 1.5 Mb was identified in a patient with ASD (AU029) using the Illumina Human 1M-Duo SNP array. The results of the SNP arrays are represented using SnipPeep (CNV viewer; http://snippeep.sourceforge.net/). Each dot shows Log R Ratio (LRR; in red) and B allele frequency (BAF; in green). QuantiSNP (CNV calling algorithm; CN = Copy Number) score is represented with a blue line and indicates the deletion size. C. Two de novo deletions altering SHANK3 were identified in two independent patients (AUN_006 & AUN_007) with ASD and ID using Multiplex Ligation-dependent Probe Amplification (MLPA) (probemix P188-B2, P343-C1& P339-A1 - MRC-Holland). The first patient AUN_006 carried a deletion including SHANK3 (exons 9 to 22), ACR and RABL2B with a breakpoint in intron 8 of SHANK3. The second patient AUN_007 carried a deletion of SHANK3 (exons 22 only) and ACR (exons 1 to 3). The parents of AUN_006 and AUN_007 probands were negative for SHANK3 CNV (FISH and MLPA analysis not shown). ASD, Autism Spectrum Disorder; ID, Intellectual Disability; FISH, Fluorescent In Situ Hybridization.
(TIF)
Pedigrees of the families carrying de novo/truncating SHANK3 mutations. The chromatograms obtained after Sanger sequencing show eight new truncating mutations altering SHANK3 detected in patients with ASD. When the DNA of the both parents was available (7 out of 9 families), all the mutations were found to be de novo. The arrows indicate the frame-shift. The patient carrying the Q1243X was found during our screening of exon 21 in 138 individuals with ASD.
(TIF)
MDS-Plot: Genetic ancestry of patients with ASD and controls. The multidimensional scaling (MDS) plot pictures the genetic distance between individuals. The density of the genetic ancestry of the HapMap populations (European, Asian, African, Mexican and Indian) allows confirming the European ancestry of the majority of the individuals from PARIS and SUVIMAX cohorts (n = 430 ASD and n = 837 controls). Patients and controls with no SHANK mutation are represented by blue crosses and blue circles, respectively. Patients and controls with SHANK mutations are indicated in red and in green, respectively. SHANK3 mutations are identified by diamonds, SHANK2 by triangles and SHANK1 by squares. Diamonds, triangles or squares are empty when the mutation is a missense and full when the mutation is truncating (CVS or CNV). CVS, Coding-sequence variant; CNV, Copy-number variant.
(TIF)
Genomic sequence covering exons 8 and 9 of human SHANK2 and exon 11 of human SHANK3. The exonic and intronic sequences are indicated in blue upper case and in black lower case, respectively. The primers used for the amplification of each exon are indicated by the black boxes. The alternative stop in exon 21b of SHANK3 is underlined.
(DOC)
Description of the cohort PARIS used for the screening of SHANK copy-number variants and coding-sequence variants. PARIS, Paris Autism Research International Sibpair; IQ, Intelligence Quotient.
(DOC)
Description of the cohorts used for the analysis of SHANK copy-number variants. a,b Indicate the publications with overlap in the cohorts. * The total number of independent cases or controls is not the addition of the cohorts from each study due to the redundancy of the cases and controls tested from these publications. The independent numbers were obtained in collaboration with the authors of the corresponding publications (see Material & Method in supplementary Appendix). The parental DNA of controls was not available. PARIS, Paris Autism Research International Sibpair study; SSC, Simons Simplex Collection; AGP, Autism Genome Project; ACC, Autism Case Control; SAGE, Study of Addiction: Genetics and Environment; CHOP, Children's Hospital of Philadelphia; WTCCC2, Wellcome Trust Case Control Consortium; AGRE, Autism Genetic Resource exchange; NIMH, National Institute of Mental Health; SNP, Single Nucleotide Polymorphism; CEU, Utah residents with Northern and Western European ancestry from the CEPH collection; BAC, Bacterial Artificial Chromosome; CGH, Comparative Genomic Hybridization; ROMA, Representational Oligonucleotide Microarray Analysis; ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision; DISCO, Diagnostic Interview for Social and Communication Disorders; IQ, Intellectual Quotient; RPM, Raven's Progressive Matrices; PPVT, Peabody Picture Vocabulary Test.
(DOC)
Description of the cohorts used for the analysis of SHANK coding-sequence variants. a In this study, controls were tested using allelic discrimination by TaqMan technology and only for the variations identified in ASD. The parental DNA of controls was not available. SUVIMAX, Supplémentation en Vitamines et Minéraux Antioxydants; ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision; DISCO, Diagnostic Interview for Social and Communication Disorders; IQ, Intellectual Quotient; RPM, Raven's Progressive Matrices; PPVT, Peabody Picture Vocabulary Test; SSC, Simons Simplex Collection.
(DOC)
Prevalence of SHANK CNVs and coding-sequence variants in patients with ASD and controls. a Sato et al. (2012), Durand et al. (2007) Leblond et al. (2012) contained overlapping cohorts. For this study, the French and Swedish cases are in Leblond et al (2012) and the Canadian cases are in Sato et al. (2012). bThe controls from Sato et al. 2012 are not included here because they were only tested by Taqman for the variants identified in ASD. cThe two SHANK3 deletions reported by Glessner et al. (2009) in control subjects have not been validated and should be interpreted with caution. CSV, Coding-Sequence Variant; 95CI, 95% Confidence Interval.
(DOC)
Prevalence of SHANK CNVs and coding-sequence variants in ASD patients with or without ID. a Sato et al. (2012) and Leblond et al. (2012) contained overlapping cohorts. For this study, the French and Swedish cases are in Leblond et al (2012) and the Canadian cases are in Sato et al. (2012). b The controls from Sato et al. 2012 are not included here because they were only tested by Taqman for the variants identified in ASD. CSV, Coding-Sequence Variant.
(DOC)
Genetic and clinical features of ASD patients carrying de novo/deleterious SHANK mutations. a Mother showed anxiety and shyness. b Mutations not present in the mother and father not tested (DNA unavailable). c Father had a balanced translocation t(14;22)(p11.2;q13.33). d Mother had a balanced translocation t(14;22)(p11.2;q13.33). e No epilepsy, but abnormal EEG with bilateral epileptiform discharges. f Relatives of proband IV-1. g Case reports not reported in a systematic screening of SHANK2 or whole genome analysis. h Patient detected in an additional mutation screening of SHANK3 exon 21. i Relatives of AU016_3. j Not included in the figure: large deletion involving numerous genes or complex chromosomal rearrangement. k For SHANK3, we only included in figure 2 the patients from the PARIS cohort. l No pictures available. m The phenotypic features were characteristic to the Phelan-Mcdermid syndrome. AS, absence seizures; ASD, autism spectrum disorder; Asp, Asperger syndrome; Aut, autism; CNV, copy number variant, CSV, coding-sequence variants; del, deletion; f, female; ID; inh, inherited; m, male; U, unknown; y, years; GTCS, generalized tonic-clonic seizures.
(DOC)
Primers used for mutation screening of SHANK1 and SHANK3. The red sequences correspond to the M13 adaptor (M13F = TGTAAAACGACGGCCAGT & M13R = GGATAACAATTTCACACAGG). PCR, Polymerase Chain Reaction; TpQ, Tampon Q (from Qiagen); DMSO, Dimethyl sulfoxide.
(DOC)
SHANK1 coding-sequence variants identified in 760 patients with ASD and 492 controls. aNucleotide positions are according to NM_016148 from NCBI37/hg19 on the positive DNA strand (chromosome 19). The patients with ASD used for this analysis came from this study (n = 240) and from the study of Sato et al. (2012) (n = 509). The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling; pph2_class, polyphen-2_class.
(DOC)
SHANK2 coding-sequence variants identified in 851 patients with ASD and 1 090 controls. #Indicates de novo mutations. aNucleotide positions are according to NM_012309.3 from NCBI37/hg19 on the positive DNA strand (chromosome 11). bMaximum Grantham score (215) given for non-sense variants. The patients with ASD and the controls used for this analysis came from Leblond et al. (2012) (455 ASD & 431 controls) and from the study of Berkel et al. (2010) (396 ASD & 659 controls). The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling; pph2_class, polyphen-2_class.
(DOC)
SHANK3 coding-sequence variants identified in 2 147 patients with ASD and 1 031 controls. #Indicates de novo mutations. +Q1243X was identified during an additional screen (nASD = 138) of exon 21 of SHANK3 and was not included in the meta-analysis. aNucleotide positions are according to NM_033517 from NCBI37/hg19 on the positive DNA strand (chromosome 22); bFor the variants with MAF>1%, the frequency was assessed only in PARIS cohort. cAverage GERP score for two sites flanking the insertion or average GERP score for deleted nucleotides; dMaximum Grantham score (215) given for splice, non-sense and frameshifting variants. The patients with ASD and the controls used for this analysis came from this study (n = 429) and from the studies reported in Table S5. The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling, pph2_class, polyphen-2_class.
(DOC)
Statistical power of the association between SHANK damaging missense variants and ASD. *Two-sided Fisher's exact test.
(DOC)
Supplementary method describing the genomic structure of the SHANK genes, coverage of SHANK genes by exome sequencing, cytogenetic analysis and FISH, multiplex ligation-dependent probe amplification (MLPA), genetic ancestry of patients with ASD and controls.
(DOC)
Acknowledgments
We thank the DNA and cell bank of Cochin hospital and of the CRICM, the Plateforme de Ressource Biologique (B. Ghaleh), the Clinical Investigation Centers of Mondor-Chenevier and Robert Debré hospitals for their assistance, and the Psychiatric Genetics team (Stéphane Jamain) of Inserm U955 for collection and management of DNAs. We also thank M. Eriksson, J. Manry and J.P. Hardelin for critical reading of the manuscript, C. Bouchier for the use of sequencing facilities and L. Lemée for the Illumina genotyping arrays at the Institut Pasteur Génopole.
Funding Statement
This work was funded by the Institut Pasteur, CNRS, INSERM, AP-HP, University Paris Diderot, the Bettencourt-Schueller foundation, the Orange foundation, the FondaMental foundation, the Conny-Maeva foundation, the Cognacq-Jay foundation, the ANR (ANR-08-MNPS-037-01 - SynGen), Neuron-ERANET (EUHF-AUTISM), the DFG (BO1718/3-1, 4-1) and Baustein L.SBN.0081. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Geschwind DH (2009) Advances in autism. Annu Rev Med 60: 367–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huguet G, Ey E, Bourgeron T (2013) The Genetic Landscapes of Autism Spectrum Disorders. Annu Rev Genomics Hum Genet 14: 191–213. [DOI] [PubMed] [Google Scholar]
- 3. Betancur C (2011) Etiological heterogeneity in autism spectrum disorders: More than 100 genetic and genomic disorders and still counting. Brain Res 1380: 42–77. [DOI] [PubMed] [Google Scholar]
- 4. Toro R, Konyukh M, Delorme R, Leblond C, Chaste P, et al. (2010) Key role for gene dosage and synaptic homeostasis in autism spectrum disorders. Trends Genet 26: 363–372. [DOI] [PubMed] [Google Scholar]
- 5. Jamain S, Quach H, Betancur C, Rastam M, Colineaux C, et al. (2003) Mutations of the X-linked genes encoding neuroligins NLGN3 and NLGN4 are associated with autism. Nat Genet 34: 27–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Durand CM, Betancur C, Boeckers TM, Bockmann J, Chaste P, et al. (2007) Mutations in the gene encoding the synaptic scaffolding protein SHANK3 are associated with autism spectrum disorders. Nat Genet 39: 25–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Szatmari P, Paterson AD, Zwaigenbaum L, Roberts W, Brian J, et al. (2007) Mapping autism risk loci using genetic linkage and chromosomal rearrangements. Nat Genet 39: 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pinto D, Pagnamenta AT, Klei L, Anney R, Merico D, et al. (2010) Functional impact of global rare copy number variation in autism spectrum disorders. Nature 466: 368–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sanders SJ, Ercan-Sencicek AG, Hus V, Luo R, Murtha MT, et al. (2011) Multiple recurrent de novo CNVs, including duplications of the 7q11.23 Williams syndrome region, are strongly associated with autism. Neuron 70: 863–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cooper GM, Coe BP, Girirajan S, Rosenfeld JA, Vu TH, et al. (2011) A copy number variation morbidity map of developmental delay. Nat Genet 43: 838–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sudhof TC (2008) Neuroligins and neurexins link synaptic function to cognitive disease. Nature 455: 903–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grabrucker AM, Schmeisser MJ, Schoen M, Boeckers TM (2011) Postsynaptic ProSAP/Shank scaffolds in the cross-hair of synaptopathies. Trends Cell Biol 21: 594–603. [DOI] [PubMed] [Google Scholar]
- 13. Moessner R, Marshall CR, Sutcliffe JS, Skaug J, Pinto D, et al. (2007) Contribution of SHANK3 mutations to autism spectrum disorder. Am J Hum Genet 81: 1289–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Berkel S, Marshall CR, Weiss B, Howe J, Roeth R, et al. (2010) Mutations in the SHANK2 synaptic scaffolding gene in autism spectrum disorder and mental retardation. Nat Genet 42: 489–491. [DOI] [PubMed] [Google Scholar]
- 15. Phelan K, McDermid HE (2012) The 22q13.3 Deletion Syndrome (Phelan-McDermid Syndrome). Mol Syndromol 2: 186–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gauthier J, Spiegelman D, Piton A, Lafreniere RG, Laurent S, et al. (2009) Novel de novo SHANK3 mutation in autistic patients. Am J Med Genet B Neuropsychiatr Genet 150B: 421–424. [DOI] [PubMed] [Google Scholar]
- 17. Boccuto L, Lauri M, Sarasua SM, Skinner CD, Buccella D, et al. (2012) Prevalence of SHANK3 variants in patients with different subtypes of autism spectrum disorders. Eur J Hum Genet 3: 310–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Leblond CS, Heinrich J, Delorme R, Proepper C, Betancur C, et al. (2012) Genetic and functional analyses of SHANK2 mutations suggest a multiple hit model of autism spectrum disorders. PLoS Genet 8: e1002521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sato D, Lionel AC, Leblond CS, Prasad A, Pinto D, et al. (2012) SHANK1 Deletions in Males with Autism Spectrum Disorder. Am J Hum Genet 90: 879–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Soorya L, Kolevzon A, Zweifach J, Lim T, Dobry Y, et al. (2013) Prospective investigation of autism and genotype-phenotype correlations in 22q13 deletion syndrome and SHANK3 deficiency. Mol Autism 4: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bonaglia MC, Giorda R, Beri S, De Agostini C, Novara F, et al. (2011) Molecular mechanisms generating and stabilizing terminal 22q13 deletions in 44 subjects with Phelan/McDermid syndrome. PLoS Genet 7: e1002173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Betancur C, Buxbaum JD (2013) SHANK3 haploinsufficiency: a “common” but underdiagnosed highly penetrant monogenic cause of autism spectrum disorders. Mol Autism 4: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jiang YH, Ehlers MD (2013) Modeling autism by SHANK gene mutations in mice. Neuron 78: 8–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hung AY, Futai K, Sala C, Valtschanoff JG, Ryu J, et al. (2008) Smaller dendritic spines, weaker synaptic transmission, but enhanced spatial learning in mice lacking Shank1. J Neurosci 28: 1697–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wohr M, Roullet FI, Hung AY, Sheng M, Crawley JN (2011) Communication impairments in mice lacking Shank1: reduced levels of ultrasonic vocalizations and scent marking behavior. PLoS One 6: e20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schmeisser MJ, Ey E, Wegener S, Bockmann J, Stempel AV, et al. (2012) Autistic-like behaviours and hyperactivity in mice lacking ProSAP1/Shank2. Nature 486: 256–260. [DOI] [PubMed] [Google Scholar]
- 27. Won H, Lee H-R, Gee HY, Mah W, Kim J-I, et al. (2012) Autistic-like social behaviour in Shank2-mutant mice improved by restoring NMDA receptor function. Nature 486: 261–265. [DOI] [PubMed] [Google Scholar]
- 28. Peca J, Feliciano C, Ting JT, Wang W, Wells MF, et al. (2011) Shank3 mutant mice display autistic-like behaviours and striatal dysfunction. Nature 472: 437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yang M, Bozdagi O, Scattoni ML, Woehr M, Roullet FI, et al. (2012) Reduced Excitatory Neurotransmission and Mild Autism-Relevant Phenotypes in Adolescent Shank3 Null Mutant Mice. Journal of Neuroscience 32: 6525–6541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang X, McCoy PA, Rodriguiz RM, Pan Y, Je HS, et al. (2011) Synaptic dysfunction and abnormal behaviors in mice lacking major isoforms of Shank3. Hum Mol Genet 20: 3093–3108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schluth-Bolard C, Labalme A, Cordier MP, Till M, Nadeau G, et al. (2013) Breakpoint mapping by next generation sequencing reveals causative gene disruption in patients carrying apparently balanced chromosome rearrangements with intellectual deficiency and/or congenital malformations. J Med Genet 50: 144–150. [DOI] [PubMed] [Google Scholar]
- 32. Sanders SJ, Murtha MT, Gupta AR, Murdoch JD, Raubeson MJ, et al. (2012) De novo mutations revealed by whole-exome sequencing are strongly associated with autism. Nature 485: 237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wischmeijer A, Magini P, Giorda R, Gnoli M, Ciccone R, et al. (2011) Olfactory Receptor-Related Duplicons Mediate a Microdeletion at 11q13.2q13.4 Associated with a Syndromic Phenotype. Mol Syndromol 1: 176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Glessner JT, Wang K, Cai G, Korvatska O, Kim CE, et al. (2009) Autism genome-wide copy number variation reveals ubiquitin and neuronal genes. Nature 459: 569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schaaf CP, Sabo A, Sakai Y, Crosby J, Muzny D, et al. (2011) Oligogenic heterozygosity in individuals with high-functioning autism spectrum disorders. Hum Mol Genet 20: 3366–3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. O'Roak BJ, Vives L, Girirajan S, Karakoc E, Krumm N, et al. (2012) Sporadic autism exomes reveal a highly interconnected protein network of de novo mutations. Nature 485: 246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Neale BM, Kou Y, Liu L, Ma'ayan A, Samocha KE, et al. (2012) Patterns and rates of exonic de novo mutations in autism spectrum disorders. Nature 485: 242–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Krumm N, O'Roak BJ, Shendure J, Eichler EE (2014) A de novo convergence of autism genetics and molecular neuroscience. Trends Neurosci 37: 95–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Guilmatre A, Huguet G, Delorme R, Bourgeron T (2013) The emerging role of SHANK genes in neuropsychiatric disorders. Dev Neurobiol 74 (2) 113–22. [DOI] [PubMed] [Google Scholar]
- 40. Shcheglovitov A, Shcheglovitova O, Yazawa M, Portmann T, Shu R, et al. (2013) SHANK3 and IGF1 restore synaptic deficits in neurons from 22q13 deletion syndrome patients. Nature 503: 267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Delorme R, Ey E, Toro R, Leboyer M, Gillberg C, et al. (2013) Progress toward treatments for synaptic defects in autism. Nat Med 19: 685–694. [DOI] [PubMed] [Google Scholar]
- 42. Durand CM, Perroy J, Loll F, Perrais D, Fagni L, et al. (2011) SHANK3 mutations identified in autism lead to modification of dendritic spine morphology via an actin-dependent mechanism. Mol Psychiatry 17: 71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arons MH, Thynne CJ, Grabrucker AM, Li D, Schoen M, et al. (2012) Autism-Associated Mutations in ProSAP2/Shank3 Impair Synaptic Transmission and Neurexin-Neuroligin-Mediated Transsynaptic Signaling. J Neurosci 32: 14966–14978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Berkel S, Tang W, Trevino M, Vogt M, Obenhaus HA, et al. (2011) Inherited and de novo SHANK2 variants associated with autism spectrum disorder impair neuronal morphogenesis and physiology. Hum Mol Genet 21: 344–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Denayer A, Van Esch H, de Ravel T, Frijns JP, Van Buggenhout G, et al. (2012) Neuropsychopathology in 7 Patients with the 22q13 Deletion Syndrome: Presence of Bipolar Disorder and Progressive Loss of Skills. Mol Syndromol 3: 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chilian B, Abdollahpour H, Bierhals T, Haltrich I, Fekete G, et al. (2013) Dysfunction of SHANK2 and CHRNA7 in a patient with intellectual disability and language impairment supports genetic epistasis of the two loci. Clin Genet 84 (6) 560–5 doi: 10.1111/cge.12105 [DOI] [PubMed] [Google Scholar]
- 47. Gauthier J, Champagne N, Lafreniere RG, Xiong L, Spiegelman D, et al. (2010) De novo mutations in the gene encoding the synaptic scaffolding protein SHANK3 in patients ascertained for schizophrenia. Proc Natl Acad Sci U S A 107: 7863–7868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lord C, Rutter M, Le Couteur A (1994) Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 24: 659–685. [DOI] [PubMed] [Google Scholar]
- 49. Lord C, Risi S, Lambrecht L, Cook EH Jr, Leventhal BL, et al. (2000) The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 30: 205–223. [PubMed] [Google Scholar]
- 50. Wing L, Leekam SR, Libby SJ, Gould J, Larcombe M (2002) The Diagnostic Interview for Social and Communication Disorders: background, inter-rater reliability and clinical use. J Child Psychol Psychiatry 43: 307–325. [DOI] [PubMed] [Google Scholar]
- 51. Sebat J, Lakshmi B, Malhotra D, Troge J, Lese-Martin C, et al. (2007) Strong association of de novo copy number mutations with autism. Science 316: 445–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Marshall CR, Noor A, Vincent JB, Lionel AC, Feuk L, et al. (2008) Structural variation of chromosomes in autism spectrum disorder. Am J Hum Genet 82: 477–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bremer A, Giacobini M, Nordenskjold M, Brondum-Nielsen K, Mansouri M, et al. (2009) Screening for copy number alterations in loci associated with autism spectrum disorders by two-color multiplex ligation-dependent probe amplification. Am J Med Genet B Neuropsychiatr Genet 153B: 280–285. [DOI] [PubMed] [Google Scholar]
- 54. Clopper CJ, Pearson ES (1934) The Use of Confidence or Fiducial Limits Illustrated in the Case of the Binomial. Biometrika 26: 404–413. [Google Scholar]
- 55. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Friedrich JO, Adhikari NK, Beyene J (2007) Inclusion of zero total event trials in meta-analyses maintains analytic consistency and incorporates all available data. BMC Med Res Methodol 7: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lane PW (2013) Meta-analysis of incidence of rare events. Stat Methods Med Res 22: 117–132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Genomic structure and phylogeny of SHANK family. A. Genomic structure of human SHANK genes. Conserved domains of protein interaction are represented in color: ANK (red), SH3 (orange), PDZ (blue) and SAM (green). Black stars identify the alternative spliced exons and turquoise stars the alternative spliced exons specifically retained in the human brain. Grey bars indicate CpGs islands and the arrows the different isoforms. The areas of the human genome with missing sequence are indicated by purple rectangles. B. Phylogenetic tree of SHANK proteins. SHANK1 was blasted with non-redundant protein sequence database and the tree was produced using the Neighbor joining method with a maximum of sequence difference = 0.85 and the Grishin Distance.
(TIF)
Genome errors covering SHANK3. A. Representation of the reference sequence and mRNA of SHANK3 in hg19 (http://genome.ucsc.edu/). Before the update of hg19 in March 2012, SHANK3 was supported by NM_001080420.1 carrying annotation and sequence errors. The false exon 11 was corrected in March 2012, but the real exon 11 still contained a wrong sequence with a gap. Using a combination of PCR and BLAST experiments, we corrected this sequence gb_JX122810. B. The clustalW2 alignment (http://www.ebi.ac.uk/Tools/msa/clustalw2/) shows the gap still present in hg19 and located in the 5′UTR and coding region of the exon 11 of SHANK3. JX122810 is the GenBank (http://www.ncbi.nlm.nih.gov/genbank/) accession number of the validated intron flanking and exon 11 sequences of NM_033517. E11, Exon 11; E12, Exon 12; gb, GenBank; hg, human genome; EST, Expressed Sequence Tag.
(TIF)
Read depth for SHANK genes using whole genome or exome sequencing. The average read depth of whole genome sequence from Complete Genomics (n = 54) and whole exome sequence from NHLBI GO Exome Sequencing Project – Exome Variant server (n = 3 510) are indicated in black and gray, respectively. The Y axis shows the average read number per nucleotide. On the X axis, the nucleotide positions are according to NM_016148 (SHANK1), NM_012309 (SHANK2), and NM_033517 (SHANK3) from NCBI37/hg19. The percentage of GC is calculated from sequences with size equal to 5 nucleotides. The arrows show the direction of the transcription. Truncating, deleterious and neutral coding-sequence variants are indicated in red, orange and green, respectively. Coding-sequence variants identified in ASD only, or in controls only, or in both ASD and controls are indicated by a star, a square or a circle, respectively. Avg, Average; ME, Multi-Ethnic; EA, European American; EVS, Exome Variant Server; CG, Complete Genomics.
(TIF)
Characterization of the de novo deletions of SHANK2 and SHANK3 identified in this study. A. A de novo deletion of 1.8 Mb including SHANK2 was identified in a patient with ASD (RDB_30769) using the HumanCytoSNP-12 Illumina array. FISH studies using the “RP11-102B19” probe covering SHANK2 showed one normal chromosome 11 with one green spot on 11q13, and the second chromosome 11 without the green signal. The parent's metaphase karyotype shows a green spot on both chromosomes 11. White arrows indicate the localization of the SHANK2 probe on chromosome 11. B. A de novo deletion of 1.5 Mb was identified in a patient with ASD (AU029) using the Illumina Human 1M-Duo SNP array. The results of the SNP arrays are represented using SnipPeep (CNV viewer; http://snippeep.sourceforge.net/). Each dot shows Log R Ratio (LRR; in red) and B allele frequency (BAF; in green). QuantiSNP (CNV calling algorithm; CN = Copy Number) score is represented with a blue line and indicates the deletion size. C. Two de novo deletions altering SHANK3 were identified in two independent patients (AUN_006 & AUN_007) with ASD and ID using Multiplex Ligation-dependent Probe Amplification (MLPA) (probemix P188-B2, P343-C1& P339-A1 - MRC-Holland). The first patient AUN_006 carried a deletion including SHANK3 (exons 9 to 22), ACR and RABL2B with a breakpoint in intron 8 of SHANK3. The second patient AUN_007 carried a deletion of SHANK3 (exons 22 only) and ACR (exons 1 to 3). The parents of AUN_006 and AUN_007 probands were negative for SHANK3 CNV (FISH and MLPA analysis not shown). ASD, Autism Spectrum Disorder; ID, Intellectual Disability; FISH, Fluorescent In Situ Hybridization.
(TIF)
Pedigrees of the families carrying de novo/truncating SHANK3 mutations. The chromatograms obtained after Sanger sequencing show eight new truncating mutations altering SHANK3 detected in patients with ASD. When the DNA of the both parents was available (7 out of 9 families), all the mutations were found to be de novo. The arrows indicate the frame-shift. The patient carrying the Q1243X was found during our screening of exon 21 in 138 individuals with ASD.
(TIF)
MDS-Plot: Genetic ancestry of patients with ASD and controls. The multidimensional scaling (MDS) plot pictures the genetic distance between individuals. The density of the genetic ancestry of the HapMap populations (European, Asian, African, Mexican and Indian) allows confirming the European ancestry of the majority of the individuals from PARIS and SUVIMAX cohorts (n = 430 ASD and n = 837 controls). Patients and controls with no SHANK mutation are represented by blue crosses and blue circles, respectively. Patients and controls with SHANK mutations are indicated in red and in green, respectively. SHANK3 mutations are identified by diamonds, SHANK2 by triangles and SHANK1 by squares. Diamonds, triangles or squares are empty when the mutation is a missense and full when the mutation is truncating (CVS or CNV). CVS, Coding-sequence variant; CNV, Copy-number variant.
(TIF)
Genomic sequence covering exons 8 and 9 of human SHANK2 and exon 11 of human SHANK3. The exonic and intronic sequences are indicated in blue upper case and in black lower case, respectively. The primers used for the amplification of each exon are indicated by the black boxes. The alternative stop in exon 21b of SHANK3 is underlined.
(DOC)
Description of the cohort PARIS used for the screening of SHANK copy-number variants and coding-sequence variants. PARIS, Paris Autism Research International Sibpair; IQ, Intelligence Quotient.
(DOC)
Description of the cohorts used for the analysis of SHANK copy-number variants. a,b Indicate the publications with overlap in the cohorts. * The total number of independent cases or controls is not the addition of the cohorts from each study due to the redundancy of the cases and controls tested from these publications. The independent numbers were obtained in collaboration with the authors of the corresponding publications (see Material & Method in supplementary Appendix). The parental DNA of controls was not available. PARIS, Paris Autism Research International Sibpair study; SSC, Simons Simplex Collection; AGP, Autism Genome Project; ACC, Autism Case Control; SAGE, Study of Addiction: Genetics and Environment; CHOP, Children's Hospital of Philadelphia; WTCCC2, Wellcome Trust Case Control Consortium; AGRE, Autism Genetic Resource exchange; NIMH, National Institute of Mental Health; SNP, Single Nucleotide Polymorphism; CEU, Utah residents with Northern and Western European ancestry from the CEPH collection; BAC, Bacterial Artificial Chromosome; CGH, Comparative Genomic Hybridization; ROMA, Representational Oligonucleotide Microarray Analysis; ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision; DISCO, Diagnostic Interview for Social and Communication Disorders; IQ, Intellectual Quotient; RPM, Raven's Progressive Matrices; PPVT, Peabody Picture Vocabulary Test.
(DOC)
Description of the cohorts used for the analysis of SHANK coding-sequence variants. a In this study, controls were tested using allelic discrimination by TaqMan technology and only for the variations identified in ASD. The parental DNA of controls was not available. SUVIMAX, Supplémentation en Vitamines et Minéraux Antioxydants; ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision; DISCO, Diagnostic Interview for Social and Communication Disorders; IQ, Intellectual Quotient; RPM, Raven's Progressive Matrices; PPVT, Peabody Picture Vocabulary Test; SSC, Simons Simplex Collection.
(DOC)
Prevalence of SHANK CNVs and coding-sequence variants in patients with ASD and controls. a Sato et al. (2012), Durand et al. (2007) Leblond et al. (2012) contained overlapping cohorts. For this study, the French and Swedish cases are in Leblond et al (2012) and the Canadian cases are in Sato et al. (2012). bThe controls from Sato et al. 2012 are not included here because they were only tested by Taqman for the variants identified in ASD. cThe two SHANK3 deletions reported by Glessner et al. (2009) in control subjects have not been validated and should be interpreted with caution. CSV, Coding-Sequence Variant; 95CI, 95% Confidence Interval.
(DOC)
Prevalence of SHANK CNVs and coding-sequence variants in ASD patients with or without ID. a Sato et al. (2012) and Leblond et al. (2012) contained overlapping cohorts. For this study, the French and Swedish cases are in Leblond et al (2012) and the Canadian cases are in Sato et al. (2012). b The controls from Sato et al. 2012 are not included here because they were only tested by Taqman for the variants identified in ASD. CSV, Coding-Sequence Variant.
(DOC)
Genetic and clinical features of ASD patients carrying de novo/deleterious SHANK mutations. a Mother showed anxiety and shyness. b Mutations not present in the mother and father not tested (DNA unavailable). c Father had a balanced translocation t(14;22)(p11.2;q13.33). d Mother had a balanced translocation t(14;22)(p11.2;q13.33). e No epilepsy, but abnormal EEG with bilateral epileptiform discharges. f Relatives of proband IV-1. g Case reports not reported in a systematic screening of SHANK2 or whole genome analysis. h Patient detected in an additional mutation screening of SHANK3 exon 21. i Relatives of AU016_3. j Not included in the figure: large deletion involving numerous genes or complex chromosomal rearrangement. k For SHANK3, we only included in figure 2 the patients from the PARIS cohort. l No pictures available. m The phenotypic features were characteristic to the Phelan-Mcdermid syndrome. AS, absence seizures; ASD, autism spectrum disorder; Asp, Asperger syndrome; Aut, autism; CNV, copy number variant, CSV, coding-sequence variants; del, deletion; f, female; ID; inh, inherited; m, male; U, unknown; y, years; GTCS, generalized tonic-clonic seizures.
(DOC)
Primers used for mutation screening of SHANK1 and SHANK3. The red sequences correspond to the M13 adaptor (M13F = TGTAAAACGACGGCCAGT & M13R = GGATAACAATTTCACACAGG). PCR, Polymerase Chain Reaction; TpQ, Tampon Q (from Qiagen); DMSO, Dimethyl sulfoxide.
(DOC)
SHANK1 coding-sequence variants identified in 760 patients with ASD and 492 controls. aNucleotide positions are according to NM_016148 from NCBI37/hg19 on the positive DNA strand (chromosome 19). The patients with ASD used for this analysis came from this study (n = 240) and from the study of Sato et al. (2012) (n = 509). The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling; pph2_class, polyphen-2_class.
(DOC)
SHANK2 coding-sequence variants identified in 851 patients with ASD and 1 090 controls. #Indicates de novo mutations. aNucleotide positions are according to NM_012309.3 from NCBI37/hg19 on the positive DNA strand (chromosome 11). bMaximum Grantham score (215) given for non-sense variants. The patients with ASD and the controls used for this analysis came from Leblond et al. (2012) (455 ASD & 431 controls) and from the study of Berkel et al. (2010) (396 ASD & 659 controls). The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling; pph2_class, polyphen-2_class.
(DOC)
SHANK3 coding-sequence variants identified in 2 147 patients with ASD and 1 031 controls. #Indicates de novo mutations. +Q1243X was identified during an additional screen (nASD = 138) of exon 21 of SHANK3 and was not included in the meta-analysis. aNucleotide positions are according to NM_033517 from NCBI37/hg19 on the positive DNA strand (chromosome 22); bFor the variants with MAF>1%, the frequency was assessed only in PARIS cohort. cAverage GERP score for two sites flanking the insertion or average GERP score for deleted nucleotides; dMaximum Grantham score (215) given for splice, non-sense and frameshifting variants. The patients with ASD and the controls used for this analysis came from this study (n = 429) and from the studies reported in Table S5. The Grantham matrix and GERP scores were obtained from SeattleSeq Annotation 134. We used the Fisher's exact test (2-sided) and Pearson's Chi-squared test with Yates' continuity correction. P, p-value; ASD, Autism Spectrum Disorder; MAF, Minor Allele Frequency; GERP, Genomic Evolutionary Rate Profiling, pph2_class, polyphen-2_class.
(DOC)
Statistical power of the association between SHANK damaging missense variants and ASD. *Two-sided Fisher's exact test.
(DOC)
Supplementary method describing the genomic structure of the SHANK genes, coverage of SHANK genes by exome sequencing, cytogenetic analysis and FISH, multiplex ligation-dependent probe amplification (MLPA), genetic ancestry of patients with ASD and controls.
(DOC)