Abstract
Background
This study aimed to investigate the correlation between quantitative retinal vascular parameters such as central retinal arteriolar equivalent (CRAE) and retinal vascular fractal dimension (D(f)), and cardiovascular risk factors in the Chinese Han population residing in the in islands of southeast China.
Methodology/Principle Findings
In this cross-sectional study, fundus photographs were collected and semi-automated analysis software was used to analyze retinal vessel diameters and fractal dimensions. Cardiovascular risk factors such as relevant medical history, blood pressure (BP), lipids, and blood glucose data were collected. Subjects had a mean age of 51.9±12.0 years and included 812 (37.4%) males and 1,357 (62.6%) females. Of the subjects, 726 (33.5%) were overweight, 226 (10.4%) were obese, 272 (12.5%) had diabetes, 738 (34.0%) had hypertension, and 1,156 (53.3%) had metabolic syndrome. After controlling for the effects of potential confounders, multivariate analyses found that age (β = 0.06, P = 0.008), sex (β = 1.33, P = 0.015), mean arterial blood pressure (β = −0.12, P<0.001), high-sensitivity C-reactive protein (β = −0.22, P = 0.008), and CRVE (β = 0.23, P<0.001) were significantly associated with CRAE. Age (β = −0.0012, P<0.001), BP classification (prehypertension: β = −0.0075, P = 0.014; hypertension: β = −0.0131, P = 0.002), and hypertension history (β = −0.0007, P = 0.009) were significantly associated with D(f).
Conclusions/Significance
D(f) exhibits a stronger association with BP than CRAE. Thus, D(f) may become a useful indicator of cardiovascular risk.
Introduction
Retinal vessels are the only segment of the human microcirculation that can be observed directly. Recently, the associations between central retinal arteriolar equivalent (CRAE) and many cardiovascular risk factors have been demonstrated [1]–[5]. The American Heart Association estimates that more than 1 in 3 adults Americans have one or more types of cardiovascular disease [6]. Because of this high prevalence, diagnostic screening tools are important in order to optimally manage the disease. Retinal vasculature changes associated with hypertension can generally be divided into three groups: 1) classic retinal vascular changes in response to blood pressure (hypertensive retinopathy), 2) changes in retinal vascular caliber, and 3) changes in global geometric patterns of the retina [7].
Quantitative assessment of retinal vascular parameters is a precise and reliable method of investigating the relationship between microcirculation and cardiovascular disease [8], and most studies have focused on retinal vascular caliber, which is correlated with blood pressure (BP) [9]. Pooled data from the Beaver Dam Eye Study and the Blue Mountains Eye Study demonstrated that smaller arterioles and larger venules predicted an increased risk of mortality from coronary heart disease [10]. A larger central retinal vein is associated with smoking, low high-density lipoprotein cholesterol (HDL-C), elevated glycated hemoglobin (HbA1c), and high body mass index (BMI), and is able to independently predict the 6-year incidence of hypertension [5], [11]. A recent study conducted over an 18-year period found that every 10 mm Hg increase in mean systolic blood pressure (SBP) was associated with a 1.9 reduction in CRAE [12].
The human retinal vascular network, including its branching pattern, has been demonstrated to have a fractal structure [13], [14]. Retinal vascular fractal dimension, D(f), has been shown to be related to hypertension [8], [9], [15], diabetic retinopathy [16], [17], chronic kidney disease (CKD) [18], stroke [19], [20], and mortality from coronary heart disease [21]. Retinal vessel diameters have been shown to vary in different populations [5], [22], and there is a paucity of data on the correlation between changes in the retinal vasculature and risk factors for cardiovascular disease in the native Chinese population [22], [23]. In addition, D(f) has not been described in the Chinese population. The coastal regions of China have a high prevalence of fishery workers, and studies of fishery workers in other countries suggest a higher prevalence of hypertension in these individuals [24], [25].
The current cross-sectional study was designed to investigate the relationship of quantitative retinal vascular parameters such as CRAE, central retinal venular equivalent (CRVE), and D(f) with cardiovascular risk factors in a Chinese Han population residing in the islands off southeast China.
Methods
Subjects
The villages of Tailu, Beijiao, and Xiubang in the Tailu township in Lienchiang county and Kungtung, Kunghsi, Yantai, and Wenwo in Haidao township in Xiapu county in Fujian Province were randomly selected for this cross-sectional investigation, which took place from July, 2011 to November, 2011. These participants were selected because it has been shown that coaster villagers are at higher risk for hypertension [26].
Inclusion criteria were voluntary participants aged 30 years or more living in Tailu and Haidao townships for more than 5 years. Subjects were excluded if they were diagnosed with or were suspected to have secondary hypertension, acute myocardial infarction, acute stroke, infection, or an inflammatory disease. Individuals who had persistent arrhythmias (e.g., atrial fibrillation), chronic heart dysfunction, pulmonary hypertension, acute and chronic infectious diseases, malignancy, hematuria or urinary tract infection, peripheral vascular disease, ankle-brachial index (ABI) <0.6, or paralysis were also excluded. In addition, individual with a history of serious eye diseases such as corneal diseases, glaucoma, macular degeneration, or eye injuries, pregnant women, and anyone who could not cooperate with study requirements were excluded.
All participants provided signed informed consent form. This study was conducted in accordance with the Declaration of Helsinki, and was approved by the Institutional Review Board of the Fujian Provincial Hospital.
Data collection
Age, educational background, smoking history, alcohol history, and relevant medical history (e.g. hypertension, chronic heart failure and arrhythmia) were obtained using questionnaires. Physical examinations included height (cm), weight (kg), heart rate (HR, beats/minute) and BP. Examinees could not smoke or drink coffee within 30 minutes before measuring blood pressure. After emptying his/her bladder and resting in a quiet environment for 5 to 10 minutes, the examinee’s BP was measured by using a standard vertical mercury sphygmomanometer on the right upper arm. The average of three BP measurements obtained 1–2 minutes apart was calculated and recorded.
Classification definitions
BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). According to the BMI, subjects were divided in three categories: normal or underweight (BMI<24 kg/m2), overweight (24–28 kg/m2) and obese (>28 kg/m2) [27]. Hypertension was defined as SBP≥140 mm Hg and diastolic BP (DBP) ≥90 mm Hg in the presence or absence of anti-hypertension medications [28]. In the absence of anti-hypertensive medications, a systolic BP of 120–139 mm Hg and diastolic BP of 80–89 mm Hg was defined as “prehypertension” and a systolic BP of <120 mm Hg and diastolic BP of <80 mm Hg was defined as normal [29].
Laboratory testing
After an 8-hour overnight fast, blood samples were obtained measurement of triglyceride (TG), total cholesterol (TC), HDL-C, low-density lipoprotein cholesterol (LDL-C), fasting plasma glucose (FPG), HbA1c, high-sensitivity C-reactive protein (hs-CRP), and serum uric acid. Participants diagnosed with diabetes, those currently taking anti-diabetic medications, or with an HbA1c≥6.5% were defined as diabetic [29].
Data collection and quantitative analysis of retinal vessels
Digital fundus photographs were obtained using non-mydriatic fundus photography. Binocular digital photographs were taken using a 45° high-resolution fundus camera (Topcon NW-8, Topcon Corp, Tokyo, Japan; Nikon D90, Nikon Corp, Tokyo, Japan). Retinal fundus images were centered on the optic disc. The side of fundus photograph with a better quality image was analyzed, and double-blinded analysis was performed by two professionally trained ophthalmologists.
Semi-automated software (Singapore I Vessel Assessment, Version 3.0 [SIVA]; Exploit Technologies Private Limited, Singapore) was used for the quantitative analysis. SIVA software was been developed in collaboration with the Singapore Eye Research Institute, and has the capability of measuring a number of retinal vessel parameters including arteriolar/venular caliber, tortuosity, branching angles, and fractals.
The SIVA software was per the developer’s protocol. The software employs automatic optic disc detection and measures caliber and geometry of peripheral vessels up to 2 DD from the optic disc margin. Measurements were taken within a concentric grid (0.5–2.0 DD) centered on the optic disc [30]. The program automatically traced and identified all vessels (artery or vein) within the concentric circular grid, thus generating a skeleton image of the retinal microvasculature. The spatial resolution of each image was 3216×2136 pixels, and the images were stored without compression before analysis. The size of the scaling window was 1366×731 pixels. With the box counting method, the digitized retinal image was divided into a large number of equally sized square boxes, and the number of boxes containing a section of the refined skeletonized line tracing is counted; the process is then repeated with a different sized box. The fractal dimension of the skeletonized line tracing is the slope of the line obtained via plotting the logarithm of the number of boxes through which the tracing passes against the logarithm of the size of the boxes. Trained graders then correctly identified all vessels traced and removed all artifacts from the fundus photographs that may have been incorrectly drawn as vessels from the tracing. The reproducibility of this method has been shown in several studies [9], [15], [30].
CRAE and CRVE measurements, performed 0.5- to 1.0-disc diameter away from the optic disc margin, were calculated by the revised Knudtson-Parr-Hubbard formula (Fig. 1) [31]. Fractal geometry can be used to quantify a branching pattern that exhibits self-similarity, and the retinal vasculature has a fractal-like architecture. D(f), which is a measure of a fractal structure characterizing the distribution of the branching vascular system in two-dimensional space, was used to quantify the branching pattern of the retinal blood vessels. Retinal vascular D(f) was calculated from a skeletonized line tracing using the box-counting method, which divides each digital photograph into a series of squares of various side lengths, and the number of boxes is counted [8], [15]. D(f) was defined as the gradient of logarithms of the number of boxes and the size of the boxes [9]. Larger values indicate a more complex branching pattern, and two-dimensional fractal dimensions are between 1 and 2. D(f) measurements were performed 0.5- to 2.0-disc diameters away from the optic disc margin, as described by Cheung et al. [8].
Figure 1. Fundus photographs processed by SIVA version 3.0 software.
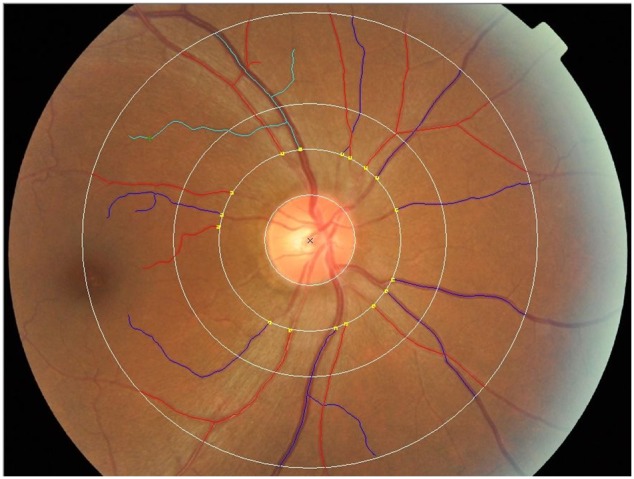
Test zone was 0.5- to 2.0-disc diameters away from the optic disc margin. A red line represents an artery and a blue line represents a vein. Fractal dimension, D(f), is a complexity indicator determined by reactive vessels obtained from vascular tracking through the box counting dimension method.
Statistical analysis
Continuous variables were presented as mean ± standard deviation, and categorical variables by count and percentage. To investigate the potential confounders associated with the retinal vascular parameters, simple and multiple linear regressions were performed. In univariate analyses, all significant factors were selected for entry into the multivariate models, except for those that had collinearity with other variables. Statistical analyses were performed with SAS software version 9.2 (SAS Institute Inc., Cary, NC). A two-sided P value<0.05 was considered to be statistically significant.
Results
Based on the household registration in the surveyed area, there were 8,947 who were more than 30 years of age. Of these, 4,616 were selected according to the age stratification theory and were issued study invitations. Of these, 3,614 received the study invitations because some people had relocated. A total of 3,343 people participated in the survey; therefore the response rate was 92.5%. A total of 1,174 subjects were excluded (421 with incomplete data, 49 with infectious diseases, 14 with atrial fibrillation, 15 with an ABI<0.6, 675 whose fundus photographs were inadequate); thus, 2,169 subjects were included in the analysis.
Baseline characteristics of the included and excluded subjects are shown in Table 1, and demographic and clinical data of the 2,169 participants are shown in Table 2. Study participants had a mean age of 51.9±12.0 years, and included 812 (37.4%) males and 1357 (62.6%) females. Among these subjects, 1,217 (56.1%) had a normal BMI, 726 (33.5%) were overweight, and 226 (10.4%) were obese. According to the JNC 7 criteria, 754 (34.8%) subjects had normal BP, 596 (27.5%) had prehypertension, and 819 (37.8%) had stage 1 or stage 2 hypertension.
Table 1. Characteristics of the included and excluded subjects (N = 3,343).
| Excluded | Included | ||
| (n = 1,174) | (n = 2,169) | P | |
| Age, y | 57.3±14.5 | 51.9±11.9 | <0.001 * |
| Males, % | 524 (44.6) | 812 (37.4) | 0.001 * |
| BMI, kg/m2 | 23.9±2.9 | 23.8±3.5 | 0.287 |
| SBP, mmHg | 134.4±25.9 | 127.0±21.9 | 0.001 * |
| DBP, mmHg | 80.2±12.8 | 78.6±11.9 | 0.322 |
| MAP, mmHg | 98.2±15.6 | 94.7±14.1 | 0.021 * |
| PP, mm Hg | 54.2±19.9 | 48.4±15.9 | <0.001 * |
| HR, beats per minute | 71.3±9.7 | 71.2±9.3 | 0.925 |
| Smoking, % | 306 (26.1) | 1828 (84.3) | <0.001 * |
| Alcohol consumption, % | 246 (21.0) | 341 (15.7) | <0.001 * |
| Diabetes, % | 183 (15.6) | 272 (12.5) | 0.016 * |
| Hypertension, % | 568 (48.4) | 819 (37.8) | <0.001 * |
| TG, mmol/L | 1.2±0.9 | 0.9±0.5 | <0.001 * |
| TC, mmol/L | 5.1±1.1 | 5.0±1.1 | 0.408 |
| HDL-C, mmol/L | 1.2±0.4 | 1.2±0.3 | 0.300 |
| LDL-C, mmol/L | 2.8±0.9 | 2.8±0.9 | 0.792 |
| FPG, mmol/L | 5.5±2.2 | 5.3±1.5 | 0.026 * |
| HbA1c, % | 5.8±0.9 | 5.7±0.7 | 0.001 * |
| Uric acid, µmol/L | 324.3±92.1 | 315.1±84.8 | 0.004 * |
| hs-CRP, mg/L | 1.9±4.7 | 1.4±3.4 | 0.001 * |
Continuous variables were reported as mean ± deviation (SD) and categorical variables as percentages (%).
SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; HR, heart rate; BMI, body mass index; TG, triglyceride; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; hs-CRP, high-sensitivity C-reactive protein.
*P<0.05 indicates a significant difference between groups.
Table 2. Characteristics of study subjects (n = 2,169).
| Age, y | 51.9±12.0 |
| Gender | |
| Males | 812 (37.4) |
| Females | 1357 (62.6) |
| BMI, kg/m2 | |
| <24 | 1217 (56.1) |
| 24–28 | 726 (33.5) |
| >28 | 226 (10.4) |
| SBP, mm Hg | 126.9±21.9 |
| DBP, mm Hg | 78.6±11.9 |
| MAP, mm Hg | 94.7±14.1 |
| PP, mm Hg | 48.4±15.9 |
| Blood pressure classification | |
| Normal | 754 (34.8) |
| Prehypertension | 596 (27.5) |
| Hypertension | 819 (37.8) |
| HR, beats/minute | 71.2±9.3 |
| Smoking | |
| Never | 1754 (80.9) |
| Current or former | 415 (19.1) |
| Alcohol consumption | |
| Never | 1828 (84.3) |
| Current or former | 341 (15.7) |
| Diabetes | |
| Absent | 1897 (87.5) |
| Present | 272 (12.5) |
| Hypertension | |
| Absent | 1431 (66.0) |
| Present | 738 (34.0) |
| Metabolic syndrome | |
| Absent | 1013 (46.7) |
| Present | 1156 (53.3) |
| TG, mmol/L | 0.9±0.5 |
| TC, mmol/L | 5.0±1.0 |
| HDL-C, mmol/L | 1.2±0.3 |
| LDL-C, mmol/L | 2.8±0.9 |
| FPG, mmol/L | 5.3±1.5 |
| Uric acid, µmol/L | 315.0±84.8 |
| HbA1c, % | 5.7±0.7 |
| hs-CRP, mg/L | 1.4±3.4 |
| CRAE, µm | 134.1±11.1 |
| CRVE, µm | 184.0±16.6 |
| D(f) | 1.4±0.1 |
Continuous variables were reported as mean ± deviation (SD) and categorical variables as count (%).
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; HR, heart rate; TG, triglyceride; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; hs-CRP, high-sensitivity C-reactive protein; CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; D(f), retinal vascular fractal dimension.
Hypertension: SBP≥140 mm Hg and DBP≥90 mm Hg, with or without medication. This group (n = 819) included subjects who were previously diagnosed (n = 738) and those diagnosed in this study based on the criteria above (n = 81).
Pre-hypertension: SBP 120–139 mm Hg and DBP 80–89 mm Hg without medication. Normal: SBP<120 mm Hg and DBP<80 mm Hg. Hypertension history was self-reported based on the questionnaire.
The mean CRAE, CRVE, and D(f) were 134.1±11.1 µm, 184.0±16.6 µm, and 1.4±0.1 µm, respectively. Simple linear regression analysis showed that age, gender, BMI, SBP, DBP, mean arterial pressure (MAP), pulse pressure (PP), BP classification, alcohol consumption, hypertension, TG, TC, LDL-C, hs-CRP, and CRVE were significantly associated with CRAE (all P≤0.041) (Table 3). After controlling for effects of potential confounders, multivariate analysis showed that age (β = 0.06, 95% confidence interval [CI] = 0.02 to 0.10, P = 0.008), sex (ß = 1.33, 95% CI = 0.26 to 2.40, P = 0.015), MAP (ß = −0.12, 95% CI = −0.17 to −0.07, P<0.001), hs-CRP (ß = −0.55, 95% CI = −0.96 to −0.15, P = 0.008) and CRVE (ß = 0.23, 95% CI = 0.20 to 0.25, P<0.001) were significantly associated with CRAE. Simple linear regression analysis also showed that age, SBP, DBP, MAP, PP, BP classification, smoking, alcohol consumption, hypertension, TG, uric acid, hs-CRP, and CRAE were significantly associated with CRVE (all, P≤0.021) (Table 4). After controlling for the effects of potential confounders, multivariate analysis showed that age (ß = −0.12, 95% CI = −0.19 to −0.05, P<0.001), smoking (ß = 2.87, 95% CI = 1.00 to 4.74, P = 0.003), and CRAE (ß = 0.51, 95% CI = 0.45 to 0.57, P<0.001) were significantly associated with CRVE.
Table 3. Simple and multiple linear regression analyses for CRAE.
| Univariate | Multivariate | |||
| β (95% CI) | P value | β (95% CI) | P value | |
| Age, y | −0.05 (−0.09, −0.01) | 0.009 * | 0.06 (0.02, 0.10) | 0.008 * |
| Gender | ||||
| Females (ref: males) | 2.12 (1.16, 3.09) | <0.001 * | 1.33 (0.26, 2.40) | 0.015 * |
| BMI, kg/m2 | ||||
| 24–28 (ref: <24) | −1.83 (−2.85, −0.81) | <0.001 * | −0.63 (−1.61, 0.35) | 0.205 |
| >28 (ref: <24) | −2.16 (−3.73, −0.58) | 0.007 * | −0.22 (−1.75, 1.32) | 0.782 |
| SBP, mm Hg | −0.09 (−0.11, −0.07) | <0.001 * | ||
| DBP, mm Hg | −0.17 (−0.21, −0.13) | <0.001 * | ||
| MAP, mm Hg | −0.15 (−0.18, −0.12) | <0.001 * | −0.12 (−0.17, −0.07) | <0.001 * |
| PP, mm Hg | −0.07 (−0.10, −0.04) | <0.001 * | 0.02 (−0.02, 0.05) | 0.345 |
| Blood pressure classification | ||||
| Prehypertension (ref: normal) | −2.28 (−3.46, −1.09) | <0.001 * | −0.42 (−1.72, 0.88) | 0.53 |
| Hypertension (ref: normal) | −3.98 (−5.07, −2.89) | <0.001 * | −0.43 (−2.28, 1.41) | 0.645 |
| HR, beats per minute | 0.03 (−0.02, 0.08) | 0.271 | ||
| Smoking | ||||
| Current or former (ref: never) | −0.35 (−1.54, 0.84) | 0.564 | ||
| Alcohol consumption | ||||
| Current or former (ref: never) | −2.12 (−3.41, −0.84) | 0.001 * | −1.01 (−2.41, 0.39) | 0.157 |
| Diabetes | ||||
| Present (ref: absent) | −0.03 (−1.45, 1.38) | 0.962 | ||
| Hypertension | ||||
| Present (ref: absent) | −1.77 (−2.76, −0.79) | <0.001 * | 0.14 (−0.99, 1.27) | 0.807 |
| Metabolic syndrome | ||||
| Present (ref: absent) | −0.72 (−1.66, 0.21) | 0.131 | ||
| TG, mmol/L | 1.29 (0.36, 2.22) | 0.007 * | 0.60 (−0.30, 1.50) | 0.195 |
| TC, mmol/L | −0.47 (−0.91, −0.02) | 0.041 * | −0.31 (−1.02, 0.39) | 0.384 |
| HDL-C, mmol/L | −0.26 (−1.68, 1.16) | 0.719 | ||
| LDL-C, mmol/L | −0.67 (−1.2, −0.14) | 0.013 * | 0.15 (−0.69, 0.98) | 0.731 |
| FPG, mmol/L | −0.17 (−0.48, 0.14) | 0.281 | ||
| Uric acid, µmol/L | 0.004 (−0.002, 0.009) | 0.218 | ||
| HbA1c, % | −0.13 (−0.82, 0.56) | 0.707 | ||
| hs-CRP, mg/L† | −1.21 (−1.60, −0.82) | <0.001 * | −0.55 (−0.96, −0.15) | 0.008 * |
| CRVE, µm | 0.52 (0.46, 0.58) | <0.001 * | 0.23 (0.2, 0.25) | <0.001 * |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; HR, heart rate; TG, triglyceride; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; hs-CRP, high-sensitivity C-reactive protein; CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; D(f), retinal vascular fractal dimension.
β (95% CI): regression coefficient and 95% confidence interval.
*P<0.05 indicates a significant association with CRAE.
Log transformation was applied.
The R2 for the multivariable regression model was 0.1621.
Table 4. Simple and multiple linear regression analyses for CRVE.
| Univariate | Multivariate | |||
| β (95% CI) | P value | β (95% CI) | P value | |
| Age, y | −0.14 (−0.2, −0.08) | <0.001 * | −0.12 (−0.19, −0.05) | <0.001 * |
| Gender | ||||
| Females (ref: Males) | −0.84 (−2.29, 0.60) | 0.253 | ||
| BMI, kg/m2 | ||||
| 24–28 (ref: <24) | −0.76 (−2.29, 0.77) | 0.330 | ||
| >28 (ref: <24) | −1.91 (−4.27, 0.45) | 0.112 | ||
| SBP, mm Hg | −0.07 (−0.10, −0.04) | <0.001 * | ||
| DBP, mm Hg | −0.08 (−0.14, −0.02) | 0.009 * | ||
| MAP, mm Hg | −0.09 (−0.14, −0.04) | <0.001 * | 0.002 (−0.08, 0.08) | 0.969 |
| PP, mm Hg | −0.09 (−0.14, −0.05) | <0.001 * | −0.04 (−0.09, 0.02) | 0.18 |
| Blood pressure classification | ||||
| Prehypertension (ref: normal) | −0.44 (−2.22, 1.34) | 0.627 | 1.34 (−0.61, 3.30) | 0.179 |
| Hypertension (ref: normal) | −2.62 (−4.26, −0.98) | 0.002 * | 1.89 (−0.89, 4.67) | 0.182 |
| HR, beats per minute | 0.02 (−0.06, 0.09) | 0.683 | ||
| Smoking | ||||
| Current or former (ref: never) | 3.60 (1.83, 5.37) | <0.001 * | 2.87 (1.00, 4.74) | 0.003 * |
| Alcohol consumption | ||||
| Current or former (ref: never) | 2.26 (0.34, 4.18) | 0.021 * | 1.96 (−0.06, 3.98) | 0.301 |
| Diabetes | ||||
| Present (ref: absent) | 1.03 (−1.08, 3.15) | 0.337 | ||
| Hypertension | −0.89 (−2.59, 0.80) | 0.301 | ||
| Present (ref: absent) | −2.59 (−4.06, −1.11) | 0.001 * | ||
| Metabolic syndrome | ||||
| Present (ref: absent) | 0.77 (−0.63, 2.17) | 0.283 | ||
| TG, mmol/L | 2.56 (1.17, 3.95) | <0.001 * | −0.10 (−0.75, 0.54) | 0.751 |
| TC, mmol/L | −0.44 (−1.11, 0.23) | 0.195 | ||
| HDL-C, mmol/L | −2.10 (−4.21, 0.02) | 0.052 | ||
| LDL-C, mmol/L | −0.78 (−1.57, 0.01) | 0.052 | ||
| FPG, mmol/L | 0.21 (−0.25, 0.68) | 0.372 | ||
| Uric acid, µmol/L | 0.012 (0.004, 0.021) | 0.003 * | 0.01 (0.0002, 0.02) | 0.044 * |
| HbA1c, % | 0.64 (−0.39, 1.66) | 0.225 | ||
| hs-CRP, mg/L† | −0.87 (−1.46, −0.28) | 0.004 * | −0.07 (−0.68, 0.54) | 0.824 |
| CRAE, µm | 0.23 (0.21, 0.26) | <0.001 * | 0.51 (0.45, 0.57) | <0.001 * |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; HR, heart rate; TG, triglyceride; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; hs-CRP, high-sensitivity C-reactive protein; CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; D(f), retinal vascular fractal dimension.
β (95% CI): regression coefficient and 95% confidence interval.
*P<0.05 indicates a significant association with CRVE.
Log transformation was applied.
The R2 for the multivariable regression model was 0.1412.
The average D(f) was 1.365 (range, 1.123 and 1.515). Simple linear regression analysis showed that age, BMI, SBP, DBP, MAP, PP, BP classification, diabetes, hypertension, metabolic syndrome, TG, TC, LDL-C, HbA1c, and hs-CRP were significantly associated with D(f) (all, P≤0.010) (Table 5). After controlling for potential confounders, multivariate analysis showed that age (ß = −0.0012, 95% CI = −0.0014 to −0.001, P<0.001), BP classification (prehypertension: ß = −0.0075, 95% CI = −0.0134 to −0.0015, P = 0.014; hypertension: ß = −0.0131, 95% CI = −0.0216 to −0.0047, P = 0.002), and history of hypertension (ß = −0.0007, 95% CI = −0.0121 to −0.0018, p = 0.009) were significantly associated with D(f).
Table 5. Simple and multiple linear regression analyses for D(f).
| Univariate | Multivariate | |||
| β (95% CI) | P value | β (95% CI) | P value | |
| Age, y | −0.0018 (−0.0019, −0.0016) | <0.001 * | −0.0012 (−0.0014, −0.001) | <0.001 * |
| Gender | ||||
| Females (ref: males) | 0.0033 (−0.0013, 0.0078) | 0.157 | ||
| BMI, kg/m2 | ||||
| 24–28 (ref: <24) | −0.0081 (−0.0129, −0.0033) | 0.001 * | 0.0024 (−0.0026, 0.0074) | 0.349 |
| >28 (ref: <24) | −0.0172 (−0.0246, −0.0098) | <0.001 * | 0.0001 (−0.0076, 0.0078) | 0.976 |
| SBP, mm Hg | −0.0008 (−0.0009, −0.0007) | <0.001 * | ||
| DBP, mm Hg | −0.0010 (−0.0012, −0.0008) | <0.001 * | ||
| MAP, mm Hg | −0.0011 (−0.0013, −0.0010) | <0.001 * | −0.0002 (−0.0004, 0) | 0.105 |
| PP, mm Hg | −0.0010 (−0.0011, −0.0009) | <0.001 * | −0.0001 (−0.0003, 0) | 0.151 |
| Blood pressure classification | ||||
| Prehypertension (ref: Normal) | −0.0188 (−0.0241, −0.0136) | <0.001 * | ||
| Hypertension (ref: Normal) | −0.0427 (−0.0476, −0.0378) | <0.001 * | −0.0075 (−0.0134, −0.0015) | 0.014 * |
| HR, beats per minute | −0.0001 (−0.0003, 0.0001) | 0.432 | −0.0131 (−0.0216, −0.0047) | 0.002 * |
| Smoking | ||||
| Current or former (ref: Never) | −0.0009 (−0.0065, 0.0047) | 0.746 | ||
| Alcohol consumption | ||||
| Current or former (ref: Never) | −0.0019 (−0.0079, 0.0042) | 0.540 | ||
| Diabetes | ||||
| Present (ref: Absent) | −0.0186 (−0.0252, −0.0120) | <0.001 * | −0.0029 (−0.0093, 0.0035) | 0.376 |
| Hypertension | ||||
| Present (ref: Absent) | −0.0291 (−0.0336, −0.0246) | <0.001 * | −0.007 (−0.0121, −0.0018) | 0.009 * |
| Metabolic syndrome | ||||
| Present (ref: Absent) | −0.0108 (−0.0152, −0.0065) | <0.001 * | −0.0024 (−0.0075, 0.0028) | 0.363 |
| TG, mmol/L | 0.0084 (0.0040, 0.0127) | <0.001 * | 0.0026 (−0.0017, 0.0069) | 0.243 |
| TC, mmol/L | −0.0038 (−0.0059, −0.0017) | <0.001 * | 0.003 (−0.0002, 0.0062) | 0.07 |
| HDL-C, mmol/L | −0.0018 (−0.0085, 0.0049) | 0.597 | ||
| LDL-C, mmol/L | −0.0071 (−0.0095, −0.0046) | <0.001 * | −0.0037 (−0.0075, 0.0002) | 0.062 |
| FPG, mmol/L | −0.0014 (−0.0029, 0.0001) | 0.061 | ||
| Uric Acid, µmol/L | −0.00002 (−0.0001, 0.000003) | 0.083 | ||
| HbA1c, % | −0.0123 (−0.0155, −0.0091) | <0.001 * | ||
| hs-CRP, mg/L† | −0.0084 (−0.0102, −0.0066) | <0.001 * | −0.0005 (−0.0024, 0.0013) | 0.563 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; HR, heart rate; TG, triglyceride; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; hs-CRP, high-sensitivity C-reactive protein; CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; D(f), retinal vascular fractal dimension.
β (95% CI): regression coefficient and 95% confidence interval.
*P<0.05 indicates a significant association with D(f).
Log transformation was applied.
The R2 for the multivariable regression model was 0.2031.
The Pearson’s correlation coefficient between PP and MAP was 0.573 (P<0.001). The variance inflation factors (VIFs) of MAP and PP were 2.785 and 1.782 in the CRAE model; 2.790 and 1.772 in the CRVE model; 2.731 and 2.755 in the D(f) model. VIF indicates the presence of multicollinearity; a VIF≥10 is often regarded as a sign of serious multicollinearity correction.
We compared FPG and diabetes in the univariate model and found no significant effect. If a variable had shown significance in the univariate model, it would have been included in the multivariate model. As seen in Tables 3, 4, and 5 FPG was not a significant factor in the univariate model, suggesting that FPG levels did not correlate with outcomes; therefore, that term was not included in the multivariate model for further analysis.
Discussion
Relationship of retinal vessel parameters with cardiovascular risk factors
A previous study reported a correlation between CRAE and plasmas TG [32]. The current study found that a narrow CRAE was associated with obesity and gender, while a large CRAE was associated age, smoking, and elevated HbA1c, consistent with previous reports [2]–[5], [33], [34]. The current study also showed that a decreased CRVE was associated with an increase of LDL-C; however, this correlation was not significant after adjusting for other cardiovascular risk factors. Therefore, we could not conclude that CRVE was associated with lipid levels. Our study did not find an association between CRVE and hs-CRP, consistent with the Cardiovascular Health Study [35], but inconsistent with the Beaver Dam [31] and multi-ethnic study of atherosclerosis (MESA) studies [5]. We suggest that differences between the current study and the Beaver Dam study including the participants’ age, angle of fundus photographs, software application for data analyses, and racial composition of the study cohorts contributed to the different findings. Compared to the MESA study, the current study subjects were ethnically homogeneous and the proportion of males was low (37.4% vs 53.6%, respectively). Additionally, our study subjects had lower educational levels, which might also have influenced the results.
A decrease in D(f) was associated with an increase of age in the current study. This finding was also shown in studies using a box counting dimension method to measure D(f) in whites and Malaysians [9], [15]. Another study using Fourier fractal dimension (FFD) techniques to express vascular network complexity also had the same results [36].
Relationship of retinal vessel parameters with BP
Hypertensive retinopathy is the most common ophthalmologic manifestation of hypertension [37]. Our study results indicated that CRAE was highly correlated with MAP, consistent with numerous studies in different populations including Singaporeans [23], Japanese [38], Caucasians [2], [3], [33], [39], African-Americans [4], and multiethnic populations [5]. MAP showed a stronger association with CRAE than PP, indicating that elevated BP has a stronger impact on central retinal artery stenosis than BP fluctuations. Similar to other studies, this study could not show causality; however, CRAE can predict stroke, mortality of cardiovascular diseases, and coronary heart disease independently of BP levels [39]–[42].
A number of studies [23], [24], [35], [37], [43] have shown that CRVE is not associated with hypertension. The current study also demonstrated no significant association between CRVE and hypertension, but found that a narrow CRVE was not related to an increased PP difference, which is inconsistent with the Rotterdam Study [34]. Increased BP and PP were associated with significant reductions in the retinal arteriolar and venular diameters and the arteriolar-to-venular ratio in the Rotterdam Study. In addition, a study with participants from southwestern Singapore found that retinal arteriolar tortuosity was correlated with elevated BP [44]. PP difference not only reflects a high SBP, but also implies different levels of arterial stiffness. We hypothesize that changes in venules may be due to the same pathological processes resulting in atherosclerosis, i.e., endothelial damage, oxidative stress, and lipid overload.
The current study showed that CRVE was independently associated with uric acid. Uric acid is an important pro-inflammatory factor [45], and some studies have found that uric acid plays a role similar to CRP. Elevated uric acid may suggest occult vasculitis or remodeling of pericapillary spaces [46]. Although the present study could not find the association between CRVE and CRP, other studies have found that increased CRVE was related to specific inflammatory factors. Despite the fact that uric acid is an antioxidant, high uric acid concentrations are associated with microvascular functional reserve or microvascular dysfunction [46]–[48]. This may be related to a series of downstream reactions caused by free radicals generated in the degradation process. Yuan et al. [49] studied a population at high-risk for diabates and found that uric acid concentrations were associated with decreased CRAE and increased CRVE. Our study was a population-based cross-sectional survey and there were methodological differences between the current study and that of Yuan et al.
Studies conducted in whites and Malaysians [9], [15] showed that D(f) was independently associated with SBP, DBP, MABP, and PP. Compared to the association between CRAE and SBP, D(f) showed a stronger association with SBP. The current study found D(f) to be highly correlated with BP classification (prehypertension, hypertension). We speculate that D(f) may have greater sensitivity than CRAE for hypertension morbidity and severity.
Relationship of retinal vessel parameters and FPG, Hba1c, and diabetes
A study in northwest Shanghai reported that participants with narrower retinal arteriolar calibers were diagnosed with metabolic syndrome nearly twice as often as their normal counterparts (odds ratio 1.78) [50]. A relationship of larger CRVE with high HbA1c has been demonstrated [2]–[5], [33]. In addition, Tsai et al. [51] reported that in diabetic patients a wider CRAE was correlated with increasing glucose (P<0.001) and HbA1c levels (P<0.001). Other studies have found correlations between increasing Hba1c levels, plasma glucose levels, and retinal venular caliber measurements [52]. It is likely that we did not find an association with these measurements due to the differences in our study population compared with previous studies.
To the best of our knowledge, D(f) independently associated with HbA1c has not been reported in other studies: however, this finding might help to explain the association between D(f) and diabetic retinopathy [16], [17], [53]. We suggest that the incidence of low D(f) and diabetic retinopathy is increased in diabetic patients with long-term poor control of blood sugar. Thus, we hypothesize that D(f) might be considered as a predictor of diabetic microangiopathy and target organ damage in diabetic patients.
Study strengths and limitations
Strengths of the current study are the large number of patients and the fact that it was restricted to the Chinese Han population in coastal regions. Limitations are the study design, which cannot determine causality, selection bias because a relatively large number of subjects were excluded, and patients with ophthalmic diseases such as refractive errors and lens opacity were excluded, which may have influenced D(f). Genetic factors, hormone levels, cell factors, and environmental influences which may have affected retinal vascular parameters were not evaluated. Some bias may be present because retinal vessel diameters are affected by the cardiac cycle.
Conclusions
In summary, CRAE is predominantly related to gender, smoking, and BP. D(f) was associated with aging, hypertension, and HbA1c level, and D(f) had a stronger association with MAP, SBP, and PP than CRAE.
Funding Statement
This study was supported by the Fujian Major Program of Basic Science Project Foundation entitled “Epidemiologic survey of hypertension and prehypertension intervention research in HaiDao County of Fujian Province” [2010Y0013] and The Predictive Value of Retinal Quantitative Parameters and Cardiovascular Risk Factors Relativity on Subclinical Arteriosclerosis: a Prospective Study [2013Y0023]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Torres FS, Fuchs SC, Maestri MK, Fuchs FD, Oliveira MM, et al. (2013) Association between carotid intima-media thickness and retinal arteriolar and venular diameter in patients with hypertension: a cross-sectional study. Atherosclerosis 229: 134–138. [DOI] [PubMed] [Google Scholar]
- 2. Wong TY, Klein R, Sharrett AR, Duncan BB, Couper DJ, et al. (2002) Retinal arteriolar narrowing and risk of coronary heart disease in men and women. The Atherosclerosis Risk in Communities Study. JAMA 287: 1153–1159. [DOI] [PubMed] [Google Scholar]
- 3. Ikram MK, de Jong FJ, Bos MJ, Vingerling JR, Hofman A, et al. (2006) Retinal vessel diameters and risk of stroke: the Rotterdam Study. Neurology 66: 1339–1343. [DOI] [PubMed] [Google Scholar]
- 4. Wong TY, Kamineni A, Klein R, Sharrett AR, Klein BE, et al. (2006) Quantitative retinal venular caliber and risk of cardiovascular disease in older persons: the cardiovascular health study. Arch Intern Med 166: 2388–2394. [DOI] [PubMed] [Google Scholar]
- 5. Wong TY, Islam FM, Klein R, Klein BE, Cotch MF, et al. (2006) Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Invest Ophthalmol Vis Sci 47: 2341–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, et al. (2012) Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation 125: e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cheung CY, Ikram MK, Sabanayagam C, Wong TY (2012) Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension 60: 1094–1103. [DOI] [PubMed] [Google Scholar]
- 8. Cheung CY, Tay WT, Mitchell P, Wang JJ, Hsu W, et al. (2011) Quantitative and qualitative retinal microvascular characteristics and blood pressure. J Hypertens 29: 1380–1391. [DOI] [PubMed] [Google Scholar]
- 9.Cheung CY, Thomas GN, Tay W, Ikram MK, Hsu W, et al. (2012) Retinal vascular fractal dimension and its relationship with cardiovascular and ocular risk factors. Am J Ophthalmol 154: 663–674 e661. [DOI] [PubMed]
- 10. Wang JJ, Liew G, Klein R, Rochtchina E, Knudtson MD, et al. (2007) Retinal vessel diameter and cardiovascular mortality: pooled data analysis from two older populations. Eur Heart J 28: 1984–1992. [DOI] [PubMed] [Google Scholar]
- 11. Roy MS, Klein R, Janal MN (2012) Relationship of retinal vessel caliber to cardiovascular disease and mortality in African Americans with type 1 diabetes mellitus. Arch Ophthalmol 130: 561–567. [DOI] [PubMed] [Google Scholar]
- 12. Avery CL, Kucharska-Newton A, Monda KL, Richey Sharrett A, Mosley TH, et al. (2012) Impact of long-term measures of glucose and blood pressure on the retinal microvasculature. Atherosclerosis 225: 412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ţălu Ş (2013) Characterization of retinal vessel networks in human retinal imagery using quantitative descriptors. Human Vet Med 5: 52–57. [Google Scholar]
- 14. Lopes R, Betrouni N (2009) Fractal and multifractal analysis: a review. Med Image Anal 13: 634–649. [DOI] [PubMed] [Google Scholar]
- 15. Liew G, Wang JJ, Cheung N, Zhang YP, Hsu W, et al. (2008) The retinal vasculature as a fractal: methodology, reliability, and relationship to blood pressure. Ophthalmology 115: 1951–1956. [DOI] [PubMed] [Google Scholar]
- 16. Lim SW, Cheung N, Wang JJ, Donaghue KC, Liew G, et al. (2009) Retinal vascular fractal dimension and risk of early diabetic retinopathy: A prospective study of children and adolescents with type 1 diabetes. Diabetes Care 32: 2081–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cheung N, Donaghue KC, Liew G, Rogers SL, Wang JJ, et al. (2009) Quantitative assessment of early diabetic retinopathy using fractal analysis. Diabetes Care 32: 106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sng CC, Sabanayagam C, Lamoureux EL, Liu E, Lim SC, et al. (2010) Fractal analysis of the retinal vasculature and chronic kidney disease. Nephrol Dial Transplant 25: 2252–2258. [DOI] [PubMed] [Google Scholar]
- 19. Cheung N, Liew G, Lindley RI, Liu EY, Wang JJ, et al. (2010) Retinal fractals and acute lacunar stroke. Ann Neurol 68: 107–111. [DOI] [PubMed] [Google Scholar]
- 20. Kawasaki R, Che Azemin MZ, Kumar DK, Tan AG, Liew G, et al. (2011) Fractal dimension of the retinal vasculature and risk of stroke: a nested case-control study. Neurology 76: 1766–1767. [DOI] [PubMed] [Google Scholar]
- 21. Liew G, Mitchell P, Rochtchina E, Wong TY, Hsu W, et al. (2011) Fractal analysis of retinal microvasculature and coronary heart disease mortality. Eur Heart J 32: 422–429. [DOI] [PubMed] [Google Scholar]
- 22. Wang S, Xu L, Wang Y, Wang Y, Jonas JB (2007) Retinal vessel diameter in normal and glaucomatous eyes: the Beijing eye study. Clin Experiment Ophthalmol 35: 800–807. [DOI] [PubMed] [Google Scholar]
- 23. Sun C, Liew G, Wang JJ, Mitchell P, Saw SM, et al. (2008) Retinal vascular caliber, blood pressure, and cardiovascular risk factors in an Asian population: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 49: 1784–1790. [DOI] [PubMed] [Google Scholar]
- 24. Kirkutis A, Norkiene S, Griciene P, Gricius J, Yang S, et al. (2004) Prevalence of hypertension in Lithuanian mariners. Proc West Pharmacol Soc 47: 71–75. [PubMed] [Google Scholar]
- 25. Fodor JG, Abbott EC, Rusted IE (1973) An epidemiologic study of hypertension in Newfoundland. Can Med Assoc J 108: 1365–1368. [PMC free article] [PubMed] [Google Scholar]
- 26. Huang F, Zhu PL, Xiao HZ, Lin F, Yuan Y, et al. (2013) [Cardiovascular disease risk and vascular damage status in pre- and hypertension population in coastal areas of Fujian province]. Zhonghua Xin Xue Guan Bing Za Zhi 41: 876–881. [PubMed] [Google Scholar]
- 27. Alberti KG, Zimmet P, Shaw J (2005) Group IDFETFC (2005) The metabolic syndrome–a new worldwide definition. Lancet 366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 28. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289: 2560–2572. [DOI] [PubMed] [Google Scholar]
- 29.Basevi V, Di Mario S, Morciano C, Nonino F, Magrini N (2011) Comment on: American Diabetes Association. Standards of medical care in diabetes–2011. Diabetes Care 2011; 34(Suppl. 1): S11–S61. Diabetes Care 34: e53; author reply e54. [DOI] [PMC free article] [PubMed]
- 30. Crosby-Nwaobi R, Heng LZ, Sivaprasad S (2012) Retinal vascular calibre, geometry and progression of diabetic retinopathy in type 2 diabetes mellitus. Ophthalmologica 228: 84–92. [DOI] [PubMed] [Google Scholar]
- 31. Knudtson MD, Lee KE, Hubbard LD, Wong TY, Klein R, et al. (2003) Revised formulas for summarizing retinal vessel diameters. Curr Eye Res 27: 143–149. [DOI] [PubMed] [Google Scholar]
- 32. Liew G, Sharrett AR, Wang JJ, Klein R, Klein BE, et al. (2008) Relative importance of systemic determinants of retinal arteriolar and venular caliber: the atherosclerosis risk in communities study. Arch Ophthalmol 126: 1404–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wong TY, Shankar A, Klein R, Klein BE, Hubbard LD (2004) Prospective cohort study of retinal vessel diameters and risk of hypertension. BMJ 329: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ikram MK, de Jong FJ, Vingerling JR, Witteman JC, Hofman A, et al. (2004) Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Invest Ophthalmol Vis Sci 45: 2129–2134. [DOI] [PubMed] [Google Scholar]
- 35. Wong TY, Klein R, Sharrett AR, Manolio TA, Hubbard LD, et al. (2003) The prevalence and risk factors of retinal microvascular abnormalities in older persons: The Cardiovascular Health Study. Ophthalmology 110: 658–66. [DOI] [PubMed] [Google Scholar]
- 36.Azemin MZ, Kumar DK, Wong TY, Wang JJ, Mitchell P, et al. (2012) Age-related rarefaction in the fractal dimension of retinal vessel. Neurobiol Aging 33: 194 e1–4. [DOI] [PubMed]
- 37. Gepstein R, Rosman Y, Rechtman E, Koren-Morag N, Segev S, et al. (2012) Association of retinal microvascular caliber with blood pressure levels. Blood Press 21: 191–196. [DOI] [PubMed] [Google Scholar]
- 38. Kawasaki R, Wang JJ, Rochtchina E, Taylor B, Wong TY, et al. (2006) Cardiovascular risk factors and retinal microvascular signs in an adult Japanese population: the Funagata Study. Ophthalmology 113: 1378–1384. [DOI] [PubMed] [Google Scholar]
- 39. Smith W, Wang JJ, Wong TY, Rochtchina E, Klein R, et al. (2004) Retinal arteriolar narrowing is associated with 5-year incident severe hypertension: the Blue Mountains Eye Study. Hypertension 44: 442–447. [DOI] [PubMed] [Google Scholar]
- 40. Wong TY, Klein R, Sharrett AR, Duncan BB, Couper DJ, et al. (2004) Retinal arteriolar diameter and risk for hypertension. Ann Intern Med 140: 248–255. [DOI] [PubMed] [Google Scholar]
- 41. Wong TY, Klein R, Couper DJ, Cooper LS, Shahar E, et al. (2001) Retinal microvascular abnormalities and incident stroke: the Atherosclerosis Risk in Communities Study. Lancet 358: 1134–1140. [DOI] [PubMed] [Google Scholar]
- 42. Wong TY, Klein R, Nieto FJ, Klein BE, Sharrett AR, et al. (2003) Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case-control study. Ophthalmology 110: 933–940. [DOI] [PubMed] [Google Scholar]
- 43. Leung H, Wang JJ, Rochtchina E, Wong TY, Klein R, et al. (2004) Impact of current and past blood pressure on retinal arteriolar diameter in an older population. J Hypertens 22: 1543–1549. [DOI] [PubMed] [Google Scholar]
- 44. Cheung CY, Zheng Y, Hsu W, Lee ML, Lau QP, et al. (2011) Retinal vascular tortuosity, blood pressure, and cardiovascular risk factors. Ophthalmology 118: 812–818. [DOI] [PubMed] [Google Scholar]
- 45. Feig DI, Kang DH, Johnson RJ (2008) Uric acid and cardiovascular risk. N Engl J Med 359: 1811–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Erdogan D, Gullu H, Caliskan M, Yildirim I, Ulus T, et al. (2006) Coronary flow reserve and coronary microvascular functions are strongly related to serum uric acid concentrations in healthy adults. Coron Artery Dis 17: 7–14. [DOI] [PubMed] [Google Scholar]
- 47. de ACT, Turner ST, Kullo IJ (2007) Serum uric acid is associated with microvascular function in hypertensive individuals. J Hum Hypertens 21: 610–615. [DOI] [PubMed] [Google Scholar]
- 48. Gullu H, Erdogan D, Caliskan M, Tok D, Kulaksizoglu S, et al. (2007) Elevated serum uric acid levels impair coronary microvascular function in patients with idiopathic dilated cardiomyopathy. Eur J Heart Fail 9: 466–468. [DOI] [PubMed] [Google Scholar]
- 49. Yuan Y, Ikram MK, Jiang S, Lin H, Ren L, et al. (2011) Hyperuricemia accompanied with changes in the retinal microcirculation in a Chinese high-risk population for diabetes. Biomed Environ Sci 24: 146–154. [DOI] [PubMed] [Google Scholar]
- 50. Yuan Y, Ikram MK, Vingerling JR, Jiang S, Lin H, et al. (2012) Retinal Vascular Caliber and Metabolic Syndrome in a Chinese Population. Intern Med J 42: 1014–1022. [DOI] [PubMed] [Google Scholar]
- 51. Tsai AS, Wong TY, Lavanya R, Zhang R, Hamzah H, et al. (2011) Differential association of retinal arteriolar and venular caliber with diabetes and retinopathy. Diabetes Res Clin Pract 94: 291–298. [DOI] [PubMed] [Google Scholar]
- 52. Cheung CY, Lamoureux E, Ikram MK, Sasongko MB, Ding J, et al. (2012) Retinal vascular geometry in Asian persons with diabetes and retinopathy. J Diabetes Sci Technol 6: 595–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Daxer A (1993) Characterisation of the neovascularisation process in diabetic retinopathy by means of fractal geometry: diagnostic implications. Graefes Arch Clin Exp Ophthalmol 231: 681–686. [DOI] [PubMed] [Google Scholar]


