Abstract
Background
Pseudomonas aeruginosa (PA) has a non-clonal, epidemic population with a few widely distributed and frequently encountered sequence types (STs) called ‘high-risk clusters’. Clinical P. aeruginosa (clinPA) has been studied in all inhabited continents excepted in Africa, where a very few isolates have been analyzed. Here, we characterized a collection of clinPA isolates from four countries of West and Central Africa.
Methodology
184 non-redundant isolates of clinPA from hospitals of Senegal, Ivory Coast, Nigeria, and Central African Republic were genotyped by MLST. We assessed their resistance level to antibiotics by agar diffusion and identified the extended-spectrum β-lactamases (ESBLs) and metallo-β-lactamases (MBLs) by sequencing. The population structure of the species was determined by a nucleotide-based analysis of the entire PA MLST database and further localized on the phylogenetic tree (i) the sequence types (STs) of the present collection, (ii) the STs by continents, (iii) ESBL- and MBL-producing STs from the MLST database.
Principal Findings
We found 80 distinct STs, of which 24 had no relationship with any known STs. ‘High-risk’ international clonal complexes (CC155, CC244, CC235) were frequently found in West and Central Africa. The five VIM-2-producing isolates belonged to CC233 and CC244. GES-1 and GES-9 enzymes were produced by one CC235 and one ST1469 isolate, respectively. We showed the spread of ‘high-risk’ international clonal complexes, often described as multidrug-resistant on other continents, with a fully susceptible phenotype. The MBL- and ESBL-producing STs were scattered throughout the phylogenetic tree and our data suggest a poor association between a continent and a specific phylogroup.
Conclusions
ESBL- and MBL-encoding genes are borne by both successful international clonal complexes and distinct local STs in clinPA of West and Central Africa. Furthermore, our data suggest that the spread of a ST could be either due to its antibiotic resistance or to features independent from the resistance to antibiotics.
Introduction
Pseudomonas aeruginosa is an important opportunistic human pathogen causing infection in patients with impaired immune systems [1]. Its intrinsic resistance to many classes of antibiotics and its capacity to acquire resistance to almost all effective antibiotics during treatment render infections with this microorganism very difficult to treat [2], [3]. Resistance to β-lactams is of particular concern in clinical practice. Hence, high-level resistance to these compounds is achieved by AmpC cephalosporinase overproduction or by the production of acquired β-lactamases with an extended spectrum (i.e., extended-spectrum-β-lactamases [ESBLs], metallo-β-lactamases [MBLs], and extended-spectrum oxacillinases) [4].
From a limited number of studies often focused on antibiotic-resistant isolates, it appears that P. aeruginosa has a non-clonal, epidemic population with a few widely distributed and frequently encountered sequence types (STs) called ‘high-risk clusters’ [5]–[10]. The population of clinical P. aeruginosa has been studied in Europe, Asia, Oceania, North and South Americas. Although West and Central Africa comprises large city agglomerations, little is known about the resistance level to antibiotics and the epidemiology of clinical P. aeruginosa. As proof, only 0.5% (8 isolates out of 1542) of the P. aeruginosa multilocus sequence typing (MLST) database concerns African isolates [11].
Large-scale epidemiological studies rely on the analysis of MLST developed by Curran et al. in 2004. This method is a reproducible manner to compare isolates that are temporally and geographically distant and handled by different laboratories, allowing a better knowledge of the global epidemiology in P. aeruginosa [7]. Quantifying the diversity of specific house-keeping genes by MLST analyses is a powerful approach for understanding the evolution of the core genome and the processes that shape the species biodiversity.
The aim of this study was to characterize a collection of clinical P. aeruginosa isolates from four countries of West and Central Africa. We assessed the resistance level to antipseudomonal agents and identified the β-lactamases with an extended-spectrum in the resistant isolates. We also identified all their STs and compared their distribution in a global phylogenetic tree built with all the currently defined STs described worldwide.
Material and Methods
Isolate collection
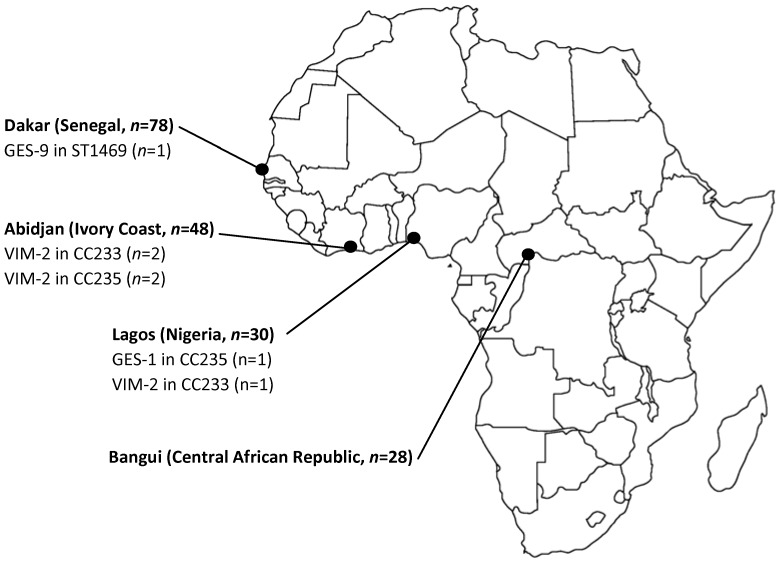
P. aeruginosa non-redundant clinical isolates were collected between 2002 and 2012 from patients hospitalized in the University Hospital of Fann (Dakar, Senegal, n = 78), in the Centre National de Référence des Antibiotiques de Côte d'Ivoire (Institut Pasteur, Abidjan, Ivory Coast, n = 48), in the Department of Medical Microbiology and Parasitology of the University of Lagos (Lagos, Nigeria, n = 30), and in the Institut Pasteur of Bangui (Bangui, Central African Republic, n = 28) for a total of 184 isolates. All the isolates were stored in Brain-Heart Infusion – Glycerol broth at −80°C and managed at the Centre de Ressources Biologiques Ferdinand Cabanne at the University Hospital of Besançon. Data were entirely anonymised throughout the entire study and thus ethical approval was not needed. Figure 1 represents the geographical origin of the isolates. All isolates were identified by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) with a Microflex LT (Bruker Daltonik GmbH, Bremen, Germany), according to the manufacturer procedures [12].
Figure 1. Map of Africa showing the four cities included in the study, the number of Pseudomonas aeruginosa clinical isolates, and the localization of ESBL- and MBL-producing isolates.
Antimicrobial susceptibility testing and β-lactamase identification
We assessed the activity of 9 antibiotics from four different classes (non-carbapenem β-lactams: cefepime, piperacillin-tazobactam, ticarcillin, ceftazidime, aztreonam; carbapenems: imipenem; aminoglycosides: tobramycin, amikacin; fluoroquinolones: ciprofloxacin) against the P. aeruginosa isolates by the disk diffusion method recommended by European Committee on Antimicrobial Susceptibility Testing (EUCAST, 2013 [13]). Here, all non-susceptible isolates were considered as resistant. We also identified extended-spectrum β-lactamases (ESBLs) and metallo-β-lactamases (MBLs) in isolates resistant to ceftazidime by the phenotypic method described elsewhere [14]. For isolates considered positive by this approach, the involved enzymes were identified by PCR and sequencing with primers targeting ESBL- and MBL-encoding genes [15].
Genotyping by pulsed-field gel electrophoresis (PFGE)
The clonality of all the isolates was investigated by PFGE, with DraI digestion, as previously described [16]. GelCompar software was used for cluster analysis (Applied Maths, Kortrijk, Belgium). The Dice correlation coefficients were grouped and the UPGMA clustering algorithm was used to depict the groups as a dendrogram. According to international recommendations, we clustered isolates that give PFGE patterns with ≤3 fragment differences in the same pulsotype (PT) [17]. We further genotyped by multi-locus sequence typing one isolate per PT.
Genotyping by multi-locus sequence typing (MLST)
MLST was performed according to the protocol of Curran et al. modified by van Mansfeld et al. [18]. Nucleotide sequences were determined for internal fragments of the acsA, aroE, guaA, mutL, nuoD, ppsA, and trpE genes and were compared with sequences in the P. aeruginosa MLST website (http://pubmlst.org/paeruginosa) for the assignment of allele numbers and sequence types (ST) [11]. Clonal complexes (CCs) were defined with the software START2 as a group of STs sharing at least 5 loci [19].
Analysis of MLST data
In order to build a dendrogram with the 1595 STs available at the time of the study (including the new ST described in this collection), we concatenated the sequences of 7 MLST genes to form a 2,882-bp sequences alignment, defining 664 polymorphic positions. The best-fit nucleotide substitution model for this data was GTR+G+I, as determined with jModelTest 0.1.1 [20]. We used the Pseudomonas fluorescens Pf0-1 as the outgroup [21]. Maximum likelihood tree was constructed with RAxML 7.2.8 [22] and visualized with Dendroscope 3.2.10 [23]. In every case, 1000 bootstrap repetitions gave values above 900 for most branches.
Results
Genotyping of the collection
We genotyped all the 184 clinical isolates from the four West and Central Africa countries by PFGE. We obtained 107 different PTs. As PFGE typing is more discriminatory than MLST, we assumed here that all the isolates that give PTs with ≤3 fragment differences shared the same ST (Cholley et al., submitted manuscript). We therefore determined the MLST profiles of one isolate for each of the 107 PTs. The ST of all the isolates is given in the Table S1. We found 80 distinct STs. Among them, 47 were already in the MLST database while the other 33 (from ST1437 to ST1493) were new [11]. Nine of these new STs belonged to widespread clonal complexes: ST1461 and ST1477 belonged to the CC195, the ST1467, ST1479, ST1481, ST1482 and ST1484 belonged to the CC244, the ST1466 belonged to the CC274 and ST1472 belonged to the CC233. Besides, 24 new STs were singletons, meaning that they share less than 5 loci with known STs. In our collection, we sought to identify isolates of successful international STs or CCs (i.e. that are found worldwide). We identified from the MLST database 15 intercontinental STs or CCs (isolated in patients from ≥3 continents among Europe, North and South Americas, Asia and Oceania): ST17, ST27, CC155, ST179, CC195, CC233, CC235, CC244, ST254, CC274, ST277, CC395, ST446, ST560, and CC654 [11]. These STs and CCs were not specific to the human host and have also been described in the environment. Nine of these widespread clinical STs or CCs were also present in West and Central Africa. Hence, CC155, CC244, CC235, CC195, CC274, CC233, CC395, CC654, and ST277 were represented by 23, 19, 8, 4, 4, 3, 3, 3, and 1 isolate, respectively in the present collection.
Resistance to antibiotics and production of extended-spectrum β-lactamases (ESBLs) and metallo-β-lactamases (MBLs)
Table 1 details the resistance rates to antibiotics of the isolates broken down by the country of origin. The antibiotic resistance profile of all the isolates is detailed in the Table S1. The resistance rates to the tested antibiotics remained low (≤10%) for isolates from Senegal and Central African Republic, with the exception of the higher resistance rate to ticarcillin in the latter country (25%). This contrasts with the much higher resistance rate of isolates from Ivory Coast and Nigeria. In these countries, 23–40% of the isolates were resistant to penicillins (ticarcillin and piperacillin/tazobactam), 13–30% were resistant to cephalosporins (cefepime and ceftazidime), 10–20% were resistant to aminoglycosides (tobramycin and amikacin), and 27% were resistant to ciprofloxacin.
Table 1. Characteristics of clinical isolates from West and Central Africa (n = 184), by country.
| Resistance rate (%) or resistance statusa | |||||||||||
| Country of isolation | Number of isolates | ST or CC | Tic | Tzp | Caz | Fep | Atm | Imp | Amk | Tob | Cip |
| Senegal | |||||||||||
| Total | 78 | - | 7.7 | 1.3 | 1.3 | 1.3 | 0b | 0 | 1.3 | 5.1 | 3.8 |
| GES-9-producing isolate | 1 | 1469 | R | S | R | R | I | S | R | R | R |
| Central African Republic | |||||||||||
| Total | 28 | - | 25.0 | 10.7 | 7.1 | 0 | 0b | 0 | 0 | 7.1 | 7.1 |
| Ivory Coast | |||||||||||
| Total | 48 | - | 29.2 | 22.9 | 14.6 | 12.5 | 2.1b | 16.7 | 16.7 | 22.9 | 27.1 |
| VIM-2-producing isolates | 4 | 244 (n = 2), 233 (n = 2) | 100 | 100 | 100 | 100 | 100b | 100 | 100 | 100 | 100 |
| Nigeria | |||||||||||
| Total | 30 | - | 40.0 | 26.7 | 20.0 | 30.0 | 3.3b | 10 | 20 | 20 | 26.7 |
| GES-1-producing isolate | 1 | 235 | R | R | R | R | I | R | R | R | R |
| VIM-2-producing isolate | 1 | 233 | R | R | R | R | I | R | R | R | R |
Resistance rate or resistance status were defined according to the 2013 recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST, 2013 [13]). Tic: ticarcillin; Tzp: Pipercillin-tazobactam; Caz: Ceftazidime; Fep: Cefepime; Atm: Aztreonam; Imp: Imipenem; Amk: Amikacin; Tob: Tobramycin; Cip: Ciprofloxacin. Here, all non-susceptible isolates were considered as resistant.
Only isolates with an inhibition diameter around the disk of aztreonam (30 µg) <16 mm were considered as resistant.
Eleven out of the 184 isolates collected were resistant to imipenem (Ivory Coast, n = 8; Nigeria, n = 3). We identified the metallo-β-lactamase VIM-2 in 5 of them. The remaining isolates did not produce any carbapenemase and were most probably resistant to imipenem after mutations in the gene encoding OprD or the down-regulation of the production of this porin [24]. Three VIM-2-producing isolates belonged to the CC233 (Ivory Coast, n = 2; Nigeria, n = 1) and two belonged to the CC244 (Ivory Coast, n = 2).
Sixteen isolates of the whole collection were resistant to ceftazidime. They were isolated mostly in Ivory Coast (n = 7) and Nigeria (n = 6). One CC235 isolate from Nigeria produced GES-1 and one ST1469 isolate from Senegal produced GES-9. Of note, none of the 28 isolates collected in Central African Republic produced β-lactamase with an extended-spectrum.
Interestingly, most of the isolates (17 out of 25) that displayed a multi-drug resistant phenotype according to the consensus definition of Magiorakos et al. (i.e., resistance to ≥1 agent in ≥3 antimicrobial categories) belonged to the intercontinental clonal complexes CC233 (n = 3), CC235 (n = 5), CC244 (n = 3), CC393 (n = 3), and CC654 (n = 3) [25]. These multi-drug resistant isolates mostly came from Nigeria (n = 11) and Ivory Coast (n = 10).
Spread of wild-type and antibiotic-resistant STs and CCs in West and Central Africa
Among the collection, seven STs were represented by more than 5 isolates. CC155 spread in Senegal with 23 isolates with a wild-type susceptibility phenotype. We retrieved the CC244 in the four countries studied. Of the 19 CC244 isolates, 4 were multi-drug resistant (among which 2 isolates produced VIM-2) while the remaining 15 displayed a wild-type susceptibility phenotype. The CC235 was represented by 8 isolates found in all countries except Senegal. Most of the CC235 isolates (6 out of 8) were resistant to ≥1 β-lactam, to ≥1 aminoglycoside, and to ciprofloxacin, and one Nigerian isolate produced the class A ESBL GES-1. All the ST699 isolates found in the collection of Nigeria, Senegal, and Ivory Coast (n = 7) were susceptible to all the antibiotics tested. The seven ST856 isolates were retrieved in Nigeria. We also found 7 isolates of CC393 coming from Nigeria (n = 6) or Central African Republic (n = 1). Finally, the 5 ST1464 isolates found in Senegal were fully susceptible to all the tested antibiotics.
Population structure of clinical Pseudomonas aeruginosa in West and Central Africa
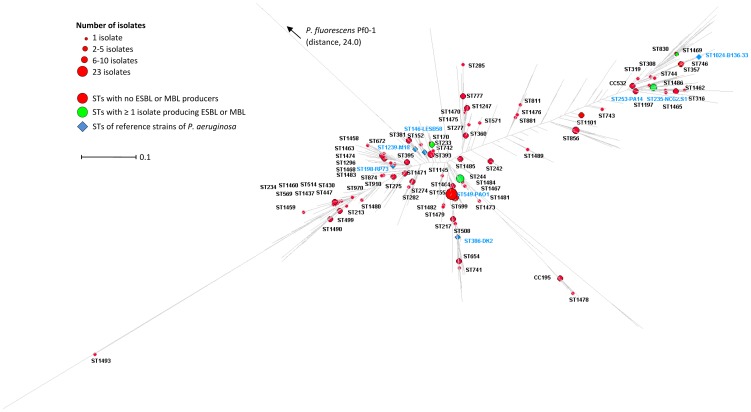
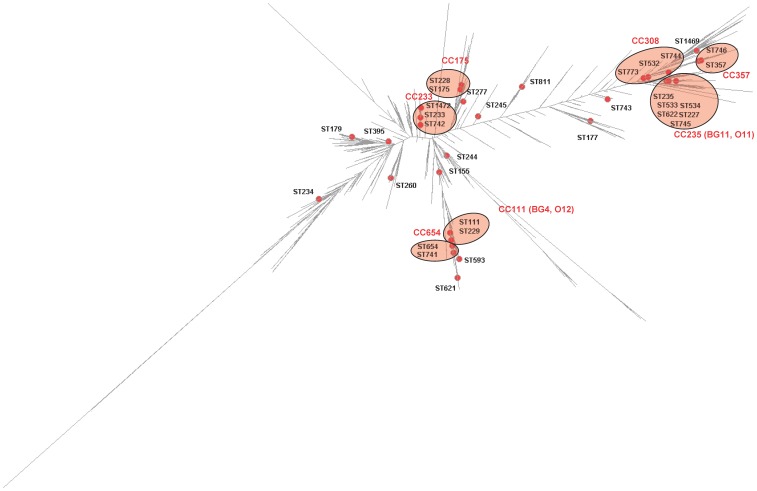
We then spotted the West and Central African P. aeruginosa isolates on the maximum likelihood (ML) tree built from the entire P. aeruginosa PubMLST isolate database (1595 STs described on July 2013) [11]. The ML tree displayed a bush-like structure (Figure 2). Clonal complex is defined as a group of STs in a population that share ≥5 alleles. In the vast majority of the cases, the STs grouped in one CC clustered on the ML tree (Figure 3). For instance, the STs that belong to the CC235 (e.g., ST235, ST533, ST534, ST622, ST227, and ST745) clustered on the ML tree. In two cases, STs from the same CC were scattered throughout the ML tree. Hence, ST743 and ST811 were distant from their respective predicted founders ST233 and ST155 (Figure 3).
Figure 2. Distribution of the STs and CCs of the 184 clinical isolates of Pseudomonas aeruginosa isolated in West and Central Africa on a dendrogram built with the data all known STs (n = 1595).
STs without any isolates producing ESBL or MBL were represented with red spots. STs represented by ≥1 isolate producing ESBL or MBL were represented with green spots. STs of reference isolates are represented with blue diamonds. The dendrogram is based on the alignment of the concatenated sequences of the acsA, aroE, guaA, mutL, nuoD, ppsA and trpE genes (forming an artificial 2,882-bp sequence) of the 1595 STs of the P. aeruginosa MLST database in July 2013 [11]. See Material and methods section for details.
Figure 3. Distribution of the STs and CCs of the Pseudomonas aeruginosa containing isolates producing either extended-spectrum β-lactamase or metallo-β-lactamase defined in the following references [5], [28], [45], [46] on a dendrogram built with the data all known STs (n = 1595).
ESBL- and MBL-producers were represented with red spots. See Figure 2 legend for the tree construction details. Pink zones surround STs that belong to the same clonal complex.
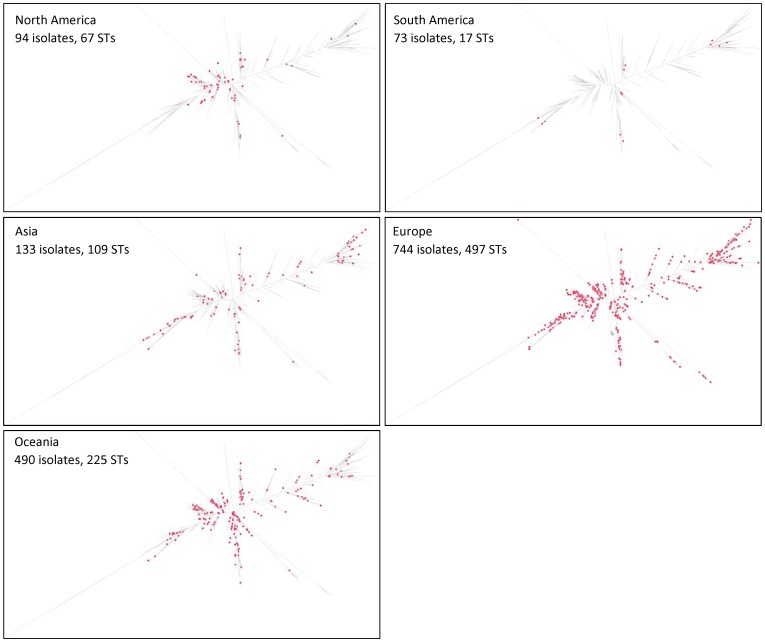
The 80 STs and CCs found in the four African countries (red dots on the Figure 2) were scattered throughout the tree with no particular association with a specific phylogroup. The STs or CCs that included ESBL- or MBL-producers (CC233, CC235, CC244, and ST1469) also were scattered throughout the ML tree (green dots on the Figure 2). We also repeated this experiment with the clinical STs and CCs isolated from the 5 other inhabited continents (Figure 4). Here again, the STs and CCs from a given continent were scattered throughout the global ML tree.
Figure 4. Distribution of the STs of clinical isolates of Pseudomonas aeruginosa on a dendrogram built with the data all known STs (n = 1595), broken down by their continent of origin.
The geographical origin of each ST was extracted from the P. aeruginosa MLST database in July 2013 [11].
Discussion
Here we analyzed the genetic diversity and the population structure of 184 clinical P. aeruginosa isolates found in West and Central Africa and identified the STs that produced β-lactamases with an extended-spectrum (ESBL and MBL). We found that β-lactamases with an extended-spectrum in this region are mostly borne by successful international clonal complexes but also by distinct local STs. Our data also suggest a very limited association between a genotype and a region.
Epidemiology of ESBL- and MBL-producers
VIM-2 was the only carbapenemase found in our collection, confirming that this enzyme is the dominant metallo-β-lactamase over the world and that it is well established in the six populated continents [26]. Here, the bla VIM-2 was borne by the international complexes CC233 (n = 3) and CC244 (n = 2). The presence of VIM-2 has been established in Africa. Hence, a ST1488 isolate harboring bla VIM-2 has been reported in Abidjan (Ivory Coast) [27]. ST1488 belongs to the CC308, already associated with bla MBL [5]. Besides, a CC233 isolate producing VIM-2 has already been described in Norway and associated with repatriation from Ghana [28]. In our collection, the three CC233 isolates (obtained from Nigeria and Ivory Coast) produced VIM-2. This confirms the presence of the VIM-2 enzyme in western African countries of the Gulf of Guinea. The intercontinental CC244 that has been described in Europe, Russia, China, Australia, and Brazil has only been associated with bla PER-1 in Poland [11], [29]. It is worth noting that we found CC244 isolates in the four African countries and that the majority of these isolates (15 out of 19) were fully susceptible to all the antibiotics tested. We also reported the production of an Ambler class A β-lactamase GES-1 in a CC235 isolate in Senegal. CC235 has been identified worldwide, in association with the carbapenemases VIM, IMP, FIM, and NDM [30]. This clonal complex falls into the CC/BURST Group 11 (BG11) with a serotype O11. GES-1-producing CC235 isolates have also been reported in Spain (Figure 3) [31]. Interestingly, all the CC235 isolates reported here (n = 8) were resistant to at least one antibiotic family. Finally, the last ESBL producer was the unrelated ST1469 found in Senegal that carried bla GES-9 (Figure 2). The gene bla GES-9 has only been reported once in an isolate of P. aeruginosa from a patient hospitalized in France [32]. These data indicated that the presence of β-lactamases with an extended-spectrum in West and Central Africa is due to both the presence of successful international clonal complexes (CC233, CC235, and CC244) and that of distinct unrelated STs (ST1469).
Resistance patterns of intercontinental clonal complexes
Many epidemiological studies focused on multidrug-resistant isolates. Consequently, the vast majority of the isolates genotyped with MLST method are representatives of multi-drug resistant and outbreak STs. All microbiologists are encouraged to submit not only new allele sequences but also isolate information from already-known allele to the MLST databases so as it becomes a comprehensive resource for global epidemiology of this species. However, the submission of data for isolates belonging to already-known STs is not the rule. This constitutes one limitation of the databases. The spread of the multidrug-resistant intercontinental STs could be due either to their resistance pattern that favours them when the antibiotic pressure is high or to their intrinsic traits, independently of the antibiotic resistance. A high-level resistance to major anti-pseudomonal agents can be the result of the acquisition of foreign resistance genes such as those encoding carbapenemase or of mutations that trigger chromosomal resistance mechanisms. To the best of our knowledge, the data published so far could hardly answer this question. One strong point of our study is the absence of selection biases of the clinical isolates. Hence, we genotyped every isolate of the collection whatever its resistance phenotype. All the CC233 and CC235 isolates (n = 3 and 8, respectively) that we tested were multidrug-resistant, with the exception of two isolates resistant only to carboxypenicillins. Cabot et al. confirmed the absence of these clonal complexes in a collection of multi-susceptible clinical isolates in Spain [33]. In contrast, all the isolates belonging to CC155 (n = 23), CC195 (n = 4), CC395 (n = 3) were fully susceptible to all the antipseudomonal compounds tested. However, CC155 associated with bla VIM-2 has been reported in Spain, and multi-drug resistant CC395 was countrywide-distributed in Hungary or epidemic in a French University Hospital [34], [35].
CC244 isolates that carry bla PER-1 or bla VEB-1 have been reported in Poland and in Bulgaria [29], [36]. We also found, in our collection, isolates producing the VIM-2 carbapenemase (n = 2) even though most of the isolates of this clonal complex (15 out of 19) displayed a fully susceptible profile. Similarly, although the CC274 was also identified within multidrug-resistant isolates circulating in Spain [37], we found that the majority of the representatives of this clonal complex in our collection were of wild-type susceptibility pattern.
Beside intercontinental clonal complexes, we observed the spread of fully susceptible STs in West and Central African countries. Hence, seven ST699 isolates were found in Ivory Coast, Nigeria, or Senegal and four ST1464 isolates were found in Senegal. Altogether, these data could suggest that the spread of a ST among patients can be the result either (i) to its antibiotic resistance (e.g., CC235 and CC233) or (ii) to features independent from the resistance to antibiotics (e.g., CC155, CC244, CC195, CC274, and CC395). These latter features could favour human infection or colonisation directly with a better adaptation to the host (e.g. through a better adhesion to eukaryotic cells, higher biofilm formation and virulence), or indirectly with a higher frequency in environmental settings. Further studies are needed to clarify this point.
Population structure of and acquisition of extended-spectrum β-lactamases by P. aeruginosa
We sought to determine whether the STs of clinical isolates of P. aeruginosa found in the West and Central Africa clustered on the global dendrogram of the 1595 currently defined STs (Figure 2). The analysis of MLST data relies on two strategies: allele- or nucleotide-based methods. The former is fast, simple, and very popular, but cannot distinguish between single-based changes in multiple loci versus multiple mutations in the same loci. It therefore disregards much of the evolutionary information contained at the nucleotide level. Nucleotide-based methods are more accurate and robust but require bioinformatics computer skills [38]. Figure 2 represents the ML tree produced by the alignment of the concatenated gene sequences of the currently known STs. Its bush-like structure confirmed that P. aeruginosa has a non-clonal structure [6]–[10]. The Figure 2 clearly shows the absence of any population substructures, confirming that P. aeruginosa evolves as a single cohesive genetic group. This, together with the large distance between the tree root and the representative of the close species P. fluorescens Pf0-1 taken as outgroup confirmed that P. aeruginosa conformed to a clear, compact, and well defined species [39].
As the 80 STs identified our isolates were scattered throughout the ML tree, they were highly representative of the global P. aeruginosa population. This suggests no evidence of STs or clades specific to a region. We also spotted on the global ML tree the STs found on the five other inhabited continents (Figure 4) [11]. Although the number of STs submitted by continent is uneven (e.g., 497 in Europe and 17 in South America), it also suggests the poor association between a phylogroup and a continent. Using other methods (eBURST and calculation of genetic diversity index), Kidd et al. also showed no significant difference between the genetic diversity of STs found in Queensland (Australia) and the global P. aeruginosa ST dataset [10], [11].
Standard phylogenetic methods assume a lack of recombination defined as the exchange of genetic information between two nucleotide sequences. Although the recombination plays a major role in the evolutionary history of P. aeruginosa genome, the housekeeping genes used for MLST are presumably not subjected to these mutational events [40]. However, the phylogenetic tree based on these data should be analyzed with caution. In addition, MLST loci such as acs, guaA and mutL underlie a high mutation rate, particularly in isolates associated with chronic infection such as cystic fibrosis [41]–[43]. Consequently, it is likely that the genetic diversity of the species is lower than that calculated from the MLST data.
Genetic diversity of P. aeruginosa producing β-lactamases with an extended-spectrum
Although bla MBL or bla ESBL genes can be borne by many STs over the world, some successful international clonal complexes are frequently multidrug-resistant and their representatives are more prone to produce ESBLs and MBLs [5]. Members of these epidemic lineages have a serotype O11 and O12. The O12 and O11 lineages fall into the P. aeruginosa CC/BURST Group 4 (BG4) and BG11 and embrace STs that cluster tightly in the ML tree (Figure 3). We confirm here that MBL and ESBL-encoding genes are mostly borne by successful international CC233, CC235, and CC244 as previously observed in other countries [28], [30], [44]. The graphical representation on the global ML tree of all the STs defined so far as potential MBL- or ESBL-producers suggested that the acquisition of this resistance enzyme has a very limited association with a genotype [5], [28], [45], [46](Figure 3).
In conclusion, we found that the resistance rates of clinical isolates to antibiotics remained low in Senegal and Central African Republic. This contrasts with the much higher resistance rate of clinical isolates from Ivory Coast and Nigeria. Our data showed that, in P. aeruginosa, the β-lactamases with an extended-spectrum in West and Central Africa are mostly borne by successful international clonal complexes but also by local distinct STs. We suggest that the spread of a ST can be the result either to its antibiotic resistance or to features independent from the resistance to antibiotics.
Supporting Information
Country of origin, sequence type and antibiotic resistance profile of the 184 clinical isolates of P. aeruginosa.
(XLS)
Acknowledgments
We thank Patrick Plésiat from the National Center of Resistance to Antibiotics for the identification of β-lactamase with extended-spectrum and Laurence Rousseaux for her technical support. We also thank Fabrice Poncet from the sequencing facility of the SFR FED 4234 (University of Franche-Comté, Besançon). This publication made use of the Pseudomonas aeruginosa MLST website (http://pubmlst.org/paeruginosa/) developed by Keith Jolley and sited at the University of Oxford [47]. The development of this site has been funded by the Wellcome Trust.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
PC, MT, XB and XB were granted by the University Hospital of Besançon (Délégation à la Recherche Clinique et l'Innovation, Commission des Examens de Laboratoire et d'Innovation Analytique, project P. aeruginosa in Sub-Saharan Africa 2012). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lyczak JB, Cannon CL, Pier GB (2000) Establishment of Pseudomonas aeruginosa infection: lessons from a versatile opportunist. Microbes Infect 2: 1051–1060. [DOI] [PubMed] [Google Scholar]
- 2. Mesaros N, Nordmann P, Plésiat P, Roussel-Delvallez M, Van Eldere J, et al. (2007) Pseudomonas aeruginosa: resistance and therapeutic options at the turn of the new millennium. Clin Microbiol Infect 13: 560–578. [DOI] [PubMed] [Google Scholar]
- 3. Breidenstein EBM, de la Fuente-Núñez C, Hancock REW (2011) Pseudomonas aeruginosa: all roads lead to resistance. Trends Microbiol 19: 419–426. [DOI] [PubMed] [Google Scholar]
- 4. Poole K (2011) Pseudomonas aeruginosa: resistance to the max. Front Microbiol 2: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Woodford N, Turton JF, Livermore DM (2011) Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol Rev 35: 736–755. [DOI] [PubMed] [Google Scholar]
- 6. Wiehlmann L, Wagner G, Cramer N, Siebert B, Gudowius P, et al. (2007) Population structure of Pseudomonas aeruginosa . Proc Natl Acad Sci U S A 104: 8101–8106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Curran B, Jonas D, Grundmann H, Pitt T, Dowson CG (2004) Development of a multilocus sequence typing scheme for the opportunistic pathogen Pseudomonas aeruginosa . J Clin Microbiol 42: 5644–5649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maatallah M, Cheriaa J, Backhrouf A, Iversen A, Grundmann H, et al. (2011) Population structure of Pseudomonas aeruginosa from five Mediterranean countries: evidence for frequent recombination and epidemic occurrence of CC235. PLoS One 6: e25617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pirnay JP, Bilocq F, Pot B, Cornelis P, Zizi M, et al. (2009) Pseudomonas aeruginosa population structure revisited. PLoS One 4: e7740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kidd TJ, Ritchie SR, Ramsay KA, Grimwood K, Bell SC, et al. (2012) Pseudomonas aeruginosa exhibits frequent recombination, but only a limited association between genotype and ecological setting. PLoS One 7: e44199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.University of Oxford, Pseudomonas aeruginosa MLST database. http://pubmlst.org/paeruginosa. Accessed July 1st, 2013.
- 12. Wieser A, Schneider L, Jung J, Schubert S (2012) MALDI-TOF MS in microbiological diagnostics—identification of microorganisms and beyond. Appl Microbiol Biotechnol 93: 965–974. [DOI] [PubMed] [Google Scholar]
- 13.European Committee on Antimicrobial Susceptibility Testing, Clinical breakpoints - bacteria (v 4.0). www.eucast.com. Accessed 2014 May 30.
- 14. Hocquet D, Dehecq B, Bertrand X, Plésiat P (2011) Strain-tailored double-disk synergy test detects extended-spectrum oxacillinases in Pseudomonas aeruginosa . J Clin Microbiol 49: 2262–2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hocquet D, Plésiat P, Dehecq B, Mariotte P, Talon D, et al. (2010) Nationwide investigation of extended-spectrum β-lactamases, metallo-β-lactamases and extended-spectrum oxacillinases produced by ceftazidime-resistant Pseudomonas aeruginosa in France. Antimicrob Agents Chemother 54: 3512–3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Talon D, Cailleaux V, Thouverez M, Michel-Briand Y (1996) Discriminatory power and usefulness of pulsed-field gel electrophoresis in epidemiological studies of Pseudomonas aeruginosa . J Hosp Infect 32: 135–145. [DOI] [PubMed] [Google Scholar]
- 17. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, et al. (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33: 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van Mansfeld R, Willems R, Brimicombe R, Heijerman H, van Berkhout FT, et al. (2009) Pseudomonas aeruginosa genotype prevalence in Dutch cystic fibrosis patients and age dependency of colonization by various P. aeruginosa sequence types. J Clin Microbiol 47: 4096–4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jolley KA, Feil EJ, Chan MS, Maiden MC (2001) Sequence type analysis and recombinational tests (START). Bioinformatics 17: 1230–1231. [DOI] [PubMed] [Google Scholar]
- 20. Posada D (2008) jModelTest: Phylogenetic model averaging. Mol Biol Evol 25: 1253–1256. [DOI] [PubMed] [Google Scholar]
- 21. Deflaun MF, Tanzer AS, McAteer AL, Marshall B, Levy SB (1990) Development of an adhesion assay and characterization of an adhesion-deficient mutant of Pseudomonas fluorescens . Appl Environ Microbiol 56: 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stamatakis A (2006) RAxML-VI-HPC: maximum likelihood-based phylogenetic analyses with thousands of taxa and mixed models. Bioinformatics 22: 2688–2690. [DOI] [PubMed] [Google Scholar]
- 23. Huson DH, Scornavacca C (2012) Dendroscope 3: An interactive tool for rooted phylogenetic trees and networks. Syst Biol 61: 1061–1067. [DOI] [PubMed] [Google Scholar]
- 24. Fournier D, Richardot C, Müller E, Robert-Nicoud M, Llanes C, et al. (2013) Complexity of resistance mechanisms to imipenem in intensive care unit strains of Pseudomonas aeruginosa . J Antimicrob Chemother 68: 1772–1780. [DOI] [PubMed] [Google Scholar]
- 25. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18: 268–281. [DOI] [PubMed] [Google Scholar]
- 26. Walsh TR (2010) Emerging carbapenemases: a global perspective. Int J Antimicrob Agents 36 Suppl 3 S8–14. [DOI] [PubMed] [Google Scholar]
- 27. Jeannot K, Guessennd N, Fournier D, Muller E, Gbonon V, et al. (2013) Outbreak of metallo- β-lactamase VIM-2-positive strains of Pseudomonas aeruginosa in the Ivory Coast. J Antimicrob Chemother 68: 2952–2954. [DOI] [PubMed] [Google Scholar]
- 28. Samuelsen Ø, Toleman MA, Sundsfjord A, Rydberg J, Leegaard TM, et al. (2010) Molecular epidemiology of metallo-β-lactamase-producing Pseudomonas aeruginosa isolates from Norway and Sweden shows import of international clones and local clonal expansion. Antimicrob Agents Chemother 54: 346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Empel J, Filczak K, Mrowka A, Hryniewicz W, Livermore DM, et al. (2007) Outbreak of Pseudomonas aeruginosa infections with PER-1 extended-spectrum β-lactamase in Warsaw, Poland: Further evidence for an international clonal complex. J Clin Microbiol 45: 2829–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Edelstein MV, Skleenova EN, Shevchenko OV, D'Souza JW, Tapalski DV, et al. (2013) Spread of extensively resistant VIM-2-positive ST235 Pseudomonas aeruginosa in Belarus, Kazakhstan, and Russia: a longitudinal epidemiological and clinical study. Lancet Infect Dis 13: 867–876. [DOI] [PubMed] [Google Scholar]
- 31. Viedma E, Juan C, Acosta J, Zamorano L, Otero JR, et al. (2009) Nosocomial spread of colistin-only-sensitive sequence type 235 Pseudomonas aeruginosa isolates producing the extended-spectrum β-Lactamases GES-1 and GES-5 in Spain. Antimicrob Agents Chemother 53: 4930–4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Poirel L, Brinas L, Fortineau N, Nordmann P (2005) Integron-encoded GES-type extended-spectrum β-lactamase with increased activity toward aztreonam in Pseudomonas aeruginosa . Antimicrob Agents Chemother 49: 3593–3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cabot G, Ocampo-Sosa AA, Dominguez MA, Gago JF, Juan C, et al. (2012) Genetic markers of widespread extensively drug-resistant Pseudomonas aeruginosa high-risk clones. Antimicrob Agents Chemother 56: 6349–6357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Libisch B, Balogh B, Füzi M (2009) Identification of two multidrug-resistant Pseudomonas aeruginosa clonal lineages with a countrywide distribution in Hungary. Curr Microbiol 58: 111–116. [DOI] [PubMed] [Google Scholar]
- 35. Hocquet D, Bertrand X, Köhler T, Talon D, Plésiat P (2003) Genetic and phenotypic variations of a resistant Pseudomonas aeruginosa epidemic clone. Antimicrob Agents Chemother 47: 1887–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vatcheva-Dobrevska R, Mulet X, Ivanov I, Zamorano L, Dobreva E, et al. (2013) Molecular epidemiology and multidrug resistance mechanisms of Pseudomonas aeruginosa isolates from Bulgarian hospitals. Microb Drug Resist 19: 355–361. [DOI] [PubMed] [Google Scholar]
- 37. Garcia-Castillo M, Del Campo R, Morosini MI, Riera E, Cabot G, et al. (2011) Wide dispersion of ST175 clone despite high genetic diversity of carbapenem-nonsusceptible Pseudomonas aeruginosa clinical strains in 16 Spanish hospitals. J Clin Microbiol 49: 2905–2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Perez-Losada M, Cabezas P, Castro-Nallar E, Crandall KA (2013) Pathogen typing in the genomics era: MLST and the future of molecular epidemiology. Infect Genet Evol 16: 38–53. [DOI] [PubMed] [Google Scholar]
- 39. Mulet M, Lalucat J, García-Valdés E (2010) DNA sequence-based analysis of the Pseudomonas species. Environ Microbiol 12: 1513–1530. [DOI] [PubMed] [Google Scholar]
- 40. Kung VL, Ozer EA, Hauser AR (2010) The accessory genome of Pseudomonas aeruginosa . Microbiol Mol Biol Rev 74: 621–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fernández-Olmos A, García-Castillo M, Alba JM, Morosini MI, Lamas A, et al. (2013) Population structure and antimicrobial susceptibility of both nonpersistent and persistent Pseudomonas aeruginosa isolates recovered from cystic fibrosis patients. J Clin Microbiol 51: 2761–2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. López-Causapé C, Rojo-Molinero E, Mulet X, Cabot G, Moyà B, et al. (2013) Clonal dissemination, emergence of mutator lineages and antibiotic resistance evolution in Pseudomonas aeruginosa cystic fibrosis chronic lung infection. PLoS One 8: e71001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. García-Castillo M, Máiz L, Morosini M-I, Rodríguez-Baños M, Suarez L, et al. (2012) Emergence of a mutL mutation causing multilocus sequence typing–pulsed-field gel electrophoresis discrepancy among Pseudomonas aeruginosa isolates from a cystic fibrosis patient. J Clin Microbiol 50: 1777–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cholley P, Thouverez M, Hocquet D, van der Mee-Marquet N, Talon D, et al. (2011) Most multidrug-resistant Pseudomonas aeruginosa isolates from hospitals in eastern France belong to a few clonal types. J Clin Microbiol 49: 2578–2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Santella G, Pollini S, Docquier JD, Mereuta AI, Gutkind G, et al. (2010) Intercontinental dissemination of IMP-13-producing Pseudomonas aeruginosa belonging in sequence type 621. J Clin Microbiol 48: 4342–4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pournaras S, Köck R, Mossialos D, Mellmann A, Sakellaris V, et al. (2013) Detection of a phylogenetically distinct IMP-type metallo-β-lactamase, IMP-35, in a CC235 Pseudomonas aeruginosa from the Dutch–German border region (Euregio). J Antimicrob Chemother 68: 1271–1276. [DOI] [PubMed] [Google Scholar]
- 47. Jolley K, Maiden M (2010) BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinformatics 11: 595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Country of origin, sequence type and antibiotic resistance profile of the 184 clinical isolates of P. aeruginosa.
(XLS)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.