Abstract
BACKGROUND
Achalasia is the most recognized motor disorder of the esophagus. Because it is an uncommon disease, most studies have reviewed small numbers of patients. Here, we report demographic, clinical features and treatment outcomes in 700 achalasia patients.
METHODS
In all patients, diagnosis was established based on clinical, radiological, endoscopic and manometric criteria. A questionnaire was completed for each patient and included the patient’s age, gender, initial symptoms, frequency of different symptoms, presence of positive family history for achalasia, other accompanying diseases and treatment outcomes.
RESULTS
In our study men were affected more than women (54.3% vs. 45.7%). Patients’ mean age was about 38 years. The most frequent symptoms noted were: dysphagia to solids and liquids, active regurgitation, passive regurgitation and weight loss, respectively. Women complained of chest pain more than men (59% vs. 47.1%, p=0.04). The vast majority of our patients were treated by pneumatic dilation (PD) of the LES and in long-term follow-up, 67% were in the responder group. Females responded better than males to PD.
CONCLUSION
Dysphagia to solids is the most common symptom in patients with achalasia. Chest pain was significantly higher among women. PD is an effective treatment for achalasia with long-term efficacy in the majority of patients.
Keywords: Dysphagia, Achalasia, Pneumatic Dilation
INTRODUCTION
Achalasia is a Greek word that means “does not relax” and is the most recognized motor disorder of the esophagus. Diagnosis of achalasia is made by clinical features plus radiographic, endoscopic and manometric findings.1,2 To date, several studies have reviewed demographic and clinical features of achalasia patients but none had large sample sizes.
The etiologies of idiopathic achalasia are still unclear but measles, genetic influences, varicella zoster virus, disorders of the immune system and autoimmunity might be probable causes.3-5
Achalasia may occur at any age but it mostly presents between third and sixth decades of life. It seems the most recognized pathologic feature of this disease is reduction of non-adrenergic, non-cholinergic inhibitory ganglion cells.1,5,6
As our center (Digestive Disease Research Center, Shariati Hospital, Tehran University of Medical Sciences) is a referral center in Iran, particularly for achalasia, we decided to gather and publish demographic, clinical features and treatment outcomes of our patients from 1994- 2009.
MATERIALS AND METHODS
In this study, 700 patients with achalasia who were referred to our center between 1994-2009 were evaluated with regards to their demographic, clinical features and treatment outcomes. Patients’ symptoms were scored according to Iranian scoring for achalasia (Table 1).
Table 1 . Iranian standardized scoring for achalasia.
| Symptom | 0 | 1 | 2 | 3 |
| Dysphagia to solids | None | Occasionally | Daily | Each meal |
| Dysphagia to liquids | None | Occasionally | Daily | Each meal |
| Active regurgitation | None | Occasionally | Daily | Each meal |
| Passive regurgitation | None | Rerely | Weekly | Daily |
| Chest pain | None | Rerely | Weekly | Daily |
A questionnaire was completed for each patient and included name, age, gender, phone, presenting symptoms, duration of symptoms, frequency of all symptoms, family history, medical history, symptoms scores, aggravating and alleviating factors, treatment obtained and follow up. Patients were followed for a mean period of 23.3 months (SD±28.4) and responses to treatment were evaluated according to the Vantrapen scoring system (Table 2).7
Table 2 . Vantrapen scoring system.* .
| Excellent: Completely free of symptoms |
| Good: Occasional (less than once a week) dysphagia or pain of short duration defined as retrosternal hesitation of food lasting from 2-3 s to 2-3 min and disappearing after drinking fluids. |
| Moderate: Dysphagia more than once a week lasting less than 2-3 min and not accompanied by regurgitation and weight loss. |
| Poor: Dysphagia more than once a week or lasting 2-3 min or longer or accompanied by regurgitation and weight loss. |
*Excellent and good were considered as responders to treatment.
Patients’ demographic, clinical features and response to treatment were analyzed by SPSS software (version 16, Chicago, IL, USA) Chi-Square and Independent t-test. Mean, median, minimum and maximum parameters were calculated.
RESULTS
In this study, men (n=380, 54.3%) were affected more than women (n=320, 45.7%), respectively. The mean age of our patients was 38 years. Approximately 60% (420) were between the ages of 21-50 years. The mean LES pressure before treatment was 44.2 mmHg. Initial symptoms in the patients were as follows: dysphagia to solids (79.7%), dysphagia to liquids (54.4%), active regurgitation (22.9%), passive regurgitation (20.9%) and chest pain (11.9%)(Figure 1).
Figure 1 .
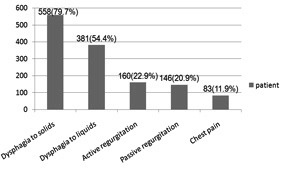
Initial achalasia symptoms
The mean duration of symptoms before diagnosis was 4.9 years, with a range of 1- 15 years. The frequency of symptoms amongst patients was: dysphagia to solids (97.3%), dysphagia to liquids (87%), active regurgitation (68%), passive regurgitation (67.7%), weight loss (64.3%), chest pain (52.9%), nocturnal cough (44.4%) and nocturnal dyspnea (18.3%) (Figure 2).
Figure 2 .
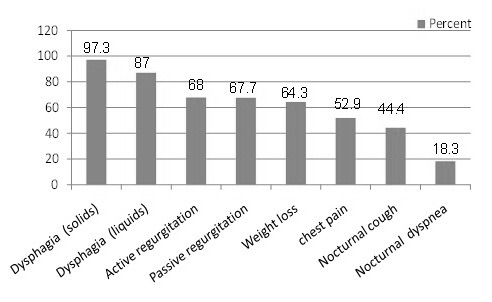
Frequency of achalasia symptoms
Aggravating and alleviating factors of dysphagia are listed Tables 3 and 4, respectively. Other less frequent symptoms were globus sensation in ten patients (1.4%), hiccups (two patients, 0.28%) and heartburn (two patients, 0.28%). Mean weight loss was 3.9 kg (range: 0-30 kg; SD±5.6) with a weight loss of 10 kg or more during six months seen in 52 patients (7.4%). In our study, chest pain was the only symptom significantly higher among women (59.7% vs. 47.1%, p=0.04). Also, patients older than 56 years complained of chest pain less often than those younger (p=0.05).
Table 3 . Aggravating factors of dysphagia.
| Aggravating factors | |
| Only during Stressful eating | 5.7% |
| Only during Hurried eating | 18.1% |
| Both during stressful and Hurried eating | 52.7% |
Table 4 . Alleviating factors of dysphagia.
| Alleviating factors | |
| Water drinking | 59% |
| Back straightening | 43% |
| Standing &walking | 28% |
| Deep breathing | 11% |
| Massage on sternum | 9% |
| Valsalva manuever | 9% |
In our study there were 21 patients with positive family histories for achalasia (3%). Interestingly, there was one case (female) with achalasia in her mother and son, one case (male) with achalasia in all his siblings and one case (male) with achalasia in his mother and his brother.
In our study there were six cases (0.85%) of triple A syndrome (achalasia, alacrimia and adrenal insufficiency), three of whom were males. Their mean age was 12 years. Additionally, there were three cases (two females and one male, 0.42%) of double A syndrome (achalasia and alacrimia) with mean age of 16 years.
Other accompanying diseases according to passive data collection and symptom-based evaluation include the following: hypothyroidism (seven females and three males), hyperthyroidism (one female), panhypopituitarism (one male), intestinal pseudo-obstruction (one male and one female), Hodgkins lymphoma (one male), Down Syndrome (one male) and SLE (one female) (Table 5). Patients, scored according to Table 1, had a mean total symptom score prior to treatment of 8.8 (SD±3).
Table 5 . Accompanying diseases in achalasia.
| Disease | Frequency (%) |
| Hypothyroidism | 0.7 |
| Intestinal pseudo-obstruction | 0.14 |
| Panhypopitutarism | 0.07 |
| Hyperthyroidism | 0.07 |
| Hodgkins lymphoma | 0.07 |
| Down syndrome | 0.07 |
| SLE* | 0.07 |
SLE* = Systemic lupus erythematosus
Of the 700 patients, 670 cases were treated by pneumatic dilation (PD) and the remaining 30 were treated with botulinum toxin (BT) according to the following criteria including: Presence of sigmoid esophagus, presence of epiphrenic diverticula, patient’s preference and older patients with cardiopulmonary disorders who were at high risk for emergency surgery in case of perforation.
Of 670 patients who were treated with PD, 188 (20.9%) received PD twice, 34 (3.8%) for three times, 8 (0.8%) for four times and one patient received five treatments. A balloon size of 30 mm was used in 578 (71.6%) patients, sizes 30 and 35 mm in 199 (24.7%) and sizes 35 & 40 mm in 3.7% of patients. Out of 670 patients treated with PD, 412 were followed. A total of 258 patients were lost to follow up due to various reasons such as changes in address or phone numbers. The mean period of follow up was 23.3 months (SD±28.4) with a minimum of 6 months and a maximum of 156 months. There were three perforations in our first 100 patients. Two of these healed spontaneously, but one required surgery.
After initiation of therapy with graded PD (use of No. 3 balloons for all patients initially, and then gradually increasing the balloon size, if needed), no other cases of perforation were noted.
According to the Vantrapen scoring system, our patients were classified into four groups: excellent (32%), good (35%), moderate (24%) and poor (9%). Patients who were placed in the excellent and good groups were considered as responders to treatment (67%). The responders underwent PD once in 37% of patients, twice times in 56% and three times in 7% of the patients.
According to the Iranian scoring for achalasia, the mean total symptom scores before and after treatment were 8.8 (SD±3) and 5.1(SD±3.8), respectively. Additionally, in our study, females responded better to PD than males (69% vs. 31%). Using the chi-square test, there was a significant relation between gender and response to PD (p<0.04). There was also a relation between total symptom score and response to treatment. Patients with lower scores before treatment responded better to PD. Although chest pain decreased significantly after treatment in both groups (p<0.001), it was still higher among women (34% vs. 21.9%, p=0.04). The mean pretreatment total symptom score was 8.55 in responders and 9 in nonresponders.
DISCUSSION
Achalasia sometimes affects more than one family member.8,9 These familial cases exist among fathers, mothers, siblings, ancestors and even children. In our study there were 21 patients with positive family histories for achalasia (3%). Alacrimia and adrenal insufficiency are sometimes concomitant with achalasia.10,11
In our study there were six cases (0.85%) of triple A syndrome (achalasia, alacrimia and adrenal insufficiency), three of whom were males.
The major clinical and demographic features of achalasia in Iran are similar to reports from other parts of the world.12 In contrast to some reports,13 in our study achalasia was more common among men and chest pain was reported more frequently by women (59.7% vs. 47.1%, p=0.04). These results compare with another study from Iran.14 In other studies, chest pain has been reported to be more common among younger patients.15 Its cause remains unknown and no treatment is reported to effectively relieve this symptom. However, with advancing age the frequency of chest pain diminishes in most patients.15,16
Additionally, the presence of familial cases and accompanying disorders are interesting and subject to additional investigation. In comparison to other articles, the numbers of studied cases in our center was significantly higher than previously reported, thus it would be valuable to compare our results with others.
We have also reported on accompanying diseases such as thyroid dysfunction, Downs syndrome, and triple A syndrome, to name a few. There have been some studies and case reports that have also reported on concomitant diseases17-21which is also a subject for additional investigation.
Dysphagia to solids and liquids were the most common symptoms in our patients (97.3% and 87%, respectively). Dysphagia has been the most common complaint of patients in other studies worldwide,1,6,12,13 but the prevalence of chest pain in other studies was not the same.12,15,16 In contrast to our study and other reports, achalasia has been more common in females in a study by Degli.22
As mentioned above, a large portion of our patients were treated by PD, and as measured by the Vantrapen scoring system, nearly 67% of treated patients were excellent and good responders to PD (32% excellent, 35% good). In a similar study of 227 patients, 51.8 % and 21.6% of patients had excellent and good therapeutic outcomes after PD, respectively.23
Another recent study reported excellent (19%), very good (26%) and good (35%) responses to PD in patients, respectively, for long term outcomes of PD in the treatment of achalasia.24 In a Turkish study on 111 patients, therapeutic outcomes were excellent in 48% (54 patients), and good in 34% (38 patients).22
In all of the represented studies, excellent and good responses to PD were considered successful.
It seems PD is a good treatment option, particularly in patients unwilling to undergo surgery.25,26
Also, our group found that the injection of BT before PD did not significantly enhance the efficacy of PD.27 In a recently published report 28 it has been stated that even though open myotomy and PD are both associated with symptom improvement, when considering other factors such as shorter hospitalization, time off from work, the risks of general anesthesia, probability of clinical relapse and cosmetic sequels into consideration, it seems that PD is preferable for the majority of patients. In this report it has been suggested that the choice between PD and myotomy as initial therapy for achalasia should be based on the patient’s preferences and on the experience of the personnel available. In two other studies,11, 29 it has been concluded that even though laparoscopic myotomy with fundoplication is the most effective treatment for achalasia, the initial cost of myotomy is usually higher and the recovery period, particularly following open myotomy, is generally longer. Thus when myotomy is not possible for any reason, e.g., medical contraindication, patient unwillingness, inability to afford surgery, or experienced centers for surgery or post-operative care are not easily accessible, therefore graded PD (using 3.0 cm balloons initially) with a slow rate of balloon inflation seems to be an effective and safe initial alternative.
Clinical and demographic findings are nearly the same among different studies. Our study determined that chest pain may be more common in women. Factors such as gender and pretreatment symptom score may also affect the response rate to PD. Thus, according to this study, PD is an effective long-term therapy for achalasia.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
REFERENCES
- 1.Francis DL, Katza DA. Achalasia: Update on the disease and its treatment. Gastroenterology. 2010;139:369–74. doi: 10.1053/j.gastro.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 2.El-Takli I, OBrien P, Paterson WG. Clinical diagnsis of achalasia: How reliable is the barium x-Ray? Can J Gasroenterol. 2006;20:335–7. doi: 10.1155/2006/193823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birgisson S, Galinski MS, Ggoldblum JR, Rice TW, Richte JE. Achalasia is not associated with virus. Dig Dis Sci. 1997;42:300–6. doi: 10.1023/a:1018805600276. [DOI] [PubMed] [Google Scholar]
- 4.Robertson CS, Martin BAB, Atkinson M. Varicella-zoster virus DNA in the oesophageal myenteric plexus in achalasia. Gut. 1993;34:299–302. doi: 10.1136/gut.34.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moses PL, Ellis LM, Anees MR, Ho W, Rothstein RI, Meddings JB. et al. Antineuronal antibodies in idiopathic achalasia and gastro-oesophageal reflux disease. Gut. 2003;52:629–36. doi: 10.1136/gut.52.5.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG. Clinical, radiological, and manometric profile in 145 patients with untreated achalasia. World J Surg. 2008;32:1974–9. doi: 10.1007/s00268-008-9656-z. [DOI] [PubMed] [Google Scholar]
- 7.Vantrapen G, Hellemans H. Treatment of achalasia and related motor disorders. Gastroenterology. 1979;76:450–7. [PubMed] [Google Scholar]
- 8.Frieling T, Berges W, Borchard F, Lübke HJ, Enck P, Wienbeck M. Family occurrence of achalasia and diffuse spasm of the esophagus. Gut. 1998;29:1595–602. doi: 10.1136/gut.29.11.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Achkar E. Diseases associated with or mimicking achalasia. Gastrointest Endosc Clin N Am. 2001;11:267–80. [PubMed] [Google Scholar]
- 10.Verma S, Brown S, Dakkak M, Bennett JR. Association of adult achalasia and alacrima. Dig Dis Sci. 1999;44:876–8. doi: 10.1023/a:1026679723941. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura K, Yoshida K, Yoshinaga T, Kodaira M, Shimojima Y, Takei Y. et al. Adult or late-onset triple A Syndrome, case report and literature review. J Neurol Sci. 2010;297:85–8. doi: 10.1016/j.jns.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Mikaeli J, Islami F, Malekzadeh R. Achalasia: A review of Western and Iranian experiences. World J Gastroentrol. 2009;15:5000–9. doi: 10.3748/wjg.15.5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut. 1992;33:1011–5. doi: 10.1136/gut.33.8.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikaeli J, Farrokhi F, Bishehsari F, Mahdavinia M, Malekzadeh R. Gender effect on clinical features of achalasia: a prospective study. BMC Gastroenterol. 2006;6:12. doi: 10.1186/1471-230X-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eckardt VF, Stauf B, Bernhard G. Chest pain in achalasia: patient characteristics and clinical course. Gastroenterology. 1999;116:1300–4. doi: 10.1016/s0016-5085(99)70493-2. [DOI] [PubMed] [Google Scholar]
- 16.Spechler SJ, Souza RF, Rosenberg SJ, Ruben RA, Goyal RK. Heartburn in patients with achalasia. Gut. 1995;37:305–8. doi: 10.1136/gut.37.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kroupa R, Starý K, Hep A, Suchánková J, Dolina J. Higher incidence of thyropathy in patients with esophageal achalasia, genetic, autoimmune, regional or just a random association? Vnitr lek. 2008;54:341–5. [PubMed] [Google Scholar]
- 18.Emami M, Raisi M, Amini J, Daghaghzadeh H. Achalasia and thyroid disease. World J Gasteroentrol. 2007;13:594–9. doi: 10.3748/wjg.v13.i4.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ang D, Teo EK, Ang TL, Lim KH, Madhukumar P, Chung AY. et al. Unexplained small-bowel obstruction in a patient with presumptive achalasia: need for early recognition of chronic intestinal pseudo-obstruction (CIPO) Dig Dis Sci. 2010;55:2691–2. doi: 10.1007/s10620-009-1048-1. [DOI] [PubMed] [Google Scholar]
- 20.Chen GC, Cheng DW, Enayati PJ, Chen G, Conklin JL, Soffer EE. et al. Concurrent findings of achalasia and duodenal duplication in a Down syndrome patient. J Formos Med Assoc. 2009;108:78–81. doi: 10.1016/S0929-6646(09)60036-X. [DOI] [PubMed] [Google Scholar]
- 21.Mayberry JF, Atkinson M. Achalasia and other diseases associated with disorders of gastrointestinal motility. Hepatogastroentrology. 1986;33:206–7. [PubMed] [Google Scholar]
- 22.Degli U, Kuran S, Savas N, Ozin Y, Alkim C, Atalay F. et al. Factors predicting outcome of baloon dilation in achalasia. Dig Dis Sci. 2009;54:1237–1242. doi: 10.1007/s10620-008-0493-6. [DOI] [PubMed] [Google Scholar]
- 23.Chuah SK, Hu TH Wu KL, Hsu PI, Tai WC, Chiu YC. et al. Clinical remission in endoscope-guided pneumatic dilation for the treatment of esophageal achalasia: 7-year follow-up results of prospective investigation. J Gastrointest Surg. 2009;13:862–7. doi: 10.1007/s11605-009-0804-z. [DOI] [PubMed] [Google Scholar]
- 24.Hulselmans M, Vanuytsel T, Degreef T, Sifrim D, Coosemans W, Lerut T. et al. Long term outcome of pneumatic dilation in treatment of achalasia. Clin Gastroenterol Hepatol. 2010;8:30–5. doi: 10.1016/j.cgh.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 25.Katsinelos P, Ouras JK, Paroutoglou G. Long term results of pneumatic dilation. World J Gastroenterol. 2005;11:5701–5. doi: 10.3748/wjg.v11.i36.5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mikaeli J, Fazel A, Montazeri G, Yaghoobi M, Malekzadeh R. Randomized controlled trial comparing botulinum toxin injection to pneumatic dilatation for the treatment of achalasia. Aliment Pharmacol Ther. 2001;15:1389–96. doi: 10.1046/j.1365-2036.2001.01065.x. [DOI] [PubMed] [Google Scholar]
- 27.Mikaeli J, Bishehsari F, Montazeri G, Mahdavinia M, Yaghoobi M, Darvish-Moghadam S. et al. Injection of botulinum toxin before pneumatic dilatation in achalasia treatment: a randomized-controlled trial. Aliment Pharmacol Ther. 2006;24:983–9. doi: 10.1111/j.1365-2036.2006.03083.x. [DOI] [PubMed] [Google Scholar]
- 28.Emami MH, Raisi M, Amini J, Tabatabai A, Haghighi M, Tavakoli H. et al. Pneumatic balloon dilation therapy is as effective as esophagomyotomy for achalasia. Dysphagia. 2008;23:155–60. doi: 10.1007/s00455-007-9115-2. [DOI] [PubMed] [Google Scholar]
- 29.Mikaeli J, Bishehsari F, Montazeri G, Yaghoobi M, Malekzadeh R. A pneumatic balloon dilatation in achalasia: a prospective comparison of safety and efficacy with different balloon diameters. Aliment Pharmacol Ther. 2004;20:431–6. doi: 10.1111/j.1365-2036.2004.02080.x. [DOI] [PubMed] [Google Scholar]


