Abstract
The shortage of donor lungs for transplantation causes a significant number of patient deaths. The availability of laboratory engineered, functional organs would be a major advance in meeting the demand for organs for transplantation. The accumulation of information on biological scaffolds and an increased understanding of stem/progenitor cell behavior has led to the idea of generating transplantable organs by decellularizing an organ and recellularizing using appropriate cells. Recellularized solid organs can perform organ-specific functions for short periods of time, which indicates the potential for the clinical use of engineered solid organs in the future.
The present review provides an overview of progress and recent knowledge about decellularization and recellularization-based approaches for generating tissue engineered lungs. Methods to improve decellularization, maturation of recellularized lung, candidate species for transplantation and future prospects of lung bioengineering are also discussed.
Keywords: lung transplantation, decellularization, recellularization, extracellular matrix, stem/progenitor cells, induced pluripotent stem cells
Introduction
Lung transplantation is the last option for the treatment of terminal lung disorders such as chronic obstructive pulmonary disorder (COPD), which is the third leading cause of death in the United States.1,2 More than 2000 lung transplants are performed annually in the United States.3 Whereas lung transplantation is recognized as an established therapy that improves survival and provides an improved quality of life for transplant recipients,4 there are several hurdles that make the transplantation of donor lungs a challenging endeavor.
One critical issue is the condition of the donor lungs. Donor lungs often suffer edema, atelectasis, or pneumonia originating from donor systemic problems or preoperative systemic control..5 The long ischemic time also causes donor lung damage, which directly correlates with primary graft failure.6 Another disadvantage of a lung transplant is the need for life-long administration of immunosuppression drugs in the recipients, which increases the risks of infections and cancer.7 The biggest problem, however, is the acute shortage of transplantable organs. In 2011, there were 2280 patients waiting for lung transplantation in the US alone with the average waiting time of about 1 y.8 The mortality for patients on the wait list is 15.7 per 100 wait-list years in the US.8 In Japan, the situation is worse. The average waiting time in Japan is about 2 y and 9 mo and the waiting mortality is 43 per 100 wait-list years.9 Thus, the demand of lungs greatly exceeds the supply. Further, a longer recipient waiting time for a suitable organ results in the deterioration of the patient’s condition and increases operational risk. Given such unresolved problems, lung transplantation is seen as a necessary but currently imperfect treatment for lung disease.
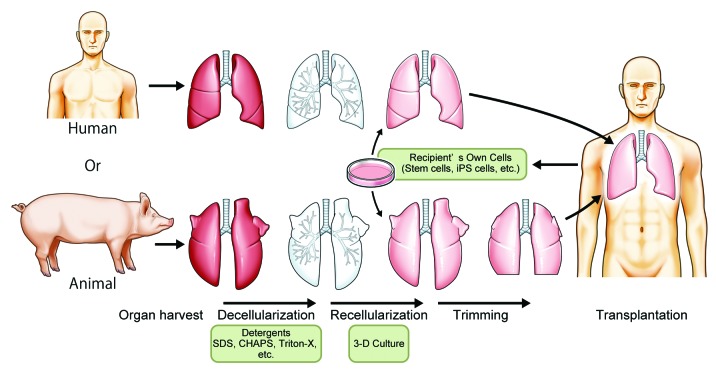
In order to address the problem of organ shortage, several approaches for making transplantable lungs have been attempted, including: biomaterial improvement, 3-dimensional (3D) cell cultures, and ex vivo bioengineering.10-12 Based on the progress of regenerative medicine and the development of recent stem cell advances, investigators have also begun to explore the idea of using decellularized native scaffolds for autologous cell recellularization to generate transplantable bioengineered lungs (Fig. 1).13,14
Figure 1. Schematic of decellularization and recellularization based whole lung regeneration for transplantation. Harvested human or animal lungs are decellularized by detergents such as SDS, CHAPS, or Triton-X. The decellularized lung is recellularized by the recipient’s own stem/progenitor cells or iPSCs.
This review describes the recent developments in using decellularization and recellularization strategies for generating functional lungs for transplantation. We will begin by introducing the concepts of decellularization and recellularization followed by the current status of the cell replacement approach for ex vivo whole lung regeneration, including the use of stem/progenitor cells and studies of extracellular matrix (ECM) preservation. Finally, we address other important aspects of the methodology, such as protocols for organ maturation, the choice of candidate species, operation procedures and the prospect of clinical application of recellularized lung transplantation.
The Concept of Decellularization and Clinical Usage
The ultimate goal of tissue engineering is to generate functional human tissue in vitro or ex vivo that has preserved organ architecture and is non-immunogenic to prevent organ rejection. Decellularized organs appear to be the ideal biomaterial for tissue engineering to achieve these two goals. Decellularized biological scaffolds preserve the 3D organ structure, while removing cells by treatment with detergent, resulting in an acellular and non-antigenic matrix, thus obviating the need for immunosuppression.15 A method for decellularizing tissue, for example, would include extensive rinsing in hypotonic saline, treatment with dilute (0.1%) peracetic acid or incubation in Triton 100X and 0.1 M ammonium hydroxide and a terminal sterilization step with either ethylene oxide, gamma irradiation or E-beam irradiation.16 Such methods have been shown to eliminate all intact cells (i.e., decellularize) and degrade any nucleic acid remnants to less than 200 base pairs with less than 50 ng of dsDNA per 1 mg dry weight of the extracellular matrix scaffold while leaving intact the constituent growth factors such as fibroblast growth factor (FGF), epidermal growth factor (EGF), hepatocyte growth factor (HGF), platelet-derived growth factor (PDGF), bone morphogenic protein (BMP) and vascular endothelial growth factor (VEGF).17,18
ECM scaffolds are currently used for arterial grafts, heart valves, urinary tract reconstitution, skin reconstruction, dura mater grafts following intracranial surgery, and orthopedic applications. Some of the scaffolds are available commercially including: porcine heart valve (Hancock IIⓇ), bovine pericardium heart valve (PERIMOUNT MagnaⓇ), human heart valve (SynegraftⓇ), human dermis (AllodermⓇ), porcine small intestinal scaffold (OaSISⓇ), and decellularized bone (Allograft c-ringⓇ).
The Concept of Recellularization and Clinical Usage
The idea of recellularization of the acellular scaffold originally arose from the clinical usage of acellular matrices and studies of acellular organs.19,20 In the field of cardiovascular surgery, for example, a glutaraldehyde treatment is used to eliminate immunogenicity, provide sterility and induce collagen cross-linking which increases tissue strength and flexibility in xenogeneic or allogeneic heart valves.21 However, the degeneration of glutaraldehyde-fixed valves, with subsequent calcification and tissue failure, was proving to be a major disadvantage of these valvular prostheses.22 Thus, the idea was conceived of covering the surface of porcine glutaraldehyde-fixed valve prostheses with autologous endothelial cells of the recipient in order to delay or eliminate valve degeneration and further reduce thromboembolic events.23 As such, the concept of recellularization involves reseeding of cells into the matrix, where they can attach, migrate, proliferate and perform specialized functions as they would in native tissue so as to recapitulate organ function.
There is clinical and practical evidence that native cells can attach or migrate into a decellularized scaffold.24,25 In animal studies, transplanted decellularized aortic valves or great vessel scaffolds were endothelialized and recellularized by the migration of recipient cells throughout the matrix in a time-dependent manner.25,26 Several cases of these approaches have been successfully utilized in clinical trials including trachea, bladder, and heart valve.27-30
Lung Recellularization Studies Using Decellularized Scaffolds
Unlike simple organs such as skin, heart valve or bone, the lung has a complex 3D structure and therefore decellularized lung by itself cannot be used clinically. However, decellularized lung has been used as a scaffold in studies to elucidate the differentiation and behavior of stem/progenitor cells. Most recellularization studies have been performed using mouse lungs (Table 1), and the recellularization routes were limited to trachea or direct seeding on lung slices. The focus of most recellularizaion strategies has been on epithelial cells and few reports have described the complete endothelialization of decellularized lung scaffolds to date. Thus, the discussion described in the following sections will mainly focus on recellularization strategies using epithelial cells and stem/progenitor cell behavior on acellular lung scaffolds, with some discussion about endothelial cell re-seeding in the lung.
Table 1. Detergents and sources of cells for recellularization in the lung.
| Author | Article | Year | Species of the scaffold | Detergents used | Cell sources for re-seeding | Route of administration | Differentiated phenotype | Institution |
|---|---|---|---|---|---|---|---|---|
| Lwega-Mukasa et al. (32) | Exp Lung Res | 1986 | Human | 0.1%Triton X-100, 2% SDS | Rat AETII cells | Direct seeding | AETI cells | Yale Univ. |
| Petersen et al. (13) | Science | 2010 | Rat (Fisher 344) | 8mM CHAPS | A549 cells, HUVECs, Rat neonatal lung cells and RMECs | Trachea and pulmonary artery | N/A (Transplantable lung) | Yale Univ. |
| Ott et al. (14) | Nature Med | 2010 | Rat (Sprague Dawley) | 0.1% SDS, 0.1%Triton X-100 | A549 cells, rat fetal lung cells and HUVECs | Trachea and pulmonary artery | N/A (Transplantable lung) | Harvard Med School |
| Price et al. (33) | Tissue Eng Part A | 2010 | Mouse (C57BL/6) | 0.1% Triton X-100, 2% SDC | Mouse fetal lung cells | Trachea | Epithelial (AETII cell-like) | Univ. of Minnesota |
| Cortiella et al. (39) | Tissue Eng Part A | 2010 | Rat (Sprague Dawley) | 1% SDS | Mouse ESCs | Trachea | Epithelial (AETII cell-like) | Univ. of Texas Medical Branch |
| Song et al. (34) | Ann Thoracic Surg | 2011 | Rat (Sprague Dawley) | 0.1% SDS, 0.1%Triton X-100 | Rat fetal lung cells and HUVECs | Trachea and pulmonary artery | N/A (Transplantable lung) | Harvard Med School |
| Shamis et al. (35) | Tissue Eng Part C | 2011 | Rat (Lewis) | 0.5% Triton X-100 | Mouse AETII cells | Direct seeding | Epithelial (AETII cell-like) | Hebrew Univ. |
| Daly et al. (50) | Tissue Eng Part A | 2011 | Mouse (C57BL/6, BALB/C) | 0.1% Triton X-100, 2% SDC | Mouse BM-MSCs and C10 epithelial cells | Trachea | Mesenchymal and osteoblast from BM-MSCs | Univ. of Vermont |
| Wallis et al. (51) | Tissue Eng Part C | 2011 | Mouse (BALB/C) | 3 different protocols; (1) 0.1% Triton X-100, 2% SDC. (2) 0.1% SDS, 0.1%Triton X-100. (3) 8mMCHAPS. | Mouse BM-MSCs and C10 epithelial cells | Trachea | N/A (Distributed on scaffold) | Univ. of Vermont |
| Jensen et al. (40) | Tissue Eng Part C | 2012 | Mouse (C57BL/6) | 0.1% Triton X-100, 2% SDC | Mouse ESCs | Trachea | Epithelial (AETII cell-like) | Univ. of Connecticut Health Center |
| Longmire et al. (41) | Cell stem cell | 2012 | Mouse (C57BL/6) | 0.1% Triton X-100, 2% SDC | Mouse ESCs | Trachea | Epithelial | Boston Univ. |
| Bonvillain et al. (77) | Tissue Eng Part A | 2012 | Rhesus macaque | 0.1% Triton X-100, 2% SDC | Rhesus BM-MSCs and AD-MSCs | Bronchioles | N/A (Distributed on scaffold) | Tulane Univ. |
| Booth et al. (78) | Am J Resp Crit Care | 2012 | Human | 0.1% Triton X-100, 2% SDC | Human lung fibroblasts | Airway and vascular | N/A (Distributed on scaffold) | Univ. of Michigan |
| Sokocevic et al. (52) | Biomaterials | 2013 | Mouse (C57BL/6) | 0.1% Triton X-100, 2% SDC | Mouse BM-MSCs and C10 epithelial cells | Trachea | N/A (Distributed on scaffold) | Univ. of Vermont |
| Bonenfant et al. (53) | Biomaterials | 2013 | Mouse (C57BL/6) | 0.1% Triton X-100, 2% SDC | Mouse BM-MSCs and C10 epithelial cells | Trachea | N/A (Distributed on scaffold) | Univ. of Vermont |
| Nichols et al. (79) | Tissue Eng Part A | 2013 | Human and Pig | 2% SDS, 1% SDS | Mouse ESCs, human fetal lung cells, pig BM-MSCs and human AETII cells | Direct seeding | N/A (Distributed on scaffold) | Univ. of Texas Medical Branch |
| Nakayama et al. (80) | PLOS one | 2013 | Rhesus monkey | 0.1% SDS, 0.01%Triton X-100 | Human ESCs | Direct seeding | N/A (Upregulate lung associated gene expression) | Univ. California Davis |
| O'Neill et al. (81) | Ann Thoracic Surg | 2013 | Human and Pig | 3 different protocols; (1) 1.8mM SDS. (2) 8mM CHAPS. (3) 3% Tween 20, 4% SDC. | Human small airway epithelial cells and AD-MSCs | Direct seeding | N/A (Distributed on scaffold) | Columba Univ. |
| Ghaedi et al. (56) | J Clin Invest | 2013 | Human and Rat (Fisher 344 or SD) | (1) 0.1% Triton X-100, 2% SDC for human lung. (2) 8mM CHAPS for rat lung. | Human AETII and iPSC-AETII cells | ①Direct seeding for human lung. ②Trachea for rat lung | AETI cells | Yale Univ. |
| Sun et al. (82) | Am J Physiol Lung Cell Mol Physiol | 2013 | Mouse | 8mM CHAPS | Mouse fibroblast A9 cells | Direct seeding | N/A (Distributed on scaffold) | Yale Univ. |
| Elizabeth-Gilpin et al. (83) | J Heart Lung Transplant | 2013 | Rat, Human and Pig | For rat; 3 different protocols; .(1) 0.1% SDS, 1% Triton-X (2) 0.1% Triton X, 2% SDC2. (3) 8mM CHAPS. For human; 1% Triton-X | Human small airway epithelial cells, pulmonary epithelial cells and HUVECs | Direct seeding for slice. Via bronchus for human lung lobe. | N/A (Distributed on scaffold) | Harvard Med School |
Triton X-100, Nonionic detergent used to solubilize proteins; mild non-denaturing detergent. SDC, Sodium deoxycholate; Water soluble ionic detergent used for disrupting and dissociated protein interaction. SDS, Sodium dodecyl sulfate; Anionic surfactant used for lysing cells and unraveling proteins. CHAPS, 3-[(3-cholamidopropyl)dimethylammonio]-1-propanesulfonate; Non-denaturing zwitterionic detergent used to solubilize proteins. AETII; alveolar epithelial type II. AETI; alveolar epithelial type I. HUVECs; human umbilical vein endothelial cells. RMECs; Rat lung microvascular endothelial cells. ESCs; Embryonic stem cells. AECII; Alveolar epithelial cell. BM-MSCs; Bone marrow derived mesenchymal stem cells. AD-MSCs; Adipose derived mesenchymal stem cells. SP-B; surfactant protein B. iPSC; induced pluripotent stem cell
Epithelial cells
The alveolar epithelium consists of two major specialized epithelial cell types: the terminally differentiated squamous alveolar epithelial type I (AETI) cells, which constitute approximately 93% of the alveolar surface area, and the surfactant producing cuboidal alveolar epithelial type II (AETII) cells. While AETII cells only cover 7% of the alveolar surface area, they constitute 67% of the epithelial cell population within the alveoli, indicating their biochemical importance.31
In 1986, Jamson and colleagues succeeded in transforming AETII cells into AETI cells by directly seeding adult rat AETII cells onto 150 µm thick fragments of acellular human alveolar matrix.32 Several groups have tried seeding fetal alveolar epithelial cells into decellularized lung via the trachea.33-35 Price and colleagues demonstrated that the decellularized lung matrix bioreactor was capable of supporting the growth of fetal AETII cells.33 Analysis of cryosections taken seven days after injection of fetal cells into lung matrices showed pro-SP-C, cytokeratin 18, and 40,6- diamidino-2-phenylindole (DAPI)-positive cells lining alveolar areas and the cells appeared to be attached to the matrix.33 This indicates that the decellularized scaffold retains the components necessary to direct the differentiation of progenitor cells into cells appropriate for that organ. A proteomic analysis showed a significantly different composition for decellularized lung scaffold compared with liver scaffold.35 Alveolar progenitor cells administrated to the liver failed to transcribe lung specific proteins of surfactant protein such as C (SP-C), an AETII cell marker, and aquaporin-5 (AQO-5), an AETI cell marker. Therefore, the ECM itself can affect alveolar epithelial cell behavior and differentiation depending on the organ from which it was derived, and thus is critical for controlling cell fate.
Endothelial cells
Like the epithelium, the endothelium exhibits significant functional heterogeneity. Proper function of the endothelium in the lung is critical for a variety of processes, including gas exchange and regulation of fluid and solute passage between blood and interstitial compartments (barrier function), supporting normal epithelial cell and progenitor cell behavior and function as well as non-respiratory metabolic processes.
Endothelial seeding in the vascular compartment of decellularized rat lung scaffolds showed uneven distribution and incomplete coverage using rat lung microvascular endothelial cells13 and HUVECs.14,34 For these reasons, thrombosis and ultimate failure of the organ occurred. Given their important role in the lung, the use of endothelial cells for recellularization needs to be examined more closely, including specific cell type, scale up potential and route of administration.
Embryonic stem cells (ESCs)
ESCs are derived from the inner cell mass of a blastocyst-stage embryo and can differentiate into any type of cell of ectodermal, endodermal or mesodermal origin.36 For example, human ESCs can differentiate into AETII and bronchial epithelial cells.37,38 Cortelia and colleagues immunohistologically confirmed that decellularized lung promoted differentiation of mouse ESCs into epithelial and endothelial lineages.39 Jensen and colleagues seeded pre-differentiated murine ESCs with phenotypic characteristics of AETII cells into decellularized lungs and found that neovascularization developed in scaffolds that were subcutaneously implanted for 14 d.40 Similarly, Longmire and colleagues demonstrated the step-wise derivation, purification, and culture of primordial lung and thyroid endodermal progenitors and purified Nkx2–1+ endodermal progenitors that differentiate into thyroid and lung lineages.41 These reports demonstrate that the decellularized scaffold also supports the differentiation of ESCs into lung-specific lineages and that the scaffold can also be recellularized by ESC-derived lung epithelial cells.
Mesenchymal stem cells (MSCs)
MSCs are known to have a capacity for self-renewal and an ability to differentiate into cells of the mesenchymal lineage, including adipocytes and osteocytes.42 MSCs can be derived from different tissues, including adipose and bone marrow, which is the main source of exogenous stem cells. Bone marrow-derived MSCs (BM-MSCs) are released into circulation upon inflammatory stimuli and facilitate recovery and repair in the inflammatory process.43,44 A club cell secretary protein (CCSP) -expressing progenitor population in the bone marrow and its role in bronchial repair has also been reported.45 Interestingly, an increase in bone marrow-derived endothelial cells within the lung capillary walls was observed during alveologenesis in mouse models of lung regeneration. This was achieved by treatment with granulocyte colony stimulating factor (GCSF),46 hepatocyte growth factor (HGF)47,48 or adrenomedullin.49
However, it is unknown whether MSCs can differentiate into lung epithelial cells in a decellularized scaffold. Daly and colleagues demonstrated that BM-MSCs administrated into the trachea initially target a region of the trachea, become established, and subsequently proliferate and migrate toward regions enriched in types I and IV collagen and laminin.50 However, BM-MSCs predominantly express genes consistent with a mesenchymal and osteoblast phenotype suggesting that MSCs cannot differentiate into AETII cells in basal medium or small airway growth media (SAGM). Bonvillain and colleagues seeded adipose tissue derived MSCs onto decellularized lung49; while they attached and could be maintained in vitro, there is no evidence that MSCs could differentiate into lung epithelial-specific lineages in decellularized lung.51-53
Induced pluripotent stems cells (iPSCs)
iPSCs have been generated from several somatic cell types by the forced expression of Oct3/4, Sox2, Klf4 and c-Myc (and recently Glis192), commonly known as the Yamanaka factors.54,55 iPSCs, similar to ESCs, can differentiate into virtually any cell type in the body, but have the advantage that they do not require the destruction of an embryo. Additionally, a significant advantage of iPSCs is the ability to obtain autologous differentiated cells for clinical therapy since they are patient-specific.
Recently, Ghaedi and colleagues generated a homogeneous population of AETII and AETI cells from human iPSCs (iPSC-AETII) using step-wise derivation, purification, and culture expansion.56 Since embryonic lung arises from definitive endoderm (DE), the first step requires saturating concentrations of activin A exposure for generating DE from iPSCs. For generating anterior foregut endoderm (AFE) from DE cells, NOGGIN and SB-431524 are then used, followed by the addition of a cocktail of trophic factors containing EGF/BMP4/Wnt3a/FGF10/KGF for generating alveolar progenitors.56 Interestingly, an air–liquid interface provided by a rotating bioreactor culture system was a potent inducer of AETI phenotype from iPSC-AETII cells.57 These techniques provide a method for large-scale production of alveolar epithelium for tissue engineering, providing an important stepping stone toward the ultimate goal of ex vivo lung regeneration from autologous cells.
Stem/progenitor cells and mixed cell repopulation
Other candidate stem/progenitor cells have been used for recellularization. Alveolar progenitor cells (AEPCs) isolated from human lungs, c-kit-positive cells, and E-Cadherin and leucine-rich repeat-containing G-protein-coupled receptor 6 double positive (E-Cad/Lgr6+) cells might have the potential for differentiation into lung specific lineages.58,59 Fujino and colleagues demonstrated that AEPCs have an epithelial phenotype with an MSC character. According to microarray analysis, AEPCs share many genes with AETII cells and mesenchymal stem cells, which suggests an overlapping phenotype with both the alveolar epithelium and the mesenchyme in these cells.58 Kajstura and colleagues isolated c-kit-positive cells from adult human lungs and when the cell population was injected into injured lungs of C57BL/6 mice, the cells differentiated not only into epithelial cells, but also into mesenchymal and endothelial cells without rejection.59 Oeztuerk-Winder and colleagues identified E-Cad/Lgr6+ cells as a distinct population of human alveolar stem cells. E-Cad/Lgr6+ single-cell injection in the kidney capsule produce differentiated bronchioalveolar tissue, while retaining self-renewal.60 These cells may potentially act as endogenous lung stem cells. However, the use of both cells for lung recellularization has not been reported yet.
In contrast to the stem/progenitor cell seeding studies, fetal or neonatal lung cells were used for re-seeding decellularized lung with the goal of achieving total organ regeneration rather than as a system for studying the behavior of stem/progenitor cells in the scaffold.13,14 Because the lung has two divaricate systems of airway and vessels, regenerated lung was seeded with pulmonary epithelial cells from airways (via trachea) and vessel endothelial cells from the pulmonary artery in addition to cells derived from fetal or neonatal whole lung. In this system, the administrated mixture of lung cell types migrated to and attached to the appropriate sites and displayed remarkable hierarchical organization. Recent studies support this homing and engrafting phenomenon; endothelial progenitor cells (EPCs) utilize adhesion molecules for homing to sites of neovascularization similar to the leukocytes.61
Current Status of Recellularized Lung Transplantation
Two institutions in the US reported the first recellularized tissue engineered lung in 2010.13,14 Using a bioreactor, they cultured pulmonary epithelium (whole cell suspension) and vascular endothelium in the acellular lung matrix. They then transplanted the engineered lungs into rats, which participated in gas exchange for 120 min in one case and 30 min in the other. Physiological treatment, including dry ventilation with positive end-expiratory pressure (PEEP), hyperosmolar perfusion before transplantation, conservative weaning and frequent suctioning through an endotracheal tube, could prolong the oxygenation for as long as 7 d at levels comparable to cadaveric lung transplants.34
Though demonstrating proof of concept, graft longevity and homeostasis are still limited. Three day air-ventilated lungs show greatly dilated airways with cell debris evident. Overall, it appears that ventilation with air in the bioreactor causes some destruction of the airway epithelium and dilation of peripheral airspaces.62 This epithelial damage due to ventilation means that the recellularized lung has incomplete architecture. Technical hurdles still need to be addressed to optimally ventilate lungs in bioreactors to mimic physiological conditions.
The Role of ECM in the Lung
Transplantation studies of recellularized lung reveal that the alveolar structure of the bioengineered lung is fragile and the histological integrity of the recellularized lung seems to be determined by damage to the ECM at the thin barrier of the alveoli.63 On the other hand, although cytokines and growth factors are present within ECM in very small quantities, they modulate cell proliferation and proper differentiation.16,64 For this reason, investigators have focused on the ECM of the lung.
Collagen is the most abundant protein within the mammalian ECM. Greater than 90% of the dry weight of the ECM from most tissues and organs consists of collagen.65 The main subtypes that make up the lung’s structure are collagens I, III, IV, and V. Type I collagen is the major structural protein present in tissues. Type IV collagen forms a complex branch network and is largely present within the basement membrane of most vascular structures and within tissues that contain an epithelial cell component.64 In nature, collagen is closely associated with glycosylated proteins, growth factors and other structural proteins such as elastin and laminin, which provide unique tissue properties.
The non-collagenous glycoproteins of fibronectin and laminin are both important ECM basement membrane proteins for cell adhesion.64,66-68 They have important biological functions in the lung, including formation and maintenance of the vasculature.69 Integrins are the major cell surface receptors for laminin.70 The crucial role of the β-1 integrin chain in mediating hematopoietic stem cell interactions with fibronectin and laminin has been firmly established.71
Glycosaminoglycans (GAGs) are found on cell surfaces, within intracellular vesicles, and are incorporated into the ECM.72 They bind growth factors and cytokines, help control macromolecular and cellular movement across the basal lamina, and contribute to the properties of the ECM by using negatively charged ‘tails’ to sequester water.16 Because GAGS are intrinsically part of the cell surface, removal of cells and cell components will ultimately cause the depletion of cell-bound GAGs.
Elastic fibers are constructed with elastin and microfibrils, such as fibrillin. Elastin contributes to tissue elasticity, stretch, and the intrinsic tissue recoil property essential for breathing.73 Additionally, elastic fibers provide the pulmonary vasculature with resilience and are critical to the function of arteries.74 Elastic fibers are highly stable constructs; however, elastin can be degraded by elastases, such as metalloproteinases.16 The de novo synthesis of elastin is difficult to achieve because of low post-natal production and slow turnover. In addition, without sufficient elastin content, tissue degradation and calcification could occur upon implantation.75 Therefore, it would be highly desirable to preserve elastin during decellularization.
The Effect of Decellularization on ECM and Cell Components
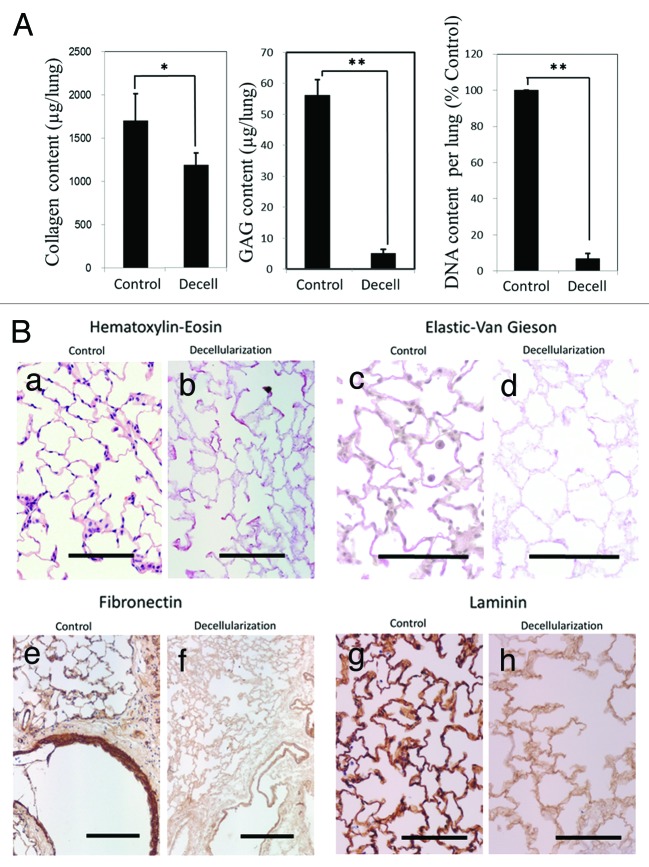
The challenge for any decellularization protocol is the effective removal of all cellular and nuclear material while retaining ECM structure and composition. Previous work has shown that detergent based decellularization can damage ECMs, with decreases in collagen, elastin, and GAG content of 0–30%, 60% and almost 90% compared with the native lung, respectively (Fig. 2A).13,63 Histological and immnohistochemical studies also reveal extreme reduction of other matrix components including elastic fibers, fibronectin, and laminin (Fig. 2B).63,76 Consequently, the preservation of the ECM during the decellularization process is critical for producing a suitable scaffold for recellularization and whole lung engineering.
Figure 2. (A) Comparison of Collagen, GAG, and DNA content in untreated control lung vs. decellularized lung. Asterisk indicates a significant difference between the groups (*; P < 0.05, **; P < 0.005,). Data are expressed as mean values ±SD, n = 5. (B) Histological and immunohistochemical comparison of the ECM in untreated control lung vs. decellularized lung. Scale bar = 100 µm
Considerable effort has gone into determining the best protocols for decellularization.69,76 The most commonly used detergents are Triton-X 100/sodium deoxycholate (Triton/SDC), sodium dodecyl sulfate (SDS), or 3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulfonate (CHAPS) (Table 1). There are few direct comparisons of various protocols utilizing different detergents, but Weiss et al. reported Triton/SDC is less disruptive to native ECM when compared with CHAPS and SDS approaches.63,76 However, when cells were intratracheally inoculated into the various decellularized lungs, the results were comparable for initial binding and short-term (2 wk) proliferation of two different cell types, a stromal progenitor cell and a mouse lung epithelial cell line.76
Cellular and nuclear remnants from the decellularization process can elicit an immune response. However, the complete elimination of all cell membrane and nuclear materials is very difficult (Fig. 2A).18 In one study of commercially available ECM scaffold materials, remnant DNA fragments were common, but do not appear to present significant risk, suggesting some amount of remnant nuclear material is acceptable.84 Furthermore, proteomic analysis utilizing mass spectrometry has revealed a wide range of residual nuclear, intracellular and cytoskeletal proteins to be present in the lungs, despite reports of effective decellularization.50-53 A recipient of such a material would be expected to mount an immune response to the foreign remnants in the ECM graft, yet it is unclear that such remnants have a negative effect on immunoreaction.85 A preliminary study of BALB/c mice implanted with porcine-derived ECM of the small intestinal submucosa showed that all animals elicited a Th2-type response, which is correlated with transplant acceptance.86 Interestingly, recipient cells produced inflammatory cytokines such as TNF-α and IL-1 and are decreased in the surrounding tissue, while anti-inflammatory cytokines such as IL-5 and IL-10 are increased. In a clinical trial, a transplanted recellularized trachea had remnant donor cellular elements in cartilaginous areas, yet it avoided rejection without the use of immunosuppressive drugs.27 On the basis of results obtained with other engineered tissues, retained ECM elements and remnants of cell components might provide helpful signals to both graft and host cells as well as reduce the inflammatory response. It is also possible that a weak immunoreaction mainly induces a Th-2 type response, which might induce graft acceptance or activate remodeling processes.86
Methods for Improving Decellularized Matrix Integrity
Because detergent-based decellularization has been shown to cause some damage to lung barrier function, there is much interest in protocols that preserve or strengthen the ECM while still achieving complete decellularization. One approach is to vary the pH of the CHAPS-based methods. Our results suggest that lower pH solutions (less basic) might reduce ECM damage. Most notably, more neutral pH detergents decreased the loss of GAG and elastin content, but did not effectively remove all DNA (unpublished data). Another method is to coat the decellularized scaffold with either collagen or Matrigel via the trachea in order to enhance cell adhesion and preserve the mechanics of the scaffold.40 This might repair the damage to the microarchitecture of the recellularized lung following decellularization, however there was no obvious improvement in lung architecture, cellular adhesion, or phenotypic expression of reseeded alveolar epithelial type II cells.40
The route by which the detergents are administered also affects lung microarchitecture integrity. Original decellularization methods utilized vascular perfusion of detergents but were found to cause barrier damage that resulted with blood in the airways upon implantation after reseeding.11,12 Decellularization via the airway might be more effective than vasculature perfusion because total surface area of the respiratory field is extremely large (100 to 140 m2) and more easily accessed.87 Maghsoudlou et al. reported a method of intermittent breathing of detergent to produce an acellular scaffold with improved preservation of pulmonary microarchitecture, including basement membranes.88 In a preliminary pathological and immunohistochemical study, however, airway-based decellularization decreased ECM retention, including proteoglycans, elastic fibers, fibronectin and laminin more than our perfusion-based method (unpublished data).
Maturation of Recellularized Lung
In order to make a more complete and functional engineered lung, a variety of physiological and external factors are necessary (Fig. 3). The stepwise differentiation method of iPSCs gives us much information on generating definitive endoderm (DE), anterior foregut endoderm (AFE) and subsequently, a homogeneous population of human AETII and AETI cells from stem cells.56 The process of organogenesis during fetal development also gives us insight into what is necessary for lung maturation.89,90 During early gestation, glucocorticoids have several effects. They stimulate cell maturation and differentiation, while inhibiting DNA synthesis. They also stimulate antioxidant enzymes, increase phospholipid synthesis, and regulate pulmonary liquid metabolism, which produce surfactant associated.91 Lung organogenesis is also controlled by mediators including Nkx2–1 and growth factors, such as PDGFs, FGFs (FGF 10/7/2) and insulin-like growth factors (IGFs).92 Retinoic acid accelerates fetal lung branching, leading to the development of the alveolar tree.93 Therefore, treatment with combinations of growth factors or hormones, with appropriate timing, might facilitate maturation and establishment of the epithelial and endothelial interactions during recellularization.
Figure 3. Possible approaches for recellularization and maturation of decellularized lung. Harvested stem cells can be matured and differentiated in vitro or left in the progenitor cell state using trophic factors and re-seeded into decellularized lung scaffolds. Mediators can then be used to support maturation, followed by bioreactor culture using intermittent mechanical stretch to simulate fetal breathing. Length and extent of organ maturation ex vivo can vary.
Fetal breathing movements (FBMs) play an important role in regulating fetal lung growth and maturation.92,94 During gestation, FBMs are detected at embryonic day (E) 14.5 in the mouse and at 10 wk gestation in human embryos.92 FBMs cause lung cells to function biochemically as well as mechanically. Clinical reports and laboratory experiments have revealed that the absence of FBMs in the embryo leads to such conditions as pulmonary hypoplasia and akinesia.
In vitro, intermittent mechanical stretch (IMS) has been used to simulate FBMs.95 In the 3D- cell culture model, IMS stimulated DNA synthesis and cell division of fetal lung fibroblasts and epithelial cells.95,96 Accordingly, in rat models, IMS increases SP-C gene expression97 and stimulates the secretion of lung surfactant lipids from AETII cells.98,99 Furthermore, mechanical stretching has a significant impact on the synthesis and secretion of several of these ECM molecules in 3D culture or fetal rat lung cells including type I and type IV collagens, fibronectin, proteoglycans, and GAGs.100-102 At the same time, IMS does not affect gene expression and activities of several matrix metalloproteinases (MMPs).102 Because the ECM structure depends on a balance between ECM synthesis and its destruction by proteolytic enzymes, mechanical stretching might only affect synthesis resulting in ECM maturation.
Candidate Species for Decellularized Scaffolds and Transplantation
In order to generate enough transplantable lungs using recellularization approaches, the selection of a donor source for generating decellularized scaffolds is an important consideration. Given the issue of immunogenicity, human organs are the most favorable candidates. However, structural lung diseases such as emphysema or pulmonary fibrosis are often present in donor organs from older people. Using immunohistochemistry and mass spectrometry, it has been shown that age, lung condition, and the cell type used for recellularization may significantly impact the usefulness of decellularized whole lungs for ex vivo lung tissue regeneration.52 Therefore, the ability to use donated human lungs might be limited because of the necessity of harvesting young and healthy lungs.
As a potential solution to the limited availability of healthy human lung tissue, animals may offer an ample supply of lungs. Among candidate species, concordant animals such as baboons would be ideal but are not viable candidates due to ethical concerns, limited populations, and the possibility of an unknown zoonosis. Among discordant animals, porcine lung might be suitable due to similarity in organ shape and size, availability in large numbers, and affordability. In addition, there is already extensive clinical experience using porcine organs and tissues. Components of the ECM may differ between human and pig, but that has not yet been demonstrated to be a problem. Many components of the ECM, such as collagen, are highly conserved across species.65 This high degree of sequence homology is one reason that xenogeneic ECM can function as a suitable scaffold in mammalian recipients.
It has been shown that ECM derived from porcine tissues contains small amounts of the α-galactosyl epitope (gal epitope), which causes a hyperacute type of rejection via a complement response.103 However, whereas the gal epitope has been shown to be present in the acellular matrix scaffold material,104 most preclinical studies using acellular matrix scaffolds have failed to show convincing evidence of an adverse immunologic response and tissue remodeling.105-107 Additionally, pigs have now been created with genetic modifications to reduce xenogenic rejection in humans.108-110 For example, the alpha1,3-galactosyltransferase gene-knockout pig has been engineered to ensure more complete immunogenicity-deleted lungs.111 The development of these gene-knockout animals may solve the potential danger of tissue rejection and coagulopathy in xenotransplantation between pigs and mammals.112
The operational procedures of engineered lung transplantation will be the final major issue. The standard technique of lung transplantation includes anastomosing the main bronchus, the pulmonary vein, and the pulmonary artery trunk. Until ECM components can be better preserved during decellularization, engineered lung remains at a mechanical disadvantage and surgical techniques must be developed to prevent tissue damage and rupture of the anastomoses. When xenogeneic engineered lungs are used, tissue trimming might also be needed (Fig. 3). For example, the porcine right lung has a specific tracheal bronchus with cranial lobe,113 which will be sacrificed in the right lung transplantation. The shape of the lung is different between the species due to the difference in the thoracic cavity. Further animal transplantation studies focusing on pig lung into primate recipients are necessary to establish an optimized surgical technique for xenogeneic engineered lungs.114
Conclusion
To address the shortage of organs for lung transplantation, many approaches have been tried. Significant progress has been made using cellular therapies for lung regeneration, including recent advances using iPSCs that can be differentiated into lung epithelium. While still in the early stages, these patient specific cells can be derived in unlimited quantities and don’t pose a risk of rejection in a transplant setting. Decellularized lung, which can maintain a near intact ECM and the complex microarchitecture of the lung, has been shown to be an ideal scaffold for reseeding with cells. Thus, recellularization based lung regeneration may prove to be an effective clinical therapy for future treatment of lung diseases.
However, there are still many issues that remain to be resolved before such bioengineered lungs become available for clinical use. Issues still to be resolved include: the ideal decellularization method, the ideal duration for whole lung recellularization and the minimum number and types of necessary cells. Many of these issues are currently being addressed through research to address the current clinical problems in lung transplantation. The success of these approaches for lung bioengineering will result in substantial benefits for the field of transplantation medicine.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
The authors thank Dr Mary Durbin and Dr Yutaka Maeda for critical reading of the manuscript.
References
- 1.Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, Egan T, Keshavjee S, Knoop C, Kotloff R, et al. Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation International guidelines for the selection of lung transplant candidates: 2006 update--a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006;25:745–55. doi: 10.1016/j.healun.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Sherry M, Xu J, Kenneth M, Kochanek M. Deaths: Final data for 2010. Natl Vital Stat Rep. 2013;61:1–116. [PubMed] [Google Scholar]
- 3.Orens JB, Garrity ER., Jr. General overview of lung transplantation and review of organ allocation. Proc Am Thorac Soc. 2009;6:13–9. doi: 10.1513/pats.200807-072GO. [DOI] [PubMed] [Google Scholar]
- 4.Kotsimbos T, Williams TJ, Anderson GP. Update on lung transplantation: programmes, patients and prospects. Eur Respir Rev. 2012;21:271–305. doi: 10.1183/09059180.00006312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Grady NP, Murray PR, Ames N. Preventing ventilator-associated pneumonia: does the evidence support the practice? JAMA. 2012;307:2534–9. doi: 10.1001/jama.2012.6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grover FL, Fullerton DA, Zamora MR, Mills C, Ackerman B, Badesch D, Brown JM, Campbell DN, Chetham P, Dhaliwal A, et al. The past, present, and future of lung transplantation. Am J Surg. 1997;173:523–33. doi: 10.1016/S0002-9610(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 7.Zafar SY, Howell DN, Gockerman JP. Malignancy after solid organ transplantation: an overview. Oncologist. 2008;13:769–78. doi: 10.1634/theoncologist.2007-0251. [DOI] [PubMed] [Google Scholar]
- 8.Valapour M, Paulson K, Smith JM, Hertz MI, Skeans MA, Heubner BM, Edwards LB, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2011 Annual Data Report: lung. Am J Transplant. 2013;13(Suppl 1):149–77. doi: 10.1111/ajt.12024. [DOI] [PubMed] [Google Scholar]
- 9.Oto T, Okada Y, Bando T, Minami M, Shiraishi T, Nagayasu T, Chida M, Okumura M, Date H, Miyoshi S, et al. Japanese Society of Lung and Heart–Lung Transplantation Registry of the Japanese society of lung and heart-lung transplantation: the official Japanese lung transplantation report 2012. Gen Thorac Cardiovasc Surg. 2013;61:208–11. doi: 10.1007/s11748-013-0215-7. [DOI] [PubMed] [Google Scholar]
- 10.Cooper DKC, Ekser B, Burlak C, Ezzelarab M, Hara H, Paris L, Tector AJ, Phelps C, Azimzadeh AM, Ayares D, et al. Clinical lung xenotransplantation--what donor genetic modifications may be necessary? Xenotransplantation. 2012;19:144–58. doi: 10.1111/j.1399-3089.2012.00708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franzdóttir SR, Axelsson IT, Arason AJ, Baldursson O, Gudjonsson T, Magnusson MK. Airway branching morphogenesis in three dimensional culture. Respir Res. 2010;11:162–72. doi: 10.1186/1465-9921-11-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huh D, Matthews BD, Mammoto A, Montoya-Zavala M, Hsin HY, Ingber DE. Reconstituting organ-level lung functions on a chip. Science. 2010;328:1662–8. doi: 10.1126/science.1188302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petersen TH, Calle EA, Zhao L, Lee EJ, Gui L, Raredon MB, Gavrilov K, Yi T, Zhuang ZW, Breuer C, et al. Tissue-engineered lungs for in vivo implantation. Science. 2010;329:538–41. doi: 10.1126/science.1189345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ott HC, Clippinger B, Conrad C, Schuetz C, Pomerantseva I, Ikonomou L, Kotton D, Vacanti JP. Regeneration and orthotopic transplantation of a bioartificial lung. Nat Med. 2010;16:927–33. doi: 10.1038/nm.2193. [DOI] [PubMed] [Google Scholar]
- 15.Gilbert TW, Sellaro TL, Badylak SF. Decellularization of tissues and organs. Biomaterials. 2006;27:3675–83. doi: 10.1016/j.biomaterials.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Badylak SF. Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol. 2004;12:367–77. doi: 10.1016/j.trim.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 17.McDevitt CA, Wildey GM, Cutrone RM. Transforming growth factor-beta1 in a sterilized tissue derived from the pig small intestine submucosa. J Biomed Mater Res A. 2003;67:637–40. doi: 10.1002/jbm.a.10144. [DOI] [PubMed] [Google Scholar]
- 18.Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials. 2011;32:3233–43. doi: 10.1016/j.biomaterials.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerson CJ, Elkins RC, Goldstein S, Heacox AE. Structural integrity of collagen and elastin in SynerGraft® decellularized-cryopreserved human heart valves. Cryobiology. 2012;64:33–42. doi: 10.1016/j.cryobiol.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Yagi H, Soto-Gutierrez A, Kitagawa Y. Whole-organ re-engineering: a regenerative medicine approach to digestive organ replacement. Surg Today. 2013;43:587–94. doi: 10.1007/s00595-012-0396-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schenke-Layland K, Vasilevski O, Opitz F, König K, Riemann I, Halbhuber KJ, Wahlers T, Stock UA. Impact of decellularization of xenogeneic tissue on extracellular matrix integrity for tissue engineering of heart valves. J Struct Biol. 2003;143:201–8. doi: 10.1016/j.jsb.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Gulbins H, Goldemund A, Anderson I, Haas U, Uhlig A, Meiser B, Reichart B. Preseeding with autologous fibroblasts improves endothelialization of glutaraldehyde-fixed porcine aortic valves. J Thorac Cardiovasc Surg. 2003;125:592–601. doi: 10.1067/mtc.2003.48. [DOI] [PubMed] [Google Scholar]
- 23.Steinhoff G, Stock U, Karim N, Mertsching H, Timke A, Meliss RR, Pethig K, Haverich A, Bader A. Tissue engineering of pulmonary heart valves on allogenic acellular matrix conduits: in vivo restoration of valve tissue. Circulation. 2000;102(Suppl 3):III50–5. doi: 10.1161/01.CIR.102.suppl_3.III-50. [DOI] [PubMed] [Google Scholar]
- 24.Sayk F, Bos I, Schubert U, Wedel T, Sievers H-H. Histopathologic findings in a novel decellularized pulmonary homograft: an autopsy study. Ann Thorac Surg. 2005;79:1755–8. doi: 10.1016/j.athoracsur.2003.11.049. [DOI] [PubMed] [Google Scholar]
- 25.Takagi K, Fukunaga S, Nishi A, Shojima T, Yoshikawa K, Hori H, Akashi H, Aoyagi S. In vivo recellularization of plain decellularized xenografts with specific cell characterization in the systemic circulation: histological and immunohistochemical study. Artif Organs. 2006;30:233–41. doi: 10.1111/j.1525-1594.2006.00210.x. [DOI] [PubMed] [Google Scholar]
- 26.Ketchedjian A, Jones AL, Krueger P, Robinson E, Crouch K, Wolfinbarger L, Jr., Hopkins R. Recellularization of decellularized allograft scaffolds in ovine great vessel reconstructions. Ann Thorac Surg. 2005;79:888–96, discussion 896. doi: 10.1016/j.athoracsur.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 27.Macchiarini P, Jungebluth P, Go T, Asnaghi MA, Rees LE, Cogan TA, Dodson A, Martorell J, Bellini S, Parnigotto PP, et al. Clinical transplantation of a tissue-engineered airway. Lancet. 2008;372:2023–30. doi: 10.1016/S0140-6736(08)61598-6. [DOI] [PubMed] [Google Scholar]
- 28.Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB. Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet. 2006;367:1241–6. doi: 10.1016/S0140-6736(06)68438-9. [DOI] [PubMed] [Google Scholar]
- 29.Biancosino C, Zardo P, Walles T, Wildfang I, Macchiarini P, Mertsching H. Generation of a bioartificial fibromuscular tissue with autoregenerative capacities for surgical reconstruction. Cytotherapy. 2006;8:178–83. doi: 10.1080/14653240600621166. [DOI] [PubMed] [Google Scholar]
- 30.Cebotari S, Lichtenberg A, Tudorache I, Hilfiker A, Mertsching H, Leyh R, Breymann T, Kallenbach K, Maniuc L, Batrinac A, et al. Clinical application of tissue engineered human heart valves using autologous progenitor cells. Circulation. 2006;114(Suppl):I132–7. doi: 10.1161/CIRCULATIONAHA.105.001065. [DOI] [PubMed] [Google Scholar]
- 31.Hermanns MI, Unger RE, Kehe K, Peters K, Kirkpatrick CJ. Lung epithelial cell lines in coculture with human pulmonary microvascular endothelial cells: development of an alveolo-capillary barrier in vitro. Lab Invest. 2004;84:736–52. doi: 10.1038/labinvest.3700081. [DOI] [PubMed] [Google Scholar]
- 32.Lwebuga-Mukasa J, Inggar D, Madri J. Repopulation of a human alveolar matrix by adult rat type II pneumocytes in vitro. A novel system for type II pneumocyte culture. Exp Cell Res. 1986;162:423–35. doi: 10.1016/0014-4827(86)90347-2. [DOI] [PubMed] [Google Scholar]
- 33.Price AP, England KA, Matson AM, Blazar BR, Panoskaltsis-Mortari A. Development of a decellularized lung bioreactor system for bioengineering the lung: the matrix reloaded. Tissue Eng Part A. 2010;16:2581–91. doi: 10.1089/ten.tea.2009.0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song JJ, Kim SS, Liu Z, Madsen JC, Mathisen DJ, Vacanti JP, Ott HC. Enhanced in vivo function of bioartificial lungs in rats. Ann Thorac Surg. 2011;92:998–1005, discussion 1005-6. doi: 10.1016/j.athoracsur.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 35.Shamis Y, Hasson E, Soroker A, Bassat E, Shimoni Y, Ziv T, Sionov RV, Mitrani E. Organ-specific scaffolds for in vitro expansion, differentiation, and organization of primary lung cells. Tissue Eng Part C Methods. 2011;17:861–70. doi: 10.1089/ten.tec.2010.0717. [DOI] [PubMed] [Google Scholar]
- 36.Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 37.Wang D, Haviland DL, Burns AR, Zsigmond E, Wetsel RA. A pure population of lung alveolar epithelial type II cells derived from human embryonic stem cells. Proc Natl Acad Sci U S A. 2007;104:4449–54. doi: 10.1073/pnas.0700052104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samadikuchaksaraei A, Cohen S, Isaac K, Rippon HJ, Polak JM, Bielby RC, Bishop AE. Derivation of distal airway epithelium from human embryonic stem cells. Tissue Eng. 2006;12:867–75. doi: 10.1089/ten.2006.12.867. [DOI] [PubMed] [Google Scholar]
- 39.Cortiella J, Niles J, Cantu A, Brettler A, Pham A, Vargas G, Winston S, Wang J, Walls S, Nichols JE. Influence of acellular natural lung matrix on murine embryonic stem cell differentiation and tissue formation. Tissue Eng Part A. 2010;16:2565–80. doi: 10.1089/ten.tea.2009.0730. [DOI] [PubMed] [Google Scholar]
- 40.Jensen T, Sc M, Roszell B, Ph D, Zang F, Girard E, Matson A, Thrall R, Jaworski DM, Hatton C, et al. A rapid lung de-cellularization protocol supports embryonic stem cell differentiation in vitro and following implantation. Tissue Eng Part C Methods. 2012;18:632–46. doi: 10.1089/ten.tec.2011.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Longmire TA, Ikonomou L, Hawkins F, Christodoulou C, Cao Y, Jean JC, Kwok LW, Mou H, Rajagopal J, Shen SS, et al. Efficient derivation of purified lung and thyroid progenitors from embryonic stem cells. Cell Stem Cell. 2012;10:398–411. doi: 10.1016/j.stem.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop Dj, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- 43.Yamada M, Kubo H, Ishizawa K, Kobayashi S, Shinkawa M, Sasaki H. Increased circulating endothelial progenitor cells in patients with bacterial pneumonia: evidence that bone marrow derived cells contribute to lung repair. Thorax. 2005;60:410–3. doi: 10.1136/thx.2004.034058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burnham EL, Taylor WR, Quyyumi AA, Rojas M, Brigham KL, Moss M. Increased circulating endothelial progenitor cells are associated with survival in acute lung injury. Am J Respir Crit Care Med. 2005;172:854–60. doi: 10.1164/rccm.200410-1325OC. [DOI] [PubMed] [Google Scholar]
- 45.Wong AP, Keating A, Lu W-Y, Duchesneau P, Wang X, Sacher A, Hu J, Waddell TK. Identification of a bone marrow-derived epithelial-like population capable of repopulating injured mouse airway epithelium. J Clin Invest. 2009;119:336–48. doi: 10.1172/JCI36882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yamada M, Kubo H, Kobayashi S, Ishizawa K, Numasaki M, Ueda S, Suzuki T, Sasaki H. Bone marrow-derived progenitor cells are important for lung repair after lipopolysaccharide-induced lung injury. J Immunol. 2004;172:1266–72. doi: 10.4049/jimmunol.172.2.1266. [DOI] [PubMed] [Google Scholar]
- 47.Hegab AE, Kubo H, Yamaya M, Asada M, He M, Fujino N, Mizuno S, Nakamura T. Intranasal HGF administration ameliorates the physiologic and morphologic changes in lung emphysema. Mol Ther. 2008;16:1417–26. doi: 10.1038/mt.2008.137. [DOI] [PubMed] [Google Scholar]
- 48.Ishizawa K, Kubo H, Yamada M, Kobayashi S, Numasaki M, Ueda S, Suzuki T, Sasaki H. Bone marrow-derived cells contribute to lung regeneration after elastase-induced pulmonary emphysema. FEBS Lett. 2004;556:249–52. doi: 10.1016/S0014-5793(03)01399-1. [DOI] [PubMed] [Google Scholar]
- 49.Nolen-Walston RD, Kim CF, Mazan MR, Ingenito EP, Gruntman AM, Tsai L, Boston R, Woolfenden AE, Jacks T, Hoffman AM. Cellular kinetics and modeling of bronchioalveolar stem cell response during lung regeneration. Am J Physiol Lung Cell Mol Physiol. 2008;294:L1158–65. doi: 10.1152/ajplung.00298.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Daly AB, Wallis JM, Borg ZD, Bonvillain RW, Deng B, Ballif BA, Jaworski DM, Allen GB, Weiss DJ. Initial binding and recellularization of decellularized mouse lung scaffolds with bone marrow-derived mesenchymal stromal cells. Tissue Eng Part A. 2012;18:1–16. doi: 10.1089/ten.tea.2011.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wallis JM, Borg ZD, Daly AB, Deng B, Ballif BA, Allen GB, Jaworski DM, Weiss DJ. Comparative assessment of detergent-based protocols for mouse lung de-cellularization and re-cellularization. Tissue Eng Part C Methods. 2012;18:420–32. doi: 10.1089/ten.tec.2011.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sokocevic D, Bonenfant NR, Wagner DE, Borg ZD, Lathrop MJ, Lam YW, Deng B, Desarno MJ, Ashikaga T, Loi R, et al. The effect of age and emphysematous and fibrotic injury on the re-cellularization of de-cellularized lungs. Biomaterials. 2013;34:3256–69. doi: 10.1016/j.biomaterials.2013.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bonenfant NR, Sokocevic D, Wagner DE, Borg ZD, Lathrop MJ, Lam YW, Deng B, Desarno MJ, Ashikaga T, Loi R, et al. The effects of storage and sterilization on de-cellularized and re-cellularized whole lung. Biomaterials. 2013;34:3231–45. doi: 10.1016/j.biomaterials.2013.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–76. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 55.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 56.Ghaedi M, Calle EA, Mendez JJ, Gard AL, Balestrini J, Booth A, Bove PF, Gui L, White ES, Niklason LE. Human iPS cell-derived alveolar epithelium repopulates lung extracellular matrix. J Clin Invest. 2013;123:4950–62. doi: 10.1172/JCI68793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghaedi M, Mendez JJ, Bove PF, Sivarapatna A, Raredon MSB, Niklason LE. Alveolar epithelial differentiation of human induced pluripotent stem cells in a rotating bioreactor. Biomaterials. 2014;35:699–710. doi: 10.1016/j.biomaterials.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fujino N, Kubo H, Suzuki T, Ota C, Hegab AE, He M, Suzuki S, Suzuki T, Yamada M, Kondo T, et al. Isolation of alveolar epithelial type II progenitor cells from adult human lungs. Lab Invest. 2011;91:363–78. doi: 10.1038/labinvest.2010.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kajstura J, Rota M, Hall SR, Hosoda T, D’Amario D, Sanada F, Zheng H, Ogórek B, Rondon-Clavo C, Ferreira-Martins J, et al. Evidence for human lung stem cells. N Engl J Med. 2011;364:1795–806. doi: 10.1056/NEJMoa1101324. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 60.Oeztuerk-Winder F, Guinot A, Ochalek A, Ventura J-J. Regulation of human lung alveolar multipotent cells by a novel p38α MAPK/miR-17-92 axis. EMBO J. 2012;31:3431–41. doi: 10.1038/emboj.2012.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chavakis E, Urbich C, Dimmeler S. Homing and engraftment of progenitor cells: a prerequisite for cell therapy. J Mol Cell Cardiol. 2008;45:514–22. doi: 10.1016/j.yjmcc.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 62.Petersen TH, Calle EA, Colehour MB, Niklason LE. Bioreactor for the long-term culture of lung tissue. Cell Transplant. 2011;20:1117–26. doi: 10.3727/096368910X544933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Petersen TH, Calle EA, Colehour MB, Niklason LE. Matrix composition and mechanics of decellularized lung scaffolds. Cells Tissues Organs. 2012;195:222–31. doi: 10.1159/000324896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dunsmore SE, Rannels DE. Extracellular matrix biology in the lung. Am J Physiol. 1996;270:L3–27. doi: 10.1152/ajplung.1996.270.1.L3. [DOI] [PubMed] [Google Scholar]
- 65.van der Rest M, Garrone R. Collagen family of proteins. FASEB J. 1991;5:2814–23. [PubMed] [Google Scholar]
- 66.Schwarzbauer JE. Fibronectin: from gene to protein. Curr Opin Cell Biol. 1991;3:786–91. doi: 10.1016/0955-0674(91)90051-Y. [DOI] [PubMed] [Google Scholar]
- 67.Nguyen NM, Senior RM. Laminin isoforms and lung development: all isoforms are not equal. Dev Biol. 2006;294:271–9. doi: 10.1016/j.ydbio.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 68.Miner JH, Yurchenco PD. Laminin functions in tissue morphogenesis. Annu Rev Cell Dev Biol. 2004;20:255–84. doi: 10.1146/annurev.cellbio.20.010403.094555. [DOI] [PubMed] [Google Scholar]
- 69.Badylak SF, Taylor D, Uygun K. Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix scaffolds. Annu Rev Biomed Eng. 2011;13:27–53. doi: 10.1146/annurev-bioeng-071910-124743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schwarzbauer J. Basement membranes: Putting up the barriers. Curr Biol. 1999;9:R242–4. doi: 10.1016/S0960-9822(99)80153-5. [DOI] [PubMed] [Google Scholar]
- 71.Ponce ML, Nomizu M, Delgado MC, Kuratomi Y, Hoffman MP, Powell S, Yamada Y, Kleinman HK, Malinda KM. Identification of endothelial cell binding sites on the laminin gamma 1 chain. Circ Res. 1999;84:688–94. doi: 10.1161/01.RES.84.6.688. [DOI] [PubMed] [Google Scholar]
- 72.Ferdous Z, Grande-Allen KJ. Utility and control of proteoglycans in tissue engineering. Tissue Eng. 2007;13:1893–904. doi: 10.1089/ten.2006.0056. [DOI] [PubMed] [Google Scholar]
- 73.Yuan H, Kononov S, Cavalcante FS, Lutchen KR, Ingenito EP, Suki B. Effects of collagenase and elastase on the mechanical properties of lung tissue strips. J Appl Physiol (1985) 2000;89:3–14. doi: 10.1152/jappl.2000.89.1.3. [DOI] [PubMed] [Google Scholar]
- 74.Kielty CM, Sherratt MJ, Shuttleworth CA. Elastic fibres. J Cell Sci. 2002;115:2817–28. doi: 10.1242/jcs.115.14.2817. [DOI] [PubMed] [Google Scholar]
- 75.Isenburg JC, Simionescu DT, Vyavahare NR. Tannic acid treatment enhances biostability and reduces calcification of glutaraldehyde fixed aortic wall. Biomaterials. 2005;26:1237–45. doi: 10.1016/j.biomaterials.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 76.Wallis JM, Borg ZD, Daly AB, Deng B, Ballif BA, Allen GB, Jaworski DM, Weiss DJ. Comparative assessment of detergent-based protocols for mouse lung de-cellularization and re-cellularization. Tissue Eng Part C Methods. 2012;18:420–32. doi: 10.1089/ten.tec.2011.0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bonvillain RW, Danchuk S, Sullivan DE, Betancourt AM, Semon JA, Eagle ME, Mayeux JP, Gregory AN, Wang G, Townley IK, et al. A nonhuman primate model of lung regeneration: detergent-mediated decellularization and initial in vitro recellularization with mesenchymal stem cells. Tissue Eng Part A. 2012;18:2437–52. doi: 10.1089/ten.tea.2011.0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Booth AJ, Hadley R, Cornett AM, Dreffs AA, Matthes SA, Tsui JL, Weiss K, Horowitz JC, Fiore VF, Barker TH, et al. Acellular normal and fibrotic human lung matrices as a culture system for in vitro investigation. Am J Respir Crit Care Med. 2012;186:866–76. doi: 10.1164/rccm.201204-0754OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nichols JE, Niles J, Riddle M, Vargas G, Schilagard T, Ma L, Edward K, La Francesca S, Sakamoto J, Vega S, et al. Production and assessment of decellularized pig and human lung scaffolds. Tissue Eng Part A. 2013;19:2045–62. doi: 10.1089/ten.tea.2012.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nakayama KH, Lee CCI, Batchelder CA, Tarantal AF. Tissue specificity of decellularized rhesus monkey kidney and lung scaffolds. PLoS One. 2013;8:e64134. doi: 10.1371/journal.pone.0064134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.O’Neill JD, Anfang R, Anandappa A, Costa J, Javidfar J, Wobma HM, Singh G, Freytes DO, Bacchetta MD, Sonett JR, et al. Decellularization of human and porcine lung tissues for pulmonary tissue engineering. Ann Thorac Surg. 2013;96:1046–55, discussion 1055-6. doi: 10.1016/j.athoracsur.2013.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sun H, Calle EA, Chen X, Mathur A, Zhu Y, Mendez J, Zhao L, Niklason LE, Peng X, Peng H, et al. Fibroblast engraftment in the decellularized mouse lung occurs via a β1 integrin dependent, FAK dependent pathway that is mediated by ERK and opposed by AKT. Am J Physiol Lung Cell Mol Physiol. 2013 doi: 10.1152/ajplung.00100.2013. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Elizabeth Gilpin S, Guyette JP, Gonzalez G, Ren X, Asara JM, Mathisen DJ, Vacanti JP, Ott HC. Perfusion decellularization of human and porcine lungs: Bringing the matrix to clinical scale. J Heart Lung Transplant. 2013 doi: 10.1016/j.healun.2013.10.030. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 84.Gilbert TW, Freund JM, Badylak SF. Quantification of DNA in biologic scaffold materials. J Surg Res. 2009;152:135–9. doi: 10.1016/j.jss.2008.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Strom TB, Roy-Chaudhury P, Manfro R, Zheng XX, Nickerson PW, Wood K, Bushell A. The Th1/Th2 paradigm and the allograft response. Curr Opin Immunol. 1996;8:688–93. doi: 10.1016/S0952-7915(96)80087-2. [DOI] [PubMed] [Google Scholar]
- 86.Allman AJ, McPherson TB, Badylak SF, Merrill LC, Kallakury B, Sheehan C, Raeder RH, Metzger DW. Xenogeneic extracellular matrix grafts elicit a TH2-restricted immune response. Transplantation. 2001;71:1631–40. doi: 10.1097/00007890-200106150-00024. [DOI] [PubMed] [Google Scholar]
- 87.Gehr P, Bachofen M, Weibel ER. The normal human lung: ultrastructure and morphometric estimation of diffusion capacity. Respir Physiol. 1978;32:121–40. doi: 10.1016/0034-5687(78)90104-4. [DOI] [PubMed] [Google Scholar]
- 88.Maghsoudlou P, Georgiades F, Tyraskis A, Totonelli G, Loukogeorgakis SP, Orlando G, Shangaris P, Lange P, Delalande J-M, Burns AJ, et al. Preservation of micro-architecture and angiogenic potential in a pulmonary acellular matrix obtained using intermittent intra-tracheal flow of detergent enzymatic treatment. Biomaterials. 2013;34:6638–48. doi: 10.1016/j.biomaterials.2013.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maeda Y, Davé V, Whitsett JA. Transcriptional control of lung morphogenesis. Physiol Rev. 2007;87:219–44. doi: 10.1152/physrev.00028.2006. [DOI] [PubMed] [Google Scholar]
- 90.Liu M, Post M. Invited review: mechanochemical signal transduction in the fetal lung. J Appl Physiol (1985) 2000;89:2078–84. doi: 10.1152/jappl.2000.89.5.2078. [DOI] [PubMed] [Google Scholar]
- 91.Bolt RJ, van Weissenbruch MM, Lafeber HN, Delemarre-van de Waal HA. Glucocorticoids and lung development in the fetus and preterm infant. Pediatr Pulmonol. 2001;32:76–91. doi: 10.1002/ppul.1092. [DOI] [PubMed] [Google Scholar]
- 92.Inanlou MR, Baguma-Nibasheka M, Kablar B. The role of fetal breathing-like movements in lung organogenesis. Histol Histopathol. 2005;20:1261–6. doi: 10.14670/HH-20.1261. [DOI] [PubMed] [Google Scholar]
- 93.Chytil F. Retinoids in lung development. FASEB J. 1996;10:986–92. doi: 10.1096/fasebj.10.9.8801181. [DOI] [PubMed] [Google Scholar]
- 94.Harding R, Hooper SB. Regulation of lung expansion and lung growth before birth. J Appl Physiol (1985) 1996;81:209–24. doi: 10.1152/jappl.1996.81.1.209. [DOI] [PubMed] [Google Scholar]
- 95.Liu M, Skinner SJ, Xu J, Han RNN, Tanswell AK, Post M. Stimulation of fetal rat lung cell proliferation in vitro by mechanical stretch. Am J Physiol. 1992;263:L376–83. doi: 10.1152/ajplung.1992.263.3.L376. [DOI] [PubMed] [Google Scholar]
- 96.Xu J, Liu M, Tanswell AK, Post M. Mesenchymal determination of mechanical strain-induced fetal lung cell proliferation. Am J Physiol. 1998;275:L545–50. doi: 10.1152/ajplung.1998.275.3.L545. [DOI] [PubMed] [Google Scholar]
- 97.Nakamura T, Liu M, Mourgeon E, Slutsky A, Post M. Mechanical strain and dexamethasone selectively increase surfactant protein C and tropoelastin gene expression. Am J Physiol Lung Cell Mol Physiol. 2000;278:L974–80. doi: 10.1152/ajplung.2000.278.5.L974. [DOI] [PubMed] [Google Scholar]
- 98.Rose F, Kürth-Landwehr C, Sibelius U, Reuner KH, Aktories K, Seeger W, Grimminger F. Role of actin depolymerization in the surfactant secretory response of alveolar epithelial type II cells. Am J Respir Crit Care Med. 1999;159:206–12. doi: 10.1164/ajrccm.159.1.9801106. [DOI] [PubMed] [Google Scholar]
- 99.Rose F, Zwick K, Ghofrani HA, Sibelius U, Seeger W, Walmrath D, Grimminger F. Prostacyclin enhances stretch-induced surfactant secretion in alveolar epithelial type II cells. Am J Respir Crit Care Med. 1999;160:846–51. doi: 10.1164/ajrccm.160.3.9812155. [DOI] [PubMed] [Google Scholar]
- 100.Mourgeon E, Xu J, Tanswell AK, Liu M, Post M. Mechanical strain-induced posttranscriptional regulation of fibronectin production in fetal lung cells. Am J Physiol. 1999;277:L142–9. doi: 10.1152/ajplung.1999.277.1.L142. [DOI] [PubMed] [Google Scholar]
- 101.Xu J, Liu M, Liu J, Caniggia I, Post M. Mechanical strain induces constitutive and regulated secretion of glycosaminoglycans and proteoglycans in fetal lung cells. J Cell Sci. 1996;109:1605–13. doi: 10.1242/jcs.109.6.1605. [DOI] [PubMed] [Google Scholar]
- 102.Xu J, Liu M, Post M. Differential regulation of extracellular matrix molecules by mechanical strain of fetal lung cells. Am J Physiol. 1999;276:L728–35. doi: 10.1152/ajplung.1999.276.5.L728. [DOI] [PubMed] [Google Scholar]
- 103.Daly KA, Stewart-Akers AM, Hara H, Ezzelarab M, Long C, Cordero K, Johnson SA, Ayares D, Cooper DKC, Badylak SF. Effect of the alphaGal epitope on the response to small intestinal submucosa extracellular matrix in a nonhuman primate model. Tissue Eng Part A. 2009;15:3877–88. doi: 10.1089/ten.tea.2009.0089. [DOI] [PubMed] [Google Scholar]
- 104.McPherson TB, Liang H, Record RD, Badylak SF. Galalpha(1,3)Gal epitope in porcine small intestinal submucosa. Tissue Eng. 2000;6:233–9. doi: 10.1089/10763270050044416. [DOI] [PubMed] [Google Scholar]
- 105.Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R. Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res. 2002;103:190–202. doi: 10.1006/jsre.2001.6349. [DOI] [PubMed] [Google Scholar]
- 106.Nuininga JE, van Moerkerk H, Hanssen A, Hulsbergen CA, Oosterwijk-Wakka J, Oosterwijk E, de Gier RPE, Schalken JA, van Kuppevelt T, Feitz WFJ. Rabbit urethra replacement with a defined biomatrix or small intestinal submucosa. Eur Urol. 2003;44:266–71. doi: 10.1016/S0302-2838(03)00249-5. [DOI] [PubMed] [Google Scholar]
- 107.Nieponice A, McGrath K, Qureshi I, Beckman EJ, Luketich JD, Gilbert TW, Badylak SF. An extracellular matrix scaffold for esophageal stricture prevention after circumferential EMR. Gastrointest Endosc. 2009;69:289–96. doi: 10.1016/j.gie.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 108.Cantu E, Parker W, Platt JL, Duane Davis R. Pulmonary xenotransplantation: rapidly progressing into the unknown. Am J Transplant. 2004;4(Suppl 6):25–35. doi: 10.1111/j.1600-6135.2004.0342.x. [DOI] [PubMed] [Google Scholar]
- 109.Toledo-Pereyra LH, Lopez-Neblina F. Xenotransplantation: a view to the past and an unrealized promise to the future. Exp Clin Transplant. 2003;1:1–7. [PubMed] [Google Scholar]
- 110.Ekser B, Rigotti P, Gridelli B, Cooper DKC. Xenotransplantation of solid organs in the pig-to-primate model. Transpl Immunol. 2009;21:87–92. doi: 10.1016/j.trim.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 111.Lai L, Kolber-Simonds D, Park K-W, Cheong H-T, Greenstein JL, Im G-S, Samuel M, Bonk A, Rieke A, Day BN, et al. Production of alpha-1,3-galactosyltransferase knockout pigs by nuclear transfer cloning. Science. 2002;295:1089–92. doi: 10.1126/science.1068228. [DOI] [PubMed] [Google Scholar]
- 112.Bush EL, Barbas AS, Holzknecht ZE, Byrne GW, McGregor CG, Parker W, Davis RD, Lin SS. Coagulopathy in α-galactosyl transferase knockout pulmonary xenotransplants. Xenotransplantation. 2011;18:6–13. doi: 10.1111/j.1399-3089.2011.00621.x. [DOI] [PubMed] [Google Scholar]
- 113.Nakakuki S. Bronchial tree, lobular division and blood vessels of the pig lung. J Vet Med Sci. 1994;56:685–9. doi: 10.1292/jvms.56.685. [DOI] [PubMed] [Google Scholar]
- 114.Daggett CW, Yeatman M, Lodge AJ, Chen EP, Linn SS, Gullotto C, Frank MM, Platt JL, Davis RD. Total respiratory support from swine lungs in primate recipients. J Thorac Cardiovasc Surg. 1998;115:19–27. doi: 10.1016/S0022-5223(98)70438-6. [DOI] [PubMed] [Google Scholar]