Abstract
Background
Occupational exposure to extremely low frequency magnetic fields (ELF) is a suspected risk factor for brain tumours, however the literature is inconsistent. Few studies have assessed whether ELF in different time windows of exposure may be associated with specific histologic types of brain tumours. This study examines the association between ELF and brain tumours in the large-scale INTEROCC study.
Methods
Cases of adult primary glioma and meningioma were recruited in seven countries (Australia, Canada, France, Germany, Israel, New Zealand, United Kingdom) between 2000 and 2004. Estimates of mean workday ELF exposure based on a job exposure matrix assigned. Estimates of cumulative exposure, average exposure, maximum exposure, and exposure duration were calculated for the lifetime, and 1–4, 5–9, and 10+ years prior to the diagnosis/reference date.
Results
There were 3,761 included brain tumour cases (1,939 glioma, 1,822 meningioma) and 5,404 population controls. There was no association between lifetime cumulative ELF exposure and glioma or meningioma risk. However, there were positive associations between cumulative ELF 1–4 years prior to the diagnosis/reference date and glioma (odds ratio (OR) ≥ 90th percentile vs < 25th percentile = 1.67, 95% confidence interval (CI) 1.36–2.07, p < 0.0001 linear trend), and, somewhat weaker associations with meningioma (OR ≥ 90th percentile vs < 25th percentile = 1.23, 95% CI 0.97–1.57, p = 0.02 linear trend).
Conclusions
Results showed positive associations between ELF in the recent past and glioma.
Impact
Occupational ELF exposure may play a role in the later stages (promotion and progression) of brain tumourigenesis.
Keywords: extremely low frequency magnetic fields, occupation, glioma, meningioma, case-control study
INTRODUCTION
There are few established risk factors for brain tumours (1). In countries with cancer registries, it is estimated that the annual age-standardized incidence rate of primary malignant tumours of the brain and nervous system is between three and four per 100,000. It is slightly higher among males than females and in developed than developing countries (1,2). Small increases in the incidence of some types of brain tumours have been observed over recent decades, due to changes in diagnosis, classification, and coding (1,3).
Although ionizing radiation is an established risk factor for the disease, it accounts for a small fraction of the total number of cases (4,5). Possible associations between occupational exposure to non-ionizing radiation sources, in particular extremely low frequency magnetic fields (ELF), which occur during the generation, distribution and use of alternating current electricity, and brain tumours have been examined; however, results are inconsistent and limited by small study sizes and a lack of occupational history data (6). Previous studies have also varied widely in terms of methodology. There have been studies of highly exposed occupational groups, including for example electrical workers, railway professionals, and resistance welders, with study designs ranging from job title-based studies, comparing rates of brain tumours to those expected in the general population (7–9), to studies based on detailed measurements and modelling (10) or job exposure matrices (JEMs) (11–12). There are also general population studies with ELF exposure assessments ranging from self-report or expert judgment through to JEMs (13–17).
A meta-analysis of 48 studies published during 1993–2007 reported a small positive association between occupational ELF and brain tumours overall (relative risk (RR) = 1.14, 95% confidence interval (CI) 1.07–1.22); however, there was no exposure-response relationship using approximations of ELF exposure categories in the original papers (18). Study characteristics that tended to be associated with stronger positive findings included a poor quality exposure assessment, a poorly defined comparison group, as well as an adequate study design.
Most recently, a US study of 489 glioma cases, 197 meningioma cases, and 799 controls reported no association between ELF and glioma (odds ratios (OR) cumulative exposure > 45 milligauss(mG)-years (1 μT = 10 mG) vs 0 exposure > 1.5 mG = 0.8, 95% CI 0.5–1.2) or meningioma risk (OR = 1.0, 95% CI 0.6–1.8) (19). A French study of 221 cases of central nervous system (CNS) tumours and 442 controls, reported a positive association between ELF and meningioma (OR = 3.02, 95% CI 1.10–8.25) (17). No association between ELF and incident brain tumours (n=233) was observed in the Netherlands Cohort Study (20) nor in a study of UK electricity supply workers (n=266) (21).
The International Agency for Research on Cancer (IARC) classified ELF as possibly carcinogenic to humans (Group 2B), based on studies of childhood leukemia, but with inadequate evidence for all other cancers (22). Similar conclusions have been reached more recently (6,23,24). Mechanistically, any role of ELF would likely manifest on the later stages of tumour development, specifically in cancer promotion/progression as suggested by some co-carcinogenicity studies (22,24,25). Few epidemiological studies have had sufficient power to address this hypothesis. Results from some, but not all, studies have observed stronger associations between ELF and brain tumours in the more recent compared to the more distant past, or with more aggressive forms of glioma (11, 13, 16, 26–29).
This study assesses the role of occupational ELF exposure for specific histologic types of brain tumours, namely glioma and meningioma, using data from the large-scale INTEROCC study. Detailed lifetime occupational histories were collected, providing a unique opportunity to examine the potential impact of ELF exposure overall and in specific exposure time windows.
MATERIALS AND METHODS
Study Population
The INTEROCC study is based on a subset of countries from INTERPHONE, a large, 13-country, population-based case-control study conducted according to a common protocol (30). Cases of primary brain (glioma, meningioma), CNS (acoustic neuroma), and salivary gland tumours, aged between 30 and 59 years were recruited between 2000 and 2004. Although INTERPHONE’s primary objective was to examine whether radiofrequency (RF) field exposure from cellular telephones was associated with cancer risk, seven of INTERPHONE 13 countries, collected detailed occupational data and participated in the subsequent INTEROCC study to address outstanding questions concerning occupational agents in glioma and meningioma.
Incident cases were rapidly recruited (median delay from diagnosis to interview ~3 months) from major treatment centers in areas of Australia, Canada, France, Germany, New Zealand, the United Kingdom, and nationwide in Israel, with completeness verified through secondary sources. An expanded age range was used for INTEROCC with Germany including cases aged up to 69 years, the UK 18 to 69 years, and in Israel cases aged 18+ years were recruited to allow for greater case ascertainment. Cases were confirmed histologically or through unequivocal diagnostic imaging.
Controls were randomly selected from electoral lists (Australia, Canada-Montreal, France, New Zealand), population-based registries (Canada-Vancouver, Germany, Israel), patient lists (UK), or random digit dialing (Canada-Ottawa) according to study center. Controls were either frequency- or individually-matched to cases by sex, age (five year groups) and study center within country.
Although the original INTERPHONE protocol called for the selection of only one control for each case of glioma or meningioma, all eligible controls were used here to maximize statistical power. The reference date of controls was calculated as the date of interview minus the median difference between the date of case diagnosis and interview by country. Participants provided written informed consent prior to interview. There were 5,399 eligible brain tumour cases (3,017 gliomas and 2,382 meningiomas) and 11,112 controls (identified from the sampling frame) among whom 3,978 cases (2,054 gliomas and 1,924 meningiomas) and 5,601 controls were interviewed. Major reasons for non-participation among controls in the overall INTERPHONE study include refusal (64%) and inability to contact (27%) (30). Overall participation rates for high-grade and low-grade glioma cases were also similar (67 vs 71% respectively) (30). Ethics approval was obtained from appropriate national and regional research ethics boards including the Ethical Review Board of IARC (Lyon) for INTERPHONE and the Municipal Institute for Medical Investigation (IMIM) Barcelona for INTEROCC.
Data Collection
Eligible participants were interviewed by trained interviewers using a computer-assisted personal interview questionnaire. If the participant had died or was unable to participate, a proxy respondent was allowed. The questionnaire captured detailed data on a range of personal and family characteristics. Participants also completed a lifetime occupational calendar for all jobs held for a minimum of six months, including job title, company name, company description, start and stop year.
Exposure Assessment
A total of 35,862 jobs were reported. A total of 599 jobs (1.7%) were excluded (assigned no ELF exposure) due to invalid start/stop dates; and an additional 23 jobs (0.06%) excluded that ceased prior to age 14 years. Job titles were coded to the International Standard Classification of Occupations 1988 (ISCO88) four digit codes as well as 1968 (ISCO68) five digit codes, since it contains codes for occupations in the utility industry. Coding guidelines were provided to study centers and an inter-coding trial conducted to ensure consistency (31). The mean (SD) number of jobs per subject was 3.9 (±2.6) for glioma cases, 3.6 (±2.6) for meningioma cases, and 3.8 (±2.5) for controls. A small number of participants (103 glioma cases, 95 meningioma cases, and 122 controls) who reported having never been employed were excluded here.
Estimates of mean workday-average ELF exposures came from an enhancement of a measurement-based JEM (32). The JEM was linked to the ISCO88 code for each job unless a JEM estimate was available for a more specific electrical job in ISCO68. The JEM was substantially enhanced by including measurement data on jobs included in the INTEROCC study based on summary statistics or primary data from published occupational studies in Canada, England, Finland, Italy, the Netherlands, New Zealand, Sweden, and the US. These studies used personal monitors to measure ELF exposure reporting the full-shift time-weighted average (TWA) “resultant” of the magnetic flux density in μT. All measurements were made using monitors with bandwidths within a range of 3 to 1,000 Hz.
Pooling studies in the JEM, estimates of geometric mean (GM) were calculated for 278 primary ISCO codes. Where there were no measurement data for a specific ISCO code, exposures were inferred based on similar jobs within the ISCO hierarchy (72 ISCO codes, 4.2% of the jobs of INTEROCC subjects) or estimated using expert judgement (60 ISCO codes, 1.8% of INTEROCC jobs). Jobs classified as an unknown occupation (n=105, 0.3% of jobs) were assigned the geometric mean of control values by centre. Supplementary Table S1 presents a description of ELF levels in selected participant jobs. An online version of the JEM is available at: http://www.crealradiation.com/index.php/en/databases?id=55.
Statistical Analysis
Conditional logistic regression models were used to obtain adjusted ORs and 95% CIs for the association between occupational ELF and brain tumours in seven countries combined stratified by region, country, sex, and five-year age group, and adjusted for education. Categorical indicators of cumulative and average ELF exposure with cut points based on the 25th, 50th, 75th, and, due to the skewed nature of the distribution, the 90th percentile of the control exposure distribution were examined for the lifetime (1-year lag) and in separate exposure-time windows defined a priori, 1–4, 5–9, and 10+ years prior to the date of diagnosis/reference date. Since ELF exposure is ubiquitous, the reference group consisted of participants in the lowest exposure category. Since the most relevant ELF metric, if any, is unknown (19), indicators of maximum exposed job and duration of employment in a job in the highest quartile of participant jobs (>= 0.18 μT) were also examined.
Potential confounding by marital status, cigarette smoking, socioeconomic position (Standard International Occupational Prestige Scale (SIOPS)) (33), allergy history, occupational ionizing radiation (reported wearing a radiation badge), occupational cosmic radiation (prior flight-related occupation), and cumulative cellular telephone use (deciles of minutes of call time for Australia, Canada, France, Israel, New Zealand) were examined but produced virtually no change (<10%) in ORs (not presented) (34, 35, 36). Potential confounding by ever exposure to 29 occupational chemicals selected a priori was also examined, based on chemical exposure estimates assigned based on a modified version of the Finnish job exposure matrix (FINJEM) to study participants as part of INTEROCC (37).
Sensitivity analyses were conducted excluding proxy interviews (30), participants who were judged by the interviewer to be reticent and uninterested in the interview and, participants > 69 years of age, participants with a history of self-reported physician-diagnosed neurofibromatosis or tuberous sclerosis, and for low and high-grade glioma separately. Potential effect modification by country, age, sex, and education was assessed by entering product terms into conditional logistic regression models and assessing their significance according to the likelihood ratio test. Analyses were conducted using SAS version 9.3 (38).
RESULTS
A total of 1,939 (94.4%) glioma cases, 1,822 (94.7%) meningioma cases and 5,404 (96.5%) controls were retained for analysis. The majority of glioma cases were male (62.0%), with meningioma cases being predominantly female (72.5%) (Table 1). The mean (SD) age of study participants was 51.0 (±12.3) years for glioma cases, 54.7 (±11.6) years for meningioma cases, and 51.8 (±11.3) years for controls. The majority of participants had at least a high school education. Levels of lifetime cumulative ELF exposure ranged from 0.02–0.05 μT-years to 467.83–715.93 μT-years in cases (glioma/meningioma) and 0.03 μT-years to 609.38 μT-years in controls (Supplementary Table S2).
Table 1.
Characteristics of case and control participants at enrollment INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
| Glioma Cases (n=1,939) | Meningioma Cases (n=1,822) | Controlsa (n=5,404) | |
|---|---|---|---|
|
| |||
| % | % | % | |
|
| |||
| Sex | |||
| Male | 62.0 | 27.5 | 45.2 |
| Female | 38.0 | 72.5 | 54.8 |
|
| |||
| Age at reference date | |||
| <35 | 11.0 | 4.4 | 7.3 |
| 35–39 | 9.3 | 5.4 | 8.7 |
| 40–44 | 11.1 | 9.2 | 11.6 |
| 45–49 | 12.3 | 14.8 | 13.8 |
| 50–54 | 18.0 | 20.4 | 18.3 |
| 55–59 | 16.1 | 17.1 | 18.7 |
| 60–64 | 9.9 | 10.3 | 9.2 |
| 65–69 | 6.8 | 8.7 | 7.9 |
| 70+ | 5.6 | 9.8 | 4.4 |
|
| |||
| Education | |||
| High School or less | 52.4 | 59.1 | 53.6 |
| Medium level technical school | 19.7 | 19.5 | 19.0 |
| University | 28.0 | 21.4 | 27.4 |
|
| |||
| Country | |||
| Australia | 14.2 | 13.9 | 12.3 |
| Canada | 8.6 | 5.1 | 11.6 |
| France | 4.8 | 7.6 | 8.5 |
| Germany | 18.6 | 20.3 | 27.5 |
| Israel | 20.5 | 36.8 | 17.3 |
| New Zealand | 3.4 | 2.7 | 2.7 |
| United Kingdom | 30.0 | 13.5 | 20.1 |
Glioma and meningioma controls combined.
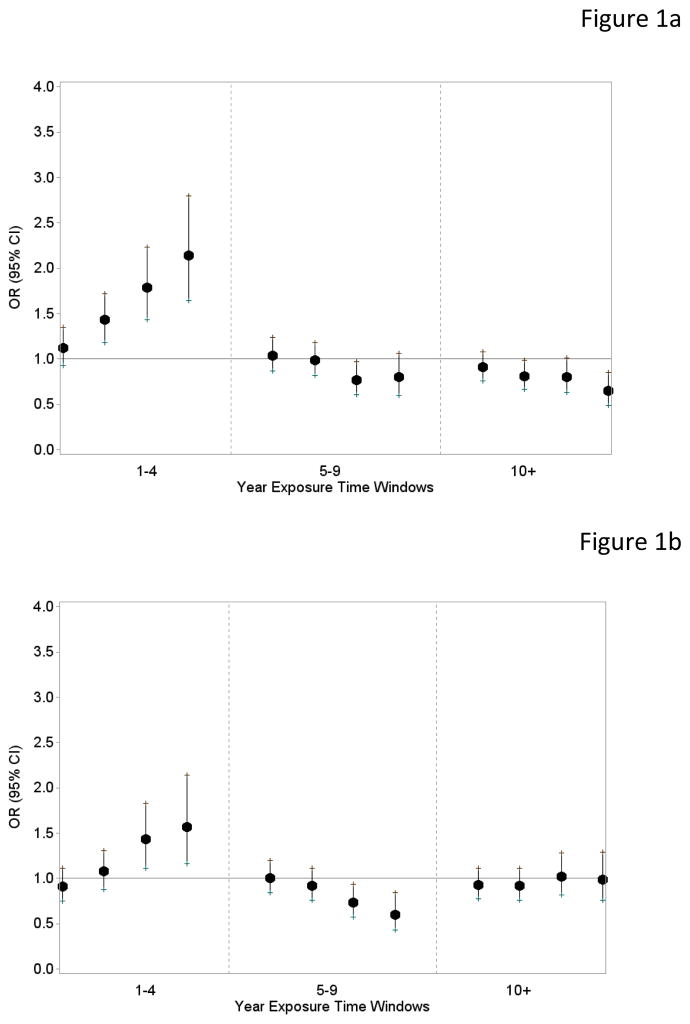
For glioma, there was no association with lifetime cumulative exposure, average exposure, maximum exposed job, or duration of exposure, and there was no exposure-response relationship (Table 2). However, for cumulative ELF there were positive associations in the 1–4 year time window prior to tumour diagnosis/reference date, with ORs ranging from 1.19 (95% CI 1.00–1.43) to 1.67 (95% CI 1.36–2.07) in the highest exposure category (≥ 90th percentile) (p linear trend < 0.0001) (Table 3), comprising ~76% of participants in that time window, relative to those < 25th percentile. There were weaker positive associations in the 5–9 year time window. In the 10+ year time window, there was a weak, non-monotonic inverse association with increasing ELF exposure (OR ≥ 90th percentile vs < 25th percentile = 0.77, 95% CI 0.60–0.99, p linear trend = 0.04). ORs (95% CIs) from a simultaneous exposure time windows model, including cumulative ELF from all three exposure time windows together in the same model, are presented in Figure 1a. Strong correlations between levels of cumulative ELF were observed for glioma cases and controls in the 1–4 and 5–9 year time windows (Supplementary Table S3), but were weaker for other time windows. Results were similar for both high- and low-grade glioma (Supplementary Table S4). Results for average exposure were generally similar in the 5–9 and 10+ year time windows, but in the 1–4 year time window, the positive association was attenuated (Supplementary Table S5). For maximum exposed job, there was a significant inverse trend (p = 0.003) in the 10+ year time window (Supplementary Table S6).
Table 2.
Adjusted ORs (95% CIs)a for glioma and meningioma in relation to categorical indicators of occupational ELF-MF exposure overall (1-year lag), INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
| Exposure Metric | Glioma | Meningioma | ||||
|---|---|---|---|---|---|---|
| Cases | Controls | OR (95% CI)a | Cases | Controls | OR 95% CIa | |
| Cumulative Exposure (μT-years) | ||||||
| < 2.11 | 475 | 1,334 | 1.00 (ref) | 473 | 1,265 | 1.00 (ref) |
| 2.11–< 3.40 | 454 | 1,327 | 1.00 (0.85, 1.18) | 465 | 1,278 | 0.96 (0.82, 1.13) |
| 3.40–< 5.00 | 441 | 1,344 | 0.93 (0.78, 1.11) | 414 | 1,295 | 0.84 (0.70, 0.99) |
| 5.00–<7.50 | 370 | 808 | 1.07 (0.88, 1.31) | 290 | 783 | 1.05 (0.86, 1.29) |
| 7.50+ | 199 | 540 | 0.80 (0.63, 1.00) | 180 | 524 | 0.89 (0.70, 1.12) |
| p-value trend | 0.08 | 0.51 | ||||
| Average Exposure (μT) | ||||||
| < 0.11 | 423 | 1,268 | 1.00 (ref) | 426 | 1,224 | 1.00 (ref) |
| 0.11–< 0.13 | 398 | 1,273 | 0.96 (0.82, 1.13) | 419 | 1,244 | 0.94 (0.79, 1.10) |
| 0.13–<0.17 | 551 | 1,411 | 1.04 (0.89, 1.22) | 510 | 1,345 | 1.18 (1.00, 1.38) |
| 0.17–<0.24 | 330 | 856 | 0.95 (0.80, 1.14) | 262 | 809 | 1.03 (0.85, 1.25) |
| 0.24+ | 237 | 545 | 1.00 (0.82, 1.23) | 205 | 523 | 1.08 (0.87, 1.33) |
| p-value trend | 0.99 | 0·41 | ||||
| Maximum Exposed Job (μT) | ||||||
| < 0.13 | 453 | 1,370 | 1.00 (ref) | 505 | 1,341 | 1.00 (ref) |
| 0.13–< 0.17 | 458 | 1,290 | 0.92 (0.79, 1.08) | 439 | 1,247 | 1.03 (0.88, 1.20) |
| 0.17–< 0.23 | 430 | 1,202 | 0.85 (0.73, 1.00) | 362 | 1,146 | 0.98 (0.83, 1.16) |
| 0.23–<0.62 | 382 | 947 | 0.92 (0.78, 1.09) | 286 | 891 | 1.01 (0.84, 1.21) |
| 0.62+ | 216 | 544 | 0.80 (0.65, 0.98) | 230 | 520 | 1.15 (0.94, 1.42) |
| p-value trend | 0.08 | 0·16 | ||||
| Exposure Duration (years) | ||||||
| < 5 | 1,333 | 3,849 | 1.00 (ref) | 1,324 | 3,716 | 1.00 (ref) |
| 5–< 15 | 295 | 805 | 0.90 (0.77, 1.05) | 255 | 754 | 0.99 (0.84, 1.17) |
| 15–< 25 | 142 | 371 | 0.94 (0.76, 1.16) | 104 | 353 | 0.85 (0.67, 1.08) |
| 25+ | 169 | 328 | 1.22 (0.99, 1.51) | 139 | 322 | 1.30 (1.03, 1.64) |
| p-value trend | 0.26 | 0.20 | ||||
OR estimated using conditional logistic regression models stratified by country, region, sex, and 5-year age group at the reference date and adjusted for level of educational attainment. Cut points based on the 25th, 50th, 75th, and, 90th percentile of the control exposure distribution. Tests for linear trend used Wald x2 tests, with categorical medians modeled as ordinal variables.
Table 3.
Adjusted ORs (95% CIs)a for glioma and meningioma in relation to categorical indicators of cumulative occupational ELF-MF exposure in three separate exposure time windows, 1–4, 5–9, and 10+ years prior to the date of diagnosis/reference date, INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
| Exposure Metric | Glioma | Meningioma | ||||
|---|---|---|---|---|---|---|
| Cumulative Exposure (μT-years) | Cases | Controls | OR 95% CIa | Cases | Controls | OR 95% CIa |
| 1–4 Years | ||||||
| < 0.34 | 332 | 1,115 | 1.00 (ref) | 315 | 1,054 | 1.00 (ref) |
| 0.34–< 0.46 | 338 | 1,012 | 1.19 (1.00, 1.43) | 301 | 970 | 1.00 (0.83, 1.21) |
| 0.46–< 0.58 | 432 | 1,140 | 1.42 (1.19, 1.69) | 350 | 1,093 | 1.12 (0.93, 1.34) |
| 0.58–<0.80 | 297 | 632 | 1.54 (1.27, 1.88) | 210 | 593 | 1.30 (1.05, 1.62) |
| 0.80+ | 237 | 439 | 1.67 (1.36, 2.07) | 142 | 420 | 1.23 (0.97, 1.57) |
| p-value trend | <0.0001 | 0.02 | ||||
| 5–9 Years | ||||||
| < 0.45 | 358 | 1,112 | 1.00 (ref) | 367 | 1,057 | 1.00 (ref) |
| 0.45–< 0.59 | 391 | 1,126 | 1.12 (0.95, 1.33) | 391 | 1,075 | 1.00 (0.84, 1.20) |
| 0.59–< 0.77 | 491 | 1,268 | 1.22 (1.03, 1.43) | 398 | 1,228 | 1.03 (0.86, 1.22) |
| 0.77–<1.07 | 263 | 671 | 1.09 (0.89, 1.32) | 185 | 636 | 0.97 (0.78, 1.20) |
| 1.07+ | 204 | 447 | 1.19 (0.96, 1.47) | 117 | 423 | 0.88 (0.68, 1.13) |
| p-value trend | 0.20 | 0.31 | ||||
| 10+ Years | ||||||
| < 1.38 | 442 | 1,277 | 1.00 (ref) | 435 | 1,198 | 1.00 (ref) |
| 1.38–< 2.48 | 432 | 1,300 | 0.96 (0.81, 1.15) | 436 | 1,251 | 0.91 (0.77, 1.08) |
| 2.48–< 3.98 | 435 | 1,290 | 0.90 (0.75, 1.09) | 433 | 1,247 | 0.90 (0.75, 1.08) |
| 3.98–<6.23 | 326 | 787 | 0.91 (0.73, 1.13) | 279 | 762 | 0.99 (0.80, 1.23) |
| 6.23+ | 197 | 522 | 0.77 (0.60, 0.99) | 189 | 510 | 0.92 (0.72, 1.17) |
| p-value trend | 0.04 | 0.76 | ||||
OR estimated for each exposure time window separately using conditional logistic regression models stratified by country, region, sex, and 5-year age group at the reference date and adjusted for level of educational attainment. Cut points based on the 25th, 50th, 75th, and, 90th percentile of the control population’s exposure distribution for each time window. Different cut-points used for each time window due to differences in exposure distribution. Different numbers of cases/controls in different time windows due to the exclusion of participants from particular time windows where they reported not being employed. Tests for linear trend used Wald x2 tests, with categorical medians modeled as ordinal variables.
Figure 1.
Figure 1a. Adjusted ORs (95% CIs) for glioma in relation to categories of cumulative occupational ELF-MF exposure in the 1–4, 5–9, and 10+ year time windows prior to the date of diagnosis/reference date from a simultaneous exposure time windows model with cutpoints based on the 25th, 50th, 75th, and 90th percentile, INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
Figure 1b. Adjusted ORs (95% CIs) for meningioma in relation to categories of cumulative occupational ELF-MF exposure in the 1–4, 5–9, and 10+ year time windows prior to the date of diagnosis/reference date from a simultaneous exposure time windows model with cutpoints based on the 25th, 50th, 75th, and 90th percentile, INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
For meningioma, there was no association with lifetime cumulative exposure, average exposure, or maximum exposed job (Table 2). However, there was an elevated OR in the highest exposure duration group (25+ vs < 5 years) (OR = 1.30, 95% CI 1.03–1.64). There was also a significant positive linear trend (p = 0.02) with cumulative ELF exposure 1–4 years prior to tumour diagnosis/reference date (Table 3). No associations were seen in the 5–9 or 10+ year time windows. Figure 1b presents ORs (95% CIs) from a simultaneous exposure time windows model. For maximum exposed job, there was a significant positive trend (p = 0.03) in the 1–4 year time window (Supplementary Table S6).
Results for glioma with cumulative ELF in the 1–4 year time window were virtually unchanged with adjustment for occupational chemical exposures, with the exception of adjustment for benzo(a)pyrene (BAP) or polycyclic aromatic hydrocarbon (PAH) exposures, where ORs increased in the highest ELF exposure categories (Supplementary Table S7). ORs in some categories increased for both glioma and meningioma when excluding participants who were judged by the interviewer to be reticent and uninterested in the interview for cumulative ELF in the 1–4 year time window, however in the 10+ year time window, the weak inverse trend attenuated (Table 4). There was no significant effect modification observed.
Table 4.
Adjusted ORs (95% CIs)a for glioma and meningioma in relation to categorical and continuous indicators of cumulative occupational ELF-MF exposure in the 1–4 year and 10+ time window prior to the date of diagnosis/reference date, including only participants who were very cooperative, responsive, and interested as determined by the interviewer, INTEROCC study, 2000–2004, Australia, Canada, France, Germany, Israel, New Zealand, and United Kingdom
| Glioma | Meningioma | |||||
|---|---|---|---|---|---|---|
| Cumulative Exposure (μT-years) 1–4 Years | Cases | Controls | OR 95% CIa | Cases | Controls | OR 95% CIa |
| < 0.34 | 218 | 826 | 1.00 (ref) | 201 | 758 | 1.00 (ref) |
| 0.34–< 0.46 | 218 | 729 | 1.21 (0.97, 1.51) | 201 | 677 | 1.07 (0.85–1.35) |
| 0.46–< 0.58 | 301 | 825 | 1.54 (1.24, 1.90) | 248 | 778 | 1.24 (0.98, 1.55) |
| 0.58–<0.80 | 186 | 450 | 1.52 (1.20, 1.94) | 133 | 400 | 1.39 (1.06, 1.82) |
| 0.80+ | 149 | 304 | 1.76 (1.35, 2.28) | 90 | 282 | 1.30 (0.96, 1.77) |
| p-value trend | <0.0001 | 0.03 | ||||
| 10+ Years | ||||||
| < 1.38 | 291 | 930 | 1.00 (ref) | |||
| 1.38–< 2.48 | 287 | 910 | 1.06 (0.85, 1.32) | |||
| 2.48–< 3.98 | 271 | 916 | 0.99 (0.78, 1.25) | |||
| 3.98–<6.23 | 214 | 539 | 1.14 (0.87, 1.50) | |||
| 6.23+ | 109 | 335 | 0.88 (0.64, 1.21) | |||
| p-value trend | 0.44 | |||||
OR estimated for each exposure time window separately using conditional logistic regression models stratified by country, region, sex, and 5-year age group at the reference date and adjusted for level of educational attainment. Cut-points from Table 3 used here. Tests for linear trend used Wald x2 tests, with categorical medians modeled as ordinal variables.
DISCUSSION
Results from this large-scale study revealed no association between lifetime occupational exposure to ELF, but positive associations with cumulative ELF 1–4 years prior to the diagnosis/reference date and glioma. Weaker positive associations were observed for meningioma. There was also a weak inverse association for glioma with ELF exposure in the distant past (10+ year time window), which attenuated when subjects judged to be reticent and unresponsive were excluded from analyses.
Some studies reported stronger associations with occupational ELF in more recent exposure time windows. Among general population studies, Villeneuve et al. (16), in a study of 543 incident brain tumour cases and controls, observed positive associations in the highest category of average ELF exposure (≥0.6 μT vs < 0.3 μT) for all brain tumours (OR = 1.33, 95% CI 0.75–2.36) and glioblastoma multiforme (OR = 5.36, 95% CI 1.16–24.78) which strengthened for ELF in the last held job (OR = 12.59, 95% CI 1.50–105.6, number of cases (controls) = 18 (6)). Floderus et al. (13), in a study of 261 brain tumour cases and 1,112 controls noted positive associations between ELF in the longest job 10 years prior to diagnosis.
Among more highly exposed occupational groups, previous results were mixed, however, there were small numbers of cases and few examined associations in different time windows (10). Savitz et al. (27), in a case-cohort study including 145 brain tumour deaths from five US electric utility companies, reported positive associations with cumulative ELF (OR = 1.79, 95% CI 0.69–4.65 highest exposed group, 4.33–12.20 vs 0–0.65 μT-years) that strengthened 2–10 years in the past (OR highest exposed group, 1.14–2.23 vs 0 μT-years = 2.62, 95% CI 1.15–5.97). Hakansson et al. (11) in a cohort of over 700,000 resistance welders, observed positive associations between average ELF and astrocytoma in women (n = 66, p for trend = 0.004) in 10 years of follow-up. However, this was not observed in other studies (21, 28, 29).
Although ELF exposure in the 1–4 year time window represents a small proportion of total lifetime occupational ELF exposure, these results are compatible with a role in tumour promotion. ELF cannot impart enough energy to DNA molecules to create mutations, however, it may act on signal transduction, cell proliferation, reactive oxygen species generation, the neuroendocrine or immune system, or interact with other chemical exposures (24, 25). Villeneuve et al. (16) suggested that stronger associations observed with more aggressive forms of glioma may also provide support for a promotional role of ELF, however similar findings were observed for both high- and low-grade glioma here. There was also a weak positive association between ELF in the longest exposure duration category and meningioma (and possibly glioma), possibly suggesting a role for prolonged ELF exposure for that slower growing tumour. Alternatively, findings in different time windows of exposures may be due to chance.
Potential limitations include low participation rates, particularly among controls (ranging from 35–74%) (30). The Swedish INTERPHONE study noted participation was positively associated with working status, income, and education (39). However education was similar for participating cases and controls here. Cases and controls reported a similar number of lifetime jobs. Mean (SD) weighted indicators of occupational prestige (SIOPS) were similar (glioma = 43.0 (±11.7), meningioma = 42.2 (±12.4), controls = 43.8 (±12.0)).
The positive association between ELF and glioma in the 1–4 year time window was seen for all exposure categories, including a large majority (~76%) of participants, across a wide spectrum of occupations, not solely “electrical occupations”. Although preclinical symptoms of a brain tumour might lead to earlier diagnosis in certain jobs; they might also influence changes in occupation in different time windows, particularly for low grade glioma. The mean (SD) difference between average ELF levels in the 10+ and 1–4 year time windows was 0.001 (±0.58) for glioma cases and 0.02 (±0.31) for controls, indicating slight increases in ELF in more recent years. The pre-clinical phase of brain tumours is poorly understood. Fewer participants reported working in a job in the 1–4 year time window; however this appears to be unrelated to case/control status with 84% and 82% of included glioma cases and controls respectively reporting a job in this time window. The association with glioma remained, though attenuated slightly, upon restriction to participants who worked for a full four years in the 1–4 year time window (OR ≥ 90th percentile vs < 25th percentile = 1.44, 95% CI 1.02–2.05, p = 0.05 linear trend).
We also excluded a small number (n=320) of participants who reported having never been employed from analysis in an attempt to avoid potential selection bias by socioeconomic and/or employment status in analysis (5% of glioma cases, 5% of meningioma cases, and 2% of controls). Results including never employed participants in the reference category attenuated somewhat for glioma for ELF in the 1–4 year time window (OR ≥ 90% vs < 25 % = 1.45, 95% CI 1.20, 1.76) but the positive linear trend remained (p < 0.0001). For meningioma, the weak positive trend for ELF in the 1–4 year time window disappeared (OR ≥ 90% vs < 25 % = 1.07, 95% CI 0.86, 1.34) and was no longer significant (p = 0.28).
The weak inverse association between ELF in the 10+ year time window and glioma attenuating when subjects judged to be reticent and unresponsive were excluded from analyses may reflect some form of reporting bias among these subjects. Reticence and unresponsiveness was based solely on the personal opinion of the 130 interviewers in INTEROCC study countries.
Limitations of using a JEM include exposure misclassification, although it is likely non-differential. A US study modified JEM values based on time and distance information for ELF sources for 24% of jobs (19). This increased the ELF exposure category for 27% of jobs and decreased it for 15% of jobs. The modification also did not include the magnitude of a source’s ELF emissions, which may introduce further misclassification. The representativeness of the JEM across different countries and time periods is also unclear. Although here we relied on the overall JEM estimates, in sensitivity analyses using country-specific estimates where they were available in the JEM, as well as sex and time-period specific estimates, results were virtually identical to those obtained here. This study’s focus on the TWA of the ELF magnetic field resultant also neglects other potentially important aspects of electromagnetic environment such as the magnetic field frequency spectrum, its polarization, intermittency, electric fields, shocks, contact currents, and neighboring bands of the EM spectrum. There is little evidence for a role of ELF electric fields in carcinogenesis (40).
In conclusion, in this large-scale study we observed no association with lifetime occupational ELF exposure. However, results from this, and several smaller previous studies showed positive associations between ELF in the more recent past and glioma, and probably with meningioma. Future work to better understand possible biological mechanims of action, interactions with other occupational exposures, associations with other occupational EMF exposures including intermediate and RFs, and to consider inter-individual variation in ELF exposure is needed.
Supplementary Material
Acknowledgments
Financial support: Michelle C Turner was funded by a Government of Canada Banting Postdoctoral Fellowship. The INTEROCC study was funded by the National Institutes for Health (NIH) Grant No. 1R01CA124759 (PI E Cardis). Coding of the French occupational data was in part funded by AFSSET (Convention N° ST-2005-004). The INTERPHONE study was supported by funding from the European Fifth Framework Program, ‘Quality of Life and Management of Living Resources’ (contract 100 QLK4-CT-1999901563) and the International Union against Cancer (UICC). The UICC received funds for this purpose from the Mobile Manufacturers’ Forum and GSM Association. In Australia, funding was received from the Australian National Health and Medical Research 5 Council (EME Grant 219129) with funds originally derived from mobile phone service license fees; a University of Sydney Medical Foundation Program; the Cancer Council NSW and The Cancer Council Victoria. In Canada funding was received from the Canadian Institutes of Health Research (project MOP-42525); the Canada Research Chair programme; the Guzzo-CRS Chair in Environment and Cancer; the Fonds de la recherche en santé du Québec; the Canadian Institutes of Health Research (CIHR), the latter including partial support from the Canadian Wireless Telecommunications Association; the NSERC Chair in Risk Science at the University of Ottawa. In France, funding was received by l’Association pour la Recherche sur le Cancer (ARC) (Contrat N85142) and three network operators (Orange, SFR, Bouygues Telecom). In Germany, funding was received from the German Mobile Phone Research Program (Deutsches Mobilfunkforschungsprogramm) of the German Federal Ministry for the Environment, Nuclear 45 Safety, and Nature Protection; the Ministry for the Environment and Traffic of the state of Baden- Wurttemberg; the Ministry for the Environment of the state of North Rhine-Westphalia; the MAIFOR Program (Mainzer Forschungsforderungsprogramm) of the University of Mainz. In New Zealand, funding was provided by the Health Research Council, Hawkes Bay Medical Research Foundation, the Wellington Medical Research Foundation, the Waikato Medical Research Foundation and the Cancer Society of New Zealand. Additional funding for the UK study was received from the Mobile Telecommunications, Health and Research (MTHR) program, funding from the Health and Safety Executive, the Department of Health, the UK Network Operators (O2, Orange, T-Mobile, Vodafone, ‘3’) and the Scottish Executive.
Rodrigo Villegas of CREAL for conducting preliminary analyses. The authors would like to thank Avital Jarus-Hakak (Israel), Louise Nadon (Canada), Hélène Tardy (France), Florence Samkange-Zeeb (Germany), and Anne Sleeuwenhoek (UK), who coded the occupations or assisted in the data clean-up. We are grateful to Mary McBride (Canada) and Drs Bruce Armstrong (Australia), Maria Blettner (Germany), Alistair Woodward (New Zealand) and Patricia McKinney (UK) for the use of the occupational data from their INTERPHONE study centres for the INTEROCC project; and Michael Kelsh (US), Kjell Hansson Mild (Sweden), and Michael Yost (US) who provided expert judgments of ELF for some job titles.
Footnotes
Conflict of Interest: The authors have no conflict of interest to declare.
References
- 1.Bondy M, Scheurer M, Malmer B, Barnholtz-Sloan JS, Davis FG, Il’yasova D, et al. Brain tumor epidemiology: consensus from the brain tumor epidemiology consortium (BTEC) Cancer. 2008;113:1953–68. doi: 10.1002/cncr.23741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Shin H, Bray F, Forman D, Mathers C, Parkin D. GLOBOCAN 2008 v2.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10. Lyon, France: International Agency for Research on Cancer; 2010. Available from: http://globocan.iarc.fr. [Google Scholar]
- 3.Kohler B, Ward E, McCarthy B, Schymura MJ, Ries LAG, Eheman C, et al. Annual report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst. 2011;103:714–36. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braganza M, Kitahara C, Berrington de Gonzalez A, Inskip P, Johnson K, Rajaraman P. Ionizing radiation and the risk of brain and central nervous system tumors: a systematic review. Neuro Oncol. 2012;14:1316–24. doi: 10.1093/neuonc/nos208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preston D, Shimizu Y, Pierce D, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950–1997. Radiat Res. 2003;160:381–407. doi: 10.1667/rr3049. [DOI] [PubMed] [Google Scholar]
- 6.Sienkiewicz Z, Schuz J, Poulsen A, Cardis E. Risk analysis of human exposure to electromagnetic fields (revised) European Health Risk Assessment Network on Electromagnetic Field Exposure; 2012. Available from: http://efhran.polimi.it/docs/EFHRAN_D2_final.pdf. [Google Scholar]
- 7.McLaughlin JK, Malker HS, Blot WJ, Malker BK, Stone BJ, Weiner JA, et al. Occupational risks for intracranial gliomas in Sweden. J Natl Cancer Inst. 1987;78:253–7. [PubMed] [Google Scholar]
- 8.Tornqvist S, Knave B, Ahlbom A, Persson T. Incidence of leukaemia and brain tumours in some “electrical occupations”. Br J Ind Med. 1991;48:597–603. doi: 10.1136/oem.48.9.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tynes T, Andersen A, Langmark F. Incidence of cancer in Norwegian workers potentially exposed to electromagnetic fields. Am J Epidemiol. 1992;136:81–8. doi: 10.1093/oxfordjournals.aje.a116423. [DOI] [PubMed] [Google Scholar]
- 10.Röösli M, Lörtscher M, Egger M, Pfluger D, Schreier N, Lortscher E, et al. Leukaemia, brain tumours and exposure to extremely low frequency magnetic fields: cohort study of Swiss railway employees. Occup Environ Med. 2007;64:553–9. doi: 10.1136/oem.2006.030270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hakansson N, Floderus B, Gustavsson P, Johansen C, Olsen JH. Cancer incidence and magnetic field exposure in industries using resistance welding in Sweden. Occup Environ Med. 2002;59:481–6. doi: 10.1136/oem.59.7.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansen C, Raaschou Nielsen O, Olsen JH, Schuz J. Risk for leukaemia and brain and breast cancer among Danish utility workers: a second follow-up. Occup Environ Med. 2007;64:782–4. doi: 10.1136/oem.2006.029116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Floderus B, Persson T, Stenlund C, Wennberg A, Ost A, Knave B. Occupational exposure to electromagnetic fields in relation to leukemia and brain tumors: a case-control study in Sweden. Cancer Causes Control. 1993;4:465–76. doi: 10.1007/BF00050866. [DOI] [PubMed] [Google Scholar]
- 14.Karipidis KK, Benke G, Sim MR, Yost M, Giles G. Occupational exposure to low frequency magnetic fields and the risk of low grade and high grade glioma. Cancer Causes Control. 2007;18:305–13. doi: 10.1007/s10552-006-0106-7. [DOI] [PubMed] [Google Scholar]
- 15.Karipidis KK, Benke G, Sim MR, Kauppinen T, Giles G. Occupational exposure to ionizing and nonionizing radiation and risk of glioma. Occup Med. 2007;57:518–24. doi: 10.1093/occmed/kqm078. [DOI] [PubMed] [Google Scholar]
- 16.Villeneuve P, Agnew D, Johnson K, Mao Y the Canadian Cancer Registries Epidemiology Research Group. Brain cancer and occupational exposure to magnetic fields among men: results from a Canadian population-based case-control study. Int J Epidemiol. 2002;31:210–7. doi: 10.1093/ije/31.1.210. [DOI] [PubMed] [Google Scholar]
- 17.Baldi I, Coureau G, Jaffre A, Gruber A, Ducamp S, Provost D, et al. Occupational and residential exposure to electromagnetic fields and risk of brain tumors in adults: a case-control study in Gironde, France. Int J Cancer. 2011;129:1477–84. doi: 10.1002/ijc.25765. [DOI] [PubMed] [Google Scholar]
- 18.Kheifets L, Monroe J, Vergara X, Mezei G, Afifi A. Occupational electromagnetic fields and leukemia and brain cancer: an update to two meta-analyses. J Occup Environ Med. 2008;50:677–88. doi: 10.1097/JOM.0b013e3181757a27. [DOI] [PubMed] [Google Scholar]
- 19.Coble J, Dosemeci M, Stewart P, Blair A, Bowman J, Fine HA, et al. Occupational exposure to magnetic fields and the risk of brain tumors. Neuro Oncol. 2009;11:242–9. doi: 10.1215/15228517-2009-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koeman T, van den Brandt P, Slottje P, Schouten LJ, Goldbohm RA, Kromhout H, et al. Occupational extremely low-frequency magnetic field exposure and selected cancer outcomes in a prospective Dutch cohort. Cancer Causes Control. 2013 doi: 10.1007/s10552-013-0322-x. [DOI] [PubMed] [Google Scholar]
- 21.Sorahan T. Magnetic fields and brain tumour risks in UK electricity supply workers. Occup Med. 2014;64:157–65. doi: 10.1093/occmed/kqu003. [DOI] [PubMed] [Google Scholar]
- 22.IARC. Non-ionizing radiation, part 1: static and extremely low-frequency (ELF) electric and magnetic fields. IARC Monogr Eval Carcinog Risks Hum. 2002;80:1–395. [PMC free article] [PubMed] [Google Scholar]
- 23.Ahlbom A, Bridges J, de Seze R, Hillert L, Juutilainen J, Mattsson MO, et al. Possible effects of electromagnetic fields (EMF) on human health -- opinion of the scientific committee on emerging and newly identified health risks (SCENIHR) Toxicology. 2008;246:248–50. doi: 10.1016/j.tox.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 24.WHO. Extremely low frequency fields. Geneva: World Health Organization; 2007. Environmental health criteria 238. [Google Scholar]
- 25.Poulletier de Gannes F, Lagroye I, Veyret B. D3 - Report on the analysis of risks associated to exposure to EMF: in vitro and in vivo (animals) studies. European Health Risk Assessment Network on Electromagnetic Fields Exposure; 2010. Available from: http://efhran.polimi.it/docs/IMS-EFHRAN_09072010.pdf. [Google Scholar]
- 26.Feychting M, Forssen U, Floderus B. Occupational and residential magnetic field exposure and leukemia and central and nervous system tumors. Epidemiology. 1997;8:384–9. doi: 10.1097/00001648-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Savitz D, Cai J, van Wijngaarden E, Loomis D, Mihlan G, Dufort V, et al. Case-cohort analysis of brain cancer and leukemia in electric utility workers using a refined magnetic field job-exposure matrix. Am J Ind Med. 2000;38:417–25. doi: 10.1002/1097-0274(200010)38:4<417::aid-ajim7>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 28.Sorahan T, Nichols L, van Tongeren M, Harrington J. Occupational exposure to magnetic fields relative to mortality from brain tumours: updated and revised findings from a study of United Kingdom electricity generation and transmission workers, 1973–97. Occup Environ Med. 2001;58:626–30. doi: 10.1136/oem.58.10.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Theriault G, Goldberg M, Miller A, Armstrong B, Guenel P, Deadman J, et al. Cancer risks associated with occupational exposure to magnetic fields among electric utility workers in Ontario and Quebec, Canada, and France: 1970–1989. Am J Epidemiol. 1994;139:550–72. doi: 10.1093/oxfordjournals.aje.a117046. [DOI] [PubMed] [Google Scholar]
- 30.Cardis E, Richardson L, Deltour I, Armstrong B, Feychting M, Johansen C, et al. The INTERPHONE study: design, epidemiological methods, and description of the study population. Eur J Epidemiol. 2007;22:647–64. doi: 10.1007/s10654-007-9152-z. [DOI] [PubMed] [Google Scholar]
- 31.McLean D, van Tongeren M, Richardson L, Cardis E. INTEROCC study group. Evaluation of the quality and comparability of job coding across seven countries in the INTEROCC study. EPICOH 2011: 23rd International Conference on Epidemiology in Occupational Health; 7–9 September 2011; Oxford, United Kingdom: University of Oxford; [Google Scholar]
- 32.Bowman J, Touchstone J, Yost M. A population-based job exposure matrix for power-frequency magnetic fields. J Occup Environ Hyg. 2007;4:715–28. doi: 10.1080/15459620701528001. [DOI] [PubMed] [Google Scholar]
- 33.Treiman D. Occupational Prestige in Comparative Perspective. New York: Academic Press; 1977. [Google Scholar]
- 34.Lacourt A, Cardis E, Pintos J, Richardson L, Kincl L, Benke G, et al. INTEROCC case- control study: lack of association between glioma tumors and occupational exposure to selected combustion produces, dusts and other chemical agents. BMC Public Health. 2013;13:340. doi: 10.1186/1471-2458-13-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McLean D, Fleming S, Turner MC, Kincl L, Richardson L, Benke G, et al. Occupational solvent exposure and risk of meningiona. Results from the INTEROCC study. Occup Environ Med. 2014;71:253–8. doi: 10.1136/oemed-2013-101780. [DOI] [PubMed] [Google Scholar]
- 36.Turner MC, Krewski D, Armstrong B, Chetrit A, Hours M, McBride M, et al. Allergy and brain tumors in the INTERPHONE study: Australia, Canada, France, Israel, and New Zealand. Cancer Causes Control. 2013;24:949–60. doi: 10.1007/s10552-013-0171-7. [DOI] [PubMed] [Google Scholar]
- 37.van Tongeren M, Kincl L, Richardson L, Benke G, Figuerola J, Kauppinen T, et al. Assessing occupational exposure to chemicals in an international study of brain tumors. Ann Occup Hyg. 2013;57:610–26. doi: 10.1093/annhyg/mes100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SAS, version 9.3. Cary, NC: SAS Institute, Inc; 2010. [Google Scholar]
- 39.Wigertz A, Lonn S, Hall P, Feychting M. Non-participant characteristics and the association between socioeconomic factors and brain tumour risk. J Epidemiol Community Health. 2010;64:736–43. doi: 10.1136/jech.2008.085845. [DOI] [PubMed] [Google Scholar]
- 40.Kheifets L, Renew D, Sias G, Swanson J. Extremely low frequency electric fields and cancer: assessing the evidence. Bioelectromagnetics. 2010;31:89–101. doi: 10.1002/bem.20527. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.