Abstract
Craniosynostosis affecting the lambdoid suture is uncommon. The definition of lambdoid craniosynostosis solely applies to those cases demonstrating true suture obliteration, similar to other forms of craniosynostosis. In patients presenting with posterior plagiocephaly, true lambdoid craniosynostosis must be differentiated from the much more common positional molding. It can occur in a unilateral form, a bilateral form, or as part of a complex craniosynostosis. In children with craniofacial syndromes, synostosis of the lambdoid suture most often is seen within the context of a pansynostotic picture. Chiari malformations are commonly seen in multisutural and syndromic types of craniosynostosis that affect the lambdoid sutures. Posterior cranial vault remodeling is recommended to provide adequate intracranial volume to allow for brain growth and to normalize the skull shape. Although many techniques have been described for the correction of lambdoid synostosis, optimal outcomes may result from those techniques based on the concept of occipital advancement.
Keywords: lambdoid craniosynostosis, Mercedes Benz pattern craniosynostosis, posterior plagiocephaly
Population-based studies estimate the birth prevalence of craniosynostosis in the United States around 1 in 2300 births.1 Of these, nonsyndromic craniosynostosis involving the lambdoid suture is uncommon, representing 1% to 5% of the craniosynostosis population. It can occur in a unilateral form, a bilateral form, or as part of a complex craniosynostosis. In children with craniofacial syndromes, synostosis of the lambdoid suture most often is seen within the context of a pansynostotic picture. Ancient skeletal remains dated to 530,000 years ago demonstrate the earliest known case of lambdoid craniosynostosis.2
Anatomy and Physiology of the Lambdoid Suture
The bones of the cranium are well developed by the fifth month of gestation.3 Posterior skull development in neonates occurs through the growth of the occipital bone, posterior parietal bones, and the cranial base. Growth is facilitated by the paired lambdoid sutures. Each lambdoid suture connects with the posterior portion of the sagittal suture and the ipsilateral parietomastoid and occipitomastoid sutures along the cranial base. The junction of the lambdoid and sagittal sutures represents the posterior fontanel that typically closes shortly after birth.
Normal or physiologic development of the lambdoid suture demonstrates the period of greatest proliferative activity is around 3 months of age. This may be due to the especially accelerated growth of the cerebellum as compared with the forebrain and brainstem during the first 2 years.4
At 3 months of age, the active front of new bone formation adjacent to the suture widens, resulting in an endocranial hump or ridge. The bone front consists of one or more tongues of bone on each side, which overlap and show early interdigitation.5
Chiari Malformation
Chiari malformations are commonly seen in multisutural and syndromic types of craniosynostosis, which affect the lambdoid sutures.6 Craniosynostosis of the lambdoid suture, especially when bilateral, may lead to a small and shallow posterior cranial fossa due to underdevelopments on the occipital bone.7 8 9
Overcrowding of the posterior fossa secondary to premature sutural fusion, along with a disproportion of hindbrain growth, may be responsible for the pathogenesis of the Chiari I malformation in children with craniosynostosis.4 In most cases, the cerebellar tonsillar herniation is not present at birth, but appears to be acquired and progressive, paralleling the modification of the posterior cranium. This downward herniation of neural tissue through the foramen magnum may lead to symptoms such as headaches and neck pain as well as to more severe neurologic problems, including weakness and lower cranial nerve dysfunction (Fig. 1).
Fig. 1.
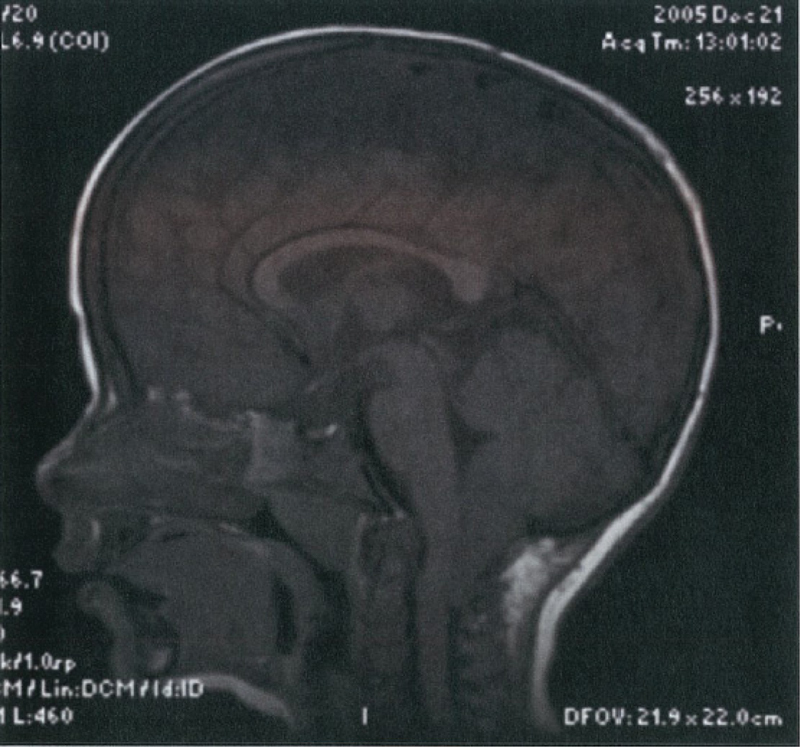
Magnetic resonance image revealing cerebellar tonsillar herniation in child with the Mercedes Benz pattern of craniosynostosis one year after surgical correction. (Reprinted with permission from Rhodes JL, Kolar JC, Fearon JA. Mercedes Benz pattern craniosynostosis. Plast Reconstr Surg 2010 Jan;125(1):302)
Functional Craniosynostosis and “The Sticky Suture”
Until the mid-1990s, an inconsistent understanding of lambdoid sutural pathology led to the development of a body of literature attempting to show that lambdoid craniosynostosis was distinct from other synostosis and did not require true bony fusion of the suture. The concept of a functional abnormality of the suture, demonstrated by a “sticky” suture was thought to be functionally significant.10 Radiographic signs of a functional synostosis were thought to include thickening and sclerosis of the inner table of the suture.10 11 It is now thought that these findings are age appropriate in the spectrum of normal sutural development. As further understanding of lambdoid sutural pathology developed, the definition of lambdoid craniosynostosis now solely applies to those cases demonstrating true sutural obliteration, similar to other forms of craniosynostosis.12 13 Criteria for the radiographic differentiation of nonsynostotic occipital plagiocephaly from true lambdoid craniosynostosis can be found in Losee et al.13
Presentation
History
It is imperative to obtain a thorough history of the head-shape abnormality as this is helpful in distinguishing the synostotic from the nonsynostotic form of plagiocephaly. In positional plagiocephaly, parents are typically able to recall a round-head shape antenatally, with the flattening developing over the ensuing weeks to months. Amelioration of the deformation may be appreciable by 6 months of age, especially with aggressive repositioning measures. True lambdoid craniosynostosis is present at birth and is a progressive deformity.
Clinical Features
Craniosynostosis versus Deformational Molding
The term “posterior plagiocephaly” refers to a generally asymmetric shape of the posterior cranium. This term can apply to a distinct phenotype observed in true lambdoid craniosynostosis as well as phenotypic changes caused by nonsynostotic causes, such as positional molding. Typically, in cases of positional posterior plagiocephaly due to deformation causes, the ear is displaced anteriorly on the side of occipital flattening and no mastoid bulge is present (Fig. 2).
Fig. 2.
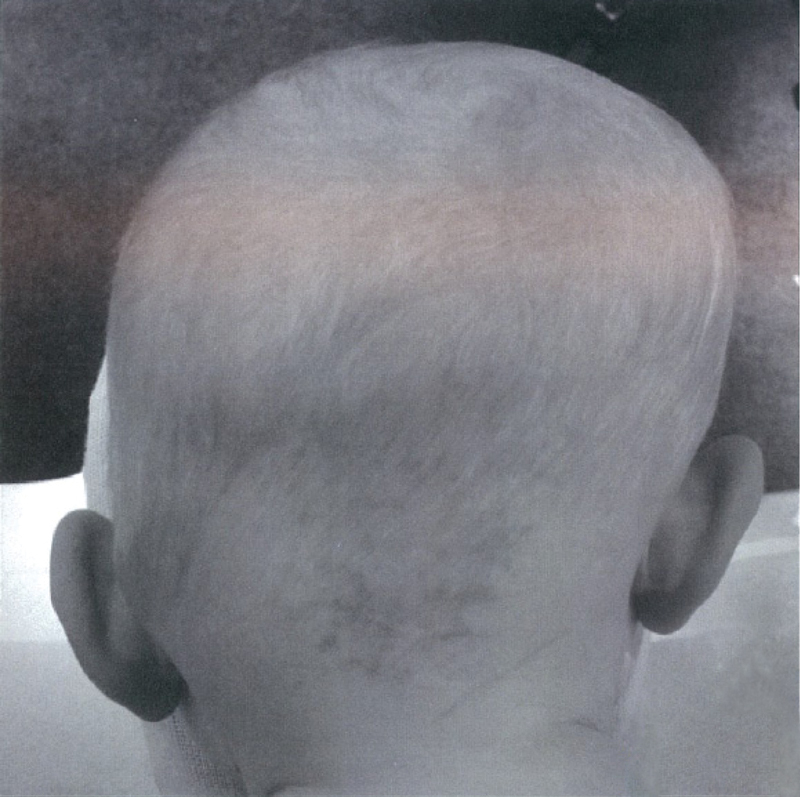
Posterior view. Infant with left lambdoid synostosis. Note right parietal bossing, left occipitomastoid bossing, left inferior tilt of skull base resulting in inferior displacement of left ear, and compensatory deformation of cervical spine.
We use the term “positional plagiocephaly” to refer to posterior plagiocephaly caused by positional modeling to ensure clear communications with pediatricians.
The prevalence of the nonsynostotic form of posterior plagiocephaly seen today is significant, and has been reported as high as 22% of infants at 7 weeks of age.14 This is estimated to be a 10-fold increase from pre-1992 levels and has been related to the supine sleeping position recommended by the American Academy of Pediatrics since 1992 to reduce the incidence of the sudden infant death syndrome.15 The distinction between the two forms of posterior plagiocephaly is critical, as lambdoid craniosynostosis requires surgical treatment, whereas deformation plagiocephaly generally improves with time and the use of conservative measures. These measures include such things as repositioning, or in more severe cases, molding helmets. Torticollis also contributes to the incidence of nonsynostotic posterior plagiocephaly. Torticollis involves a shortened sternocleidomastoid muscle, which can result in flattening of the temporal and occipital region. The anterior deformity typically is greater than the posterior deformity and is found on the side of the abnormality. This usually mild deformity improves with neck exercises and physical therapy. The muscle rarely needs to be divided or lengthened. The natural history of positional plagiocephaly demonstrates a significant drop in the prevalence with time, irrespective of any intervention. By 2 years of age, the prevalence decreases to as low as 3%.14
Unilateral
The following phenotypic features typify lambdoid craniosynostosis: ipsilateral occipitomastoid bulge, compensatory contralateral parietal and frontal bossing, and shifting of the ear inferiorly and posteriorly (although this is not always the case and should be not considering pathognomonic).12 The contralateral parietal and ipsilateral occipitomastoid bossing cause the head to be wider posteriorly than anteriorly, resulting in a trapezoid head shape when viewed from above. Notably, there is also a reduction in posterior skull height on the affected side.
Bilateral
It is estimated that 15% of cases of lambdoid craniosynostosis are bilateral.10 In bilateral cases, the entire occipital region is flat and widened.16 This condition is associated with elongation of the vertex to accommodate the growing brain. Both ears are displaced anteriorly and inferiorly.17 Increased intracranial pressure has been reported in up to 86% of cases.18 The incidence of Chiari I malformation in bilateral lambdoid craniosynostosis is not currently known, but is presumably elevated.
Bilateral Lambdoid and Sagittal Craniosynostosis
“Mercedes Benz” Pattern
This complex craniosynostosis is rare, but presents with a markedly distinct clinical picture. Affected patients present with a varying degree of anterior turricephaly (an increase in the height of the head) with mild brachycephaly (a shortening of the length of the head), and a diminished posterior skull height, a reduced posterior skull width, and occipital flattening (Figs. 3 and 4).19 In the largest series published to date, two-thirds of patients have evidence of a Chiari I malformation on imaging performed within the first year of life. Over half of this group have gone on to require neurosurgical decompression secondary to the development of symptoms (i.e., central sleep apnea or syringomyelia).19
Fig. 3.
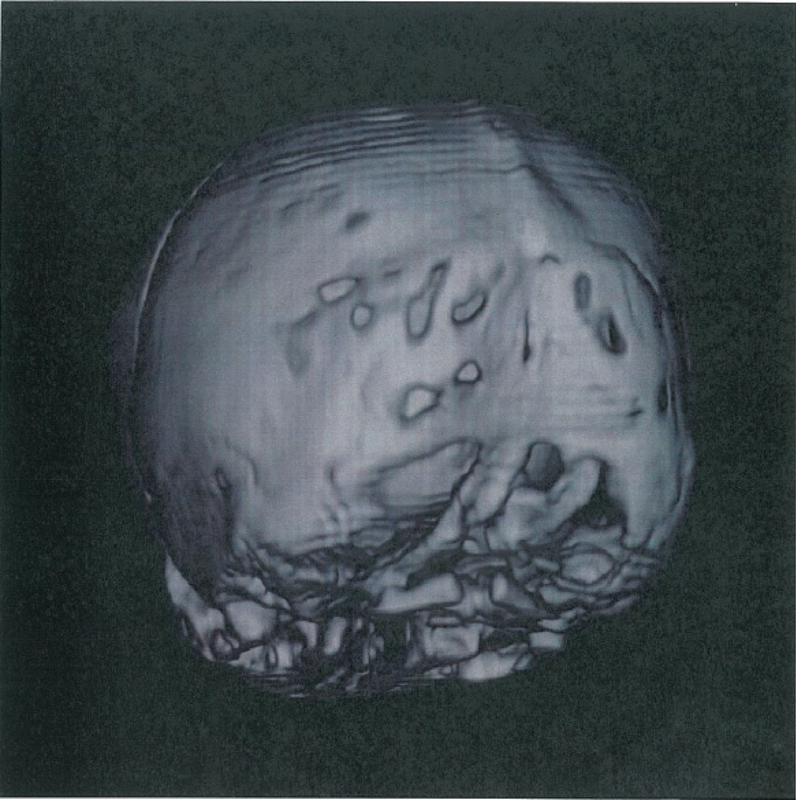
Radiographic findings of the Mercedes Benz pattern of synostosis. A three-dimensional computed tomography scan revealing sagittal and bilateral lambdoid craniosynostosis. (Reprinted with permission from Rhodes JL, Kolar JC, Fearon JA. Mercedes Benz pattern craniosynostosis. Plast Reconstr Surg 2010 Jan;125(1):301)
Fig. 4.

Phenotypic findings of the Mercedes Benz pattern of synostosis include anterior tifficephaly (A) and a sublambda indentation (B). (Reprinted with permission from Rhodes JL, Kolar JC, Fearon JA. Mercedes Benz pattern craniosynostosis. Plast Reconstr Surg 2010 Jan;125(1):301.)
Radiology
The diagnosis of lambdoid craniosynostosis can be made on clinical examination alone by experienced craniofacial surgeons.20 However, when the diagnosis is in question, a computed tomography (CT) scan can confirm the presence of a true lambdoid craniosynostosis from plagiocephaly due to molding with patent sutures (Fig. 5).
Fig. 5.
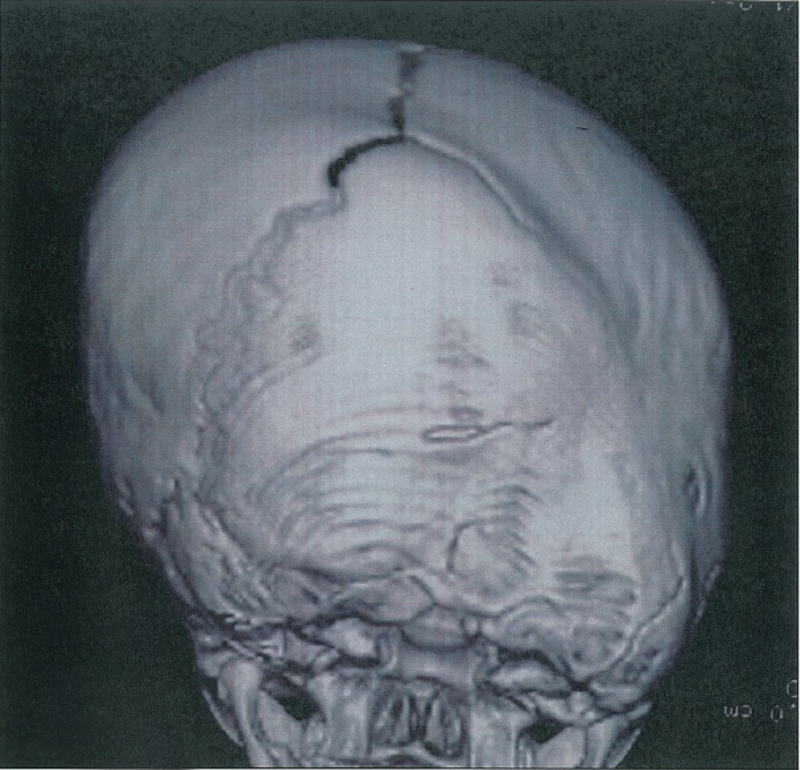
Three-dimensional computed tomography scans, posterior view. Patient with right lambdoid synostosis. Note external ridging and right inferior tilt of skull base.
Treatment
The goal of treatment is to provide adequate intracranial volume to allow for brain growth and to normalize the skull shape. The optimal age for surgical intervention remains somewhat controversial, but in the opinion of the senior author (JAF) correction between 10 and 12 months of age minimizes relapse rates. If there is evidence of increased intracranial pressure, which as a bulging fontanels or the presence of a Chiari I malformation with a significant number of central sleep apneas documented on a sleep study, operative intervention in indicated at an earlier time. The authors believe that preoperative magnetic resonance imaging (MRI) is imperative to assess for the presence of a Chiari malformation and to evaluate the position of the torcula as well as the sagittal and transverse sinus locations.20
Currently, we recommend the preoperative use of recombinant human erythropoietin to stimulate an increase in red cell volume.21 In addition, the use of intraoperative blood recycling devices is important to minimize the likelihood of an allogenic transfusion.22 23 Anthropometric analysis published for other single sutural synostoses show diminished postoperative skull growth, with a tendency for the skull to recapitulate the pretreatment deformity, suggesting the need to overcorrect the presenting deformity.19 24 25
Although many techniques have been described for the correction of lambdoid synostosis, optimal outcomes may result from those techniques based on the concept of occipital advancement.18 26
This concept borrows from the technique of fronto-orbital advancement in that a bandeau is selected to define the reconstruction.27 A posterior bandeau is harvested either horizontally from the middle of the occipital region, or from the vertex of the skull in the coronal plane, depending upon which will give the best correction (Figs. 6 and 7). A large bone flap, similar in shape to the bifrontal flap taken with an anterior cranial vault reconstruction, is removed from the superior-aspect half of the posterior cranium (Fig. 8). Another bone flap is removed from the inferior aspect of the posterior cranium. The bandeau is rotated 180 degrees so that the flat side is now overcorrected posterolaterally (Fig. 9). The larger upper bone flap is typically reversed as well, allowing overcorrection of the vertical height discrepancy. The reconstruction is then completed below the bandeau (Fig. 10). Emphasis is placed on ensuring overcorrection of the posterior flatness as well as the ipsilateral reduction in skull height.
Fig. 6.
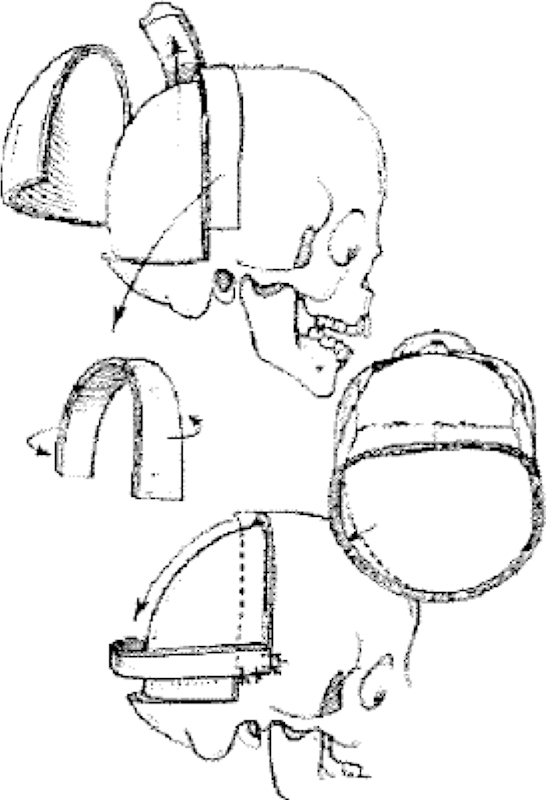
Lambdoid synostosis is corrected by first cutting a neobandeau from the vertex of the skull. This new bandeau is then rotated 180 degrees so that the right side is switched to the left, and then rotated down 90 degrees in a “bucket handle” repair. Bone grafts are placed above and below the new bandeau, completing the reconstruction. (Reprinted with permission from Fearon JA. Rigid Fixaton of the calvaria in craniosynostosis without using “rigid” fixation. Plast Reconstr Surg 2003;11(1):30.)
Fig. 7.

Design template for harvest of posterior bandeau.
Fig. 8.
Design template for superior craniotomy.
Fig. 9.

Overcorrection of posterior flatness established by inset of bandeau.
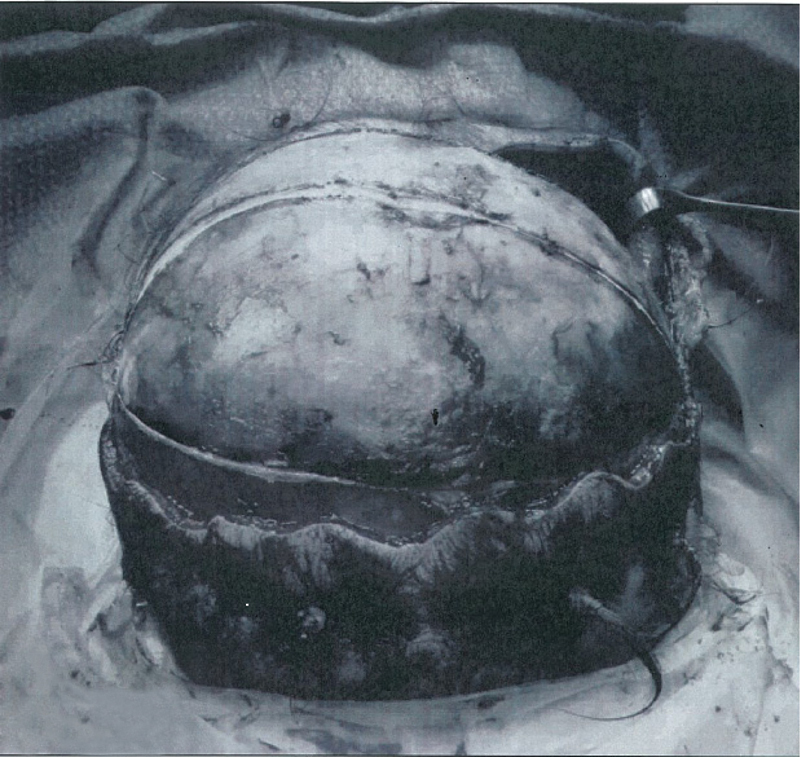
Fig. 10.

Completed calvarial reconstruction.
As both the sagittal and paired transverse sinuses can be partially embedded in the occipital bone, the dura must be meticulously dissected from the bone.
Surgical Treatment of Mercedes-Benz-Pattern Craniosynostosis
Surgical correction of this pattern of craniosynostosis needs to be quite different from that of an isolated sagittal synostosis, with skull elongation instead of shortening; it is also different from the surgical correction of a bilateral lambdoid synostosis (described above). A posterior cranial vault remodeling procedure is performed that is tailored to the observed deformity. Primary goals included sagittal lengthening as well as widening and elevation of the posterior cranium.
The senior author (JAF) has elected to consider primary repairs for children with Mercedes-Benz-pattern craniosynostosis at 8 to 10 months of age, based on concerns for potentially adverse sequelae, such as raised intracranial pressure and the development of an anomalous compensatory growth patterns (progressive anterior turricephaly that might require an additional corrective procedure), which may potentially arise if corrected at a later age. Unlike conventional isolated sagittal synostosis repairs where an anteroposterior reduction in skull length is sought, this pattern of trisutural fusion requires sagittal elongation of the skull. Consideration is given to a simultaneous enlargement of the foramen magnum, given the high potential for future Chiari development. Preoperative MRI scans are recommended for affected patients, with annual to biennial MRI surveillance throughout childhood.19 When cerebellar tonsillar herniation is identified, we recommend overnight sleep studies to assess for central sleep apnea, and additional spinal MRI scans to screen for a potential syringomyelia.
Outcomes
Posterior cranial vault remodeling utilizing a bandeau, based on occipital advancement techniques, has demonstrated the most consistently favorable aesthetic outcomes.18 26 In a series of 21 patients, normalization of all the preoperatively elevated intracranial pressures was found.18 Additionally, a tendency toward improved neurodevelopment, as measured by the Bayley Scales of Infant Development-II, has also been observed.18
Conclusion
Lambdoid synostosis, although rare, must be recognized and differentiated from posterior plagiocephaly. Surgical intervention is indicated to correct potentially increased intracranial pressure as well as to ameliorate progression of a calvarial deformity. Due to the potential difficulty in diagnosis, prompt referral to a center with an experienced team is imperative.
References
- 1.Boulet S L, Rasmussen S A, Honein M A. A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet A. 2008;146A(8):984–991. doi: 10.1002/ajmg.a.32208. [DOI] [PubMed] [Google Scholar]
- 2.Gracia A, Martínez-Lage J F, Arsuaga J L, Martínez I, Lorenzo C, Pérez-Espejo M A. The earliest evidence of true lambdoid craniosynostosis: the case of “Benjamina”, a Homo heidelbergensis child. Childs Nerv Syst. 2010;26(6):723–727. doi: 10.1007/s00381-010-1133-y. [DOI] [PubMed] [Google Scholar]
- 3.Nemzek W R, Brodie H A, Hecht S T, Chong B W, Babcook C J, Seibert J A. MR, CT, and plain film imaging of the developing skull base in fetal specimens. AJNR Am J Neuroradiol. 2000;21(9):1699–1706. [PMC free article] [PubMed] [Google Scholar]
- 4.Cinalli G, Renier D, Sebag G, Sainte-Rose C, Arnaud E, Pierre-Kahn A. Chronic tonsillar herniation in Crouzon's and Apert's syndromes: the role of premature synostosis of the lambdoid suture. J Neurosurg. 1995;83(4):575–582. doi: 10.3171/jns.1995.83.4.0575. [DOI] [PubMed] [Google Scholar]
- 5.Hinton D R, Becker L E, Muakkassa K F, Hoffman H J. Lambdoid synostosis. Part 1. The lambdoid suture: normal development and pathology of “synostosis”. J Neurosurg. 1984;61(2):333–339. doi: 10.3171/jns.1984.61.2.0333. [DOI] [PubMed] [Google Scholar]
- 6.Cinalli G, Spennato P, Sainte-Rose C. et al. Chiari malformation in craniosynostosis. Childs Nerv Syst. 2005;21(10):889–901. doi: 10.1007/s00381-004-1115-z. [DOI] [PubMed] [Google Scholar]
- 7.Marin-Padilla M, Marin-Padilla T M. Morphogenesis of experimentally induced Arnold—Chiari malformation. J Neurol Sci. 1981;50(1):29–55. doi: 10.1016/0022-510x(81)90040-x. [DOI] [PubMed] [Google Scholar]
- 8.Nishikawa M, Sakamoto H, Hakuba A, Nakanishi N, Inoue Y. Pathogenesis of Chiari malformation: a morphometric study of the posterior cranial fossa. J Neurosurg. 1997;86(1):40–47. doi: 10.3171/jns.1997.86.1.0040. [DOI] [PubMed] [Google Scholar]
- 9.Stovner L J, Bergan U, Nilsen G, Sjaastad O. Posterior cranial fossa dimensions in the Chiari I malformation: relation to pathogenesis and clinical presentation. Neuroradiology. 1993;35(2):113–118. doi: 10.1007/BF00593966. [DOI] [PubMed] [Google Scholar]
- 10.Vander Kolk C A, Carson B S. Lambdoid synostosis. Clin Plast Surg. 1994;21(4):575–584. [PubMed] [Google Scholar]
- 11.McComb J G. Treatment of functional lambdoid synostosis. Neurosurg Clin N Am. 1991;2(3):665–672. [PubMed] [Google Scholar]
- 12.Huang M H Gruss J S Clarren S K et al. The differential diagnosis of posterior plagiocephaly: true lambdoid synostosis versus positional molding Plast Reconstr Surg 1996985765–774., discussion 775–776 [DOI] [PubMed] [Google Scholar]
- 13.Losee J E, Feldman E, Ketkar M. et al. Nonsynostotic occipital plagiocephaly: radiographic diagnosis of the “sticky suture”. Plast Reconstr Surg. 2005;116(7):1860–1869. doi: 10.1097/01.prs.0000191176.62532.5e. [DOI] [PubMed] [Google Scholar]
- 14.Bialocerkowski A E, Vladusic S L, Wei Ng C. Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol. 2008;50(8):577–586. doi: 10.1111/j.1469-8749.2008.03029.x. [DOI] [PubMed] [Google Scholar]
- 15.Carson B S James C S VanderKolk C A Guarnieri M Lambdoid synostosis and occipital plagiocephaly: clinical decision rules for surgical intervention Neurosurg Focus 199722e5, discussion 1, e5 [DOI] [PubMed] [Google Scholar]
- 16.Delashaw J B, Persing J A, Jane J A. Cranial deformation in craniosynostosis. A new explanation. Neurosurg Clin N Am. 1991;2(3):611–620. [PubMed] [Google Scholar]
- 17.Leboucq N, Montoya P, Martinez Y, Castan P, Bourbotte G. Lambdoid craniosynostosis. A 3D-computerized tomographic approach. J Neuroradiol. 1993;20(1):24–33. [PubMed] [Google Scholar]
- 18.Zöller J E, Mischkowski R A, Speder B. Preliminary results of standardized occipital advancement in the treatment of lambdoid synostosis. J Craniomaxillofac Surg. 2002;30(6):343–348. doi: 10.1054/jcms.2002.0326. [DOI] [PubMed] [Google Scholar]
- 19.Rhodes J L, Kolar J C, Fearon J A. Mercedes Benz pattern craniosynostosis. Plast Reconstr Surg. 2010;125(1):299–304. doi: 10.1097/PRS.0b013e3181c2a6aa. [DOI] [PubMed] [Google Scholar]
- 20.Fearon J A, Singh D J, Beals S P, Yu J C. The diagnosis and treatment of single-sutural synostoses: are computed tomographic scans necessary? Plast Reconstr Surg. 2007;120(5):1327–1331. doi: 10.1097/01.prs.0000279477.56044.55. [DOI] [PubMed] [Google Scholar]
- 21.Fearon J A, Weinthal J. The use of recombinant erythropoietin in the reduction of blood transfusion rates in craniosynostosis repair in infants and children. Plast Reconstr Surg. 2002;109(7):2190–2196. doi: 10.1097/00006534-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Fearon J A. Reducing allogenic blood transfusions during pediatric cranial vault surgical procedures: a prospective analysis of blood recycling. Plast Reconstr Surg. 2004;113(4):1126–1130. doi: 10.1097/01.prs.0000110324.31791.5c. [DOI] [PubMed] [Google Scholar]
- 23.Krajewski K, Ashley R K, Pung N. et al. Successful blood conservation during craniosynostotic correction with dual therapy using Procrit and cell saver. J Craniofac Surg. 2008;19(1):101–105. doi: 10.1097/scs.0b013e3180f6112f. [DOI] [PubMed] [Google Scholar]
- 24.Fearon J A, McLaughlin E B, Kolar J C. Sagittal craniosynostosis: surgical outcomes and long-term growth. Plast Reconstr Surg. 2006;117(2):532–541. doi: 10.1097/01.prs.0000200774.31311.09. [DOI] [PubMed] [Google Scholar]
- 25.Fearon J A, Ruotolo R A, Kolar J C. Single sutural craniosynostoses: surgical outcomes and long-term growth. Plast Reconstr Surg. 2009;123(2):635–642. doi: 10.1097/PRS.0b013e318195661a. [DOI] [PubMed] [Google Scholar]
- 26.Goodrich J T, Argamaso R. Lambdoid stenosis (posterior plagiocephaly) and craniofacial asymmetry: long-term outcomes. Childs Nerv Syst. 1996;12(11):720–726. doi: 10.1007/BF00366157. [DOI] [PubMed] [Google Scholar]
- 27.Fearon J A Rigid fixation of the calvaria in craniosynostosis without using “rigid” fixation Plast Reconstr Surg 2003111127–38., discussion 39 [DOI] [PubMed] [Google Scholar]


