Abstract
Familial adenomatous polyposis (FAP) is an autosomal dominant disorder characterized by hundreds of colorectal adenomatous polyps that progress to colorectal cancer. Management of patients with FAP is with a total colectomy. Chemopreventive strategies have been studied in FAP patients in an effort to delay the development of adenomas in the upper and the lower gastrointestinal tract and to prevent recurrence of adenomas in the retained rectum of patients after prophylactic surgery. Sulindac, a nonsteroidal anti-inflammatory drug, causes regression of colorectal adenomas in the retained rectal segment of FAP patients. However, evidence regarding long-term use of this therapy and its effect on the intact colon has been insufficient. We report a case in which the long-term use of sulindac was effective in reducing the size and the number of colonic polyps in patients with FAP without a prophylactic colectomy and polypectomy; we also present a review of the literature.
Keywords: Adenomatous polyposis coli, Sulindac, Therapy, Chemoprevention
INTRODUCTION
Familial adenomatous polyposis (FAP) is an autosomal dominant disease caused by a mutation in the adenomatous polyposis coli (APC) gene located on chromosome 5q21 [1]. This mutation accelerates the initiation of the adenoma-carcinoma sequence, resulting in the development of numerous adenomatous colorectal polyps at a young age. Polyposis will inevitably progress to colorectal cancer if a prophylactic colectomy is not performed. Given the predictability of the development of colorectal cancer in patients with FAP, the safest preventative strategy is surgical resection of the colon when polyposis develops [2]. In 1983, Waddell and Loughry [3] were the first to report sulindac-induced regression of adenomas in patients who underwent a colectomy with ileorectal anastomosis (IRA). However, evidence regarding long-term use of this therapy and its effect on the intact colon is insufficient [4]. In the present study, we report a case of FAP, in which the patient took sulindac without surgery or a polypectomy and showed regression of the colonic adenomas for more than 2 years.
CASE REPORT
A 25-year-old woman visited Department of Internal Medicine, Kyungpook National University Medical Center due to multiple colon polyps that had been detected incidentally. She had been healthy and had no remarkable medical history. According to her family history, her mother had colon cancer, and her brother had undergone a prophylactic colectomy for the treatment of FAP. The results of physical examination and laboratory data, including complete blood count and serum carcinoembryonic antigen level, were all within normal limits. Esophagogastroduodenoscopy showed a normal mucosa finding. Colonoscopy examination revealed hundreds of polyps carpeting the entire colon and rectum, consistent with FAP (Fig. 1). Histologically, these polyps were all proven to be tubular adenomas. Because the standard therapy is a prophylactic total colectomy, we recommended that she undergo a prophylactic surgical treatment. However, the patient was fully aware of the unfavorable effect that a total colectomy had had on her brother. In addition, she was 25 and single. She had no large-sized polyps and no colon cancer. Her family agreed with our second proposal, which was not to perform surgical treatment until the subject was in her late twenties, if there was no apparent development of colonic cancer. Therefore, we delayed the prophylactic colectomy and decided on a treatment with oral sulindac, 100 mg twice a day.
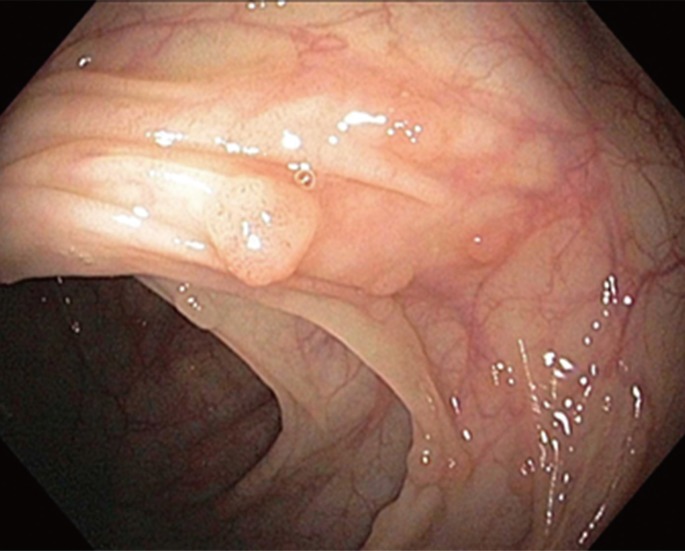
Fig. 1.
Colonoscopy showed hundreds of polyps of various sizes carpeting the entire colon and rectum, which is consistent with familial adenomatous polyposis.
After the sulindac medication had been taken for 5 months, colonoscopy showed that the number and the size of polyps had been drastically decreased and that the polyps had almost completely disappeared (Fig. 2). Sulindac was found to have a sustained effect on the complete regression of colonic adenomas without the need for a polypectomy. Mild nausea was a side effect of the medication. However, after a few days, symptoms had disappeared without treatment. After the sulindac medication had been taken for 25 months, colonoscopy showed several sporadic, tiny polyps (Fig. 3). Thus, the effect of sulindac on the regression of the colonic adenomas had been maintained. We had been continuously treating her with oral sulindac, 100 mg twice a day. Esophagogastroduodenoscopy and colonoscopy were scheduled at regular intervals of one year.
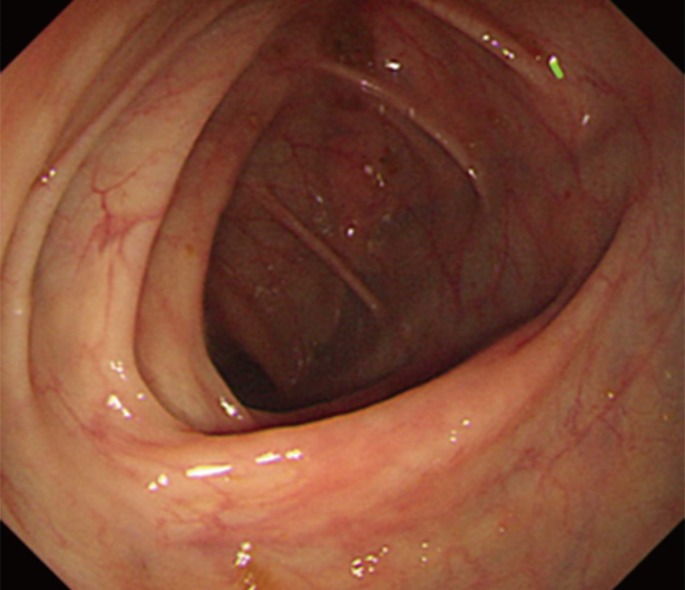
Fig. 2.
After sulindac medication had been taken for 5 months, colonoscopy showed that the number and the size of polyps had been drastically decreased and that the polyps had almost completely disappeared.
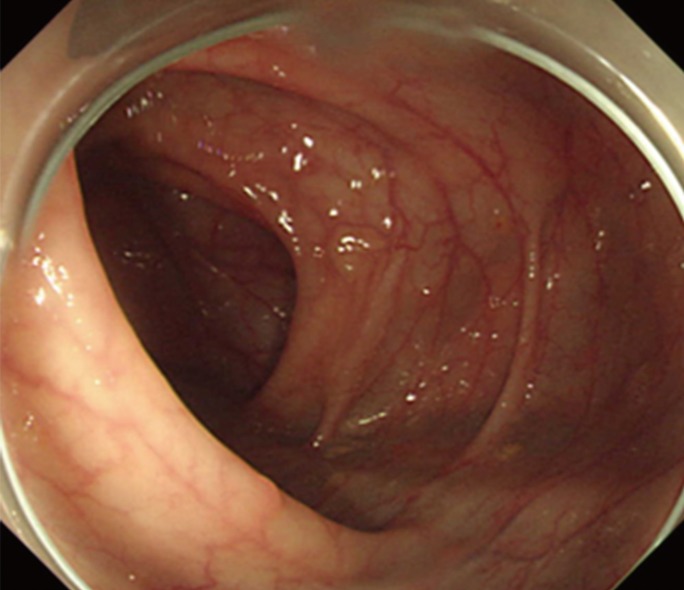
Fig. 3.
After sulindac medication had been taken for 25 months, colonoscopy showed several, sporadic, tiny polyps.
DISCUSSION
Cancer prevention and maintenance of a good quality of life are the main goals in management of patients with clinical or genetic evidence of FAP. The two main options for prophylactic removal of the large intestine are a colectomy with IRA and a proctocolectomy with ileal pouch-anal anastomosis [2]. Chemoprevention is the use of pharmaceuticals or natural agents to prevent or delay the development of cancer in healthy patients. Ideally, the agents used in chemoprevention should be well tolerated, low in toxicity, cheap, and effective. Chemoprevention can play three main roles in patients with FAP: (1) delay of the prophylactic colectomy, (2) prevention of cancer development in the retained rectum in patients after a colectomy with IRA, and (3) prevention of cancer development in the upper gastrointestinal tract, especially the duodenum [5].
Sulindac is a nonsteroidal anti-inflammatory drug (NSAID) that inhibits prostaglandin synthesis. NSAIDs have been studied extensively as chemopreventive agents in patients with FAP. NSAIDs (including sulindac) inhibit cyclooxygenase (COX), a key enzyme in the conversion of arachidonic acid to prostaglandins and other eicosanoids. Prostaglandins appear to play a key role in the adenoma-carcinoma sequence by altering cell adhesion, inhibiting apoptosis, and promoting angiogenesis. Elevated prostaglandin levels are found in many premalignant and malignant lesions, including colorectal adenomas and adenocarcinomas. Sulindac reduces prostaglandin synthesis by inhibiting the expressions of the COX-1 and the COX-2 enzymes [5].
In this case, we administered sulindac for more than 2 years. Regression of the colonic adenomas occurred 5 months after the start of treatment and has continued for more than 20 months since that time. In 1983, Waddell and Loughry [3] reported that sulindac, a NSAID, caused regression of rectal adenomatous polyps in patients with FAP. One patient had diffuse polyposis in an intact colon. In their case, after sulindac therapy for one year, only three small mucosal polyps could be identified by colonoscopy.
The effect of sulindac was confirmed in randomized, double-blind, placebo-controlled studies (Table 1) [6, 7, 8]. One study [6] showed a significant decrease in the number and the size of polyps in the intact colon of 18 patients. However, in all studies, the rate of complete resolution during a treatment period shorter than one year was not so high, and the effect of sulindac proved to be transient and reversible. Several nonrandomized clinical trials have verified the chemoprevention effect of sulindac in FAP patients (Table 2) [9, 10, 11, 12]. Two studies [10, 11] showed apparent effects on the regression of adenomas in the intact colon.
Table 1.
Randomized, placebo-controlled, clinical trials of sulindac chemoprevention in familial adenomatous polyposis patients
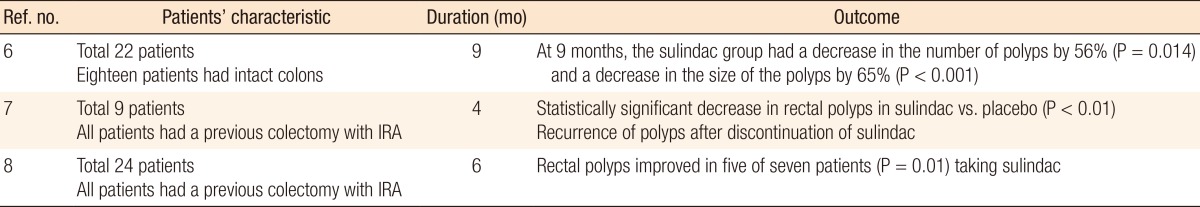
IRA, ileorectal anastomosis.
Table 2.
Nonrandomized, clinical trials of sulindac chemoprevention in familial adenomatous polyposis patients
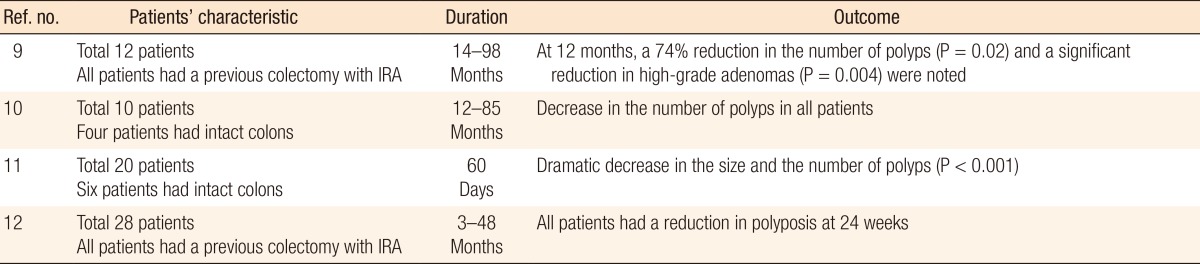
IRA, ileorectal anastomosis.
However, in other studies, whether the effect of sulindac in preventing polyps also applies to carcinomas is not clear. The persistence of an abnormal mucosal proliferation after sulindac therapy, in spite of a reduction in the number of polyps, suggests that caution is needed in assuming a lower risk of rectal cancer in patients with FAP [11]. Accordingly, the longer the period of treatment with sulindac is, the more intensive the surveillance that is necessary. Moreover, two studies have been done on the development of colorectal adenocarcinomas during sulindac therapy with polyp regression. One study [13] reported a patient with FAP who developed a second primary carcinoma in a remnant rectal segment after a colectomy with IRA during sulindac treatment. Despite intensive endoscopic follow-up, the patient developed an adenocarcinoma of the rectum 28 months after the colectomy. This finding may have important implications for our understanding of the development of colon cancer in patients with FAP and the use of sulindac to prevent it. Development of de novo carcinoma in microadenomatous tissue of the rectal mucosa, which bypasses the polyp-cancer sequence, must be considered as a possibility in these patients. The other study [14] reported a patient with FAP in whom a rectal adenocarcinoma developed 15 months after beginning chemoprevention with sulindac. The carcinoma was a metastatic adenocarcinoma in 6 of 20 perirectal lymph nodes, although an endoscopic examination performed 3 months before had been unremarkable. In addition to the carcinoma, the rectal mucosa contained two adenomas and multiple foci of adenomatous changes in the flat mucosa. This study concluded that sulindac may not alter the pathogenesis of FAP. The authors recommended that patients undergoing sulindac chemoprevention be monitored closely, including endoscopic examination with an aggressive biopsy approach, because the absence of polyps does not prove the absence of neoplastic change.
Giardiello et al. [15] reported that sulindac's potential as a primary chemopreventive agent in patients with FAP. Forty-one patients with APC mutations, who were genotypically affected, but were not yet phenotypically affected, were randomized into a group that received a placebo and a group that received sulindac as a primary prophylaxis against the development of colorectal adenomas. After four years of treatment, no significant differences between the two groups were seen. Adenomas had developed in 9 of 21 patients receiving sulindac (43%) and in 11 of 20 patients receiving the placebo (55%, P = 0.54). No significant differences in the mean numbers of polyps and in the sizes of the polyps were noted between the two groups. This result provided no support for the use of NSAIDs such as sulindac for the primary treatment of FAP. The prophylactic colectomy remains the treatment of choice to prevent colorectal cancer in patients with FAP [15].
In conclusion, sulindac cannot replace a prophylactic total colectomy as the primary therapy for treating patients with FAP. However, sulindac therapy may be useful for postponing the total colectomy, especially for a young person who refuses prophylactic surgery or for attenuated FAP.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kinzler KW, Nilbert MC, Su LK, Vogelstein B, Bryan TM, Levy DB, et al. Identification of FAP locus genes from chromosome 5q21. Science. 1991;253:661–665. doi: 10.1126/science.1651562. [DOI] [PubMed] [Google Scholar]
- 2.Vasen HF, Moslein G, Alonso A, Aretz S, Bernstein I, Bertario L, et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP) Gut. 2008;57:704–713. doi: 10.1136/gut.2007.136127. [DOI] [PubMed] [Google Scholar]
- 3.Waddell WR, Loughry RW. Sulindac for polyposis of the colon. J Surg Oncol. 1983;24:83–87. doi: 10.1002/jso.2930240119. [DOI] [PubMed] [Google Scholar]
- 4.Tonelli F, Valanzano R, Messerini L, Ficari F. Long-term treatment with sulindac in familial adenomatous polyposis: is there an actual efficacy in prevention of rectal cancer? J Surg Oncol. 2000;74:15–20. doi: 10.1002/1096-9098(200005)74:1<15::aid-jso4>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 5.Kim B, Giardiello FM. Chemoprevention in familial adenomatous polyposis. Best Pract Res Clin Gastroenterol. 2011;25:607–622. doi: 10.1016/j.bpg.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giardiello FM, Hamilton SR, Krush AJ, Piantadosi S, Hylind LM, Celano P, et al. Treatment of colonic and rectal adenomas with sulindac in familial adenomatous polyposis. N Engl J Med. 1993;328:1313–1316. doi: 10.1056/NEJM199305063281805. [DOI] [PubMed] [Google Scholar]
- 7.Labayle D, Fischer D, Vielh P, Drouhin F, Pariente A, Bories C, et al. Sulindac causes regression of rectal polyps in familial adenomatous polyposis. Gastroenterology. 1991;101:635–639. doi: 10.1016/0016-5085(91)90519-q. [DOI] [PubMed] [Google Scholar]
- 8.Nugent KP, Farmer KC, Spigelman AD, Williams CB, Phillips RK. Randomized controlled trial of the effect of sulindac on duodenal and rectal polyposis and cell proliferation in patients with familial adenomatous polyposis. Br J Surg. 1993;80:1618–1619. doi: 10.1002/bjs.1800801244. [DOI] [PubMed] [Google Scholar]
- 9.Cruz-Correa M, Hylind LM, Romans KE, Booker SV, Giardiello FM. Long-term treatment with sulindac in familial adenomatous polyposis: a prospective cohort study. Gastroenterology. 2002;122:641–645. doi: 10.1053/gast.2002.31890. [DOI] [PubMed] [Google Scholar]
- 10.Waddell WR, Ganser GF, Cerise EJ, Loughry RW. Sulindac for polyposis of the colon. Am J Surg. 1989;157:175–179. doi: 10.1016/0002-9610(89)90442-x. [DOI] [PubMed] [Google Scholar]
- 11.Spagnesi MT, Tonelli F, Dolara P, Caderni G, Valanzano R, Anastasi A, et al. Rectal proliferation and polyp occurrence in patients with familial adenomatous polyposis after sulindac treatment. Gastroenterology. 1994;106:362–366. doi: 10.1016/0016-5085(94)90593-2. [DOI] [PubMed] [Google Scholar]
- 12.Winde G, Schmid KW, Brandt B, Muller O, Osswald H. Clinical and genomic influence of sulindac on rectal mucosa in familial adenomatous polyposis. Dis Colon Rectum. 1997;40:1156–1168. doi: 10.1007/BF02055161. [DOI] [PubMed] [Google Scholar]
- 13.Niv Y, Fraser GM. Adenocarcinoma in the rectal segment in familial polyposis coli is not prevented by sulindac therapy. Gastroenterology. 1994;107:854–857. doi: 10.1016/0016-5085(94)90136-8. [DOI] [PubMed] [Google Scholar]
- 14.Lynch HT, Thorson AG, Smyrk T. Rectal cancer after prolonged sulindac chemoprevention: a case report. Cancer. 1995;75:936–938. doi: 10.1002/1097-0142(19950215)75:4<936::aid-cncr2820750407>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 15.Giardiello FM, Yang VW, Hylind LM, Krush AJ, Petersen GM, Trimbath JD, et al. Primary chemoprevention of familial adenomatous polyposis with sulindac. N Engl J Med. 2002;346:1054–1059. doi: 10.1056/NEJMoa012015. [DOI] [PMC free article] [PubMed] [Google Scholar]