Abstract
[Purpose] The purpose of this study was to examine the effects of manual therapy using joint mobilization and flexion-distraction techniques on chronic low back pain and disc heights. [Subjects] This study was conducted with 31 chronic low back pain patients who were divided into a manual therapy group (MTG; n=16) and a spinal decompression therapy group (SDTG; n=15). [Methods] The MTG was treated using joint mobilization techniques and flexion-distraction techniques, and the SDTG was treated using spinal decompression therapeutic apparatuses. Conservative physical therapy was used in both groups, and the therapy was implemented three times per week for 6 weeks. The visual analog scale (VAS) was used to measure patient’s low back pain scores, and a picture archiving and communication system was used to measure disc height by comparing and analyzing the images. [Results] In comparisons of the VAS within each of the two groups, both the MTG and the SDTG showed significant decreases. In comparisons of disc height within each of the two groups, the MTG showed statistically significant increases. [Conclusion] Manual therapy using joint mobilization techniques and flexion-distraction techniques is considered an effective intervention for addressing low back pain and disc heights in patients with chronic low back pain.
Key words: Manual therapy, Joint mobilization techniques, Spinal decompression therapy
INTRODUCTION
Among the many musculoskeletal system diseases, low back pain is one that frequently occurs on a daily basis. It is also a factor that greatly affects quality of life, leading to socioeconomic problems due to increases in treatment expenses and other troubles that affect a person’s life1).
The causes of low back pain include structural causes that arise due to lesions in the spine, psychological causes due to stress, and biodynamic causes resulting from declines in musculoskeletal system functions. The pain restricts activities, reduces use of joints, weakens secondary muscle strength, and leads to a vicious cycle that curtails physical functions and productive activities2). There are diverse treatment methods for low back pain. In most cases, these treatment methods include bed rest, wearing of assistive devices, traction therapy, thermotherapy, electrical stimulation therapy, exercise therapy, drug treatment, spinal decompression therapy, or manual therapy, and surgery is performed when treatment is not effective or conditions are serious3).
Among manual therapy techniques, joint mobilization techniques affect the neurophysiological and mechanical aspects of pain, pain arc, or muscle spasm, and they are effectively used in treating joints with hypomobility, those that gradually show mobility restrictions, and those that are functionally fixed4). Treatment with flexion-distraction techniques, which is another method of manual therapy, is used to restore damaged spinal nerves and surrounding structures by reducing the stricture of the paraspinal ligaments, increasing the movement of metabolites in discs, reducing the stress and internal pressure imposed on the posterior discs through the opening of the spinal facet joints, and expansion intervertebral foramens5).
Spinal decompression therapy is used to treat radiating pain resulting from chronic low back pain. This is a treatment method that alleviates disc problems and removes the pressure imposed on the discs by creating zero gravity or negative pressure conditions inside the spinal canal so that nutritive substances and oxygen are supplied to the discs. This reduces pressure inside the intervertebral discs by softly extending certain parts of the discs through the decompression of lesion sites6).
Although there have been many studies of manual therapy methods for chronic low back pain patients, few studies have compared manual therapy using joint mobilization techniques and flexion-distraction techniques with spinal decompression therapy. Therefore, the aim of this study was to examine the effects of manual therapy using joint mobilization techniques and flexion-distraction techniques and using spinal decompression therapy on the low back pain and disc heights of patients with chronic low back pain.
SUBJECTS AND METHODS
This study was conducted with 31 patients (eight male, 23 female) who visited S Orthopedic Hospital located in Daegu, Korea, because their low back pain had persisted for at least three months. These patients had been diagnosed by orthopedic specialists as having radiating pain resulting from chronic low back pain. Among the study subjects, the manual therapy group’s (MTG; n=16) mean age was 45.75±8.51 years, mean height was 162.00±8.98 cm, and mean weight was 59.00±12.22 kg. The spinal decompression therapy group’s (SDTG, n=15) mean age was 48.25±9.53 years, mean height was 160.25±6.14 cm, and mean weight was 62.25±11.96 kg. All the subjects read and signed consent forms, in accordance with the ethical standards of the Declaration of Helsinki. The study subjects were selected from among those who had no history of surgery in the region of their lumbar vertebrae, spinal tumor or intervertebral disc infection, inflammatory disease (such as rheumatism), or findings of fracture and were diagnosed as having no contraindication to manual therapy.
All the subjects were treated three times per week for 6 weeks. The MTG was treated with joint mobilization techniques and flexion-distraction techniques for 15 minutes per time, and the SDTG was treated with spinal decompression therapy for 20 minutes per time. Both groups were treated with a hot pack (20 minutes), ICT (15 minutes), and ultrasound (10 minutes) from among conservative physical therapy techniques for approximately 45 minutes per time.
The joint mobilization techniques used on the MTG included two techniques. Lumbar segmental flexion mobilization was applied as the first technique as follows: When the patient was lying on his/her side on a hospital bed, the patient’s hip joint and knee joints were bent. While facing the patient, the therapist placed his right hand (fixed hand) on the lumbar vertebrae of the patient and fixed his fingers on the transverse process or spinous process of the vertebra to be treated. The therapist’s left hand (moving hand) was placed on the sacral vertebrae of the patient, and his fingers were placed on the transverse process or spinous process of the vertebra to be treated. The therapist’s chest was put into tight contact with the two knee joints of the patient to move the patient’s pelvis in a caudal–ventral direction. Second, lumbar segmental extension mobilization was applied as the second technique as follows: In the same position as used for lumbar segmental flexion mobilization, the fingers of the theraphist’s right hand were placed and fixed on the spinous process of the vertebra, and the therapist’s left hand was placed behind the two knees of the patient to extend the patient’s pelvis in a cranial-dorsal direction with the patient’s lower extremities lifted slightly from the floor.
Flexion-distraction techniques were implemented using a Zenith-Cox flexion table (Zenith-100, Williams Healthcare Systems, Elgin, IL, USA). In a prone position on the table, the patient fixed his/her two ankles, and the therapist fixed his right hand’s thenar eminence on the spinous process of the vertebra of the patient and grabbed the handle above the fixed ankles with his left hand. The therapist moved his left hand slowly down to below the table to move the patient’s pelvis in a caudal-ventral direction and maintained this for approximately 4 seconds. Flexion-distraction motions were applied five times to cause flexion-distraction for a total of 20 seconds. Five repetitions of the motions were defined as one set, and three sets were performed.
The SDTG was treated using a spinal decompression therapeutic apparatus (MID 4 M Series; WIZ Medical, Geumsan, Republic of Korea). The patient took a supine position on the therapeutic apparatus, and the pelvic and thoracic regions were fixed using air belts; a sacrum extension was applied so that lumbar lordosis could be maintained. A traction power equivalent to one-quarter of the weight of the subject was first applied, and the level of traction power was increased by one level at a time at a certain rate. When the patient felt pain due to the increased traction power, the traction power was reduced or maintained. The ratio between hold time and rest time was set to 2:1 for the treatment.
The Visual Analogue Scale (VAS) was used to assess pain scales. To measure disc heights, images of discs were taken using radiation tomography equipment (R-630-150; Dongkwang, Republic of Korea), and the images were magnified three times using a picture archiving and communication system (PACS; Infinitt, Healthcare, Seoul, Republic of Korea). Intervertebral disc (L4–5) heights were measured by summing disc heights measured from the front, middle, and rear of the intervertebral disc and dividing the sum by 3. The measurement formula was (a+b+c/3) (Fig. 1).
Fig 1.
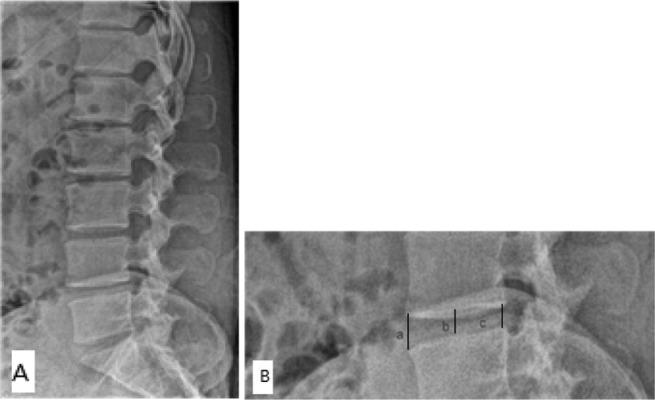
A: Lateral plain film for lumbar spine. B: Disc heights of the anterior (a), middle (b), and posterior portions (c). (DH=a+b+c/3).
The data in this study were statistically processed using SPSS 12.0 for Windows, and the significance level α was set to 0.05. To examine the pain scales and disc heights of the chronic low back pain patients, paired sample t-tests were conducted for comparison within groups.
RESULTS
Both the MTG and the SDTG showed significant decreases (p<0.05) in VAS in within-group comparisons. The MTG showed a statistically significant increase (p<0.05) in disc heights in within-group comparisons (Table 1).
Table 1. Comparison of VAS score and DH within each group.
| Group | Pre | Post | |
|---|---|---|---|
| VAS | MTG** | 6.5±1.8 | 4.38±1.4 |
| score (point) | SDTG* | 6.2±1.5 | 5.69±2.1 |
| DH (mm) | MTG* | 13.8±2.9 | 14.5±3.1 |
| SDTG | 13.1±3.1 | 13.6±2.8 |
VAS, visual analog scale; DH, disc height; MTG, manual therapy group; SDTG, spinal decompression therapy group. * p<0.05 by paired t-test; ** p<0.01
DISCUSSION
Manual therapy has been frequently used to reduce low back pain and increase the range of joint motions. Godges et al.7) stated that among manual therapy methods, joint mobilization techniques are valuable for clinical utilization in the treatment of low back pain. Cox et al.8) reported that when manual flexion-distraction correction was applied to 94 out of 100 patients with low back pain or lower extremity pain, good or excellent results were obtained by 73%, and low back pain and lower extremity pain were reduced by 50% in 15.95 days. In a study conducted by Ferreira et al.9), when manual spinal therapy was administered to chronic low back pain patients, statistically significant decreases were found in VAS scores. Kruse and Cambron10) reported that when Cox’s flexion-distraction therapy was implemented 16 times on patients with L3–4 and L4–5 intervertebral disc herniation who reported lumbar neuropathy, the patients’ numeric pain scale scores significantly decreased. Wheeler and Hanley11) applied Cox’s flexion-distraction therapy 12 times to sprain or strain patients, and the patients showed good or excellent responses in the L4–5 region at rates of 83.1% and 83.5% respectively. Gose et al.12) reported that decompression therapy reduced pain, increased mobility, and showed significant effects through changes in MRI images.
In the present study, both the MTG and the DTG showed significant decreases in VAS score within each of the groups. The significant decreases in VAS score in the MTG are considered to have occurred because the joint mobilization techniques and flexion-distraction techniques applied to the spine stimulate the mechanical receptor that suppresses the transmission of pain stimuli at the level of the spinal cord and brain stem to produce pain-reducing effects; in the manual spinal therapy, the movements of the joints reduce the transmission of stimuli by the ligaments and articular capsules, which are pain-sensitive tissues, in the spine to reduce pain. The significant decreases in VAS scores in the SDTG occurred because spinal decompression therapy generates a negative pressure to reduce the pressure inside the intervertebral disc to below −100 mmHg, increases the diameter of the intervertebral foramen through separation of the centrum, and relieves the pressure on the nervous tissues, thereby reducing radiating pain and the neurologic defect6, 10). An increase in the diameter of the intervertebral foramen can induce an increase in blood flow through the blood vessels in spinal nerves and the intervertebral foramen, and the increased blood flows can remove inflammatory exudate. In addition, spinal decompression therapy increases the generation of constituents through decompression to improve the ability to bind to water so that the water content increases, and the relief of degenerative changes enables increased nutrition supply. Therefore, the space in the spinal cavity is widened, and the paraspinal muscles and ligaments are extended to reduce secondary myofascial pain5, 13).
In a study of the relationship between flexion-distraction therapy and intervertebral disc spaces, Gudavalli14) experimented with the lumbar vertebrae in dead bodies and reported that the L4–5 disc space increased by approximately 1.87 mm, the intervertebral disc angle increased by approximately 3.5°, and the L5–S1 disc space and angle increased by approximately 3 mm and 6°, respectively. Gay et al.15) reported distraction techniques performed on 15 dead bodies, and measurements of nucleus pulposus pressure and annulus fibrosus compressive stress indicated a pressure decrease in the intervertebral disc of 99% using distraction techniques, 73% using extension-distraction techniques, and 65% using flexion-distraction techniques. Ozturk et al.16) reported that patients with herniated intervertebral disks treated with traction therapy showed significant effects in straight leg raise and disc herniation indexes.
In the present study, comparisons within groups showed that disc heights significantly increased in the MTG treated with joint mobilization techniques and flexion-distraction techniques but showed no significant difference in the SDTG. The reason for these results is that the application of joint mobilization techniques and flexion-distraction techniques produced negative pressure in the intervertebral disc space so that the disc part that was pushed to the rear of the intervertebral disc went inside and the vertebral pulp was positioned in the center of the annulus fibrosus. This removed stimuli from the annulus fibrosus fibers that feel pain and restored the physiological movements of the spinal joints, reducing low back pain and inducing structural changes, i.e., widening the spaces between spinous processes to widen the spaces between intervertebral discs17). In addition, the aforementioned techniques increase the diameter of the intervertebral foramen, reduce pressure on the nervous tissues, widen the spaces between the intervertebral discs, and open the posterior motor units by enlarging the sagittal diameter in the spinal canal18). The stress imposed on the posterior disc decreases as the spinal facet joints are opened by flexion-distraction correction, and the incompletely dislocated spinal facet joints recover to provide the normal range of posterior spinal movements.
There were several limitations of this study. First, the number of subjects was small because the subjects were selected from those who visited the hospital for 6 weeks. Second, the subjects’ daily lives could not be completely controlled. Third, the treatment period was short, and thus long-term monitoring was not possible. In future studies, the effects of long-term decompression therapy and manual therapy should be examined using a large group of patients.
REFERENCES
- 1.Kim SB: Effect of manual adjustment and gym-ball exercise on sEMG, cobb’s angle, VAS, Flexibility, and strength in elderly women with low back pain symptom. Kyung-hee University, Dissertation of master’s degree, 2012
- 2.Woo YJ: An analysis of differences in subjective pain between low back pain patient groups treated by chiropractic combined with taping and by chiropractic with exercise. Kook-Min University, Dissertation of master’s degree, 2003
- 3.Jung OH: The effects of traditional physical therapy on pain reduction and depression level of patients with chronic low back pain. Dan-kook university, Dissertation of master’s degree, 2000
- 4.Kisner C, Colby LA: Therapeutic Exercise. Foundations and Techniques, 4th ed. Philadelphia: 2002, pp 657–659.
- 5.Onel D, Tuzlaci M, Sari H, et al. : Computed tomographic investigation of the effect of traction on lumbar disc herniations. Spine, 1989, 14: 82–90 [DOI] [PubMed] [Google Scholar]
- 6.Ramos G, Martin W: Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg, 1994, 81: 350–353 [DOI] [PubMed] [Google Scholar]
- 7.Godges JJ, Mattson-Bell M, Thorpe D, et al. : The immediate effects of soft tissue mobilization with proprioceptive neuromuscular facilitation on glenohumeral external rotation and overhead reach. J Orthop Sports Phys Ther, 2003, 33: 713–718 [DOI] [PubMed] [Google Scholar]
- 8.Cox JM, Fromelt KA, Shreiner S: Chiropractic statistical survey of 100 consecutive low back pain patients. J Manipulative Physiol Ther, 1983, 6: 117–128 [PubMed] [Google Scholar]
- 9.Ferreira ML, Ferreira PH, Latimer J, et al. : Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain, 2007, 131: 31–37 [DOI] [PubMed] [Google Scholar]
- 10.Kruse RA, Cambron JA: Cox decompression chiropractic manipulation of a patient with postsurgical lumbar fusion: a case report. J Chiropr Med, 2011, 10: 255–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wheeler AH, Hanley EN., JrNonoperative treatment for low back pain. Rest to restoration. Spine, 1995, 20: 375–378 [DOI] [PubMed] [Google Scholar]
- 12.Gose EE, Naguszewski WK, Naguszewski RK: Vertebral axial decompression therapy for pain associated with herniated or degenerated discs or facet syndrome: an outcome study. Neurol Res, 1998, 20: 186–190 [DOI] [PubMed] [Google Scholar]
- 13.Gudavalli MR, Cambron JA, McGregor M, et al. : A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J, 2006, 15: 1070–1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gudavalli M: Biomechanics Research on Flexion-Distraction Procedure. Low Back Pain: Mechanism, Diagnosis and Treatment, 6th ed. Baltimore: Williams & Wilkins, 1998, pp 261–272. [Google Scholar]
- 15.Gay RE, Ilharreborde B, Zhao KD, et al. : Stress in lumbar intervertebral discs during distraction: a cadaveric study. Spine J, 2008, 8: 982–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozturk B, Gunduz OH, Ozoran K, et al. : Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int, 2006, 26: 622–626 [DOI] [PubMed] [Google Scholar]
- 17.Hwang EH, Kim JY: The study on the asymmetry ratio of surface EMG in low back pain groups. —before and after flexion—distraction technique. J Korea CHUNA. Man Med, 2004, 5: 243–249 [Google Scholar]
- 18.Cox JM: Low Back Pain: Mechanisms, Diagnosis, and Treatment, 5th ed. Baltimore: Williams & Wilkins, 1990, pp 532–584. [Google Scholar]


