Abstract
Background and Aims:
i-gel®, a recently introduced supraglottic airway device (SAD) has been claimed to be an efficient supraglottic airway. It can also be used as a conduit for endotracheal intubation. However, LMA Fastrach® frequently used for this purpose; hence in this randomized study, success rate of blind tracheal intubation through two different SADs i-gel® and LMA Fastrach® was evaluated. The complications if any were also studied.
Methods:
A total of 100 patients undergoing elective surgery under general anaesthesia were randomised in two groups comprising of 50 patients each to tracheal intubation using either i-gel (I group) or LMA Fastrach (F group). After induction of anaesthesia SAD was inserted and on achieving adequate ventilation with the device, blind tracheal intubation was attempted through the SAD. Success at first-attempt and overall tracheal intubation success rates were evaluated, and tracheal intubation time was measured. Data were analysed using IBM SPSS Statistics 20.0 software (Statistical Package for Social Sciences by International Business Machines Corporation). P < 0.05 was considered as statistically significant.
Results:
There was no difference in the incidence of adequate ventilation with either of the SAD. The success rate of tracheal intubation in first attempt was 66% in Group I and 74% in Group F, while overall success rate of tracheal intubation was 82% in Group I when compared to 96% in Group F. Time taken for successful tracheal intubation through LMA Fastrach was lesser (20.96 s) when compared to i-gel (24.04 s). Complication rates were statistically similar in both the groups.
Conclusion:
i-gel® is a better device for rescue ventilation due to its quick insertion but an inferior intubating device in comparison to LMA Fastrach®.
Keywords: Blind intubation, external laryngeal manoeuvre, i-gel®, laryngeal mask airway Fastrach®
INTRODUCTION
Endotracheal intubation is a definitive way of securing the airway and is routinely done by laryngoscopy and visualisation of cords. However, this involves distortion of upper airway to bring glottis into the line of sight[1] and in some situations such as high larynx, facial trauma, etc., tracheal intubation fails. Supraglottic airway devices (SADs) are useful in such situations for rescue ventilation. Laryngeal mask airway (LMA) classic (c-LMA)[2] is one such device which is included in Difficult Airway Society guidelines for unanticipated difficult intubation.[3]
Laryngeal mask airway classic was designed for maintenance of airway in emergency situations, especially by untrained personnel. Later it was modified into intubating LMA (ILMA) or LMA Fastrach®.[1] Major difference between standard LMA and LMA Fastrach® lies in the design and function of the shaft which is rigid as compared to soft silicone shaft of c-LMA thus facilitating adjusting manoeuvres to align the mask's aperture against the glottis opening.
The i-gel® is a relatively new single-use SAD which does not have an inflatable cuff.[4] It is made from a soft, gel-like and transparent thermoplastic elastomer (styrene ethylene butadiene styrene) which creates a noninflatable seal which is a mirror impression of the supraglottic anatomy.[5] The i-gel® has several other useful design features including a gastric channel, an epiglottic ridge and a ridged flattened stem to aid insertion and reduce the risk of axial rotation.[6] The stem of the i-gel® is less flexible than that of the LMA-classic and has an integral bite.[7] i-gel® has also been used in rescue airway management and as a conduit for tracheal intubation.[8,9,10,11,12]
The aim of our study was to compare the success rate of blind tracheal intubation through the i-gel versus the LMA Fastrach®. Because of higher airway leak pressure[13,14,15] and better visualization of glottis,[16] as compared to LMA Fastrach®, we assumed a better first-attempt success rate during blind tracheal intubation through i-gel®.
METHODS
After receiving approval from Ethical Committee and informed consent from patients, 100 patients were randomly assigned using a chit method into two groups of 50 each: The LMA Fastrach group (group F) and the I-gel group (group I). Patients between 18 and 60 years of age, American Society of Anaesthesiologists (ASA) grade I/II, with adequate mouth opening who required general anaesthesia and tracheal intubation for an elective surgical procedure were included in the study. Exclusion criteria were ASA class > II, mouth opening < 2 cm, increased risk of aspiration, oral pathology and known or anticipated difficult tracheal intubation or facemask ventilation. Injection ranitidine 50 mg and metoclopramide 10 mg were administered intravenously 30 min before the operation. In the operation theatre, infusion of Ringer lactate solution was started. Patients were connected to a multichannel monitor showing electrocardiography, oxygen saturation, noninvasive blood pressure and end-tidal carbon dioxide (EtCO2). All patients were administered injection glycopyrrolate 0.2 mg, injection midazolam 0.02 mg/kg and injection fentanyl 2 μg/kg IV. Preoxygenation was done for 3 min. All patients were induced with injection propofol 2 mg/kg IV in slow incremental dose and ease of mask ventilation was noted. After confirming adequate mask ventilation, injection rocuronium 0.9 mg/kg was administered to facilitate intubation. The supraglottic device was inserted once the jaw relaxation was achieved. The investigator had already gained experience of blind intubation in 50 patients with LMA Fastrach® and i-gel® each before the study. These cases were not included in the study.
Selection of size of the LMA Fastrach® and the i-gel® was on the basis of the weight of the patient. For the lubrication of the SADs, we used water-based lubricating jelly. Both SADs were introduced as per manufacturer's user booklet.[4,17] The i-gel® was inserted in sniffing morning air position, while the LMA Fastrach® was inserted in neutral neck position. Adequate ventilation was confirmed by chest movements and EtCO2 waveforms. When ventilation was not adequate, or there was an audible leak, while ventilating with an inspiratory pressure of 20 cm H2O, up down manoeuvre causing change in depth of insertion was performed. Use of different size of SAD were attempted if required.
Time required for insertion of SAD was defined from removal of the facemask to the time where adequate ventilation was established through SAD with capnographic confirmation.
Conventional polyvinyl chloride (PVC) endotracheal tubes (ETTs) were used for blind tracheal intubation in both the groups. ETT was lubricated with water-based lubricating jelly prior to insertion. Size 7.0 mm internal diameter (ID) ETT was used in patients weighing > 50 kg and 6.0 mm ID ETT for patients < 50 kg.[12]
In group F, ETT was inserted with reverse orientation.[18,19,20] In this manoeuvre, ETT is rotated through 180° once it crosses the proximal opening in LMA. If resistance was encountered during insertion of tracheal tube in F group, a standardised algorithm was followed on the basis of the distance at which the resistance was felt, as recommended by manufacturer.[21] If no resistance was felt during insertion of tracheal tube, it was advanced fully into the ILMA. Intubation was considered successful, if adequate ventilation produced a chest rise and a capnographic waveform.
In group I, ETT was rotated 90° counter-clockwise during insertion [Figures 1 and 2].[12] This method was used by Halwagi et al. and resulted in increased success rate, so it was incorporated in our study. If the resistance was felt during insertion, i-gel® was readjusted and stabilised at the point of maximum chest expansion, and an assistant was asked to perform optimum external laryngeal manipulation (OELM) by applying backward pressure on thyroid cartilage. This resulted in increased success rate of intubation and prevents the impingement of bevel on glottis structures. However, the disadvantage was that we had to take the help from the second person to perform external laryngeal manipulation, but the results were satisfactory.
Figure 1.

Direction of bevel during blind intubation through i-gel causing impingement on right glottic structures
Figure 2.

Direction of bevel after 90° counter clock rotation preventing impingement on glottic structures
Time required for blind endotracheal intubation was defined from disconnection of the breathing circuit of the SAD to confirmation of the tracheal intubation by auscultation and capnograph trace.
After confirmation of correct placement of ETT, supraglottic device was removed using a stabilizing rod.
In both study groups, two attempts at device insertion and intubation were allowed. Intubation was only attempted if appropriate ventilation was obtained through SAD. If tracheal intubation through the device was unsuccessful, it was performed by direct laryngoscopy.
During intraoperative and postoperative period and upto 24 h patients were evaluated for any adverse event or postoperative complaints such as sore throat, pain on swallowing and hoarseness.
The sample size was calculated to detect a 10% difference in first-attempt success rate in ETT insertion between devices with a type-1 error of 0.05 and a power of 90%, requiring 25 patients per group. We included 50 patients in each group to allow for potential drop-outs. Normally distributed data were analysed using t-test, and categorical data were analysed using the Chi-square test. Continuous data are presented as mean and standard deviation, whereas categorical data are presented as number of patients and percentage. Data were analysed using IBM SPSS statistics 20.0 software. P < 0.05 was considered statistically significant.
RESULTS
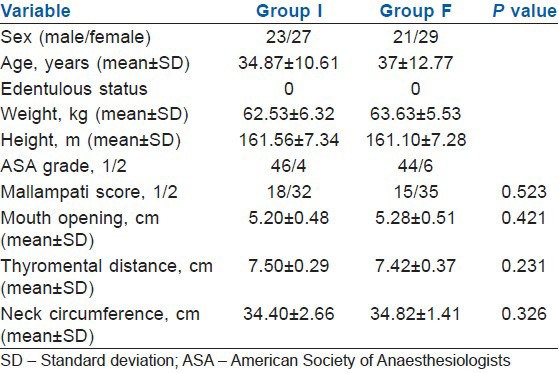
Out of 147 patients that were evaluated for the study, 41 patients were excluded according to the exclusion criteria. Six patients did not give informed consent, hence, we randomized 100 patients in two groups of 50 each. Demographic data were similar in both the groups [Table 1].
Table 1.
Patient characteristics
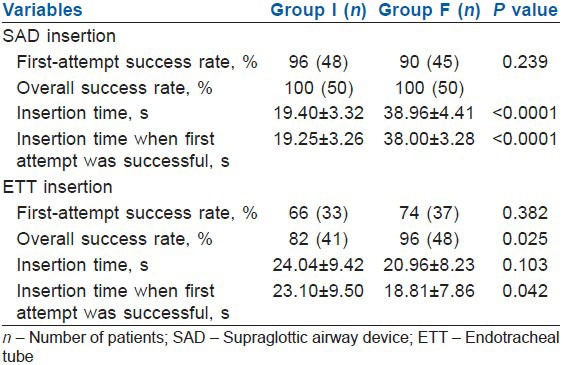
There was no difference in the successful insertion of SADs between the two groups, that is, i-gel and ILMA. With the first attempt of SAD insertion, the successful ventilation rate was 96% in I group and 90% in F group. With the second attempt of SAD insertion, the successful ventilation rate was 100% in both the groups [Table 2]. With the first attempt, blind tracheal intubation was successful in 66% cases (33 patients) of I group and in 74% cases (37 patients) of group F. With the second attempt, blind tracheal intubation was successful in 82% cases (41 patients) of group I and 96% cases (48 patients) of group F [Table 2]. Total time to achieve successful ventilation with SAD was shorter in group I. Time for successful ventilation with SAD was 19.40 s in the group I and 38.96 s in group F (P < 0.0001). Time to achieve successful intubation through the SADs was 24.04 s in the group I when compared to 20.96 s in group F (P = 0.103) [Table 2].
Table 2.
Success rate and time for device insertion and tracheal intubation
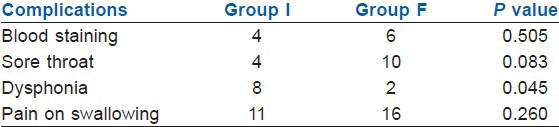
Postoperative complications in both the groups were comparable. However, dysphonia was more in the group I but still i-gel proved to be slightly safer than LMA Fastrach [Table 3].
Table 3.
Complications
DISCUSSION
In this study, overall success rate of insertion of supraglottic devices in both the groups was 100% which was similar to various previously conducted studies.[12,22] In the present study, first-attempt success rate for blind tracheal intubation was comparable in both the groups and overall success rate was higher in F group as compared to I group, which is similar to the results of Halwagi et al. (2012) and Sastre et al. (2012) who noticed higher success rate of blind tracheal intubation with ILMA®. This could be due to a “V” shaped tracheal tube guiding ramp in LMA Fastrach® that centralizes the ETT towards the glottic aperture as the ETT emerges from the metal shaft and guides it anteriorly to reduce the risk of arytenoids trauma and oesophageal placement[21] and the presence of the handle in LMA Fastrach® which resulted in stabilization and manipulations which could not be done in i-gel®. So in group I, we did external manipulation of the larynx. In our study, when first attempt of blind intubation was unsuccessful in group I, we stabilized the i-gel® at the point of maximum chest expansion by readjusting and took the help of an assistant to apply external laryngeal pressure. This resulted in better overall success rate of ETT insertion through i-gel (82%) as compared to studies by Halwagi et.al (73%) and Sastre et.al (40%). In group F, ETT was inserted with reverse orientation[18,19,20] as this method resulted in higher success rate in various studies.[18,19,20] It optimises the ETT with the angle of trachea resulting in better first-attempt success rate of ETT insertion.
The overall intubation success rate using LMA Fastrach was comparable to published studies.[23,24,25,26] The cases in which blind tracheal intubation failed only two patients needed stylet for intubation with Macintosh laryngoscope in group I and none in group F. The easier and a quicker insertion of i-gel® was probably due to noninflation of cuff. Time was not wasted in inflating the cuff, and moreover, the rigid structure of LMA Fastrach® causes delay in insertion as compared to i-gel®.
i-gel® has been used as a conduit for tracheal intubation with the help of fibreoptic bronchoscope in several case reports.[27,28,29] But limited studies are there to prove the efficacy of use of i-gel® for blind intubation. Michalek et al. did blind tracheal intubation in three different airway manikins through the i-gel® with a success rate of 51%. Theiler et al. studied “visualised blind intubation” through the i-gel® and the LMA Fastrach®. Their results showed a poor success rate (15%) with i-gel® as compared with the LMA Fastrach® (69%). Sastre et al. also showed an inferior intubation rate of 40% through i-gel® as compared to 70% with LMA Fastrach®. We observed that 90° counter-clock rotation and OELM resulted in substantially superior results.
The incidence of postoperative complications was comparable in both the groups. In the present study, dysphonia was more in I group which was similar to study conducted by Sastre et al. While the incidence of sore throat was lesser in I group when compared to F group; this observation is similar to that of Keijzer et al.[15]
There are however some limitations to our study. Data were collected in an unblended manner, some bias was possible. All the patients were ASA grade I or II with no anticipated difficult intubation. This does not represent the general population. Furthermore, the investigator had less prior experience with i-gel® as compared to LMA Fastrach®.
The use of wire reinforced tubes would have resulted in better success rate, but conventional PVC tubes are readily available and cheaper. However, in LMA Fastrach®, there was no difference in successful blind tracheal intubation with conventional tracheal tube and silicon wire-reinforced tracheal tube in studies conducted by Lu et al.[19] and Kundra et al.[26] but in case of i-gel further studies are required.
CONCLUSION
We concluded that i-gel® can be used as a conduit for endotracheal intubation. Though it is an effective SAD, it is slightly inferior to LMA Fastrach® as the intubating device. Further studies are required to prove its efficacy as a conduit for intubation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Brain AI, Verghese C, Addy EV, Kapila A. The intubating laryngeal mask. I: Development of a new device for intubation of the trachea. Br J Anaesth. 1997;79:699–703. doi: 10.1093/bja/79.6.699. [DOI] [PubMed] [Google Scholar]
- 2.Brain AI. The laryngeal mask – A new concept in airway management. Br J Anaesth. 1983;55:801–5. doi: 10.1093/bja/55.8.801. [DOI] [PubMed] [Google Scholar]
- 3.Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59:675–94. doi: 10.1111/j.1365-2044.2004.03831.x. [DOI] [PubMed] [Google Scholar]
- 4.7th ed. Wokingham, UK: Intersurgical Ltd; 2009. i. gel User Guide. [Google Scholar]
- 5.Levitan RM, Kinkle WC. Initial anatomic investigations of the i-gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia. 2005;60:1022–6. doi: 10.1111/j.1365-2044.2005.04258.x. [DOI] [PubMed] [Google Scholar]
- 6.Uppal V, Gangaiah S, Fletcher G, Kinsella J. Randomized crossover comparison between the i-gel and the LMA-Unique in anaesthetized, paralysed adults. Br J Anaesth. 2009;103:882–5. doi: 10.1093/bja/aep292. [DOI] [PubMed] [Google Scholar]
- 7.Lee JR, Kim MS, Kim JT, Byon HJ, Park YH, Kim HS, et al. A randomised trial comparing the i-gel (TM) with the LMA Classic (TM) in children. Anaesthesia. 2012;67:606–11. doi: 10.1111/j.1365-2044.2012.07072.x. [DOI] [PubMed] [Google Scholar]
- 8.Michalek P, Hodgkinson P, Donaldson W. Fiberoptic intubation through an i-gel supraglottic airway in two patients with predicted difficult airway and intellectual disability. Anesth Analg. 2008;106:1501–4. doi: 10.1213/ane.0b013e31816f22f6. [DOI] [PubMed] [Google Scholar]
- 9.Campbell J, Michalek P, Deighan M. i-gel supraglottic airway for rescue airway management and as a conduit for tracheal intubation in a patient with acute respiratory failure. Resuscitation. 2009;80:963. doi: 10.1016/j.resuscitation.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 10.Michalek P, Donaldson W, Graham C, Hinds JD. A comparison of the i-gel supraglottic airway as a conduit for tracheal intubation with the intubating laryngeal mask airway: A manikin study. Resuscitation. 2010;81:74–7. doi: 10.1016/j.resuscitation.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Theiler L, Kleine-Brueggeney M, Urwyler N, Graf T, Luyet C, Greif R. Randomized clinical trial of the i-gel™ and Magill tracheal tube or single-use ILMA™ and ILMA™ tracheal tube for blind intubation in anaesthetized patients with a predicted difficult airway. Br J Anaesth. 2011;107:243–50. doi: 10.1093/bja/aer102. [DOI] [PubMed] [Google Scholar]
- 12.Halwagi AE, Massicotte N, Lallo A, Gauthier A, Boudreault D, Ruel M, et al. Tracheal intubation through the i-gel™ supraglottic airway versus the LMA Fastrach™: A randomized controlled trial. Anesth Analg. 2012;114:152–6. doi: 10.1213/ANE.0b013e318236f438. [DOI] [PubMed] [Google Scholar]
- 13.Francksen H, Renner J, Hanss R, Scholz J, Doerges V, Bein B. A comparison of the i-gel with the LMA-Unique in non-paralysed anaesthetised adult patients. Anaesthesia. 2009;64:1118–24. doi: 10.1111/j.1365-2044.2009.06017.x. [DOI] [PubMed] [Google Scholar]
- 14.Janakiraman C, Chethan DB, Wilkes AR, Stacey MR, Goodwin N. A randomised crossover trial comparing the i-gel supraglottic airway and classic laryngeal mask airway. Anaesthesia. 2009;64:674–8. doi: 10.1111/j.1365-2044.2009.05898.x. [DOI] [PubMed] [Google Scholar]
- 15.Keijzer C, Buitelaar DR, Efthymiou KM, Srámek M, ten Cate J, Ronday M, et al. A comparison of postoperative throat and neck complaints after the use of the i-gel and the La Premiere disposable laryngeal mask: A double-blinded, randomized, controlled trial. Anesth Analg. 2009;109:1092–5. doi: 10.1213/ANE.0b013e3181b6496a. [DOI] [PubMed] [Google Scholar]
- 16.Theiler LG, Kleine-Brueggeney M, Kaiser D, Urwyler N, Luyet C, Vogt A, et al. Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology. 2009;111:55–62. doi: 10.1097/ALN.0b013e3181a4c6b9. [DOI] [PubMed] [Google Scholar]
- 17.Laryngeal Mask Company Limited. Ireland: The Laryngeal Mask Company Limited, Teleflex Medical Ireland; 2006. ILMA Fastrach Instruction Manual. [Google Scholar]
- 18.Ye L, Liu J, Wong DT, Zhu T. Effects of tracheal tube orientation on the success of intubation through an intubating laryngeal mask airway: Study in Mallampati class 3 or 4 patients. Br J Anaesth. 2009;102:269–72. doi: 10.1093/bja/aen365. [DOI] [PubMed] [Google Scholar]
- 19.Lu PP, Yang CH, Ho AC, Shyr MH. The intubating LMA: A comparison of insertion techniques with conventional tracheal tubes. Can J Anaesth. 2000;47:849–53. doi: 10.1007/BF03019663. [DOI] [PubMed] [Google Scholar]
- 20.Joo HS, Rose DK. The intubating laryngeal mask airway with and without fiberoptic guidance. Anesth Analg. 1999;88:662–6. doi: 10.1097/00000539-199903000-00036. [DOI] [PubMed] [Google Scholar]
- 21.Brain AI, Verghese C, Addy EV, Kapila A, Brimacombe J. The intubating laryngeal mask. II: A preliminary clinical report of a new means of intubating the trachea. Br J Anaesth. 1997;79:704–9. doi: 10.1093/bja/79.6.704. [DOI] [PubMed] [Google Scholar]
- 22.Sastre JA, López T, Garzón JC. Blind tracheal intubation through two supraglottic devices: i-gel versus Fastrach intubating laryngeal mask airway (ILMA) Rev Esp Anestesiol Reanim. 2012;59:71–6. doi: 10.1016/j.redar.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 23.Fun WL, Lim Y, Teoh WH. Comparison of the GlideScope video laryngoscope vs. The intubating laryngeal mask for females with normal airways. Eur J Anaesthesiol. 2007;24:486–91. doi: 10.1017/S0265021506002067. [DOI] [PubMed] [Google Scholar]
- 24.Nileshwar A, Thudamaladinne A. Comparison of intubating laryngeal mask airway and Bullard laryngoscope for oro-tracheal intubation in adult patients with simulated limitation of cervical movements. Br J Anaesth. 2007;99:292–6. doi: 10.1093/bja/aem127. [DOI] [PubMed] [Google Scholar]
- 25.Teoh WH, Lim Y. Comparison of the single use and reusable intubating laryngeal mask airway. Anaesthesia. 2007;62:381–4. doi: 10.1111/j.1365-2044.2007.04980.x. [DOI] [PubMed] [Google Scholar]
- 26.Kundra P, Sujata N, Ravishankar M. Conventional tracheal tubes for intubation through the intubating laryngeal mask airway. Anesth Analg. 2005;100:284–8. doi: 10.1213/01.ANE.0000139348.00435.33. [DOI] [PubMed] [Google Scholar]
- 27.Sharma S, Scott S, Rogers R, Popat M. The i-gel airway for ventilation and rescue intubation. Anaesthesia. 2007;62:419–20. doi: 10.1111/j.1365-2044.2007.05045.x. [DOI] [PubMed] [Google Scholar]
- 28.Bamgbade OA, Macnab WR, Khalaf WM. Evaluation of the i-gel airway in 300 patients. Eur J Anaesthesiol. 2008;25:865–6. doi: 10.1017/S0265021508004511. [DOI] [PubMed] [Google Scholar]
- 29.Emmerich M, Dummler R. Use of the i-gel laryngeal mask for management of a difficult airway. Anaesthesist. 2008;57:779–81. doi: 10.1007/s00101-008-1386-y. [DOI] [PubMed] [Google Scholar]


