Abstract
Acute myocardial infarction (AMI) remains a major cause of death in the US. An early and reliable diagnosis may warrant immediate initiation of reperfusion therapy to potentially improve the survival rate among the AMI patients. Currently, cardiac troponins (i.e. cTnT and cTnI) and creatine kinase MB (CK-MB) are widely used for AMI diagnosis. However, elevation of these biomarkers is also observed in human patients with myocarditis, aortic dissection, pulmonary embolism, congestive heart failure and renal failure. Furthermore, measurable amounts of troponin proteins are usually not released from damaged myocardium before 4 to 8 h after onset of symptoms, making an early biomarker-based diagnosis of AMI rather difficult. Therefore, new biomarkers with high sensitivity and specificity in early diagnosis of AMI are greatly needed.
Do plasma/serum microRNAs serve as biomarkers for early diagnosis of AMI?
MicroRNAs (miRNAs or miRs) are short, noncoding RNAs that are important for many aspects of homeostasis and disease [1–5]. Recent studies have excitingly demonstrated that miRs can be detected in circulating blood and that these circulating miRs are remarkably stable even under conditions as harsh as boiling, low or high pH, long-time storage at room temperature, and multiple freeze-thaw cycles [6]. These findings have raised the question of whether circulating miRs may serve as early diagnostic biomarkers for AMI.
Given that myocardial infarction is characterized by the necrotic cardiomyocyte death, which results in the passive release of myocyte miRs. Therefore, initial studies mainly focused on determining the alterations of cardimyocyte-enriched miRs (i.e. miR-1, miR-133a/b, miR-208a/b, and miR-499) in plasma/serum samples collected from human AMI patients. Indeed, at least 11 independent studies from different countries by July 2012 have confirmed in human AMI patients that these circulating muscle-/myocardium-derived miRs might be useful as potential diagnostic biomarkers for acute myocardial infarction [7–17]. For example: 6 h after AMI, serum miR-1 was increased by nearly 100-fold in a small cohort of 31 AMI patients, compared with those of 20 healthy controls [11]. Consistently, in a large cohort of 159 patients with or without AMI, plasma miR-1 levels were found to be significantly higher in AMI patients, and the level returned to normal on discharge [10]. Serum levels of miR-133a/b, which belongs to the same cluster and is co-transcribed with miR-1, were also elevated in humans after AMI [15, 16]. Several additional studies showed that circulating levels of the myosin-related miR-499 are increased in patients after AMI [9, 13–15, 17].
Notably, in 33 patients with AMI, Wang et al. [12] observed that plasma levels of miR-1, miR-133a, miR-499, and miR-208a were substantially higher than those from healthy individuals (n=30), patients with non-AMI coronary heart disease (n=16), or patients with other cardiovascular disease (n=17). Interestingly, miR-208a remained undetectable in non-AMI patients, but was easily detected in 90.9% AMI patients and in 100% AMI patients within 4 h of the onset of symptoms. By receiver operating characteristic (ROC) curve analysis, among the four miRNAs examined, miR-208a revealed the higher sensitivity and specificity for diagnosing AMI. Likewise, the comparison of miR-208b, miR-499, miR-133, and miR-1 by Corsten et al. [13] revealed that miR-208b and miR-499 were more profoundly regulated and showed a higher specificity and sensitivity [areas under the curve (AUC) of 0.94 and 0.92, respectively] in comparison to miR-1 and miR-133, which were only modestly increased in patient with AMI in this study. In addition, miR-208b levels correlated with plasma troponin T levels, confirming the link to myocardial damage.
Collectively, these studies indicate that circulating cardiac-enriched or specific miRNAs (miR-1, miR-133a/b, miR-208a/b, and miR-499) are clinically useful as early diagnosis biomarkers for AMI. However, acute myocardial infarction not only induces sudden cardiomyocyte death, but also induces other types of cell death (i.e., smooth muscle cells and endothelial cells), as well as activates inflammatory cells and platelets. Therefore, we should not neglect those miRs released from non-cardiomyocytes which may serve as meaningful diagnosis biomarkers for AMI. At this point, future investigations will be needed to perform miR-profile analysis in whole plasma or serum samples collected from AMI patients. Indeed, Meder et al. [18] recently profiled whole-genome miRNA expression in blood samples from AMI patients. They identified 121 miRNAs, which are significantly dysregulated in AMI patients (n=20) in comparison to healthy controls (n=20). Among these, miR-1291 and miR-663b show the highest sensitivity and specificity for the discrimination of cases from controls. Using a novel self-learning pattern recognition algorithm, they further discovered a unique signature of 20 miRNAs that predicts AMI with even higher power (specificity 96%, sensitivity 90%, and accuracy 93%). In addition, they showed that the vascular smooth muscle-enriched miR-30c and miR-145 levels correlate with infarct sizes estimated by troponin T release. This study indicates that single miRNAs and especially miRNA signatures derived from peripheral blood, could serve as valuable biomarkers for AMI.
Finally, it is important to mention here that most published data are derived from rather small numbers of patients, who are mostly compared with healthy controls. Therefore, additional studies are mandatory to confirm the findings described above. Moreover, future investigations should specifically evaluate whether any of the newly identified circulating miRs are competitive with the known markers of cardiac injury, such as high-sensitivity troponins.
Can plasma/serum microRNA-carriers serve as biomarkers for early diagnosis of AMI?
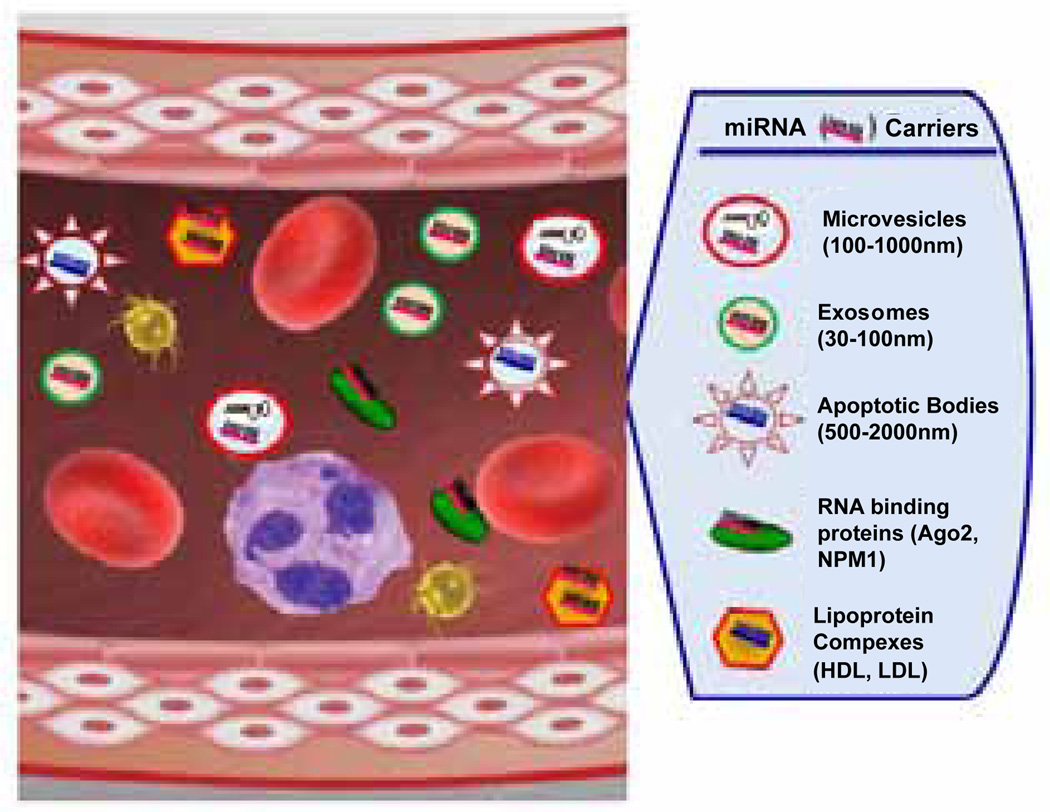
It is well recognized that circulating miRNAs are either packaged in microparticles (exosomes, microvesicles and apoptotic bodies) or associated with RNA-binding proteins [Argonaute 2 (Ago2)] or lipoprotein complexes [high-density lipoprotein (HDL)] [3, 19–22] (Figure 1). Now that circulating miRNAs have been confirmed to serve as novel biomarkers for diagnosis of AMI, one question will be asked whether these miRNA-carriers serve as diagnostic biomarkers for AMI.
Figure 1.
Circulating miRNAs are wrapped in small membrane vesicles (microvesicles, exosomes, and apoptotic bodies), RNA-binding proteins (Ago2 and NPM1) and lipoprotein complexes (HDL and LDL complexes). In response to AMI, these miRNA carriers are released into the bloodstream.
Actually, upon myocardial infarction, activated platelets and damaged/apoptotic endothelial cells are responsible for the release of microparticles (MPs) into the bloodstream [23, 24]. Jung et al. [24] recently measured levels of CD31+/CD42− MPs and CD144+ MPs (endothelial cell origin, EMP), as well as CD31+/CD42+ (platelet origin, PMP), in the plasma samples collected from 36 patients with first time ST-elevation myocardial infarction using flow cytometry. They observed that patients with occlusion of the left anterior descending artery (LAD infarctions, n=11) had higher levels of CD31+/CD42− EMP (p < 0.05) and CD31+/CD42+ PMP (p < 0.05) than those with other infarct-related arteries (n=25). CD144+ EMP did not differ between the two groups. CD31+/CD42− EMP and CD31+/CD42+ PMP both correlated to the area under the curve of troponin T levels, but not to CKMB. These results suggest that some specific types of microparticles may serve as biomarkers for diagnosis of AMI. Nonetheless, it remains unclear whether circulating miRNA-carriers can serves as AMI diagnostic biomarkers. Therefore, future clinical studies will be required to focus on these miRNA-carriers in plasma/serum samples collected from AMI patients. Conceptually, it is intriguing to speculate that specific miRNA-carriers might be released very early after cellular injury, which is a characteristic feature of the initiating processes of cellular stress responses or apoptosis.
In summary, several lines of evidence have suggested that circulating miRNAs and miRNA carriers both can serve as valuable biomarkers for the early diagnosis of AMI. However, it is still unclear which of the measured miRNAs or miRNA-carriers is best suited and might represent a meaningful superior alternative to already established biomarkers of AMI, such as troponins. At this point, there are lots of work needs to be done in the future.
References
- 1.Ren XP, Wu J, Wang X, Sartor MA, Qian J, et al. MicroRNA-320 is involved in the regulation of cardiac ischemia/reperfusion injury by targeting heat-shock protein 20. Circulation. 2009;119:2357–2366. doi: 10.1161/CIRCULATIONAHA.108.814145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X, Zhang X, Ren XP, Chen J, Liu H, et al. MicroRNA-494 targeting both proapoptotic and antiapoptotic proteins protects against ischemia/reperfusion-induced cardiac injury. Circulation. 2010;122:1308–1318. doi: 10.1161/CIRCULATIONAHA.110.964684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu H, Fan GC. Extracellular/circulating microRNAs and their potential role in cardiovascular disease. Am J Cardiovasc Dis. 2011;1:138–149. [PMC free article] [PubMed] [Google Scholar]
- 4.Wang X, Zhu H, Zhang X, Liu Y, Chen J, et al. Loss of the miR-144/451 cluster impairs ischaemic preconditioning-mediated cardioprotection by targeting Rac-1. Cardiovasc Res. 2012;94:379–390. doi: 10.1093/cvr/cvs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu H, Fan GC. Role of microRNAs in the reperfused myocardium towards post-infarct remodelling. Cardiovasc Res. 2012;94:284–292. doi: 10.1093/cvr/cvr291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A. 2008;105:10513–10518. doi: 10.1073/pnas.0804549105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ji X, Takahashi R, Hiura Y, Hirokawa G, Fukushima Y, et al. Plasma miR-208 as a biomarker of myocardial injury. Clin Chem. 2009;55:1944–1949. doi: 10.1373/clinchem.2009.125310. [DOI] [PubMed] [Google Scholar]
- 8.D’Alessandra Y, Devanna P, Limana F, Straino S, Di Carlo A, et al. Circulating microRNAs are new and sensitive biomarkers of myocardial infarction. Eur Heart J. 2010;31:2765–2773. doi: 10.1093/eurheartj/ehq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adachi T, Nakanishi M, Otsuka Y, Nishimura K, Hirokawa G, et al. Plasma microRNA 499 as a biomarker of acute myocardial infarction. Clin Chem. 2010;56:1183–1185. doi: 10.1373/clinchem.2010.144121. [DOI] [PubMed] [Google Scholar]
- 10.Ai J, Zhang R, Li Y, Pu J, Lu Y, et al. Circulating microRNA-1 as a potential novel biomarker for acute myocardial infarction. Biochem Biophys Res Commun. 2010;391:73–77. doi: 10.1016/j.bbrc.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Cheng Y, Tan N, Yang J, Liu X, Cao X, et al. A translational study of circulating cell-free microRNA-1 in acute myocardial infarction. Clin Sci (Lond) 2010;119:87–95. doi: 10.1042/CS20090645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang GK, Zhu JQ, Zhang JT, Li Q, Li Y, et al. Circulating microRNA: a novel potential biomarker for early diagnosis of acute myocardial infarction in humans. Eur Heart J. 2010;31:659–666. doi: 10.1093/eurheartj/ehq013. [DOI] [PubMed] [Google Scholar]
- 13.Corsten MF, Dennert R, Jochems S, Kuznetsova T, Devaux Y, et al. Circulating microRNA-208b and microRNA-499 reflect myocardial damage in cardiovascular disease. Circ Cardiovasc Genet. 2010;3:499–506. doi: 10.1161/CIRCGENETICS.110.957415. [DOI] [PubMed] [Google Scholar]
- 14.Adachi T, Nakanishi M, Otsuka Y, Nishimura K, Hirokawa G, et al. Plasma microRNA 499 as a biomarker of acute myocardial infarction. Clin Chem. 2010;56:1183–1185. doi: 10.1373/clinchem.2010.144121. [DOI] [PubMed] [Google Scholar]
- 15.Widera C, Gupta SK, Lorenzen JM, Bang C, Bauersachs J, et al. Diagnostic and prognostic impact of six circulating microRNAs in acute coronary syndrome. J Mol Cell Cardiol. 2011;51:872–875. doi: 10.1016/j.yjmcc.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Kuwabara Y, Ono K, Horie T, Nishi H, Nagao K, et al. Increased microRNA-1 and microRNA-133a levels in serum of patients with cardiovascular disease indicate myocardial damage. Circ Cardiovasc Gene. 2011;4:446–454. doi: 10.1161/CIRCGENETICS.110.958975. [DOI] [PubMed] [Google Scholar]
- 17.Olivieri F, Antonicelli R, Lorenzi M, D’Alessandra Y, Lazzarini R, et al. Diagnostic potential of circulating miR-499-5p in elderly patients with acute non ST-elevation myocardial infarction. Int J Cardiol. 2012 doi: 10.1016/j.ijcard.2012.01.075. [DOI] [PubMed] [Google Scholar]
- 18.Meder B, Keller A, Vogel B, Haas J, Sedaghat-Hamedani F, et al. MicroRNA signatures in total peripheral blood as novel biomarkers for acute myocardial infarction. Basic Res Cardiol. 2011;106:13–23. doi: 10.1007/s00395-010-0123-2. [DOI] [PubMed] [Google Scholar]
- 19.Vickers KC, Palmisano BT, Shoucri BM, Shamburek RD, Remaley AT. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol. 2011;13:423–433. doi: 10.1038/ncb2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, et al. Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci U S A. 2011;108:5003–5008. doi: 10.1073/pnas.1019055108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turchinovich A, Weiz L, Langheinz A, Burwinkel B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. 2011;39:7223–7233. doi: 10.1093/nar/gkr254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleissner F, Goerzig Y, Haverich A, Thum T. Microvesicles as novel biomarkers and therapeutic targets in transplantation medicine. Am J Transplant. 2012;12:289–297. doi: 10.1111/j.1600-6143.2011.03790.x. [DOI] [PubMed] [Google Scholar]
- 23.Zielinska M, Koniarek W, Goch JH, Cebula B, Tybura M, et al. Circulating endothelial microparticles in patients with acute myocardial infarction. Kardiol Pol. 2005;62:531–542. [PubMed] [Google Scholar]
- 24.Jung C, Sorensson P, Saleh N, Arheden H, Ryden L, et al. Circulating endothelial and platelet derived microparticles reflect the size of myocardium at risk in patients with ST-elevation myocardial infarction. Atherosclerosis. 2012;221:226–231. doi: 10.1016/j.atherosclerosis.2011.12.025. [DOI] [PubMed] [Google Scholar]