Abstract
Objectives
Elder abuse is associated with increased morbidity and mortality. This study aims to develop a vulnerability index for elder abuse in a community-dwelling population.
Design
Population-based study
Setting
Geographically defined community in Chicago.
Participants
A population-based study was conducted in Chicago of community-dwelling older adults who participated in the Chicago Health and Aging Project (CHAP). Of the 8,157 participants in the CHAP study, 213 participants were reported to social services agency for suspected elder abuse.
Measurements
A vulnerability index for elder abuse was constructed from sociodemographic, health-related, and psychosocial factors. The outcomes of interest were reported and confirmed elder abuse. Logistic regression models were used to determine the accuracy of the index with respect to elder abuse outcomes.
Results
Out of the selected risk index for elder abuse, every one point increase in the 9 item vulnerability index items, there was a two fold increase in the risk for reported elder abuse (OR, 2.19 (2.00–2.40) and confirmed elder abuse (OR, 2.19 (1.94–2.47). Compared to the reference group, older adults with 3–4 vulnerability index items had increased risk for reported elder abuse (OR, 2.98 (1.98–4.49) and confirmed elder abuse (OR, 3.90, (2.07–7.36); and older adults with 5 or more risk index items, there was an 18 fold increase in risk for reported elder abuse (OR, 18.46 (12.15–28.04) and confirmed elder abuse (OR, 26.79 (14.18–50.61). Receiver Operating Characteristic (ROC) statistically derived curves for identifying reported elder abuse ranged between 0.77–0.84 and for predicting confirmed elder abuse ranged between 0.79–0.86.
Conclusion
The vulnerability risk index demonstrates value for identifying individuals at risk for elder abuse. Additional studies are needed to validate this index in other community dwelling populations.
Keywords: elder abuse index, population-based study
INTRODUCTION
Elder abuse includes physical abuse, sexual abuse, psychological abuse, caregiver neglect and financial exploitation (1). Available data suggest that 10% US elderly persons experience some forms of abuse (2;3). In addition, the most recent data from Adult Protective Services Agencies depict an increasing trend in the reporting of elder abuse (4). Moreover, literature suggests that elder abuse is associated with increased risk of morbidity and mortality, especially among the most vulnerable populations (5–7). However, we are not aware of any study that has systematically examined a vulnerability index tool to predict the occurrences of elder abuse in community-dwelling populations.
This study followed the conceptual framework of Socio-Cultural Context suggested by the National Research Council (1). Elder abuse is defined as “intentional actions that cause harm or create a serious risk of harm, whether or not intended, to a vulnerable elder by a caregiver or other person who stands in a trust relationship to the elder; or failure by a caregiver to satisfy the elder’s basic needs or to protect the elder from harm.” In this manuscript, we will focus on the key factor: vulnerability, which refers to the cluster of risk factors that have been associated with elder abuse; namely: age, sex, race/ethnicity, socioeconomic status, cognitive impairment, physical disability, depressive symptoms, social network and social participation. The amalgamation of these potential risk factors may be associated with increased likelihood of predicting the occurrence of elder abuse.
Improved understanding of risk prognostication for elder abuse could inform strategies for health care professionals, social services practice, health policy (8;9). In this manuscript, we aim to construct a vulnerability elder abuse index for reported and confirmed elder abuse in a community-dwelling population of older adults.
METHODS
Setting
Chicago Health and Aging Project (CHAP), a community-based study of risk factors for Alzheimer’s disease among older adults aged 65 and over begun in 1993 (baseline). Its participants include residents of three adjacent neighborhoods on the south side of Chicago and are followed every 3 years. More in-depth details of the study design of CHAP have been previously published (10;11). In-home data collection occurred in cycles, each lasting 3 years, with each cycle ending as the succeeding cycle began. All CHAP participants received structured in-person interviews. Written informed consent was obtained, and the study was approved by the Institutional Review Board at Rush University Medical Center.
Dependent Variable: Elder Abuse
In the current study, participants were enrolled in CHAP study (N=8,157). From this cohort, we identified a subset of participants (N=213) who were reported to social services agencies for elder abuse. In Illinois (IL), suspected elder abuse should occur only if the person over the age of 60, due to dysfunction, is unable to report themselves, and elder abuse has occurred within the last 12 months. Confirmed cases of elder abuse in this study were ascertained through investigation by Adult Protective Services (APS).
In Illinois APS, the definition used for abuse included physical abuse, sexual abuse, psychological abuse, neglect and financial exploitation. Physical abuse was defined as inflicting physical pain or injury upon an older adult. Sexual abuse was touching, fondling, intercourse, or any other sexual activity with an older adult, when the older adult was unable to understand, unwilling to consent, threatened or physically forced. Psychological abuse involved verbal assaults, threat of abuse, harassment or intimidation. Confinement was restraining or isolating an older adult, other than for medical reasons. Neglect was a caregiver’s failure to provide an older adult with life’s necessities, including, but not limited to, food, clothing, shelter or medical care. Willful deprivation was defined as willfully denying an older adult medication, medical care, shelter, food, a therapeutic device or other physical assistance. Financial exploitation included the misuse, or withholding of an older adult’s resources by another, to the disadvantage of the elderly person or the profit or advantage of someone else. Confirmed elder abuse indicates that there was evidence of elder abuse after the APS investigation. However, unconfirmed elder abuse cases do not necessarily mean there was no evidence of elder abuse; as sometime APS staff could not gain access to older adults or older adult victim refused to cooperate in services suggested by APS.
Independent Variable: Vulnerability Index Items
Demographic variables were assessed prior to the report of elder abuse and include age (in years), sex (men or women), race (self-reported: non-Hispanic black versus non-Hispanic white), and income categories (1=$0–4,999; 2=$5,000–9,999; 3=$10,000–14,999; 4=$15,000–19,999; 5=$20,000–24,999; 6=$25,000–29,999; 7=$30,000–34,999; 8=$35,000–49,999; 9=$50,000–74,999; 10=$75,000 and over). Self-reported medical conditions included summary of number of common conditions: hypertension, diabetes mellitus, stroke, coronary artery disease, hip fracture, and cancer. These variables have been associated with increased risk for elder abuse (12;13).
Cognitive and physical function has been associated with increased risk for elder abuse (14;15). Cognitive testing in CHAP include the Mini-Mental State Examination (MMSE) (16), the East Boston Memory Test (17) and the Symbol Digit Modalities Test (18). Physical function was assessed using the Katz Index of Activities of Daily Living (19), which measured limitations in an individual’s ability to perform basic self-care tasks. The second measure was an index of mobility, based on work by Rosow and Breslau (20). It is composed of three items measuring the ability to do heavy work around the house, climbing a flight of stairs, and walk half a mile. The third measure used in this study was an index of basic physical activities, and is based on work by Nagi (21). It measures five activities of upper or lower extremity function.
Psychosocial factors have been associated with increased risk for elder abuse (22–24). Psychosocial factors included assessment of depressive symptoms and social network. Symptoms of depression were measured using a modified version(25) of the Center for Epidemiologic Studies of Depression Scale (CES-D)(26). Social network was summarized as the total number of children, relatives, and friends seen at least monthly(27).
Analytic Approach
Descriptive characteristics for the potential vulnerability factors were provided across the sociodemographic, medical conditions, cognitive function, physical function and psychosocial factors for 4 groups: the total cohort, no elder abuse, reported elder abuse and confirmed elder abuse. Our independent variables of interest were the vulnerability factors. Our outcome of interests was the reported and confirmed elder abuse.
Based on available CHAP data and up-to-date literature search, we selected the nine key variables to be considered in the vulnerability elder abuse index; age, sex, race, income, medical conditions, cognitive function, physical function, depressive symptoms and social network. In constructing the elder abuse index, we utilized an approach that provided most relevance to clinicians and practitioners by creating categorical cutoff points for each of these variables of interest in order to examine its precision in detecting elder abuse. For each of the variables above, we conducted close examination of multiple cutoff points and examined the bivariate associations between the variables of interest with the elder abuse outcomes. For example, for age, we used every 5 years interval cutoff points (65, 70, 75, 80, 85 yr) to examine its association with elder abuse. We then selected the cutoff points with the strongest association with elder abuse outcomes (for age, it was age 80 years or older). For gender, we selected female as oppose to male. For race, we selected blacks as oppose to whites. For income, we selected annual income greater than $15,000. For medical conditions, we examine both the cumulative total number of medical conditions as well as each specific medical condition with respect to elder abuse outcomes. From these bivariate analyses, we selected the presence of total medical conditions ≥ 3 as the categorical cutoff point.
For cognitive function, even though CHAP study collects detailed data on a number of cognitive measures, MMSE is one of the most commonly used and has most relevance to clinicians and practitioners. After examining multiple cutoff points, we found MMSE ≤23 had the strongest association with elder abuse outcomes. For physical function, we examined the multiple self-reported physical function measures and found that “ability to climb 1 flight of stairs” had the greatest association with elder abuse outcomes. For depressive symptoms, we found that CESD ≥ 4 had the greatest association with elder abuse. For social network, we found that social network size < 2 persons had the greatest association with elder abuse outcomes. Next, the frequency with which each of the characteristics that constituted the vulnerability risk index occurred were examined in each of the four groups: total cohort, no elder abuse, reported elder abuse and confirmed elder abuse. Lastly, we calculated the cumulative prevalence of reported and confirmed elder abuse cases, based on the additive presence of these categorically defined vulnerability risk factors.
Multivariable logistic regression models were used to quantify the relation between the 9-item vulnerability index and elder abuse. Odd Ratio (OR) and 95% Confidence Interval (CI) were reported for the regression models. We used the Receiver Operating Characteristic (ROC) curves, which were plotted for both reported and confirmed elder abuse using the vulnerability risk indexes. ROC curve permits the study to contrast the true positive rates (sensitivity) compared to the false positive rate (1 – specificity) and to evaluate the accuracy of the elder abuse index. Analyses were carried out using SAS®, Version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Baseline Characteristics
There were 8,157 CHAP participants in this study and 213 participants were investigated by social services agencies for elder abuse from 1993 to 2010. Of the 213 reported cases of elder abuse, there were 109 cases of confirmed elder abuse. The characteristic of the cohort was described in Table 1 based on the previously mentioned cutoff points of the vulnerability factors for overall cohort, no elder abuse, reported elder abuse and confirmed elder abuse groups. In Table 2, we described the prevalence of reported and confirmed elder abuse based on the number of the vulnerability risk index. As shown, the greater number of risk factor index, the greater prevalence of elder abuse in this community-dwelling population.
Table 1.
Characteristic of the Study Population
| Total Cohort: N=8,157 | No Elder Abuse: N=7,944 | Reported Abuse: N=213 | Confirmed Abuse: N=109 | |
|---|---|---|---|---|
| Age >80, Number, % | 1368 (17) | 1284 (16) | 84 (39) | 42 (39) |
| Female, Number, % | 4852 (59) | 4694 (59) | 158 (74) | 79 (72) |
| Black, Number, % | 4826 (59) | 4638 (57) | 188 (88) | 101 (92) |
| Annual Income ≥ $15,000, Number, % | 7082 (87) | 6920 (87) | 162 (76) | 88 (81) |
| Medical Condition ≥ 3, Number, % | 514 (6) | 476 (6) | 38 (18) | 21 (19) |
| MMSE ≤23, Number, % | 1256 (15) | 1164 (14) | 92 (43) | 47 (43) |
| Difficulty w/1 Flight of Stairs, Number, % | 741 (9) | 671 (8) | 70 (33) | 32 (29) |
| CESD ≥ 4, Number, % | 1163 (35) | 1089 (14) | 74 (35) | 40 (37) |
| Social Network < 2, Number, % | 717 (9) | 678 (8) | 39 (18) | 22 (20) |
MMSE: Mini-Mental State Examination.
CESD: Center for Epidemiologic Studies of Depression Scale
Table 2.
Vulnerability Risk Index Factors and the Prevalence of Reported and Confirmed Elder Abuse
| Number of the Vulnerability Index Items | Total Cohort Participants with Risk Factors | No Abuse with Risk Factors | Reported Abuse with Risk Factors | Confirmed Abuse with Risk Factors | Prevalence of Reported Elder Abuse (%) | Prevalence of Confirmed Elder Abuse (%) |
|---|---|---|---|---|---|---|
| 0 | 16 | 16 | 0 | 0 | 0% | 0% |
| 1 | 966 | 962 | 4 | 0 | 0.4% | 0% |
| 2 | 2727 | 2700 | 27 | 12 | 0.9% | 0.4% |
| 3 | 2660 | 2617 | 43 | 24 | 1.6% | 0.9% |
| 4 | 1127 | 1077 | 50 | 23 | 4.4% | 2.1% |
| 5 | 431 | 392 | 39 | 25 | 9.0% | 6.0% |
| 6 | 162 | 132 | 30 | 17 | 18.5% | 11.4% |
| 7 | 60 | 43 | 17 | 7 | 28.3% | 14.0% |
| 8 | 8 | 5 | 3 | 1 | 37.5% | 16.7% |
Individual Items of the Vulnerability Index and Risk for Elder Abuse
In the multivariable regression model adjusting for all 9 variables of interest (Table 3), we examined the independent association between each of the categorically defined variables to the elder abuse outcomes. Briefly, age greater than 80, female gender, non-Hispanic black, those with 3 or more medical conditions, MMSE < 23, difficulty with stairs, depressive symptoms (CESD≥4) and social network <2 were all associated with the increased risk for elder abuse outcomes.
Table 3.
Association Between Index Items and Risk for Elder Abuse
| Reported Elder Abuse | Confirmed Elder Abuse | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Age > 80 | 3.01 (2.16–4.19) | 3.34 (2.13–5.24) |
| Female | 1.76 (1.27–2.45) | 1.76 (1.13–2.75) |
| Black | 5.76 (3.69–8.99) | 10.10 (4.78–21.34) |
| Income ≥ $15,000 | 1.31 (0.91–1.89) | 1.87 (1.10–3.18) |
| Medical Condition ≥ 3 | 2.26 (1.53–3.35) | 2.67 (1.60–4.47) |
| MMSE ≤23 | 1.88 (1.35–2.62) | 1.94 (1.24–3.04) |
| Difficulty w/Stairs: 1 Flight | 2.20 (1.56–3.11) | 1.78 (1.10–2.89) |
| CESD ≥ 4 | 1.68 (1.22–2.29) | 1.82 (1.19–2.79) |
| Social Network < 2 | 1.61 (1.10–2.36) | 1.84 (1.11–3.04) |
Cumulative Vulnerability Index and Risk for Elder Abuse
With the composite 9-item vulnerability index of interest, we examined the incremental impact of the index as a continuous variable to the risk of elder abuse (Table 4). For every 1 point increase in vulnerability index, there was a two fold increase in the risk for reported elder abuse (OR, 2.19 (2.00–2.40)) and confirmed elder abuse (OR, 2.27 (2.01–2.57)). Using those with 0–2 risk factors as a reference, those with 3–4 risk factor indexes (OR, 3.90 (2.07–7.36)) and those with 5 or more risk factor indexes (OR, 26.79 (14.18–50.61)) had even greater risk for confirmed elder abuse.
Table 4.
Association Between Elder Abuse Index and Risk for Elder Abuse
| Reported Elder Abuse | Confirmed Elder Abuse | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| All Variables Index | ||
| Continuous Index (0–9) | 2.19 (2.00–2.40) | 2.27 (2.01–2.57) |
| Categorical Index (0–9) | ||
| 0–2 (Reference) | 1.0 | 1.0 |
| 3–4 | 2.98 (1.98–4.49) | 3.90 (2.07–7.36) |
| 5–9 | 18.46 (12.15–28.04) | 26.79 (14.18–50.61) |
| Sociodemographic Index | ||
| Continuous (0–4) | 3.08 (2.51–3.78) | 3.61 (2.69–4.82) |
| Categorical Index (0–4) | ||
| 0–2 (Reference) | 1.0 | 1.0 |
| 3–4 | 3.44 (2.58–4.58) | 3.49 (2.34–5.21) |
| Health-Related Index | ||
| Continuous (0–5) | 2.32 (2.07–2.59) | 2.34 (2.01–2.72) |
| Categorical Index (0–5) | ||
| 0–2 (Reference) | 1.0 | 1.0 |
| 3–5 | 9.12 (6.41–12.95) | 8.85 (5.49–14.28) |
Sociodemographic Index: Age >80, Female, Black and Income ≥ $15K
Health-Related Index: Med condition ≥ 3, MMSE ≤23, Difficulty with 1 Flight of Stairs, CESD ≥4, and Social Network < 2
Continous refers to the cummulative impact for each of the items as continuous variables.
Categorical index reference group (1.0) refers to the comparison to other groups either in the total vulnerbility index or subindex of sociodemographic index or health-related index.
In addition, we examined the association between two major components of the vulnerability index (sociodemographic index (0–4 risk factors) and health-related index (0–5 risk factors)) and risk for elder abuse. For sociodemographic index (age, sex, race, income) with reference group being (0–2), those with 3–4 risk factor indexes (OR, 3.49 (2.34–5.21)) had greater increased risk for elder abuse. For health-related index (medical conditions, cognitive function, physical function, depression and social network) with reference group being (0–2), those with 3–4 factor indexes (OR, 8.85 (5.49–14.28) had greater increased risk for elder abuse.
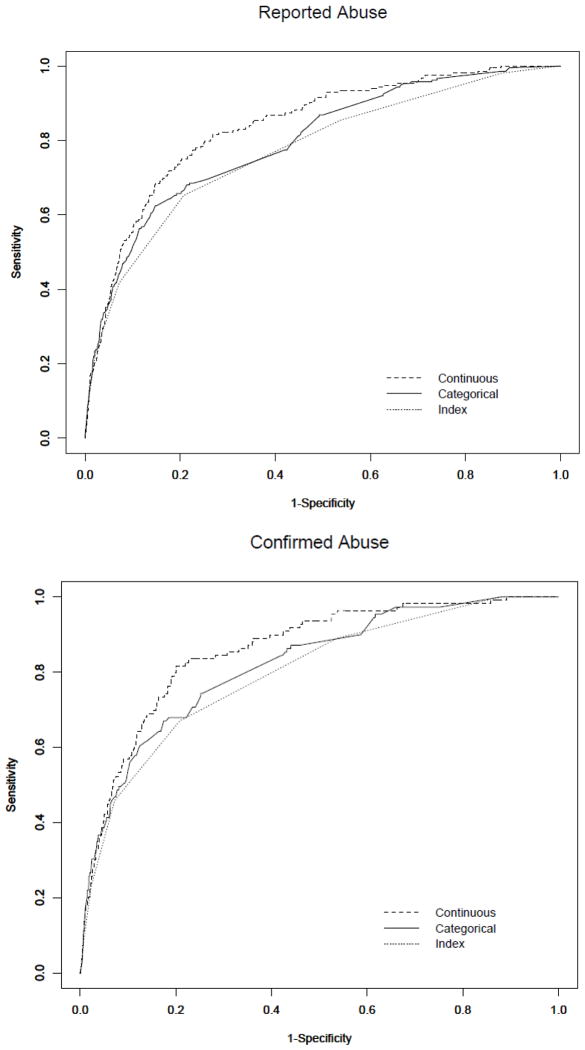
ROC Curves for Elder Abuse Index
In order to measure the accuracy of the elder abuse index using the vulnerability factors, we used the Receiver Operating Characteristic (ROC) curves, which permits the study to contrast the true positive rates (sensitivity) compared to the false positive rate (1 – specificity) and to evaluate the accuracy of the elder abuse index (Figure 1). We provided ROC model for three different approaches: 1) Vulnerability index: 9-item as a continuous measure; 2) Categorical: cumulative impact of each of the 9-item cutoff points as categorical variables; and 3) Continuous: cumulative impact of the each of the 9-item as continuous variables. The ROC model for vulnerability index for reported elder abuse was 0.77. Then ROC curve was plotted for each individual vulnerability factor items as defined categorically and areas under the curve was 0.79. The ROC curve was again plotted for the each individual vulnerability factor items as a continuous variable, the area under the curve was 0.84. For confirmed elder abuse outcomes, the ROC model area under the curve was 0.79 for the vulnerability index. Then ROC curve was plotted for each individual vulnerability factor items as defined categorically and areas under the curve was 0.82. The ROC curve was again plotted for the each individual vulnerability factor items as a continuous variable, the area under the curve was 0.86.
Figure 1. Accuracy of the Vulnerability Index for Reported and Confirmed Elder Abuse.
Note:
In order to measure the accuracy of the elder abuse index using the vulnerability factors, we used the Receiver Operating Characteristic (ROC) curves, which permits the study to contrast the true positive rates (sensitivity) compared to the false positive rate (1 – specificity) and to evaluate the accuracy of the vulnerability index.
Index refers to the 9-items vulnerability index as a continuous measure (0–9).
Categorical refers to the cummulative impact for each of the 9 items cutoff points as categorical variables.
Continous refers to the cummulative impact for each of the 9 items as continuous variables.
Areas under the curves for reported elder abuse were 0.77 for index, 0.79 for categorical, and 0.84 for continuous.
Areas under the curves for confirmed elder abuse were 0.79 for index, 0.82 for categorical, and 0.86 for contiuous.
DISCUSSION
In this prospective epidemiological study of 8,157 older adults, 9-item vulnerability index demonstrated good accuracy for both reported and confirmed elder abuse outcomes. Older individuals with 3–4 risk factors were almost 4 times more likely to experience elder abuse, and those with 5 or more risk factors were 26 times more likely to experience elder abuse.
Prior studies on risk factors associated with elder abuse have greatly contributed to this manuscript. A number of studies have suggested the association between sociodemographic characteristics associated with elder abuse (3,12,13). In addition, evidence suggest that elder abuse occurs commonly among those with cognitive impairment and physical function impairment and that cognitive and functional decline are associated with increased risk for elder abuse (14,15,28). Moreover, psychosocial distress have been associated both as risk factors as well as consequences of elder abuse. The collective knowledge of these prior studies has helped to shape the constructions of the vulnerability index for elder abuse.
To our knowledge, this is the only study to examine the association between vulnerability index and risk for elder abuse; demonstrating a good accuracy to identify the occurrences of elder abuse. Our data suggest that the accuracy of the vulnerability index is particularly high, when older adults have 5 or more of the vulnerability risk factors. This information could be useful in future prevention and intervention strategies to identify high-risk older adults who may be at greater risk to experience elder abuse. Second, our population-based study has been well characterized in the community setting for more than 17 years. In addition, the CHAP has detailed potential confounding variables of interest, which permit the rigorous examination of accuracy of the vulnerability index and the elder abuse outcomes.
Third, our prior studies suggest that elder abuse victims have significant greater utilization of health care services, especially in terms of emergency department visit, hospitalization, nursing home placement and hospice utilizations. With our present study, the vulnerability risk index provides clinicians and practitioners to evidence-based tool to assess and determine high-risk groups for elder abuse. It is critical for health care providers, social services agencies and other relevant disciplines to identify older adults who may be at greater risk for abuse and intervene before more elder abuse occurs. Improved understanding of factors that may increases unnecessary health services use could also have significant implications for social and health policy as well as clinical care of the vulnerable patients.
Our study also has a number of limitations. First, it is important to point out that our study is designed to construct a vulnerability index and not to construct an elder abuse screening measure. There have been a number of self-reported screening tools designated to detect the specific acts of elder abuse from the perspective of older adults (29–31). However, very few conduct a “gold standard” validation by the APS. In our study, elder abuses have already been detected and validated by APS after applying a strict number of indicators. Our present study aims to examine the cumulative impact of sociodemographic, health-related and psychosocial risk factors associated with elder abuse within the context of a population-based cohort study.
Second, our study focused on the reporting of elder abuse to adult protective services as the primary outcome. Elder abuse was not ascertained uniformly for all members of the CHAP population, but only for participants referred to the agencies because someone suspected problems. Although precise rate of under-reporting is unknown, it is estimated that 1/15 cases of elder abuse are not reported adult protective services (1). Third, our sample size for specific subtypes of elder abuse has limited our ability to examine the association between the vulnerability index and elder abuse subtypes. Improved knowledge of vulnerability risk index with specific subtypes of elder abuse would improve our understanding of strategies for more targeted risk predictor for specific elder abuse types (32;33).
Fourth, there are likely to be additional factors that may account for the increased risk for elder abuse outcomes (lack of social support, loneliness, severity of medical conditions, injury, and etc). Regrettably, we do not have data to consider these additional factors in our analyses, which may in-part, influence our finding in this report. Lastly, although it may increase usability in clinical practice by dichotomizing certain variables (i.e., age, income), it may also reduce the sensitivity of these vulnerability index items.
Our findings have clinical implications for health care providers in screening, prevention, and intervention of elder abuse case. Health care professionals should consider screening for elder abuse among older patients who may have frequent encounters with health care systems, as well as those who present to healthcare settings for cognitive impairment, physical disability, depression and social isolation. Identification of potential elder abuse victims could help health care providers devise interventions to prevent adverse health outcomes.
Moreover, our findings could have important implications for other relevant disciplines that work with elder abuse victims. Other health care professionals (nursing, social workers, and social services agencies) who work with elder abuse victims or who may be at increased risk for elder abuse could be in unique positions to further monitor the precipitating and predisposing factors that may exacerbate the unnecessary adverse health outcomes. In addition, it is important for all relevant disciplines to monitor the severity and the exacerbation of abusive behaviors towards older adults. Identification of signs of elder abuse and devising targeted prevention and intervention strategies could prevent deterioration of abusive acts into more severe forms. Close monitoring and improved understanding of vulnerability factors that may exacerbate abusive situations could also help health care providers to leverage family members, social workers, health professionals, and public health and community organizations to create a multi-disciplinary approach to care for and protect the elder abuse victims. Future studies are needed to validate this vulnerability index in a different epidemiological cohort.
Conclusion
We conclude that the vulnerability risk index demonstrates value for risk prognostication of elder abuse outcomes in a community-dwelling population. The risk for elder abuse is particularly high if an older adult have 5 or more of the risk indexes. Future investigations are needed to explore the risk index to predict specific subtypes of elder abuse in community-dwelling populations.
Acknowledgments
Authors would like to thank the adult protective services staff of IL for their continued dedication to protect the vulnerable victims of elder abuse.
Dr. Dong is supported by National Institute on Aging grant (R01 AG042318, R01 MD006173, R01 AG11101 & RC4 AG039085), Paul B. Beeson Award in Aging (K23 AG030944), The Starr Foundation, American Federation for Aging Research, John A. Hartford Foundation and The Atlantic Philanthropies.
Sponsor’s Role: None
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Drs Dong, Simon declare no conflict of interest.
Author Contributions:
Drs. Dong, Simon were responsible for the conception and design as well as analysis and interpretation of data. All these authors were involved in the drafting of the manuscript, critical revision of the manuscript and statistical analysis of the manuscript.
References
- 1.National Research Council. Elder Mistreatment: Abuse, neglect and exploitation in an Aging America. Washington, D.C: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Beach SR, Schulz R, Castle NG, et al. Financial Exploitation and Psychological Mistreatment Among Older Adults: Differences Between African Americans and Non-African Americans in a Population-Based Survey. Gerontologist. 2010;50:744–757. doi: 10.1093/geront/gnq053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. Am J Public Health. 2010;100:292–297. doi: 10.2105/AJPH.2009.163089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teaster PB, Dugar T, Mendiondo M, et al. [Accessed April 4th, 2007];The 2004 Survey of Adult Protective Services: Abuse of Adults 60 Years of Age and Older. 2007 www.elderabusecenter.org/pdf/research/apsreport030703.pdf.
- 5.Schofield MJ, Powers JR, Loxton D. Mortality and disability outcomes of self-reported elder abuse: A 12-year prospective investigation. J Am Geriatr Soc. 2013;61:679–685. doi: 10.1111/jgs.12212. [DOI] [PubMed] [Google Scholar]
- 6.Dong X, Simon M, Mendes de Leon C, et al. Elder self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009;302:517–526. doi: 10.1001/jama.2009.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong X, Simon MA, Beck T, et al. Elder abuse and mortality: The role of psychological and social wellbeing. Gerontology. 2011;57:549–558. doi: 10.1159/000321881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dong X, Simon MA. Enhancing National Policy and Programs to Address Elder Abuse. JAMA. 2011;305:2460–2461. doi: 10.1001/jama.2011.835. [DOI] [PubMed] [Google Scholar]
- 9.Mosqueda L, Dong X. Elder abuse and self-neglect: “I don’t care anything about going to the doctors.. to be honest”. JAMA. 2011;306:532–540. doi: 10.1001/jama.2011.1085. [DOI] [PubMed] [Google Scholar]
- 10.Bienias JL, Beckett LA, Bennett DA, et al. Design of the Chicago Health and Aging Project (CHAP) J Alzheimers Dis. 2003;5:349–355. doi: 10.3233/jad-2003-5501. [DOI] [PubMed] [Google Scholar]
- 11.Evans DA, Bennett DA, Wilson RS, et al. Incidence of Alzheimer disease in a biracial urban community: Relation to apolipoprotein E allele status. Arch Neurol. 2003;60:185–189. doi: 10.1001/archneur.60.2.185. [DOI] [PubMed] [Google Scholar]
- 12.Laumann EO, Leitsch SA, Waite LJ. Elder Mistreatment in the United States: Prevalence Estimates From a Nationally Representative Study. J Gerontol B Psychol Sci Soc Sci. 2008;63:S248–S254. doi: 10.1093/geronb/63.4.s248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mouton CP, Rodabough RJ, Rovi SL, et al. Psychosocial effects of physical and verbal abuse in postmenopausal women. Ann Fam Med. 2010;8:206–213. doi: 10.1370/afm.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dong X, Simon M, Beck T, et al. Decline in cognitive function and elder mistreatment: findings from the Chicago Health and Aging Project. Am J Geriatr Psychiatry. doi: 10.1016/j.jagp.2012.11.004. (0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dong X, Simon M, Evans D. Decline in physical function and risk of elder abuse reported to social services in a community-dwelling population of older adults. J Am Geriatr Soc. 2012;60:1922–1928. doi: 10.1111/j.1532-5415.2012.04147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 17.Albert M, Smith LA, Scherr PA, et al. Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer’s disease. Int J Neurosci. 1991;57:167–178. doi: 10.3109/00207459109150691. [DOI] [PubMed] [Google Scholar]
- 18.Smith A. Symbol Digit Modalities Test Manual-Revised. Los Angeles: Western Psychological; 1984. [Google Scholar]
- 19.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 20.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 21.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54:439–467. [PubMed] [Google Scholar]
- 22.Dong X, Simon MA, Odwazny R, et al. Depression and elder abuse and neglect among community-dwelling Chinese elderly population. J Elder Abuse Negl. 2008;20:25–41. doi: 10.1300/J084v20n01_02. [DOI] [PubMed] [Google Scholar]
- 23.Dong X, Simon MA, Gorbien M, et al. Loneliness in older Chinese adults: A risk factor for elder mistreatment. J Am Geriatr Soc. 2007;55:1831–1835. doi: 10.1111/j.1532-5415.2007.01429.x. [DOI] [PubMed] [Google Scholar]
- 24.Abrams RC, Lachs M, McAvay G, et al. Predictors of self-neglect in community-dwelling elders. Am J Psychiatry. 2002;159:1724–1730. doi: 10.1176/appi.ajp.159.10.1724. [DOI] [PubMed] [Google Scholar]
- 25.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 26.Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 27.Cornoni-Huntley J, Brock DB, Ostfeld A, et al. Established Populations for Epidemiological Studies of the Elderly Resource Data Book (Rep. No. NIH Publication No. 86–2443) Washington, D.C: US Department of Health and Human Services; 1986. [Google Scholar]
- 28.Paveza GJ, Cohen D, Eisdorfer C, et al. Severe family violence and Alzheimer’s disease: prevalence and risk factors. Gerontologist. 1992;32:493–497. doi: 10.1093/geront/32.4.493. [DOI] [PubMed] [Google Scholar]
- 29.Hwalek MA, Sengstock MC. Assessing the Probaility of Abuse of the Elderly: Toward the Development of a Clinical Screening Instrument. J Appl Gerontol. 1986;5:153–173. [Google Scholar]
- 30.Schofield MJ, Mishra GD. Validity of self-report screening scale for elder abuse: Women’s Health Australia Study. Gerontologist. 2003;43:110–120. doi: 10.1093/geront/43.1.110. [DOI] [PubMed] [Google Scholar]
- 31.Yaffe MJ, Weiss D, Lithwick M. Seniors’ self-administration of the Elder Abuse Suspicion Index (EASI): A feasibility study. J Elder Abuse Negl. 2012;24:277–292. doi: 10.1080/08946566.2011.652930. [DOI] [PubMed] [Google Scholar]
- 32.Dong X, Chang E-S, Wong E, et al. How do U.S. Chinese older adults view elder mistreatment? Findings from a Community-Based Participatory Research Study. J Aging Health. 2011;23:289–312. doi: 10.1177/0898264310385931. [DOI] [PubMed] [Google Scholar]
- 33.Dong X, Simon M, Evans D. Elder self-neglect is associated with increased risk for elder abuse in a community-dwelling population: Findings fFrom the Chicago Health and Aging Project. J Aging Health. 2013;25:80–96. doi: 10.1177/0898264312467373. [DOI] [PMC free article] [PubMed] [Google Scholar]