Abstract
Purpose: We examine the effects of use of adult day service (ADS) by caregivers of individuals with dementia (IWD) on daily stressors, affect, and health symptoms. Participants were interviewed for 8 consecutive days. On some days, the IWD attended an ADS program and on the other days caregivers provide most or all of the care at home. Methods: Participants were 173 family caregivers of IWDs using an ADS program. Daily telephone interviews assessed care-related stressors, noncare stressors, positive events, affect, and health symptoms. Multilevel models with data nested within persons were used to examine effects of ADS use on daily stressor exposure, affect, and health symptoms. Results: Caregivers had lower exposure to care-related stressors on ADS days, more positive experiences, and more noncare stressors. ADS use lowered anger and reduced the impact of noncare stressors on depressive symptoms. Implications: The findings demonstrate that stressors on caregivers are partly lowered, and affect is improved on ADS days, which may provide protection against the effects of chronic stress associated with caregiving.
Key Words: Caregivers, Daily stress, Adult day services
Family caregivers, particularly those assisting an individual with dementia (IWD), encounter high levels of care-related stressors on a daily basis, which have adverse effects on their health and emotional well-being (Aneshensel, Pearlin, Mullen, Zarit, & Whitlatch, 1995). Prior studies suggest that use of adult day services (ADS) and other types of respite care reduce the exposure that caregivers have to care-related stressors by as much as 40% (Zarit, Kim, Femia, Almeida, Savla, & Molenaar, 2011). This present study extends this work by assessing on a new sample the effects of ADS days and daily stressors and their interactive effects on daily affect and health symptoms. Specifically, interviews were conducted with caregivers of IWDs over eight consecutive days. On some of those days, the IWD attended ADS, and on some other days, the IWD did not attend ADS. We compared whether caregivers’ exposure to care-related stressors is lower on ADS than on non-ADS days and whether lower exposure to stressors is associated with improved daily affect and health symptoms. We also considered caregivers’ exposure to daily stressors not related directly to providing care and to positive events on ADS and non-ADS days and their associations with daily affect and health symptoms. Prior research has shown that the impact of daily stressors may be greatest on the day those events occurred (Almeida, 2005). By extension, we expect that ADS would have substantial effect on caregivers on days it is used because it lowers exposure to daily stressors. By interrupting the stress-overload cycle typically observed in people experiencing high chronic stress, ADS and similar respite services may make daily life more manageable at least on days that caregivers receive respite.
Vulnerabilities Associated With Daily Stressors
Studies of daily stressors have provided valuable information about the relation of the daily events to physical and emotional well-being in middle-aged and older adults (Almeida, 2005; Almeida, McGonagle, & King, 2009, Bolger, Davis, & Rafaeli, 2003; Charles & Almeida, 2006). Daily stressors exert their influence by having separate and immediate effects on emotional and physical functioning and through the accumulation of residual effects over a series of days that create persistent feelings of distress and overload, and lead to adverse outcomes such as clinical depression and increased health problems. These effects have generally been demonstrated in samples that report relatively low levels of stressors that emerge from the circumstances of everyday life. For example, in the National Study of Daily Experiences (NSDE), participants reported at least one stressor on 40% of observation days and multiple stressors on only 10% of days (Almeida, 2005). The impact of daily stressors on affect and physical health symptoms may be considerably greater when people experience relatively high levels of stressors.
One such group experiencing high levels of daily stressors is family caregivers, particularly those caring for IWDs. Among the stressors caregivers experience, behavioral and psychological symptoms of the IWD (BPSD) are typically reported as the most frequent, distressing, and upsetting (Teri, 1997). The time, effort, and emotional strain involved in providing care can also spill over into other areas of the person’s life, leading to an increase in stressors not directly related to care (Aneshensel et al., 1995).
The application of a daily diary approach has several advantages for examining mechanisms linking daily stressors to well-being for caregivers. Much prior research on caregiving has been cross-sectional or involved one or two longitudinal follow-ups. These designs confound between-person differences in mean levels of stressors and outcomes and within-person associations. By contrast, multiple daily reports make it possible to examine between-person differences and within-person processes of change. Specifically, a within-person perspective allows us to compare each person with him/herself on ADS and non-ADS days. We can then assess if each person shows improvement in stressor exposure, affect, and health symptoms on ADS days compared with him/herself on non-ADS days, which is a more fundamental indicator of improvement than how that individual might compare with a group average. Daily interviews also place lower burden on recall of specific stressors and do not require that people average how they have felt over a long period of time (e.g., a week or a month). By shortening the period of recall, studies of daily stressors can better identify proximate events that lead to exacerbation or reduction of feelings of distress, including caregivers’ immediate responses to intervention (Zarit et al., 2011).
Several studies have used daily assessments in samples of caregivers assisting older adults (Koerner, Shirai, & Kenyon, 2010; Mausbach, Harmell, Moore, & Chattillion, 2011), as well as those helping an adult offspring with chronic disabilities (Seltzer et al., 2009). In a study using data from the NSDE, participants who were providing assistance to an older parent reported more stressors and higher emotional distress on days they helped their parent (Savla, Almeida, Davey, & Zarit, 2008). Mausbach and colleagues (2011) found that over a 14-day period, leisure activities were associated with daily positive and negative affects for caregivers of IWDs. In a study of caregivers of people with mild cognitive impairment, daily fluctuations of positive and negative affects were associated with daily behavioral problems and secondary role stressors and strain (Savla, Roberto, Blieszner, Cox, & Gwazdauskas, 2011). Taken together, these studies demonstrate the within-person associations of daily stressors and events with affect.
The present study extends this prior work by focusing on caregivers who use an intervention, ADS, that affects the amount of daily exposure to stressors. This strategy allows us to examine caregivers’ responses on high-stress days when they provide all the care to their IWD and on low-stress days when their relative attends ADS. This approach has three advantages. First, greater differences from day to day in levels of stressors allow us to differentiate more clearly the effects of daily stressors on affect from mean levels of chronic stressors. Second, a daily approach allows us to evaluate what impact ADS has on affect and health symptoms on days it is used, where the benefits may be clearest, compared with days when ADS is not used. Third, consistent with the stress suppression model of Ensel and Lin (1991), we may find that relief from some daily stressors allows caregivers to manage remaining challenges more effectively, specifically showing less affective reactivity to these events. Prior work has found that affective reactivity to stressors is more important for health outcomes than number or type of stressors (Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013).
Three important considerations underlie the comparison of caregivers on ADS and non-ADS days. First, we use within-person comparisons to examine the effects of ADS and non-ADS days on daily levels of stressors and outcomes. This approach is comparable with an A-B-A-B within-person treatment design (Barlow, Nock, & Hersen, 2009), in which a critical variable, in this case, care-related stressor exposure, is modified by treatment (ADS use), and effects are assessed at the within-person level by comparing individuals on days they received and did not receive treatment. Second, we need to determine if ADS use actually reduces overall exposure to multiple types of daily stressors. Although caregivers may receive a break from some stressors on ADS days, they may encounter different stressors during the respite period, for example, performing housework or errands or dealing with demands at work (Gottlieb & Johnson, 2000). Taking this possibility into account, we asked caregivers on each day about stressors they experienced that were not directly related to care they gave to their IWD. We also asked about positive events they experienced to determine if respite gave caregivers opportunities to engage in enjoyable activities. Third, caregivers who are not providing care to their IWD at home on a regular basis would experience less difference in exposure to care-related stressors on ADS and non-ADS days. For that reason, we limited the study to caregivers who lived with the IWD and provided most or all care at home.
The study tested the following hypotheses. First, we hypothesized that care-related stressors as measured by BPSD would be lower on ADS days compared with non-ADS days. This hypothesis could also be considered a manipulation check that the intervention (i.e., ADS use) produced the intended effect on care-related stressors. Second, we hypothesized that noncare stressors and positive events would both be higher on ADS days. Third, we hypothesized that daily ADS use, lower stressor exposure, and higher positive events would be related to improved daily affect and less health symptoms. Fourth, we hypothesized that ADS will buffer the effects of stressors on affect and health symptoms. The study will lead to greater understanding of how daily stressors can affect the affect and health symptoms in the context of chronic stress and will provide practical information on benefits to caregivers from ADS use.
Methods
Participants
Participants were 173 family caregivers of IWDs who were using an ADS program. To be eligible for the study, caregivers had to be related to the IWD and to indicate that they had primary responsibility for the IWD. Primary responsibility was defined as spending the most time helping the IWD with daily tasks. To assure differences in stressor exposure between ADS and non-ADS days, we required that caregiver and IWD lived in the same household. The IWD had to have been diagnosed by a physician as having a type of dementia. (e.g., Alzheimer’s disease). Persons whose relative was diagnosed with “mild cognitive impairment” or similar predementia syndromes were not included. Participants were also excluded if their IWD was scheduled to attend ADS less than 2 days a week. Five participants subsequently used ADS only once during the observation period due to cancelling scheduled days (n = 3) or not completing interviews for all 8 days (n = 2) but were retained in the sample.
A total of 241 people participated in an initial telephone screening interview, and 41 people (17%) were not eligible for the study. The most frequent reasons were not having eligible dementia diagnosis (n = 16), not living with the IWD (n = 5), and not using enough days of ADS (n = 11). Following the screening, 6 of the 200 eligible participants (3%) decided not to enroll in the study. Ten participants (5%) did not complete the initial in-home interview, and two persons (1%) only completed the initial interview but no daily interviews. Finally, nine caregivers (4.5%) were eliminated from the present analysis because their daily interviews did not include both days their relative attended ADS and days their relative did not attend ADS. The resulting sample was 173 people (86.5% of eligible participants).
Procedures
ADS programs were identified through their regional and state associations in five areas: Northern and Central New Jersey, the greater Philadelphia area, the greater Pittsburgh area, Northern Virginia, and Denver, Colorado. Meetings were held to explain the study to representatives of the ADS programs. Programs that agreed to participate in the study received fliers for potential participants, which contained information about the study and the e-mail and telephone number of the study’s research coordinator. We also placed announcements in newsletters of participating programs and gave reminders and study updates to staff. A total of 57 programs provided referrals over a 3-year recruitment period.
Family caregivers who contacted the research coordinator were told about the study and screened for eligibility. Eligible caregivers were scheduled for an initial interview, which was nearly always conducted in the caregiver’s home, although phone interviews were used in a few instances. The interviewer obtained signed consent and gathered sociodemographic information and baseline data on a number of measures. The Penn State Survey Research Center conducted the daily interviews. Calls took place in the evenings. Participants received payments for completing the initial interview and the eight daily interviews.
Measures
Type of Day.
Type of day, that is, whether the IWD used ADS (ADS = 1) or did not use ADS (ADS = 0), was confirmed at the end of each day during the telephone interview.
Daily Stressors.
We gathered information on two types of daily stressors: care-related stressors and stressors not involving daily care.
Care-related Stressors.
We focused on BPSD, which are found by caregivers as the most challenging and upsetting in their daily care (Teri, 1997). The daily record of behavior (DRB), which was designed specifically for use in a daily interview format (Fauth, Zarit, Femia, Hofer, & Stephens, 2006; Femia, Zarit, Stephens, & Greene, 2007), measured BPSD. The version of the DRB in this study includes 19 items drawn from six behavioral categories: resistance to help with activities of daily living (ADL), restless behaviors, reality problems, depressive behaviors, disruptive behaviors, and memory-related behaviors. Up to three other care-related behavioral events could be added by caregivers.
To assist caregivers in reporting daily behavior problems, the day is divided up into four periods: waking to 9:00 a.m., 9:00 a.m. to 4:00 p.m., 4:00 p.m. to bedtime, and overnight. This time frame corresponded to the modal period (9:00 a.m. to 4:00 p.m.) during which caregivers use ADS. For each period, caregivers were asked if a behavior had occurred, and if yes, to rate the subjective severity of the behavior along a 5-point scale ranging from 1 (not at all stressful) to 5 (very stressful). If the behavior occurred more than once during the time period, caregivers reported on the most stressful occurrence. We summed the total number of behaviors reported each day and computed the mean score for subjective severity for all occurrences.
The DRB was administered during the eight daily phone interviews. Caregivers reported IWDs’ behaviors for the previous 24hr from the time of the call. For the purposes of analyses, we constructed complete days from the reports. Prior work indicates adequate psychometric properties of the DRB (Fauth et al., 2006). Internal reliability for BPSD occurrence in the current sample was high (α = 0.90).
Noncare Stressors.
Noncare daily stressors were assessed through the Daily Inventory of Stressful Events (DISE, Almeida, 1998; Almeida, Wethington, & Kessler, 2002). Caregivers reported on the occurrence of eight items over the previous 24-hr period. They were instructed to report events they experienced as stressful other than events encountered while assisting their IWD. Items included arguments with other people, avoiding an argument, stressors affecting friends or family, health-related issues, financial issues, work-related events, or any other incidents. Caregivers rated the subjective severity of each event on a 5-point scale ranging from 1 (not at all stressful) to 5 (very stressful). We summed the number of events reported each day and computed the mean subjective severity for all daily events.
Positive Events.
Using items from the DISE (Almeida, 1998), we asked if any of five positive events had occurred in the past day: share a good laugh with someone, a positive experience at home, a positive experience with a close friend or relative, a positive experience at work, and any other positive experience. The number of positive events that occurred each day was summed.
Daily Affect and Health Symptoms
Daily Affect.
We measured daily psychological distress using an adapted inventory from the Non-Specific Psychological Distress Scale (Kessler et al., 2002; Mroczek & Kolarz, 1998). The 22-item scale assesses four affective domains relevant to caregivers: anxiety symptoms, anger, depressive symptoms, and positive affect. Positive affect was supplemented with two items (interested, attentive) from the Positive and Negative Affect Schedule (Watson, Clark, & Tellegen, 1988) to create a broader assessment of positive emotions. Respondents reported the frequency of each emotion over the past day along a 5-point scale from 1 (none of the day) to 5 (all day).
A factor analysis was performed that replicated the four affective domains. Four items were dropped because they did not load on any scale or loaded approximately equally on two or more domains. The final scales included the following: anxiety symptoms (three items, α = 0.84), anger (four items, α = 0.83), depressive symptoms (four items, α = 0.84), and positive affect (nine items, α = 0.92). The four scales represent dimensions usually included in models of affect: high-activation negative emotion (anger), low-activation negative emotion (depressive symptoms), trait-related negative emotion (anxiety symptoms), and positive affect (Watson & Tellegen, 1985).
Daily Health Symptoms.
Daily health symptoms were assessed using an adapted version of Larsen and Kasimatis’ symptom checklist (Larsen & Kasimatis, 1991). We omitted items that overlapped with the psychological distress scale (e.g., “urge to cry”). The six clusters of symptoms were pain, gastrointestinal symptoms, upper respiratory symptoms, cardiovascular, fatigue, and symptoms not covered in the other items. Women were asked two additional items related to menopausal symptoms. Respondents indicated how often they experienced each symptom in the past day, using a 5-point scale that ranged between 1 (none of the day) and 5 (all day). Mean scores were calculated. Internal reliability for the final scale was low (α = 0.60), which is typical of inventories of events, which occur independently of one another (Bollen & Lennox, 1991).
Covariates.
We included variables likely to affect levels of stressors and daily affect and health symptoms. Sociodemographic variables included age, gender, and employment status of caregivers. We also considered two variables representing the caregiving trajectory. First, we assessed duration of caregiving as reported by caregivers. Second, we assessed the extent of IWD’s disability in activities of daily living (ADL). Caregivers were asked about the amount of assistance their IWD needed to perform 13 ADLs. Items were drawn from scales assessing personal ADL (Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963) and instrumental ADL (Lawton & Brody, 1969). Responses ranged from 1, indicating that the IWD could do the activity by him/herself and needs no help, to 4, indicating that the IWD is unable to do the activity by him/herself and needs help all the time. Mean scores of the items were calculated. Finally, we included total number of days the IWD used ADS during the eight interview days as a control variable.
Analysis
We employed two-level multilevel models (SAS PROC MIXED) to examine daily diary data nested within persons (Littell, Miliken, Stroup, & Wolfinger, 1996). First, to address hypotheses 1 and 2 regarding effects of ADS on daily experiences, we modeled care-related stressors, noncare stressors, and positive events for dth day in the ith person as follows:
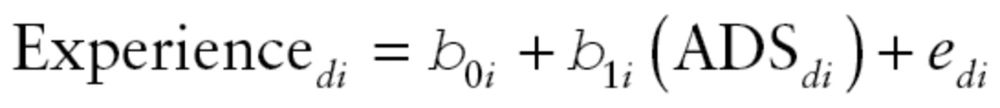 |
Daily experience is a function of an intercept (β 0i, the average score on non-ADS days), ADS use (β 1i, the difference in daily experiences on ADS days compared with non-ADS days), and the person-specific deviations from the intercept (e di) at Level 1 (within person). At Level 2, we included six (between person) covariates: caregiver’s age, gender, employment status, duration of care, IWD ADL impairment, and number of ADS days (out of 8 days).
To examine effects of ADS use and daily experiences on daily affect and health symptoms (hypothesis 3), we parameterized the models of five daily well-being scores (positive affect, depressive symptoms, anger, anxiety symptoms, and health symptoms) for dth day in the ith person at Level 1 (within person):
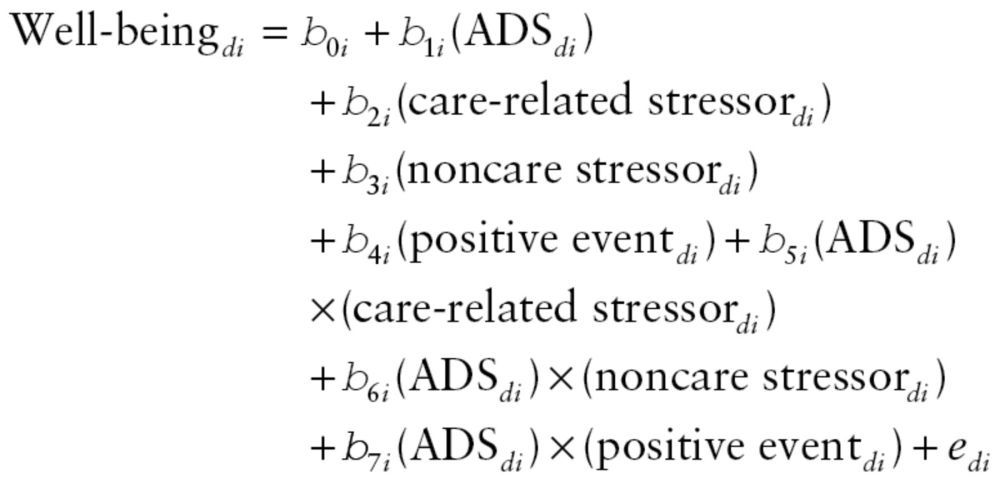 |
We first included ADS use (β 1i) to examine differences in the well-being measures by type of day and then added occurrence scores for three daily experiences (β 2i, β 3i, and β 4i), which were centered at person-mean to represent the within-person effects (Hoffman & Stawski, 2009). To test buffering effects of ADS use on daily well-being (hypothesis 4), we computed interactions between ADS use and daily experiences (β 5i, β 6i, and β 7i). At Level 2 (between-person), we controlled six covariates (i.e., caregiver’s age, gender, and employment status, duration of care, IWD’s ADL impairment, and number of ADS days) as well as the person-mean levels of the three daily experiences.
Results
Caregivers completed 98% of all daily interviews. An average of 4.09 interviews (standard deviation [SD] = 1.46) were on ADS days and 3.77 interviews (SD = 1.43) were on non-ADS days. Characteristics of caregivers and IWDs are shown in Table 1.
Table 1.
Characteristics of Caregivers and Individuals with Dementia
| M | SD | Range | |
|---|---|---|---|
| CG’s characteristics | |||
| Age | 61.97 | 10.66 | 39–89 |
| Educationa | 4.46 | 1.20 | 1–6 |
| Incomeb | 6.68 | 3.10 | 1–11 |
| Duration of care (month) | 61.12 | 45.55 | 3–264 |
| Female (yes = 1) | 0.87 | 0.34 | 0–1 |
| Relation to IWD | |||
| Spouse (yes = 1) | 0.38 | 0.49 | 0–1 |
| Child (yes = 1) | 0.58 | 0.49 | 0–1 |
| Others (yes = 1) | 0.04 | 0.20 | 0–1 |
| White (yes = 1) | 0.73 | 0.45 | 0–1 |
| Married (yes = 1) | 0.69 | 0.46 | 0–1 |
| Employed (yes = 1) | 0.42 | 0.49 | 0–1 |
| Number of daily interview days | 7.86 | 0.65 | 3–8 |
| Number of ADS days | 4.09 | 1.46 | 1–6 |
| Number of non-ADS days | 3.77 | 1.43 | 2–7 |
| IWD’s characteristics | |||
| Age | 82.02 | 8.34 | 57–100 |
| Female (yes = 1) | 0.60 | 0.49 | 0–1 |
| ADL impairmentc | 3.06 | 0.49 | 2–4 |
Notes: Participant N = 173; ADS = adult day services; CG = caregiver; IWD = individual with dementia.
aRated on a 6-point scale ranging from 1 (less than high school) to 6 (post college degree).
bRated on a 11-point scale ranging from 1 (less than $10,000) to 11 ($100,000 or over).
cMean scores of 13 items rated on a 4-point scale ranging from 1 (does not need help) to 4 (cannot do without help); Cronbach’s α = 0.83.
Next, we tested differences in daily experiences, affect, and health symptoms on ADS and non-ADS days. Table 2 shows within-person means for each variable, intraclass correlations, and the effect of type of day. Multilevel models indicated that caregivers reported significantly lower care-related stressors on ADS days compared with non-ADS days (Unstandardized beta B = −1.12, p < .001). Subjective severity of care-related stressors did not differ across type of day. Analysis by what period of the day stressors occurred (data not shown in tables) indicated that stressor exposure was lower mainly during the time the IWD was at ADS. Noncare stressors were significantly higher on ADS days (B = 0.15, p < .01), as were positive events (B = 0.15, p < .01). Severity of noncare stressors did not differ by type of day. We further examined which noncare stressors increased on ADS days (data not shown in tables). Caregivers reported significantly more events affecting a friend or relative other than the IWD on ADS days than on non-ADS days (19% compared with 11%) and more work-related events on ADS days than on non-ADS days (11% compared with 4%). Analysis of positive events indicated that the difference among type of days was due to significant increases in caregivers’ reports of positive experiences at work on ADS days compared with non-ADS days (24% vs 9%) and sharing a good laugh with someone (73% compared with 68%).
Table 2.
Daily Experiences and Well-Being of Family Caregivers by Adult Day Service Use
| Total | ADS day | Non-ADS day | ADS effecta | ||
|---|---|---|---|---|---|
| M (SD) | ICC | M (SD) | M (SD) | B a (SE) | |
| Care-related daily experiences | |||||
| Occurrence of care-related stressorsb | 4.27 (5.01) | 0.73 | 3.75 (5.09) | 4.85 (5.39) | −1.12 (0.17)** |
| Subjective severity of care-related stressorsc | 2.91 (0.81) | 0.55 | 2.89 (0.89) | 2.97 (0.84) | −0.06 (0.04) |
| Noncare daily experiences | |||||
| Occurrence of noncare stressorsb | 1.17 (0.89) | 0.42 | 1.22 (0.96) | 1.07 (1.00) | 0.15 (0.05)** |
| Subjective severity of noncare stressorsc | 3.34 (0.72) | 0.32 | 3.33 (0.79) | 3.38 (0.78) | −0.08 (0.06) |
| Occurrence of positive eventsb | 2.46 (0.97) | 0.45 | 2.52 (1.03) | 2.35 (1.05) | 0.17 (0.06)** |
| Daily well-being: Health symptoms and affect | |||||
| Health symptomsd | 1.51 (0.36) | 0.60 | 1.52 (0.38) | 1.49 (0.38) | 0.03 (0.02)* |
| Positive affecte | 3.02 (0.83) | 0.74 | 3.04 (0.83) | 3.00 (0.88) | 0.04 (0.03) |
| Depressive symptoms | 1.17 (0.44) | 0.73 | 1.16 (0.46) | 1.17 (0.43) | −0.01 (0.02) |
| Angerf | 1.73 (0.53) | 0.49 | 1.70 (0.58) | 1.75 (0.60) | −0.06 (0.03)* |
| Anxiety symptomsg | 1.44 (0.60) | 0.68 | 1.43 (0.60) | 1.46 (0.65) | −0.03 (0.02) |
Notes: Participant N = 173; Observation N = 1,359; ADS = adult day services; CG = caregiver; IWD = individual with dementia; ADL = activities of daily living; B = unstandardized Beta.
aFixed effects of ADS use (ADS day = 1, non-ADS day = 0) for differences between ADS day and non-ADS day in multilevel models; CG’s age, gender, and employment, duration of care, IWD’s ADL impairment, and number of ADS days were included as (between-person) control variables.
bCount of occurred stressors or events.
cMean scores of subjective severity only for occurred stressors; rated on a 5-point scale ranged from 1 (not stressful at all) to 5 (very stressful).
dAge (B = −0.01, p < .01) and employment (B = −0.15, p < .05) were significant controls.
eNumber of ADS days (B = 0.09, p < .05) was a significant control.
fEmployment (B = −0.20, p < .05) was a significant control.
gEmployment (B = −0.29, p < .01) was a significant control.
**p < .001. **p < .01. *p < .05.
Turning to daily affect and health symptoms (Table 2), type of day had significant main effects for anger (B = −0.06, p < .05) and health symptoms (B = 0.03, p < .01). Anger was lower on ADS than on non-ADS days and health symptoms were higher.
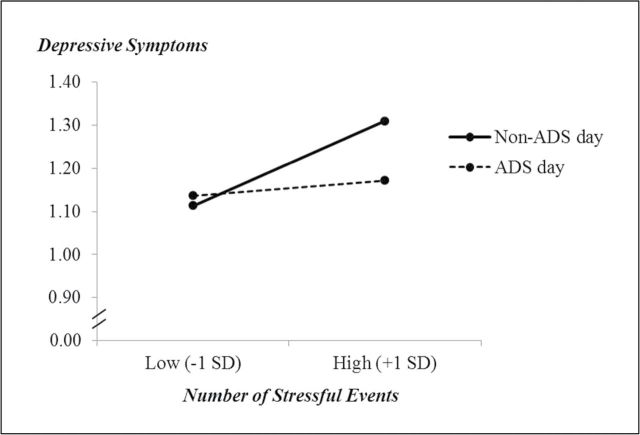
We then constructed models that examined type of day and the measures of occurrence of care-related stressors, noncare stressors, and positive events as time-varying covariates on affect and health symptoms. We tested interactions of type of day and the two stressors. Nonsignificant interactions were trimmed from the models. Although we also included the person-mean for those variables as time-invariant covariates in the models, we focused on the time-varying predictors, which capture daily fluctuation of experiences within person. As shown in Table 3, the within-person effects for care-related stressors, noncare stressors, and positive events showed significant covariations with each affect measure and health symptoms. Both types of stressors were associated with more depressive symptoms, anger, anxiety symptoms, and health symptoms and less-positive affect, whereas associations of positive events with each dependent variable were in the opposite direction. Type of day was no longer significant for anger after inclusion of care-related stressors in the model. The other daily events did not affect the association between type of day and anger. We found a significant type of day by noncare stressors interaction for depressive affect (B = −0.04, p < .05). As shown in Figure 1, when number of noncare stressors was low, type of day made no difference in depressive symptoms, but when stressors were high, depressive symptoms increased only on non-ADS days. The mean levels of stressors across all days, as indicated by the fixed effects, were significant for each of the outcome variables in the expected direction.
Table 3.
The Effects of Adult Day Service Use and Daily Experiences on Health Symptoms and Affect of Family Caregivers
| Health symptoms | Positive affect | Depressive symptoms | Anger | Anxiety symptomsa | |
|---|---|---|---|---|---|
| B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | |
| Fixed effects | |||||
| Intercept | 1.55 (0.07)** | 2.95 (0.16)** | 1.17 (0.09)** | 1.79 (0.10)** | 1.59 (0.12)** |
| Within-person predictors | |||||
| ADS use (yes = 1) | 0.04 (0.02)** | 0.01 (0.03) | 0.01 (0.02) | −0.03 (0.03) | −0.01 (0.02) |
| Care-related stressorsa | 0.01 (0.00)** | −0.01 (0.00)** | 0.01 (0.00)** | 0.04 (0.00)** | 0.02 (0.00)** |
| Noncare stressorsa | 0.06 (0.01)** | −0.08 (0.01)** | 0.05 (0.01)** | 0.17 (0.01)** | 0.08 (0.01)** |
| Positive eventsa | −0.02 (0.01)** | 0.17 (0.01)** | −0.03 (0.01)** | −0.08 (0.01)** | −0.03 (0.01)** |
| ADS use × noncare stressorsa | – | – | −0.04 (0.02)* | – | – |
| Between-person predictors | |||||
| CG Female (yes = 1) | −0.03 (0.07) | 0.05 (0.16) | 0.02 (0.09) | −0.00 (0.10) | −0.08 (0.12) |
| CG Age | −0.01 (0.00)* | 0.00 (0.01) | 0.01 (0.00) | −0.00 (0.00) | 0.00 (0.00) |
| CG employed (yes = 1) | −0.09 (0.05) | 0.07 (0.12) | −0.05 (0.07) | −0.09 (0.08) | −0.19 (0.09)* |
| Duration of care | 0.00 (0.00) | 0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| IWD ADL impairment | 0.01 (0.05) | 0.02 (0.11) | −0.08 (0.07) | −0.10 (0.07) | −0.08 (0.09) |
| Number of ADS days | 0.02 (0.02) | 0.06 (0.04) | −0.00 (0.02) | −0.01 (0.02) | 0.02 (0.03) |
| Care-related stressorsb | 0.02 (0.01)** | −0.02 (0.01) | 0.02 (0.01)** | 0.04 (0.01)** | 0.04 (0.01)** |
| Noncare stressorsb | 0.13 (0.03)** | −0.19 (0.07)** | 0.13 (0.04)** | 0.19 (0.04)** | 0.15 (0.05)** |
| Positive eventsb | −0.06 (0.03)* | 0.46 (0.06)** | −0.07 (0.03) | −0.13 (0.04)** | −0.06 (0.04) |
| Random effects | |||||
| Intercept VAR. | 0.09 (0.01)** | 0.45 (0.05)** | 0.16 (0.02)** | 0.16 (0.02)** | 0.26 (0.03)** |
| Residual VAR. | 0.07 (0.00)** | 0.19 (0.01)** | 0.06 (0.00)** | 0.21 (0.01)** | 0.15 (0.01)** |
| −2 Log Likelihood | 805.7 | 2195.0 | 731.8 | 2141.7 | 1783.4 |
| AIC | 809.7 | 2199.0 | 735.8 | 2145.7 | 1787.4 |
Notes: Participant N = 173; observation N = 1,359; ADS = adult day services; AIC = Akaike’s Information Criterion; CG = caregiver; IWD = individual with dementia; VAR = variance.
aPerson-mean-centered scores (i.e., time varying).
bPerson-mean scores across days (i.e., time invariant).
**p < .001. **p < .01. *p < .05.
Figure 1.
This graph demonstrates the interaction effect between noncare stressors and adult day service (ADS) use (B = −0.04, p < .05) on depressive symptoms. When experiencing more noncare stressors than own averages, caregivers showed more increases in depressive symptoms on non-ADS days.
Finally, we considered if number of ADS days might buffer the impact of stressors on daily affect and health symptoms (data not shown in tables). We found an interaction effect between care-related stressors and number of ADS days on depressive symptoms (B = −0.01, p < .05). Caregivers who used more ADS had smaller increases in depressive symptoms when care-related stressors were higher than did caregivers who used fewer days.
Discussion
The findings confirmed that ADS use changes the structure of daily events experienced by caregivers. Care-related stressors decreased on ADS days, whereas noncare stressors and positive events increased. Although number of events differed by type of day, subjective severity of the events was similar across days. The increases in noncare stressors and positive events on ADS days were mainly due to positive and stressful experiences at work. Rather than just adding challenges to their lives as some observers have suggested (Gottlieb & Johnson, 2000), work also provides an outlet that some caregivers report as enjoyable (Aneshensel et al., 1995).
These findings also demonstrate that in the context of chronic stress, daily affect and health symptoms were driven by daily fluctuations in exposure to stressors and positive events. Mean levels of stressors and positive events also had significant effects on levels of the outcomes, but as found in other studies that took a daily approach (Mausbach et al., 2011; Savla et al., 2011), daily measures of stressors demonstrate considerable effects on caregivers’ experiences. Further, the two types of stressors and positive events contributed independently to the explained variance in daily outcomes in all models. These findings indicate that we need to consider multiple dimensions of caregivers’ daily experiences for understanding their well-being.
The effects of ADS on daily affect and health symptoms are more complex and reflect two mechanisms: changes in stressor exposure and reactivity of ADS-emotion links. ADS use had a buffering effect on the relation of noncare stressors on depressive affect and a main effect on daily anger. The buffering effect is particularly noteworthy because ADS days were associated with a small increase in noncare stressors, yet caregivers reacted to high levels of noncare stressors with less depressive affect on ADS days than on non-ADS days. Number of ADS days used across the 8 days also buffered the effects of care-related stressors on depressive symptoms such that caregivers who used more days of ADS had smaller increases in depressive symptoms when care-related stressors were greater. In turn, anger is often an immediate and spontaneous reaction to events. By reducing exposure to care-related stressors, ADS use may allow caregivers to manage challenges without a build up of tension or frustration that leads to outbursts of anger. As found with depressive affect, ADS use allows caregivers to respond to daily challenges in a more composed way. These effects demonstrate that ADS use leads to reduced reactivity to stressors, which has positive implications for long-term health outcomes (Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013).
ADS use had no main effect on depressive or anxiety symptoms but did lead to lower care-related stressors, which in turn was associated with improved affect. ADS days were also unexpectedly associated with a small increase in health symptoms. It may be that when caregivers have time away from the IWD, it gives them more time to focus on themselves and on minor health symptoms that they otherwise might ignore. We also considered if caregivers might have sent their IWDs to ADS on some days specifically because they were not feeling well. To test this possibility, we reran the analysis excluding ADS days that were not part of caregivers’ planned schedule for using ADS (n = 36 days), but the findings were unchanged. Whether there is a more direct link of increased health symptoms with ADS use needs to be explored further.
A fundamental assumption of ADS and other respite programs is that stressors on caregivers are relieved and create opportunities for restorative activities. The current study found evidence that directly links daily use of respite to improved daily affect. The study also showed that caregivers do more than relax on ADS days but encounter other challenges, whether related to work, family, or other areas, and have positive experiences as well. The finding that ADS use is associated with temporary relief is encouraging and suggests that it could play a critical role in comprehensive efforts to assist caregivers and to prevent a downward spiral of emotional and physical health. Programs such as ADS-Plus (Gitlin, Reever, Dennis, Mathieu, & Hauck, 2006), which provide services specifically for caregivers, may be able to target ongoing concerns not addressed by respite alone, thereby augmenting benefits to caregivers.
There are limitations of this research. There may be selection bias in the sample. We depended on caregivers to volunteer for the research and do not know how many caregivers heard about the research and decided not to contact us. Participation in ADS by itself and sharing a household with the care recipient may introduce additional biases. On the other hand, the sample reported fairly typical levels of stressors and affect compared with other caregivers of IWDs.
Finally, we view the significance of these daily effects as analogous to many medical treatments. An analgesic, for example, is considered successful if it reduces pain on the day it is administered. Policy makers are concerned with long-term benefits of respite programs (e.g., lower health costs, delayed institutionalization). Daily benefits of ADS, however, have intrinsic value and can lead to a better understanding of long-term impact although examination of factors such as differences in response to, dosage, and cumulative effects of ADS use need to be undertaken.
Funding
This research was supported by National Institute of Aging (R01 AG031758, “Daily Stress and Health Study”).
References
- Almeida D. M. (1998). Daily Inventory of Stressful Events (DISE) expert coding manual. Tucson, AZ: Division of Family Studies and Human Development, University of Arizona; [Google Scholar]
- Almeida D. M. (2005). Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science, 14, 64–68. 10.1111/j.0963-7214.2005.00336.x [Google Scholar]
- Almeida D. M., McGonagle K., King H. (2009). Assessing daily stress processes in social surveys by combining stressor exposure and salivary cortisol. Biodemography and Social Biology, 55, 219–237. 10.1080/19485560903382338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida D. M., Wethington E., Kessler R. C. (2002). The daily inventory of stressful events: an interview-based approach for measuring daily stressors. Assessment, 9, 41–55. 10.1177/1073191102091006 [DOI] [PubMed] [Google Scholar]
- Aneshensel C. S., Pearlin L. I., Mullan J. T., Zarit S. H., Whitlatch C. J. (1995). Profiles in caregiving: The unexpected career. New York: Academic Press; [Google Scholar]
- Barlow D. H., Nock M. K., Hersen M. (2009). Single case experimental designs: Strategies for studying behavior change (3rd ed.). Boston, MA: Pearson Allyn & Bacon; [Google Scholar]
- Bolger N., Davis A., Rafaeli E. (2003). Diary methods: Capturing life as it is lived. Annual Review of Psychology, 54, 579–616. 10.1146/annurev.psych.54.101601.145030 [DOI] [PubMed] [Google Scholar]
- Bollen K. A., Lennox R. (1991). Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin, 110, 305–314. 10.1037/0033-2909.110.2.305 [Google Scholar]
- Charles S. T., Almeida D. M. (2006). Daily reports of symptoms and negative affect: Not all symptoms are the same. Psychology and Health, 21, 1–17. 10.1080/147683205001129239 [Google Scholar]
- Ensel W. M., Lin N. (1991). The life stress paradigm and psychological distress. Journal of Health and Social Behavior, 32, 321–341. 10.2307/2137101 [PubMed] [Google Scholar]
- Fauth E. B., Zarit S. H., Femia E. E., Hofer S. M., Stephens M. A. (2006). Behavioral and psychological symptoms of dementia and caregivers’ stress appraisals: Intra-individual stability and change over short-term observations. Aging & Mental Health, 10, 563–573. 10.1080/13607860600638107 [DOI] [PubMed] [Google Scholar]
- Femia E. E., Zarit S. H., Stephens M. A., Greene R. (2007). Impact of adult day services on behavioral and psychological symptoms of dementia. The Gerontologist, 47, 775–788. 10.1093/geront/47.6.775 [DOI] [PubMed] [Google Scholar]
- Gitlin L. N., Reever K., Dennis M. P., Mathieu E., Hauck W. W. (2006). Enhancing quality of life of families who use adult day services: Short- and long-term effects of the adult day services plus program. The Gerontologist, 46, 630–639. 10.1093/geront/46.5.630 [DOI] [PubMed] [Google Scholar]
- Gottlieb B. H., Johnson J. (2000). Respite programs for caregivers of persons with dementia: A review with practice implications. Aging and Mental Health, 4, 119–129. 10.1080/13607860050008637 [Google Scholar]
- Hoffman L., Stawski R. S. (2009). Person as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. 10.1080/15427600902911189 [Google Scholar]
- Katz S., Ford A. B., Moskowitz R. W., Jackson B. A., Jaffe M. W. (1963). Studies of illness in the aged. The index of adl: A standardized measure of biological and psychosocial function. JAMA: the Journal of the American Medical Association, 185, 914–919. 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Andrews G., Colpe L. J., Hiripi E., Mroczek D. K., Normand S. -L. T., Walters E. E., Zaslavsky A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psyshological distress. Psychological Medicine, 32, 959–976. 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- Koerner S. S., Shirai Y., Kenyon D. B. (2010). Socio-contextual circumstances in daily stress reactivity among caregivers for elder relatives. Journal of Gerontology: Psychology Sciences, 65, P561–P572. 10.1093/geronb/gbq045 [DOI] [PubMed] [Google Scholar]
- Larsen R. J., Kasimatis M. (1991). Day-to-day physical symptoms: Individual differences in the occurrence, duration, and emotional concomitants of minor daily illnesses. Journal of Personality, 59, 387–423. 10.1111/j.1467-6494.1991.tb00254.x [DOI] [PubMed] [Google Scholar]
- Lawton M. P., Brody E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9, 179–186. 10.1093/geront/9.3_Part_1.179 [PubMed] [Google Scholar]
- Littell R. C., Miliken G. A., Stroup W. W., Wolfinger R. D. (1996). SAS systems for mixed models. Cary, NC: SAS Institute; [Google Scholar]
- Mausbach B. T., Harmell A. L., Moore R. C., Chattillion E. A. (2011). Influence of caregiver burden on the association between daily fluctuations in pleasant activities and mood: A daily diary analysis. Behaviour Research and Therapy, 49, 74–79. 10.1016/j.brat.2010.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek D. K., Kolarz C. M. (1998). The effect of age on positive and negative affect: A developmental perspective on happiness. Journal of Personality and Social Psychology, 75, 1333–1349. 10.1037// 0022-3514.75.5.1333 [DOI] [PubMed] [Google Scholar]
- Piazza J. R., Charles S. T., Sliwinski M. J., Mogle J., Almeida D. M. (2013). Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 45, 110–120. 10.1007/s12160-012-9423-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savla J., Almeida D. M., Davey A., Zarit S. H. (2008). Routine assistance to parents: effects on daily mood and other stressors. Journal of Gerontology: Social Sciences, 63, S154–S161. 10.1093/geronb/ 63.3.S154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savla J., Roberto K. A., Blieszner R., Cox M., Gwazdauskas F. (2011). Effects of daily stressors on the psychological and biological well-being of spouses of persons with mild cognitive impairment. Journal of Gerontology: Psychological Sciences, 66, P653–P664. 10.1093/geronb/gbr041 [DOI] [PubMed] [Google Scholar]
- Seltzer M. M., Almeida D. M., Greenberg J. S., Savla J., Stawski R. S., Hong J., Taylor J. L. (2009). Psychosocial and biological markers of daily lives of midlife parents of children with disabilities. Journal of Health and Social Behavior, 50, 1–15. 10.1177/002214650905000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teri L. (1997). Behavior and caregiver burden: Behavioral problems in patients with Alzheimer disease and its association with caregiver distress. Alzheimer Disease and Associated Disorders, 11(Suppl 4)S35–S38 [PubMed] [Google Scholar]
- Watson D., Clark L. A., Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Watson D., Tellegen A. (1985). Toward a consensual structure of mood. Psychological Bulletin, 98, 219–235. 10.1037/0033-2909.98.2.219 [DOI] [PubMed] [Google Scholar]
- Zarit S. H., Kim K., Femia E. E., Almeida D. M., Savla J., Molenaar P. C. (2011). Effects of adult day care on daily stress of caregivers: A within-person approach. Journal of Gerontology: Psychological Sciences, 66, P538–P546. 10.1093/geronb/gbr030 [DOI] [PMC free article] [PubMed] [Google Scholar]