Abstract
Although depression and conduct disorder frequently co-occur with substance use disorders (SUDs), few studies have investigated the individual and interactive effects of these conditions on SUD treatment outcome. Data were collected from 90 adolescents aged 13–21 (M = 17.1, SD = 2.07) who received a brief evidence-based intervention for SUD. Hierarchical regressions assessed the relationship among demographic variables, depression, conduct disorder, and two substance use outcomes (frequency and problems) at two intervals (three months, six months). Results revealed that higher baseline substance use and lower socioeconomic status significantly predicted higher substance problems and frequency at three-months. At six months, higher three month substance problems and lower depressive symptoms predicted substance problems. In addition, an interaction indicated that the effect of conduct disorder on substance problems was greatest at lower levels of depression. Results are discussed in the context of previous research indicating mixed effects of depression on SUD treatment outcome.
Keywords: Adolescent, substance use disorder, treatment, comorbidity, depression
Introduction
Over 50% of adolescents who meet criteria for a substance use disorder (SUD) will also meet criteria for a co-occurring mental health condition (Armstrong & Costello, 2002). In clinical samples, rates of comorbid substance use and mental health diagnoses can reach as high as 75% (Grella, Hser, Joshi, & Rounds-Bryant, 2001). Comorbid youth generally begin using substances at an earlier age, and use more frequently and chronically than do those without a comorbid condition (Grella et al., 2001; Rowe, Liddle, Greenbaum, & Henderson, 2004). Relative to youth with only an SUD diagnosis, comorbid teens also have more interpersonal difficulties, school and legal problems, suicidal behavior, sexual or physical abuse, and parental substance use or mental health problems (Couwenbergh, Brink, Zwart, Vreugdenhill, van Wijngaarden-Cremers, & van der Gaag, 2006; Grella et al., 2001; Rowe et al., 2004).
Comorbid youth present to treatment reporting more frequent substance use, use of greater amounts of substances, more withdrawal symptoms, and higher rates of substance dependence (e.g., Shane, Jasiukaitis, & Green, 2003; Tomlinson, Brown, & Abrantes, 2004). Additionally, clinical studies indicate that comorbid youth have different treatment outcomes (e.g., Grella et al., 2001; Tomlinson et al., 2004). In the Drug Abuse Treatment Outcome Study-Adolescents (DATOS-A), Grella and colleagues (2001) found that compared with SUD-only adolescents, those with mental health diagnoses were more likely to use marijuana and hallucinogens during the 12 months following SUD treatment. Rowe and colleagues’ (2004) similarly found that those with an SUD only had a significantly faster rate of improvement than those with an additional comorbidity. Furthermore, those with an SUD plus both internalizing and externalizing comorbidities had the worst trajectory of substance use post-treatment.
Several studies support the need to consider more specifically the associations of depression with adolescent substance abuse treatment outcome. Among adolescents treated for alcohol use disorders, comorbid depression predicts earlier alcohol relapse (Cornelius et al., 2004). Further, having both an SUD and depression increases the risk of negative and potentially lethal outcomes, including suicidal ideation, attempts, and completed suicide (Curry et al., 2003). For instance, one school-based study found that juniors and seniors who attempted suicide were more likely to have both an SUD and depression than either of these disorders alone (Wagner, Cole, & Schwartzman, 1996). It is also noteworthy that relative to adolescents with poor depression treatment response, adolescents with positive treatment response experience lower probability of subsequent SUDs, whether the treatment is CBT or another intervention (Curry et al., 2012).
Although a number of studies provide evidence suggesting that depression is associated with worse SUD treatment outcomes (e.g., Cornelius, 2004; Dobkin, Chabot, Maliantovich, & Craig, 1998; Vourakis, 2005; White et al., 2004), several studies have failed to replicate this finding. For instance, two studies investigating depression’s effect on SUD treatment found no impact (Crowley, Mikulich, MacDonald, Young, & Zerbe, 1998; Whitmore, Mikulich, Ehlers, & Crowley, 2000), and a residential treatment study showed a positive impact (Deskovitz, Key, Hill, & Franklin, 2004). These mixed results may be partly explained by wide variability in assessment measures, trial methodology, treatment modality, and setting (ranging from ER visits to residential treatment). Additional clarification of these mixed findings may be gained by simultaneous consideration of comorbid conduct disorder.
Conduct disorder is the most frequent comorbid condition in SUD adolescents (Armstrong & Costello, 2002) and having an early diagnosis of it has been shown to be associated with double the risk for an SUD (Sung, Erkanli, Angold, & Costello, 2004). Further, conduct disorder is associated with adolescent initiation of alcohol use, onset of alcohol-related problems, and development of alcohol abuse or dependence (e.g., Deas & Thomas, 2002). The deleterious effects of comorbid conduct disorder on SUD treatment outcome are strong and consistently replicated. Comorbid conduct disorder is associated with poorer SUD treatment outcomes, including greater frequency of substance use, substance-related problems, and substance withdrawal symptoms (Brown, Gleghorn, Schuckit, Myers, & Mott, 1996; Galaif, Hser, Grella, & Joshi, 2001; Grella et al., 2001; Hser, Grella, Collins, & Teruya, 2003). Comorbidity of conduct disorder with depression is also common (Angold & Costello, 1993) and some evidence suggests that the highest prevalence of SUDs exists in adolescents with both conduct disorder and depression (Greenbaum, Prange, Friedman, & Silver, 1991).Thus, it is important to investigate conduct disorder when researching the influence of depression on adolescent SUD treatment outcome.
A primary limitation of prior research has been a broad focus on internalizing and externalizing comorbidities, with relatively less inquiry into specific diagnoses (e.g., Shane et al., 2003; Winters, Stinchfield, Latimer, & Stone, 2008). A second limitation of prior research has been failure to consider both individual and interactive effects. While prior studies have shown that the combination of specific conditions are often associated with worse treatment outcomes, it is not clear whether the combined effect is worse than the additive effects of the individual conditions. Using only categorical diagnoses to research comorbidity is a third limitation of prior research. Studies have shown that sub-threshold depression significantly impairs adults and youths (Gonzalez-Tejera et al., 2005; Judd, Paulus, Wells, & Rapaport, 1996; Rapaport & Judd, 1998). Relying upon categorical diagnoses ignores the many adolescents who have defining symptoms of the disorders and related impairment but do not meet diagnostic criteria.
The current study addresses the aforementioned limitations by investigating the individual and interactive effects of depression and conduct disorder on substance use outcomes three and six months after initiation of brief treatment. In order to provide a robust view of the influence of comorbidity, the current study examines two substance use outcomes: frequency and problems. Based on previous research, it was hypothesized that 1) higher severity scores on depression and/or conduct disorder scales would predict greater substance frequency and problems at three and six month follow-up and 2) the interactive effects of the two comorbidities would be greater than their additive effects.
The treatment in this study was an integrated motivational enhancement therapy (MET) and cognitive-behavioral therapy (CBT). In a review of adolescent SUD treatment studies, Becker and Curry (2008) found evidence that CBT had proportionally more methodologically strong studies than other effective treatment modalities and that CBT had comparable or superior treatment effectiveness. In a study with dually-diagnosed adolescents, researchers found that CBT led to a significant reduction in the severity of substance use suggesting that CBT is a useful treatment for youth with substance abuse and comorbid disorders (Kaminer, Burleson, Blitz, Sussman, & Rounsaville, 1998). It is particularly useful to incorporate MET in CBT with SUD youth because of their frequently low treatment motivation and poor treatment retention (Crits-Christoph & Siqueland, 1996). Sampl and Kadden (2001) developed a brief outpatient treatment combining MET and CBT, for use in the Cannabis Youth Treatment (CYT) experiment (Dennis et al., 2004). This treatment, MET/CBT-5, consists of two sessions of motivation enhancement and three sessions of cognitive behavioral skill building, as described more completely below. Despite its brevity, MET/CBT-5 led to significant reductions in substance use during the CYT experiment, with results equivalent to those of four more intensive outpatient interventions (Dennis et al., 2004). Thus, there was reason to expect that MET/CBT-5 would be associated with meaningful change in substance use that would enable us to examine treatment outcome in the current study.
Cognitive behavioral therapy (CBT) may be effective with substance abusing adolescents because it addresses social cognitive variables central to substance abuse. Among these are favorable expectancies about alcohol and drug effects, poor consequential thinking (with resultant impulsivity), and poor assertion skills in substance use situations (Beck, Wright, Newman, & Liese, 1993; Weinberg, Rahdert, Colliver, & Glantz, 1998). Similarly, CBT may address the negative automatic thoughts or social withdrawal characteristic of adolescent depression (Garber et al., 1993; Ingram et al., 2007; Becker & Curry, 2007), and/or the poor problem-solving and hostile attribution bias characteristic of adolescents with conduct disorder (Lochman, Powell, Whidby, & FitzGerald, 2012). In MET/CBT-5, MET sessions focus in part on the already experienced consequences of drug or alcohol use, and on potential reasons for quitting, thus contributing to consequential thinking. Goal-setting, which has been found helpful for children with externalizing disorders, such as conduct disorder, is a major outcome of the second MET session. The three CBT sessions address refusal skills, a form of assertion in situations that may lead to substance use; social support, which may serve to counter the withdrawal of depressed adolescents as well as to facilitate the process of overcoming substance misuse; and preparation to deal with relapse risk situations, a form of ‘thinking ahead’ and planning.
Methods
This study represents a secondary analysis of data collected by one of 36 sites participating in the Substance Abuse and Mental Health Services Administration’s Effective Adolescent Treatment (EAT) Initiative, which aimed to increase the adoption of a brief, evidence-based intervention (MET/CBT-5) for adolescent SUDs.
Participants and Procedures
Procedures have been described in prior publications (Becker, Curry, Yang, 2009; Becker, Curry, Yang, 2011). Briefly, cannabis or alcohol abusing adolescents, aged 13 to 21 years old, were referred from community clinics, local college counseling centers, and local advertisements. Participants were excluded if: (1) their substance use was severe enough to warrant more intensive treatment; (2) their substance use disorder did not include alcohol or marijuana as the primary substance; (3) they were experiencing an acute untreated psychiatric or medical condition that required immediate attention or would hinder participation in the treatment study; (4) they exhibited insufficient mental capacity to comprehend research procedures or participate in treatment. In an effort to increase generalizability, adolescents were not excluded for receiving concomitant medication or psychotherapy although participants were asked to refrain from additional services targeting substance abuse while in the study.
The sample for this study included 90 adolescents (76.2% male) who completed the baseline and three month follow-up assessments. Additionally, 73 of these adolescents also completed the six month follow-up assessment. Participants were primarily Caucasian (75.6%) with some African American (8.9%), Latino (1.1%), and mixed race participants (14.4%). Mean age was 17.1 (SD = 2.07) with 62% of youth under 18 years of age.
Using IRB-approved procedures, written informed consent was obtained for participants age 18 and older. For those under 18 years of age, written parental consent and adolescent assent were obtained. Adolescents were administered a comprehensive diagnostic interview by a trained interviewer at baseline, three months, six months, and 12 months. To focus on acute treatment outcome, only the three and six month assessments are included in the current analysis.
Intervention
Participants received an outpatient intervention consisting of two sessions of motivational enhancement therapy and three sessions of cognitive behavior therapy (MET/CBT-5; Sampl & Kadden, 2001). MET-1 initially includes rapport building, review of alcohol and drug use and related problems, and psycho-education about the treatment. MET-2 continues this process and includes a functional analysis of the adolescent’s substance use, ending with the setting of treatment goals. The three subsequent CBT sessions follow a consistent session structure, in which skill building is embedded. In each session, the therapist and adolescent review previous homework tasks and progress toward goals, and then focus on a skill essential to overcoming substance abuse. Skills include learning how to: refuse drugs or alcohol; seek social support from adults and peers; and plan for and cope with high substance abuse risk situations. Following the standard MET/CBT-5 treatment, adolescents were offered a final session focused on interpretive feedback and the provision of appropriate recommendations. To ensure therapist competence and adherence, a stringent protocol utilizing a train-the-trainers model and weekly supervision was implemented (For more details see Becker, Livas Stein, Curry, & Hersh, 2012).
Measures
Ratings of substance use and psychopathology were determined by responses to scales included in the comprehensive interview, the Global Appraisal of Individual Needs (GAIN; Dennis, Titus, White, Unsicker, & Hodgkins, 2003).
The Substance Problem Scale (SPS) is a count of 16 substance-related problems that an individual endorses having over the past month. The problems include symptoms of abuse and dependence referenced in the Diagnostic and Statistical Manual of Mental Disorders (e.g., tolerance; failed responsibilities) (American Psychiatric Association [DSM-IV-TR], 2000) as well as physical health and psychological problems related to substance use. Higher scores reflect increasing problems. Consistent with other studies (Dennis et al., 2003) the current study yielded a Cronbach's alpha of .79 for SPS at baseline.
The Substance Frequency Scale (SFS) is a multiple item measure that averages: percent of days reported of alcohol, marijuana, crack/cocaine and heroin/opioid use during the past 90 days; days of heavy alcohol or drug (AOD) use; days of problems from AOD use; and days of use in risky situations. Scores range from 0.00 to 1.00. Also consistent with other studies (Dennis et al., 2003) the current study yielded a Cronbach's alpha of .78 for SFS at baseline.
The Depressive Symptom Scale (DSS) consists of nine items and represents a count of the DSM-IV symptoms commonly associated with depression (e.g., feeling depressed and lonely, loss of interest or pleasure) over the past year. The Conduct Disorder Scale (CDS) consists of 15 items and reflects a count of DSM-IV symptoms of conduct disorder (e.g., setting fires and stealing) over the past year, with higher scores suggesting more delinquency. Internal consistency of these scales was .77 for DSS and .76 for CDS.
Demographic variables including age, gender, race, and socioeconomic status (SES) were based on adolescent report. Age was dichotomized to account for differences between high school age (13–17 years) and college-age (18–21 years) youth. SES was calculated using the Hollingshead (1975) 4-factor scale of mother’s and father’s occupations and levels of education.
Analytical plan
Baseline correlations and paired t-tests were examined to determine if demographic and comorbidity scores were associated with substance problems and substance frequency. Then, hierarchical regressions tested the study hypotheses. In each hierarchical regression, baseline demographic and substance use variables were entered in the first step. For parsimony, demographic variables that were non-significant were removed from the model. In the second step, DSS and CDS baseline scores were entered into the model to allow for a direct comparison of coefficients. The DSS*CDS interaction was added in the third step to examine the interactive effect beyond that of the individual scales. Each continuous variable was standardized and centered to reduce multicollinearity among the variables and allow for more meaningful interpretations of the regression coefficients.
Results
Sample Characteristics
Baseline means, standard deviations, and correlations among the variables are shown in Table 1. Paired t-tests did not reveal any differences in baseline substance problems or frequency as a function of age, gender or race (Caucasian vs. minority).
Table 1.
Means, Standard Deviations, and Intercorrelations Among Baseline Variables
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. SPS | 1 | ||||
| 2. SFS | .55** | 1 | |||
| 3. Socioeconomic status | .04 | .06 | 1 | ||
| 4. DSS | .23* | .02 | −0.17 | 1 | |
| 5. CDS | .26* | .22* | −0.04 | .37** | 1 |
| Mean | 4.99 | .16 | 25.12 | 3.22 | 2.73 |
| SD | 3.35 | .11 | 11.28 | 2.50 | 2.47 |
Note.
N=90.
p < .05.
p < .001.
SPS = Substance Problem Scale; SFS = Substance Frequency Scale; DSS = Depressive Symptom Scale; CDS = Conduct Disorder Scale.
Chi-squares and independent sample t-tests were conducted to assess whether the 17 participants who dropped out of the study after the three month assessment systematically differed from the 73 participants who completed the six month assessment. Assessment dropouts did not significantly differ from completers by age [t(88) = .09, p = .93], race [χ2(1, N = 90) = .47, p = .49], or gender [χ2(1, N = 90) = .30, p = .59]. Additionally, dropouts and completers did not significantly differ by baseline scores on the substance use measures (SPS [t(88) = −1.44, p = .15]; SFS [t(88) = −1.23, p = .22]) or on the CDS [t(88) = 1.04, p = .30]. However, dropouts had higher DSS scores [t(88) = 1.99, p = .05].
Anticipated treatment duration for the five sessions was 6 to 7 weeks. Retention in the MET/CBT-5 protocol was very good (M = 4.6 sessions, SD = 1.02), with 98% of adolescents receiving at least the two MET sessions and 87% receiving all five sessions. The 17 assessment dropouts did not significantly differ from the 73 completers by number of sessions received [t(88) = −.213, p = .83].
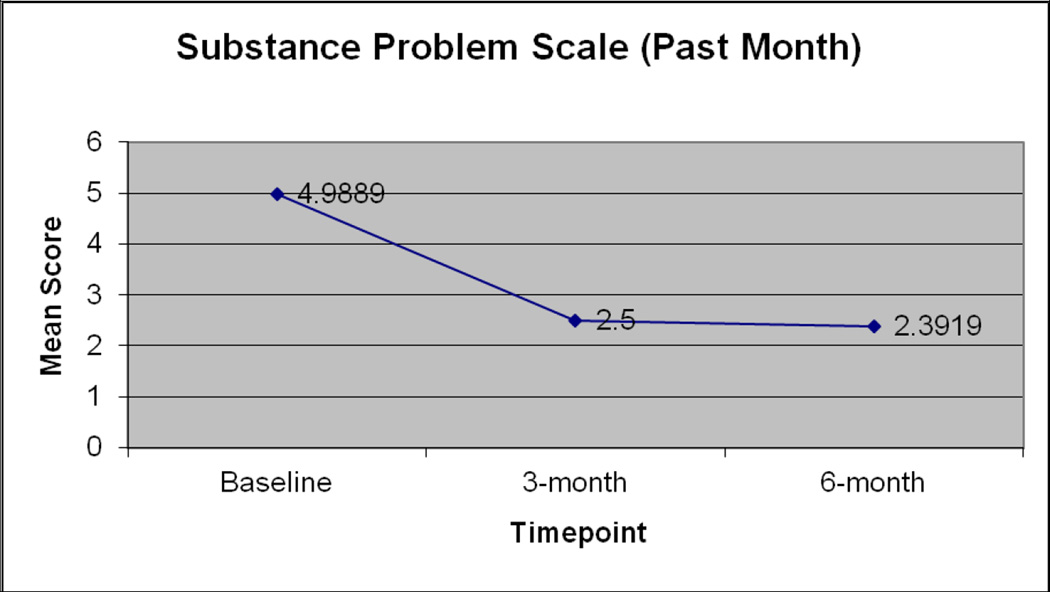
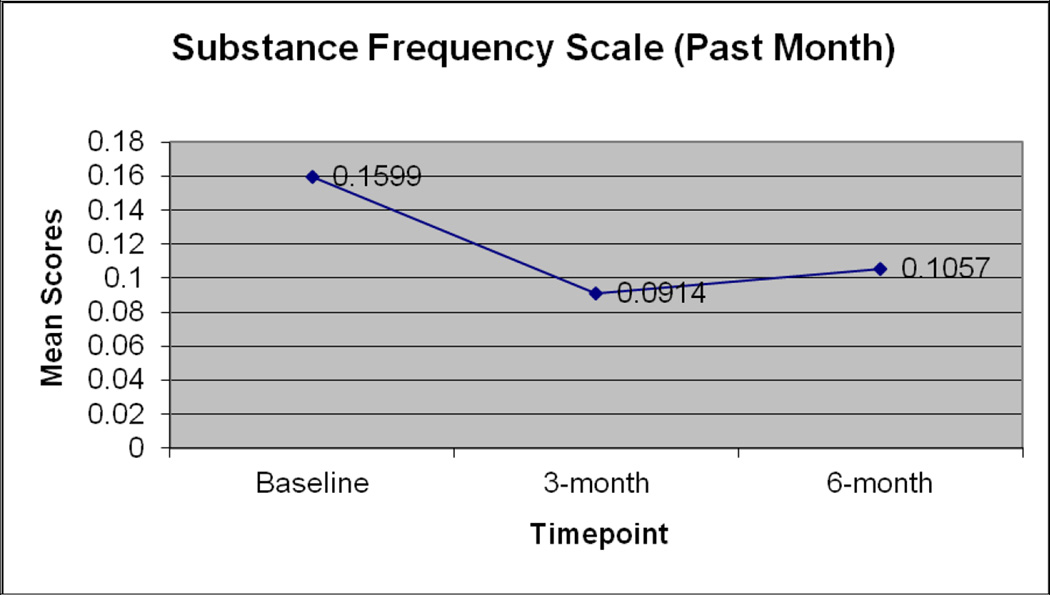
Treatment Effectiveness
Paired-samples t-tests were conducted to examine if the MET/CBT-5 treatment had an effect on substance problems and frequency at three and six months. Although the lack of a control condition precludes causal inferences, the treatment was associated with favorable results. As shown in Figure 1, there was a significant decrease in SPS scores from baseline (M= 4.99, SD= 3.35) to three months (M= 2.50, SD= 3.14; t(89) = 6.26, p < .001) and from baseline to six months (M= 2.39, SD= 2.72; t(73) = 6.45, p < .001). Similarly for SFS, as shown in Figure 2, both three month (M= .10, SD= .11) and six month (M= .10, SD= .11) scores were significantly lower than baseline scores (M= .16, SD= .11). Estimates of Cohen’s d effect sizes were calculated by subtracting the mean pre-treatment score from the mean post-treatment score and dividing the difference by the standard deviation of the pre- to post- difference scores. For SPS, the effect sizes for baseline to three month and baseline to six month were .66 and .75, respectively. For SFS, the effect sizes for baseline to three month and baseline to six month were .64 and .51, respectively.
Figure 1.
Mean substance problems scores at baseline, three months, and six months.
Figure 2.
Mean substance frequency scores at baseline, three months, and six months.
Hierarchical Regression of Follow-up Substance Problems
Results of the hierarchical regression predicting substance problems at three months are presented in Table 2. The first step examined whether demographic variables or baseline SPS significantly predicted substance problems at three months. Race, age, and gender were non-significant and were dropped from the final regression. SES and baseline SPS were significant, with lower SES scores [β = −0.28, t(84) = −2.88, p < .05] and higher baseline SPS scores [β = 0.31, t(84) = 3.02, p < .05] predicting higher SPS scores at three month follow-up.
Table 2.
Hierarchical Regression Analysis for Variables Predicting Adolescent Substance Problems at three month follow-up (N=90)
| Predictors | B | β | t | p | ESa | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | 0.192 | |||||
| Baseline SPS | 0.33 | 0.35 | 3.63 | 0.000* | 0.12 | |
| Socioeconomic status | −0.07 | −0.29 | −3.02 | 0.003* | 0.08 | |
| Step 2 | 0.032 | |||||
| Depression | 0.08 | 0.06 | .58 | 0.560 | 0.00 | |
| Conduct Disorder | 0.20 | 0.16 | 1.49 | 0.141 | 0.02 | |
| Step 3 | 0.002 | |||||
| Depression X Conduct Disorder | −0.22 | −0.07 | −0.69 | 0.490 | 0.00 |
Note.
Effect size measured by squared semi-partial correlations (Type II).
p < .05.
SPS = Substance Problem Scale; DSS = Depressive Symptom Scale; CDS = Conduct Disorder Scale.
In the second and third regression steps, neither DSS [β = .06, t(85) = .58, p = .56] nor CDS [β = .16, t(85) = 1.49, p = .14], nor their interaction [β = −.07, t(84) = −.69, p = .49] uniquely contributed to the prediction of substance problems at three month follow-up. The final model accounted for 22.9% of the variance in three month substance problems.
Results of the hierarchical regression predicting substance problems at six months are presented in Table 3 with unadjusted change in R-square values. None of the demographic variables significantly predicted six month substance problems. Hence only substance problems at baseline and three months (to account for potential changes in use during treatment) were included in the first step of the regression. In the final regression model, only three month SPS [β = 0.57, t(67) = 5.46, p < .0001] and baseline DSS [β = −0.25, t(67) = −2.27, p < .05] predicted six month substance problems. Higher three month SPS scores and lower DSS scores were each associated with higher six month problems. Baseline substance problems, CDS, and the DSS*CDS interaction were non-significant. The final model accounted for 40.09% of the variance in six month problems.
Table 3.
Hierarchical Regression Analysis for Variables Predicting Adolescent Substance Problems at six month follow-up (N=73)
| Predictors | B | β | t | p | ESa | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | 0.344 | |||||
| Baseline SPS | 0.08 | 0.10 | 0.95 | 0.347 | 0.01 | |
| Three month SPS | 0.47 | 0.55 | 5.39 | 0.000* | 0.27 | |
| Step 2 | 0.037 | |||||
| Depression | −0.25 | −0.22 | −2.01 | 0.048* | 0.04 | |
| Conduct Disorder | 0.08 | 0.07 | 0.65 | 0.518 | 0.00 | |
| Step 3 | 0.020 | |||||
| Depression X Conduct Disorder | −0.40 | −0.15 | −1.49 | 0.142 | 0.02 |
Note.
Effect size measured by squared semi-partial correlations (Type II).
p < .05.
SPS = Substance Problem Scale; DSS = Depressive Symptom Scale; CDS = Conduct Disorder Scale.
Hierarchical Regression of Follow-up Substance Frequency
Two separate hierarchical regressions were conducted predicting substance frequency at three and six months. Results for the three and six month outcomes are summarized in Tables 4 and 5, respectively. For three month SFS scores, demographic variables and baseline SFS were entered in the first step. Race, age, and gender were non-significant and were dropped from the final model. Conversely, SES [β = −0.24, t(84) = −2.48, p < .05] and baseline SFS [β = 0.50, t(84) = 5.50, p < .0001], were significant, with lower SES scores and higher baseline SFS scores predicting higher three month SFS scores. Neither the comorbidity scales nor their interaction uniquely predicted substance frequency at three month follow-up. The final model accounted for 30.3% of the variance in three month frequency.
Table 4.
Hierarchical Regression Analysis for Variables Predicting Adolescent Substance Frequency at three month follow-up (N=90)
| Predictors | B | β | t | p | ESa | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | 0.302 | |||||
| Baseline SFS | 0.48 | 0.53 | 5.86 | 0.000* | 0.28 | |
| SES | −0.00 | −0.23 | −2.50 | 0.014* | 0.05 | |
| Step 2 | 0.000 | |||||
| Depression | 0.00 | 0.01 | .13 | 0.899 | 0.00 | |
| Conduct Disorder | −0.00 | −0.00 | −0.04 | 0.971 | 0.00 | |
| Step 3 | 0.000 | |||||
| Depression X Conduct Disorder | 0.00 | 0.02 | 0.19 | 0.851 | 0.00 |
Note.
Effect size measured by squared semi-partial correlations (Type II).
p < .05.
SFS = Substance Frequency Scale; DSS = Depressive Symptom Scale; CDS = Conduct Disorder Scale.
Table 5.
Hierarchical Regression Analysis for Variables Predicting Adolescent Substance Frequency at six month follow-up (N=73)
| Predictors | B | β | t | p | ESa | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | 0.755 | |||||
| Baseline SFS | −0.04 | −0.04 | −0.64 | 0.525 | 0.00 | |
| Three month SFS | 0.99 | 0.89 | 12.94 | 0.000* | 0.58 | |
| Step 2 | 0.001 | |||||
| Depression | −0.00 | −0.02 | −0.33 | 0.742 | 0.00 | |
| Conduct Disorder | 0.00 | 0.03 | 0.42 | 0.674 | 0.00 | |
| Step 3 | 0.015 | |||||
| Depression X Conduct Disorder | −0.02 | −0.15 | −2.41 | 0.019* | 0.02 |
Note.
Effect size measured by squared semi-partial correlations (Type II).
p < .05.
SFS = Substance Frequency Scale; DSS = Depressive Symptom Scale; CDS = Conduct Disorder Scale.
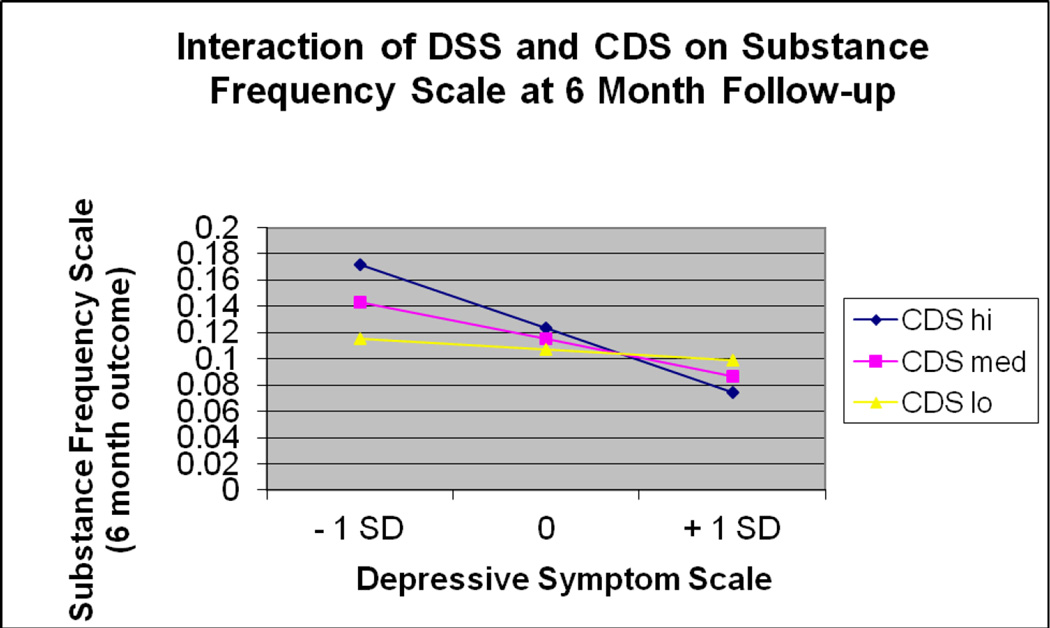
For the six month SFS scores, demographic variables were again tested in the first step. None of the demographic variables were significant and hence were dropped from the model. Baseline and three month SFS scores were included in the first step as controls. In the final model, only three month SFS scores [β = 0.89, t(67) = 13.11, p < .0001] and the DSS*CDS interaction was significant [β = −0.15, t(67) = −2.41, p < .05]. The final model accounted for 77.6% of the variance in six month frequency.
The DSS* CDS interaction was probed by plotting the regression of substance frequency at six month follow-up on depression at three severity levels of conduct disorder: high (M + 1 SD), moderate (M), and low (M - 1 SD) as suggested by Cohen, Cohen, West, and Aiken (2003). The plot of the simple regression lines (Figure 3) confirmed that the effect of depression varied across levels of conduct disorder. Results indicated that higher levels of conduct disorder were associated with more frequent six month substance use among adolescents with lower levels of depression.
Figure 3.
Interaction of baseline depression (DSS) and conduct disorder (CDS) on substance frequency at six month follow-up.
Discussion
Past research suggests that adolescents with an SUD diagnosis plus another DSM Axis I disorder enter treatment with more frequent alcohol use and more withdrawal symptoms than SUD-only youth (Shane et al., 2003; Tomlinson et al., 2004). Having both an SUD and depression has been associated with increased likelihood and faster rate of relapse (Greenfield et al., 1998; White et al., 2004). In the present study, contrary to hypotheses, comorbidity did not consistently predict increased substance problems or frequency. Baseline depression symptoms were higher in dropouts compared to completers suggesting that baseline depression symptoms affected retention in a negative way. However, baseline depressive symptomatology predicted six month substance use problems in the direction opposite to our hypothesis: higher baseline depressive symptoms were associated with fewer substance problems at six months.
Prior research also implies that youth who have both internalizing and externalizing psychopathology may have the worst trajectories (Rowe et al., 2004). For instance, Shane and colleagues (2003) found that these adolescents enter and end treatment with the most substance-related problems and experience a higher likelihood of relapse. Due to the frequent co-occurrence of depression and conduct disorder with SUD, the current study hypothesized that the interactive effect of these two comorbidities would be greater than their additive effects.
In partial support of this hypothesis, the current study found that baseline depression and conduct disorder symptoms had a significant interactive effect on substance use frequency at six months. Analysis of the interaction revealed that increased conduct disorder symptoms at baseline were more strongly associated with increased substance use frequency at six months among youth with low levels of baseline depression than among those with high levels of depression. When combined with the finding that low levels of baseline depression predicted more six month substance problems, these data suggest that among the current sample of adolescents receiving a brief evidence-based treatment for SUDs, depression symptoms may be associated with better SUD treatment outcomes. This is consistent with some past research demonstrating that increased depression is associated with better alcohol, health, and substance-related treatment outcomes (e.g., Deskovitz et al., 2004; Kranzler, Del Boca, & Rounsaville, 1996; Powell, Penick, Othmer, Bingham, & Rice, 1982). Several researchers have hypothesized that the association between higher levels of depression and better treatment outcomes is related to motivation (Blood & Cornwall, 1994; Pagnin, Queiroz, & Saggese, 2005; Tapert et al., 2003). One prevailing theory is that the self-perception of distress associated with internalizing symptoms acts as a motivator for treatment and enhances treatment adherence in a quest for symptom relief (e.g., Blood & Cornwall, 1994; Pagnin et al., 2005), while another theory is that depressive symptoms may reflect acknowledgment of a problem and the desire to change (Tapert et al., 2003). Further research needs to be conducted to test these different theories and better understand the relationship between depression and SUD outcomes following CBT treatment.
A number of factors may have contributed to the discrepancies in results between the current study and prior research documenting detrimental effects of comorbid conditions on SUD treatment outcomes. First, differences might be due to the length of treatment or follow-up. The current study utilized a brief outpatient treatment as opposed to previous studies that used either longer outpatient treatments (e.g., Rowe et al., 2004) or more intensive inpatient treatments (e.g., Tomlinson et al., 2004; Winters et al., 2008). Whereas other studies have predominantly had follow-up periods of over six months, this study focused on acute treatment outcome at three months and six months. Hence, the results may indicate that comorbidity is less influential with brief treatments or in early follow-up.
Second, the differences between past research and the current study may be related to sample characteristics or diagnostic procedures. For instance, some prior studies of comorbid youth have been comprised of mostly minority youth, from large cities, and/or juvenile court referrals (e.g., Grella et al., 2001; Rowe et al., 2004; Shane et al., 2003). In contrast, the current study included primarily Caucasian youth from a predominantly suburban area. Furthermore, the current study used continuous measures of comorbidity, whereas most prior studies have used categorical indicators (Grella et al., 2001; Rowe et al., 2004; Shane et al, 2003). Finally, the time frame for depression diagnoses in the current study was one year, suggesting that not all adolescents with depression were necessarily in a current episode at treatment initiation.
With regard to other findings, it was noteworthy that higher SES predicted fewer substance problems and lower substance frequency at three months. These results may reflect the advantages that high SES provides. Tomlinson and colleagues (2004) note that adolescents with SUDs may have increased access to substances through greater involvement with delinquent substance-abusing peers, which in turn, may be associated with poorer treatment outcomes. Although speculative, one potential explanation for the predictive effects of SES is that youth with higher SES may have more opportunities to remove themselves from these negative peer associations. The final session of MET/CBT-5 teaches adolescents to change the people they choose to be around and the places they choose to go, based on the assumption that these were previously opportunities for substance-use and may be triggers for relapse (Beck et al., 1993). While higher SES youth may be able to change the people and places they frequent, lower SES youth may be forced to remain in neighborhoods where they may often encounter drugs and alcohol.
Consistent with the present findings, two large multi-site clinical trials investigating psychopathology among children and adolescents found SES differences in who benefited the most from behavioral treatments. Results from a moderator analysis conducted as part of the Treatment for Adolescents with Depression Study (TADS; Curry et al., 2006) found that for youth from families with high annual income, cognitive behavioral therapy (CBT) was as effective as a combined treatment of CBT and medication. Higher SES youth were the only group for whom CBT was not inferior to the combination treatment. Similarly, the Multimodal Treatment Study of Children with Attention-Deficit/Hyperactivity Disorder (MTA) found that youth from more educated households benefited more from a combination of behavioral treatment and medication than from either medication or behavioral treatment alone (Rieppi et al., 2002). Alternately, youth with ADHD from less educated households benefited equally from medication and the combined treatment, both of which were superior to the behavioral treatment alone. The authors propose that more educated families "may have benefited more [from the combined treatment] because they could more easily integrate and use the added behavioral ADHD treatments" (Rieppi et al., 2002; p. 275). Consistent with these two clinical trials, the current findings suggest that youth from more advantaged families may experience more acute benefit from cognitive behavioral treatments than youth from lower SES families.
Study results should be interpreted within the context of several limitations. First, the scales used to assess comorbid psychopathology assessed symptoms experienced over the past year. It is possible that youth with high levels of past year symptoms were not as symptomatic at baseline. Additionally, substance use and comorbidity measures were all self-report, which may have been subject to self-report bias. Second, follow-up comorbidity scores were not obtained. Future research should investigate whether comorbid symptomatology decreases with SUD treatment, specifically for depression and conduct disorder. A final limitation of the current study is the small sample size, which may have reduced the power needed to obtain significant results.
Findings from the current study suggest that CBT protocols for substance abuse and depression might be enhanced in two ways. First, the results highlight the utility of finding components and approaches that can address both depression and substance use within one treatment. Second, the findings suggest that SES can negatively influence CBT treatment outcomes. Although the small sample and lack of a control condition preclude clinical inferences, the current study suggests that CBT programs should consider means to increase access to care and reduce societal barriers to receiving treatment. Additionally, at intake to treatment, it may be useful for CBT treatment providers to consider how SES may affect client presenting problems and ways of coping.
Future studies should investigate how specific comorbidities influence CBT substance abuse treatment outcomes among adolescents with larger and more diverse populations to test the generalizability of the results. Given the complex findings in the current study, more needs to be known regarding when and how comorbidity matters. The potentially protective effects of depression on SUD treatment outcome should also be further explored. Identifying the individual and interactive effects of specific mental health diagnoses on SUD treatment outcome can help to inform treatment development and delivery.
Acknowledgments
This research was supported by Grant TI-15-447 from the Substance Abuse and Mental Health Services Administration awarded to John F. Curry, Ph.D.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edition. Washington, DC: Author; 2000. text revision (DSM-IV-TR) [Google Scholar]
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. The American Journal of Psychiatry. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric Comorbidity. Journal of Consulting and Clinical Psychology. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Beck AT, Wright FD, Newman CF, Liese BS. Cognitive Therapy of Substance Abuse. New York: The Guilford Press; 1993. [PubMed] [Google Scholar]
- Becker SJ, Curry JF. Interactive effect of substance abuse and depression on adolescent social competence. Journal of Clinical Child and Adolescent Psychology. 2007;36:469–475. doi: 10.1080/15374410701448638. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: A quality of evidence review. Journal of Consulting and Clinical Psychology. 2008;76:531–543. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF, Yang C. Longitudinal association between frequency of substance use and quality of life among adolescents receiving a brief outpatient intervention. Psychology of Addictive Behaviors. 2009;23:482–490. doi: 10.1037/a0016579. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. Journal of Substance Abuse Treatment. 2011;41:294–304. doi: 10.1016/j.jsat.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Livas Stein G, Curry JF, Hersh J. Ethnic differences among substance-abusing adolescents in a treatment dissemination project. Journal of Substance Abuse Treatment. 2012;42:328–336. doi: 10.1016/j.jsat.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Blood L, Cornwall A. Pretreatment Variables That Predict Completion of an Adolescent Substance Abuse Treatment Program. Journal of Nervous & Mental Disease. 1994;182:14–29. doi: 10.1097/00005053-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol. 1996;57:314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analyses for the behavioral sciences. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Cornelius JR, Maisto SA, Martin CS, Bukstein OG, Salloum IM, Daley DC, et al. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addictive Behaviors. 2004;29(5):1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- Couwenbergh C, Brink W, Zwart K, Vreugdenhill C, van Wijngaarden-Cremers P, van der Gaag RJ. Comorbid psychopathology in adolescents and young adults treated for substance use disorders. European Child & Adolescent Psychiatry. 2006;15:319–328. doi: 10.1007/s00787-006-0535-6. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L. Psychosocial treatment for drug abuse. Arch Gen Psychiatry. 1996;53:749–756. doi: 10.1001/archpsyc.1996.01830080103015. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, MacDonald M, Young SE, Zerbe GO. Substance-dependent, conduct-disordered adolescent males: severity of diagnosis predicts 2-year outcome. Drug and Alcohol Dependence. 1998;49(3):225–237. doi: 10.1016/s0376-8716(98)00016-7. [DOI] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent. 2006;45:1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Curry J, Silva S, Rohde P, Ginsburg G, Kennard B, Kratochvil C, March J. Onset of alcohol or substance use disorders following treatment for adolescent depression. Journal of Consulting and Clinical Psychology, No Pagination Specified. 2012 doi: 10.1037/a0026929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry JF, Wells KC, Lochman JE, Craighead WE, Nagy PD. Cognitive-behavioral intervention for depressed, substance-abusing adolescents: Development and pilot testing. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(6):656–665. doi: 10.1097/01.CHI.0000046861.56865.6C. [DOI] [PubMed] [Google Scholar]
- Deas D, Thomas S. Comorbid psychiatric factors contributing to adolescent alcohol and other drug use. Alcohol Research & Health. 2002;26(2):116–121. [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker JI, Hodgkins D. Global appraisal of individual needs (GAIN): Trainer’s training manual and resources. Bloomington, IL: Chestnut Health Systems; 2003. [Google Scholar]
- Dennis ML, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Deskovitz M, Key DE, Hill EM, Franklin JT. A Long-Term Family-Oriented Treatment for Adolescents with Substance-Related Disorders: An Outcome Study. Child and Adolescent Social Work Journal. 2004;21:265–284. [Google Scholar]
- Dobkin PL, Chabot L, Maliantovich K, Craig W. Predictors of outcome in drug treatment of adolescent inpatients. Psychological Reports. 1998;83:175–186. doi: 10.2466/pr0.1998.83.1.175. [DOI] [PubMed] [Google Scholar]
- Galaif ER, Hser YI, Grella CE, Joshi V. Prospective risk factors and treatment outcomes among adolescents in DATOS-A. Journal of Adolescent Research. 2001;16(6):661–678. [Google Scholar]
- Garber J, Weiss B, Shanley N. Cognitions, depressive symptoms, and development in adolescents. Journal of Abnormal Psychology. 1993;102:47–57. doi: 10.1037//0021-843x.102.1.47. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Tejera G, Canino G, Ramirez R, Chavez L, Shrout P, Bird H, et al. Examining minor and major depression in adolescents. Journal of Child Psychology and Psychiatry. 2005;46:888–899. doi: 10.1111/j.1469-7610.2005.00370.x. [DOI] [PubMed] [Google Scholar]
- Greenbaum PE, Prange ME, Friedman RM, Silver SE. Substance abuse prevalence and comorbidity with other psychiatric disorders among adolescents with severe emotional disturbances. J Am Acad Child Adolesc Psychiatry. 1991;30:575–583. doi: 10.1097/00004583-199107000-00008. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, et al. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser Y, Joshi V, Rounds-Bryant J. Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. Journal of Nervous and Mental Disease. 2001;189:384–392. doi: 10.1097/00005053-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. A.B Four factor index of social status. New Haven: Yale University; 1975. Unpublished manuscript. [Google Scholar]
- Hser YI, Grella CE, Collins C, Teruya C. Drug-use initiation and conduct disorder among adolescents in drug treatment. Journal of Adolescence. 2003;26(3):331–345. doi: 10.1016/s0140-1971(03)00012-5. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Nelson T, Steidtmann DK, Bistricky SL. Comparative Data on Child and Adolescent Cognitive Measures Associated With Depression. Journal of Consulting and Clinical Psychology. 2007;75:390–403. doi: 10.1037/0022-006X.75.3.390. [DOI] [PubMed] [Google Scholar]
- Judd L, Paulus M, Wells K, Rapaport M. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. American Journal of Psychiatry. 1996;153:1411–1417. doi: 10.1176/ajp.153.11.1411. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapies for adolescent substance abusers - A pilot study. Journal of Nervous and Mental Disease. 1998;186(11):684–690. doi: 10.1097/00005053-199811000-00004. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: A posttreatment natural history study. Journal of Studies on Alcohol. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Powell NR, Whidby JM, FitzGerald DP. Aggression in children. In: Kendall PC, editor. Child and adolescent therapy: Cognitive-behavioral procedures. 4th Edition. New York: The Guilford Press; 2012. pp. 27–60. [Google Scholar]
- Pagnin D, Queiroz V, de, Saggese EG. Predictors of attrition from day treatment of adolescents with substance-related disorders. Addictive Behaviors. 2005;30(5):1065–1069. doi: 10.1016/j.addbeh.2004.09.013. [DOI] [PubMed] [Google Scholar]
- Powell BJ, Penick EC, Othmer E, Bingham SF, Rice AS. Prevalence of additional psychiatric syndromes among male alcoholics. Journal of Clinical Psychiatry. 1982;43:404–407. [PubMed] [Google Scholar]
- Rapaport M, Judd L. Minor depressive disorder and subsyndromal depressive symptoms: Functional impairment and response to treatment. Journal of Affective Disorders. 1998;48:227–232. doi: 10.1016/s0165-0327(97)00196-1. [DOI] [PubMed] [Google Scholar]
- Rieppi R, Greenhill LL, Ford RE, Chuang S, Wu M, Davies M, et al. Socioeconomic status as a moderator of ADHD treatment outcomes. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:269–277. doi: 10.1097/00004583-200203000-00006. [DOI] [PubMed] [Google Scholar]
- Rowe CL, Liddle HA, Greenbaum PE, Henderson CE. Impact of comorbidity on treatment of adolescent drug abusers. Journal of Substance Abuse Treatment. 2004;26:129–140. doi: 10.1016/S0740-5472(03)00166-1. [DOI] [PubMed] [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy (MET-CBT-5) for adolescent cannabis users. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. [Google Scholar]
- Shane PA, Jasiukaitis P, Green RS. Treatment outcomes among adolescents with substance abuse problems: The relationship between comorbidities and post-treatment substance involvement. Evaluation and Program Planning. 2003;26:39three–402. [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello J. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers MG, et al. Depressed mood, gender, and problem drinking in youth. Journal of Child & Adolescent Substance Abuse. 2003;12(4):55–68. [Google Scholar]
- Tomlinson KL, Brown SA, Abrantes A. Psychiatric comorbidity and substance use treatment outcomes of adolescents. Psychology of Addictive Behaviors. 2004;18:160–169. doi: 10.1037/0893-164X.18.2.160. [DOI] [PubMed] [Google Scholar]
- Vourakis C. Admission Variables as Predictors of Completion in an Adolescent Residential Drug Treatment Program. Journal of Child and Adolescent Psychiatric Nursing. 2005;18:161–170. doi: 10.1111/j.1744-6171.2005.00031.x. [DOI] [PubMed] [Google Scholar]
- Wagner BM, Cole RE, Schwartzman P. Comorbidity of symptoms among junior and senior high school suicide attempters. Suicide Life Threat Behav. 1996;26(3):300–307. [PubMed] [Google Scholar]
- Weinberg N, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- White AM, Jordan JD, Schroeder KM, Acheson SK, Georgi BD, Sauls G, et al. Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Substance Abuse. 2004;25:53–59. doi: 10.1300/J465v25n01_08. [DOI] [PubMed] [Google Scholar]
- Whitmore EA, Mikulich SK, Ehlers KM, Crowley TJ. One-year outcome of adolescent females referred for conduct disorder and substance abuse/dependence. Drug and Alcohol Dependence. 2000;59(2):131–141. doi: 10.1016/s0376-8716(99)00112-x. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD, Latimer WW, Stone A. Internalizing and externalizing behaviors and their association with the treatment of adolescents with substance use disorder. Journal of Substance Abuse Treatment. 2008;35:269–278. doi: 10.1016/j.jsat.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]