Abstract
Background
The aim of this study was to comprehensively examine clinical risk factors, including suicide intent and hopelessness, for suicide and risk of death from all causes after attempted suicide over a 12-year follow-up period.
Methods
A systematic sample of 224 patients from consecutive cases of attempted suicide referred to health care in four Finnish cities between 1 January and 31 July 1990 was interviewed.
Results
After 12 years of follow-up 22% of these patients had died, 8% by committing suicide. The only statistically significant risk factor for eventual suicide was high scores on Beck's Suicidal Intention Scale. Male gender, older age, physical illness or disability and high scores on Beck's Suicidal Intention Scale predicted death overall.
Conclusions
Following attempted suicide, high intention to kill oneself is a significant risk factor for both death from all causes and suicide.
Keywords: attempted suicide, suicide, outcome, follow-up studies, risk factors, suicide intent, hopelessness
Background
Among the factors found to predict suicide, a previous suicide attempt is one of the strongest [1]. Suicidal intent, defined as the seriousness or intensity of the patient's wish to terminate his or her life [2], has been found to predict completed suicide in most [3-7], although not all studies [8]. Hopelessness, defined as a state of negative expectations [9], appears to be another predictor of suicide [10-15]. Other factors found to associate with increased suicide risk after attempted suicide include male gender, advancing age, psychiatric disorder, previous psychiatric treatment, long-term use of hypnotics, poor physical health, living alone, and "wish to die" as a motive for the index attempt [16-18]. While both level of suicidal intent and hopelessness are likely to be significant predictors of completed suicide after a suicide attempt, their relative importance has remained unknown since few prospective studies have measured both.
The aim of the present study was to comprehensively examine clinical risk factors for suicide and other causes of death after attempted suicide, including suicidal intent and hopelessness.
Methods
Subjects
A systematic sample of 224 subjects aged 15 years or more from consecutive cases of attempted suicide admitted to health care in four cities in Finland from January 1st to July 31st 1990 was comprehensively interviewed after obtaining written informed consent [19]. The sample of the present study forms part of a database for an epidemiological monitoring project on attempted suicide in Finland. The project was carried out in collaboration with the WHO/EURO Multicentre Study on Parasuicide [20-22], which investigates factors predicting future suicidal behaviour. The repetition-prediction part of the study in Finland was carried out in four cities: Helsinki (Southern region), Jyväskylä (Central), Rovaniemi (Northern) and Seinäjoki (Western).
As parasuicide patients in Helsinki are treated in general hospitals only, the data were gathered at all five of the city's general hospitals (three university clinics and two municipal hospitals). In other regions some mild cases are treated in local health centres. In Jyväskylä, data collection was carried out at one general hospital and nine health centres, in Seinäjoki at one general hospital and six health centres, and in Rovaniemi at one general hospital and two health centres treating suicide attempters [19]. In the four research areas a total of 600 patients were asked to participate, of whom 224 (37%) consented and completed the initial interview. The numbers of attempted suicide patients participating in the study were 114 (53 men and 61 women) in Helsinki, 33 (11 men and 22 women) in Jyväskylä, 30 (12 men and 18 women) in Rovaniemi and 47 (23 men and 24 women) in Seinäjoki. The details of the methodology have been reported earlier [19].
The WHO definition of parasuicide [23] was used, and attempted suicide and parasuicide are used as synonyms in this report. All 224 suicide attempters were interviewed according to a structured schedule, the European Parasuicide Study Interview Schedule (EPSIS I) [24].
Interview schedule
The interview form [24] contained 424 items concerning the patient's everyday life, state of health, use of alcohol and other drugs, previous suicidality, treatment in the health care system including psychiatric consultation, and life events. Beck's Suicidal Intention Scale (SIS) [2], Beck's Hopelessness Scale (HS) [9], the State Trait Anger Scale (STAS) [25], the Self Esteem Scale (SES) [26], Motives for present parasuicide (ML) [27,28] and Beck's Depression Inventory (BDI) [29] were all used.
Long-standing physical illness or disability was defined as a physical illness or disability that had troubled a patient for at least one year [24]. Mental health symptoms spanning the previous 12 months was used to define a patient's experience of prolonged periods (at least one year) of troubles within herself/himself that had hindered functioning [24]. Mental health symptoms during the past three months were categorised as on the whole poor or fair, according to the patient's evaluation of her/his mental health [24]. The assessment of lethality (somatic severity) of the suicide attempt was based on the patients' physical condition in the emergency room, the amount and type of drugs taken, and on all available information from the medical records, as in previous Finnish studies [7,18]. Here, three defined grades (mild, moderate and serious) were used.
Outcome
The outcome of suicide attempters, using mortality by suicide and other causes of death as the outcome criteria, was examined for a follow-up period of 12 years (1.1.1990–31.12.2002). The index suicide attempt was defined as first admission to the emergency unit because of suicide attempt during the study period 1.1.1990–31.7.1990. Occurrence of death data were obtained from Statistics Finland [30]. The definition of suicide was based on Finnish law for determining causes of death [31]. In every case of violent, sudden or unexpected death in Finland, the cause of death is assessed by police and medicolegal investigations involving autopsy and forensic examination.
The subjects of this study were 224 suicide attempters treated for an index suicide attempt in health care in Finland (Helsinki, Jyväskylä, Rovaniemi and Seinäjoki) during a seven-month study period in 1990.
Statistical analysis
The two-tailed chi-square test with Yates' correction, Fisher's exact test and the two-tailed t-test were employed in basic comparisons. For the survival analyses Kaplan-Meier and Cox regression models were used.
We analysed mortality and suicide mortality in the study population using Cox proportional hazards regression models with gender, age, number of previous suicide attempts, lethality of index attempt, Beck's Depression Inventory scores, Beck's Hopelessness Scale scores, Beck's Suicidal Intention Scale scores, physical illness or disability and use of alcohol at the time of the index attempt as covariates. The backward stepwise method (Wald) was used.
Results
By the end of the 12-year follow-up 22% (50 out of 224) had died: 31% of male (n = 31) and 15% of female (n = 19) suicide attempters (Fisher's exact test p = 0.006) (Table 1). Seventeen (8%) of the patients had committed suicide: 9 (9%) of the males and 8 (6%) of the females. Suicide accounted for 34% of all deaths. There were no statistically significant differences in suicide rates or overall mortality between the four Finnish centres. 41% (N = 7) of the subjects completing suicide switched the suicide method to another. 21 attempters (9%; 11 males and 10 females) had died by natural causes, 11 (5%; 10 males and 1 female) had died by accidents and one male was murdered.
Table 1.
Clinical and sociodemographic characteristics of 224 suicide attempters who committed suicide or not, died from all causes, or survived during the 12-year follow-up.
| Variable | Suicide (N = 17) | Not suicide (N = 207) | Death, all causes (N = 50) | Survived (N = 174) |
| Gender a (%) | ||||
| Male | 53 | 3 | 62 | 39 |
| Mean age (years) b | 36.6 ± 8.1 | 36.2 ± 12.3 | 41.9 ± 14.3 | 34.5 ± 10.8 |
| Marital status c (%) | ||||
| Single | 53 | 47 | 40 | 50 |
| Married | 35 | 24 | 28 | 24 |
| Widowed | 6 | 3 | 12 | 1 |
| Separated | 6 | 25 | 20 | 25 |
| Had children (%) | 59 | 55 | 64 | 53 |
| Physical illness or disability d (%) | 53 | 42 | 62 | 37 |
| Mental health symptoms (%) | ||||
| Last year | 65 | 72 | 72 | 71 |
| Last three months | 94 | 86 | 92 | 85 |
| Visited general practitioner | ||||
| during the last year (%) | 79 | 86 | 91 | 84 |
| during the last week (%) | 6 | 3 | 6 | 13 |
| Lifetime in-patient psychiatric treatment (%) | 43 | 51 | 54 | 49 |
| Method of index attempt (%) | ||||
| Violent | 0 | 9 | 6 | 9 |
| Lethality of index attempt (%) | ||||
| Mild | 40 | 48 | 56 | 46 |
| Intermediate | 20 | 31 | 19 | 33 |
| Severe | 40 | 21 | 25 | 21 |
| Used alcohol before the attempt (%) | 71 | 65 | 66 | 65 |
| Previous parasuicide (%) | 47 | 51 | 50 | 48 |
| Psychiatric consultation (%) | 47 | 47 | 44 | 48 |
| Beck Depression Inventory | 21.1 ± 12.4 | 20.8 ± 10.6 | 22.5 ± 11.7 | 20.3 ± 10.4 |
| Beck Hopelessness Scale | 9.3 ± 5.7 | 9.0 ± 5.1 | 9.0 ± 5.6 | 9.0 ± 5.0 |
| Beck Suicidal Intention Scale e | 14.5 ± 7.7 | 10.7 ± 6.5 | 12.2 ± 7.1 | 10.7 ± 6.5 |
| Self Esteem Scale | 21.5 ± 4.0 | 22.5 ± 2.5 | 21.8 ± 3.4 | 22.6 ± 2.4 |
| State Trait Anger Scale | 36.2 ± 7.2 | 35.2 ± 9.0 | 35.3 ± 8.5 | 35.2 ± 9.0 |
| Recommended aftercare f (%) | ||||
| Nothing | 24 | 23 | 22 | 23 |
| Outpatient | 76 | 56 | 60 | 57 |
| Inpatient | - | 21 | 18 | 20 |
| Suicide method (%) | ||||
| Drug overdose | 59 | |||
| Hanging | 18 | |||
| Shooting | 6 | |||
| Jumping from high place | 6 | |||
| Jumping under vehicle | 12 |
a Death (all causes) vs. survived Fisher's exact test, p = 0.006 b Death (all causes) vs. survived F = 3.9, df = 222, p < 0.001 c Death (all causes) vs. survived: widowed vs. other χ2 = 10.3, df = 1, p = 0.001 d Death (all causes) vs. survived Fisher's exact test, p = 0.002 e Suicide vs. not suicide F = 2.3, df = 221, p = 0.02 f Suicide vs. not suicide Likelihood ratio χ2 = 7.8, df = 2, p = 0.02
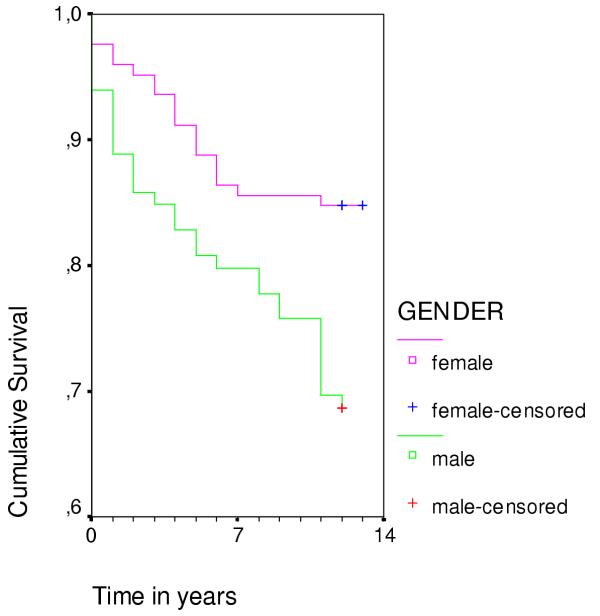
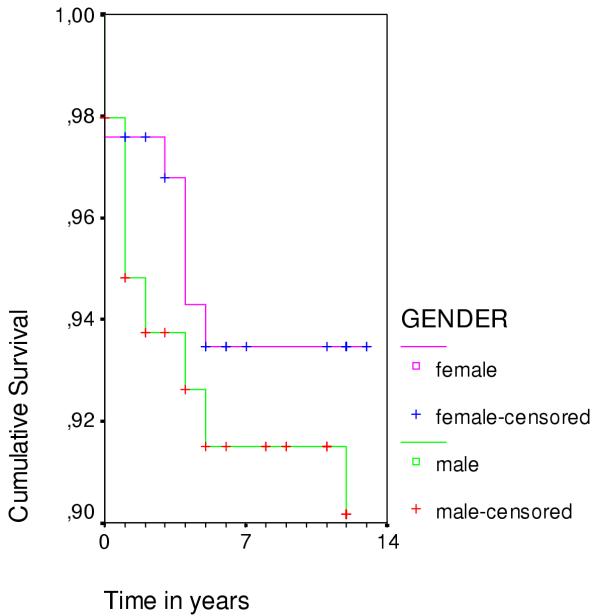
The cumulative survival curve plots for the 12-year follow-up appear in Figures 1 and 2 for each gender. The overall risk of death among males was significantly higher (log rank statistics 8.06, df = 1, p = 0.0045) (Figure 1). There was no statistically significant gender difference in suicide risk during the follow-up period (log rank statistics 0.75, df = 1, p = 0.4) (Figure 2).
Figure 1.
Cumulative proportion of patients surviving after index suicide attempt. Males have significantly less favourable prognosis than females. Censored cases are cases for which the event is not recorded = patients surviving. Kaplan-Meier survival curves: log rank statistics 8.06, df = 1, p = 0.0045.
Figure 2.
Cumulative proportion of patients not committing suicide after the index suicide attempt. No significant difference between males and females. Censored cases are cases for which the event is not recorded = patients not committing suicide. Kaplan-Meier survival curves: log rank statistics 0.75, df = 1, p = 0.4.
Suicide attempters who eventually committed suicide had scored higher on Beck's Suicidal Intention Scale (Table 1). Reasons and motives for the suicide attempt appear in Table 2. Problems with partner, having wanted to die, and having wanted to make things easier for others were more common among those who committed suicide. Physical illness or disability and problems with partner were more common among suicide attempters who died (all causes) during the follow-up. High scores on Beck's Suicidal Intention Scale predicted suicide (Table 3). Male gender, older age, physical illness or disability and high scores on Beck's Suicidal Intention Scale predicted death (all causes) (Table 3).
Table 2.
Reasons and motives for the index suicide attempt.
| Variable | Suicide (N = 17) | Not suicide (N = 207) | Death, all causes (N = 50) | Survived (N = 174) |
| Reasons why patient took pills or injured himself/herself (%) | ||||
| Problems with partner a | 33 | 61 | 44 | 63 |
| Problems with parents | 38 | 34 | 38 | 34 |
| Problems with children | 25 | 17 | 15 | 18 |
| Problems with loneliness | 75 | 72 | 79 | 71 |
| Problems in making or maintaining friendships and social relations | 50 | 46 | 49 | 46 |
| Rejection by lover | 27 | 39 | 44 | 37 |
| Physical illness or disability b | 31 | 20 | 36 | 17 |
| Mental illness and psychiatric symptoms | 50 | 69 | 64 | 68 |
| Unemployment | 38 | 21 | 30 | 21 |
| Addiction | 56 | 44 | 58 | 42 |
| Motives for the suicide attempt (%) | ||||
| My thoughts were so unbearable | 77 | 74 | 70 | 76 |
| I wanted to show someone how much I loved him/her | 31 | 36 | 36 | 36 |
| I lost control over myself | 62 | 69 | 65 | 70 |
| The situation was so unbearable | 79 | 76 | 77 | 77 |
| I wanted to get away from an unacceptable situation | 62 | 59 | 60 | 59 |
| I wanted others to know how desperate I felt | 39 | 54 | 42 | 56 |
| I wanted to die c | 93 | 62 | 67 | 64 |
| I wanted to get help from someone | 33 | 59 | 49 | 60 |
| I wanted to know if someone really cared about me | 29 | 42 | 33 | 44 |
| I wanted others to pay for the way they treated me | 29 | 27 | 30 | 26 |
| I wanted to make someone feel guilty | 36 | 27 | 30 | 26 |
| I wanted to persuade someone to change his/her mind | 21 | 26 | 14 | 29 |
| I wanted to make things easier for others d | 79 | 39 | 46 | 41 |
| I wanted to sleep for a while | 54 | 44 | 40 | 46 |
a Suicide vs. not suicide Fisher's exact test, p = 0.05; Death (all causes) vs. survived Fisher's exact test, p = 0.05 b Death (all causes) vs. survived Fisher's exact test, p = 0.007 c Suicide vs. not suicide Fisher's exact test, p = 0.02 d Suicide vs. not suicide Fisher's exact test, p = 0.005
Table 3.
Risk factors for suicide and death (all causes) (Survival analysis: Cox regression models)
| Suicide | Death, all causes | |||||
| Risk factors | OR | 95% Cl | p | OR | 95% Cl | p |
| Male gender | 3.04 | 1.56–5.94 | 0.001 | |||
| Age | 1.04 | 1.02–1.07 | 0.002 | |||
| Beck Suicidal Intention Scale | 1.18 | 1.06–1.33 | 0.004 | 1.06 | 1.01–1.11 | 0.03 |
| Physical illness or disability | 3.08 | 0.87–10.97 | 0.08 | 2.22 | 1.10–4.49 | 0.03 |
Discussion
The findings of the present study confirm previous research suggesting that a high level of suicidal intent is a significant predictor of both subsequent death and suicide following a suicide attempt. Moreover, high suicidal intent scores at index attempt seem to be a more powerful predictor of eventual suicide than previous attempts or hopelessness.
To our knowledge, this is the first follow-up study of attempted suicide in Finland to include regions beyond the capital area, and is thus more representative of the country as a whole than earlier studies. As no differences in mortality between the four regions emerged, our findings support the generalizability of our previous findings from Helsinki-based cohorts to other parts of the country. The extensive structured interview and case report method used in the present study is comprehensive and provides a broad picture of suicide attempters and their outcomes. Most previous studies have been based on hospital records only or have included only attempters referred for psychiatric consultation or attempts made by self-poisoning.
The disadvantage of an interview study is that some patients refuse to participate. In this study no significant differences were found in sociodemographic variables between the interviewees and the entire suicide attempt population [19]. The only statistically significant difference was that the male interviewees were more likely to have received psychiatric consultation than the other men in the entire parasuicide population [19]. Thus we cannot exclude the possibility of overrepresentation of more severe cases in our initial parasuicide sample. However, our sample appears to be representative of those suicide attempters who are sufficiently motivated to stay in health care. The main limitation of the present study is that we were unable to use a structured diagnostic interview for all patients and thus could not include the DSM-diagnoses as possible risk factors. Previous studies have found that the vast majority of suicide attempters suffer from mental disorders [32-36]. However, there appears to be only one previous study with 30 months of follow-up using structured diagnostic information [37].
The overall mortality of suicide attempters was remarkably high, in accordance with previous studies [17,38-41]: a fifth of the cohort died during the 12-year follow-up. The risk for suicide (8%) in the present study is consistent with the findings of a recent review of fatal repetition of self-harm [42]. Most previous studies have found significant gender differences in suicide and overall mortality after attempted suicide [17,18,38,39,43-45]. Somewhat surprisingly, we did not detect a statistically significant gender difference in suicide mortality in the present study. We cannot, however, exclude the possibility that male suicide attempters who were more motivated to stay in health care and to participate in the interviews and psychiatric consultation were selected. It has been found that patients who discharge themselves before completing initial management have a considerably increased rate of repetition [46]. Furthermore, males with higher intent may have used more lethal methods and died rather than survived at an index attempt. Although the cohort was collected from several cities, the sample size remained moderate, and due to limited statistical power, we cannot rule out the possibility of gender differences in suicide mortality. However, male gender was a risk factor for death by all causes during the follow-up. These latter results accord with Nordentoft et al. [16], who found male gender to be a predictive factor for death by all causes, but not for suicide during a ten-year follow-up period in Denmark.
Previously, hopelessness has been found predictive of actual suicide, both in psychiatric outpatients [13] and in hospitalized suicide ideators [12]. However, these studies measured only hopelessness and depression, not level of suicidal intent. Furthermore, in a sample of hospitalized suicide attempters a diagnosis of alcoholism and the SIS Precautions subscale predicted eventual suicide [47], not hopelessness. In addition, Nimeus et al. [48] found in a similar sample of suicide attempters with different diagnoses that the Hopelessness Scale was an unsatisfactory instrument for predicting future suicide; hopelessness was better associated with mood disorders. On the other hand, in patients with affective disorders [11,15] degree of hopelessness appeared to be an important factor predicting eventual suicide, although its significance may depend on the history of drug and alcohol abuse [49].
Very few follow-up studies after attempted suicide have used a comprehensive interview including known scales for assessing the severity of the attempt. Most follow-up studies have had small clinical samples or been large epidemiological studies without structured interview information. Thus, strongly significant risk factors for subsequent suicide, particularly high suicidal intent, may have remained undetected. Suicide attempters with high intent is a risk group of patients with high suicide and overall mortality, therefore various possibilities of surveillance may be considered. However, as the suicide risk remains high for decades, a more feasible approach might be focusing clinical attention to periods of likely elevated risk, such as episodes of depression.
Conclusions
In conclusion, the level of suicidal intent appears to be the most powerful predictor of eventual suicide after attempted suicide. As most previous parasuicide follow-up studies have not reliably measured level of suicide intent, its important role as a predictor of eventual suicide has remained largely unrecognised.
Competing interests
None declared.
Authors' contributions
JL conceived and designed the collection of the initial study sample. AO participated in conceiving and designing the collection of the initial study sample and coordinated the study. KS analysed the data of the present study and wrote the report. EI participated in writing the paper. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
We are grateful to the interviewers: V. Granström, S. Heinonen, U. Mustonen, L. Rantanen, M-L Rasanen I. Sovijärvi and T. Viirre in Helsinki; J. Happonen, A Hytönen, E-L Männistö, E. Roivainen and J. Salkosalo in Jyväskylä; S Nikkanen and I Paasivirta in Rovaniemi; H Takala in Seinäjoki.
Contributor Information
Kirsi Suominen, Email: kirsi.suominen@ktl.fi.
Erkki Isometsä, Email: erkki.isometsa@ktl.fi.
Aini Ostamo, Email: aini.ostamo@ktl.fi.
Jouko Lönnqvist, Email: jouko.lonnqvist@ktl.fi.
References
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Beck AT, Schuyler D, Herman I. Development of Suicidal Intent Scales. In: Beck AT, Resnick HLP, Lettieri DJ, editor. In The Prediction of Suicide. Bowie, Maryland: Charles Press; 1974. pp. 45–56. [Google Scholar]
- Pierce DW. The predictive validation of a suicide intent scale: a five year follow-up. Br J Psychiatry. 1981;139:391–396. doi: 10.1192/bjp.139.5.391. [DOI] [PubMed] [Google Scholar]
- Pallis DJ, Gibbons JS, Pierce DW. Estimating suicide risk among attempted suicides II. Efficiency of predictive scales after the attempt. Br J Psychiatry. 1984;144:139–148. doi: 10.1192/bjp.144.2.139. [DOI] [PubMed] [Google Scholar]
- Lönnqvist J, Tolppanen E-M. Outcome of attempted suicide. In: Pichot P, Berner P, Wolf R, Thau K, editor. In Psychiatry – the state of the art. New York: Plenum Press; 1985. pp. 889–894. [Google Scholar]
- Lönnqvist J, Ostamo A. Suicide following the first suicide attempt. A five-year follow-up using a survival analysis. Psychiatr Fenn. 1991;22:171–179. [Google Scholar]
- Suokas J, Lönnqvist J. Outcome of attempted suicide and psychiatric consultation: risk factors and suicide mortality during a five-year follow-up. Acta Psychiatr Scand. 1991;84:545–549. doi: 10.1111/j.1600-0447.1991.tb03191.x. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Suicidal people: One population or two? In: Mann JJ, Stanley M, editor. In Psychobiology of Suicidal Behavior Ann NY Acad Sci. Vol. 487. 1986. pp. 16–33. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W. Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry. 1987;144:35–40. doi: 10.1176/ajp.144.1.35. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. J Consult Clin Psychol. 1989;57:309–310. doi: 10.1037//0022-006X.57.2.309. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry. 1990;147:190–195. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Weishaar ME, Beck AT. Hopelessness and suicide. Int Review Psychiatry. 1992;4:177–184. [Google Scholar]
- Keller F, Wolfersdorf M. Hopelessness and the tendency to commit suicide in the course of depressive disorders. Crisis. 1993;14:173–177. [PubMed] [Google Scholar]
- Nordentoft M, Breum L, Munck LK, Nordestgaard AG, Hunding A, Bjaeldager PAL. High mortality by natural and unnatural causes: a 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. BMJ. 1993;306:1637–1641. doi: 10.1136/bmj.306.6893.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Fagg J. Suicide, and other causes of death, following attempted suicide. Br J Psychiatry. 1988;152:359–366. doi: 10.1192/bjp.152.3.359. [DOI] [PubMed] [Google Scholar]
- Suokas J, Suominen K, Isometsä E, Ostamo A, Lönnqvist J. Long-term risk factors for suicide mortality after attempted suicide – findings of a 14-year follow-up study. Acta Psychiatr Scand. 2001;104:117–121. doi: 10.1034/j.1600-0447.2001.00243.x. [DOI] [PubMed] [Google Scholar]
- Ostamo A, Rasanen L, Valjakka S, Lönnqvist J. WHO/EURO Multicentre Study on Parasuicide: The repetition-prediction study in Finland Materials and Methods. Publications of the National Public Health Institute B 18/1995. Helsinki: Yliopistopaino; 1995. [Google Scholar]
- Bille-Brahe U, Kerkhof A, De Leo D, Schmidtke A, Crepet P, Lönnqvist J, Michel K, Salander-Renberg E, Stiles TC, Wasserman D, Egebo H. A repetition-prediction study on European parasuicide populations. Part II of the WHO/Euro Multicentre Study on Parasuicide in cooperation with the EC concerted action on attempted suicide. Crisis. 1996;17:22–31. doi: 10.1027/0227-5910.17.1.22. [DOI] [PubMed] [Google Scholar]
- Bille-Brahe U, Kerkhof A, De Leo D, Schmidtke A, Crepet P, Lönnqvist J, Michel K, Salander-Renberg E, Stiles TC, Wasserman D, Aagaard B, Egebo H, Jensen B. A repetition-prediction study of European parasuicide populations: a summary of the first report from Part II of the WHO/EURO Multicentre Study on Parasuicide in co-operation with the EC Concerted Action on Attempted Suicide. Acta Psychiatr Scand. 1997;95:81–86. doi: 10.1111/j.1600-0447.1997.tb00378.x. [DOI] [PubMed] [Google Scholar]
- Schmidtke A, Bille-Brahe U, De Leo D, Kerkhof A, Bjerke T, Crepet P, Haring C, Hawton K, Lönnqvist J, Michel K, Pommereau X, Querejeta I, Phillipe I, Salander-Renberg E, Temesvary B, Wasserman D, Fricke S, Weinacker B, Sampaio-Faria JG. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989–1992. Results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatr Scand. 1996;93:327–338. doi: 10.1111/j.1600-0447.1996.tb10656.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Working Group on Preventive Practices in Suicide and Attempted Suicide: Summary Report (ICP/PSF 017 (s) 6526 V) Copenhagen: WHO Regional Office for Europe; 1986. [Google Scholar]
- Kerkhof AJFM, Bernasco W, Bille-Brahe U, Platt S, Schmidtke A. European Parasuicide Study Interview Schedule (EPSIS I). Version 5.1. In: Bille-Brahe U, Bjerke T, Crepet P, De Leo D, Haring C, Hawton K, Kerkhof A, Lönnqvist J, Michel K, Philippe A, Pommereau X, Querejeta I, Salander-Renberg E, Schmidtke A, Temesvary B, Wasserman D, Sampaio Faria J, editor. In WHO/EURO Multicentre Study on Parasuicide Facts and figures. Copenhagen: World Health Organization Regional Office for Europe; 1993. pp. 53–118. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory Research edition. Odessa, Florida: Psychological Assessment Resources, Inc; 1988. [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- Bancroft JHJ, Skrimshire AM, Simkin S. The reasons people give for taking overdoses. Br J Psychiatry. 1976;128:538–548. doi: 10.1192/bjp.128.6.538. [DOI] [PubMed] [Google Scholar]
- Bancroft JHJ, Hawton K, Simkin S, Kingston B, Cumming C, Whitwell D. The reasons people give for taking overdoses: a further inquiry. Br J Modern Psychology. 1979;52:353–365. doi: 10.1111/j.2044-8341.1979.tb02536.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Statistics Finland Causes of death 2002 Official Statistics of Finland, Health 2003: 2 Helsinki. 2003.
- Suomen säädöskokoelma Laki kuolemansyyn selvittämisestä (459/1973) Helsinki. 1997.
- Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry. 1996;153:1009–1014. doi: 10.1176/ajp.153.8.1009. [DOI] [PubMed] [Google Scholar]
- Suominen K, Henriksson M, Suokas J, Isometsä E, Ostamo A, Lönnqvist J. Mental disorders and comorbidity in attempted suicide. Acta Psychiatr Scand. 1996;94:234–240. doi: 10.1111/j.1600-0447.1996.tb09855.x. [DOI] [PubMed] [Google Scholar]
- Ferreira de Castro E, Cunha MA, Pimenta F, Costa I. Parasuicide and mental disorders. Acta Psychiatr Scand. 1998;97:25–31. doi: 10.1111/j.1600-0447.1998.tb09958.x. [DOI] [PubMed] [Google Scholar]
- Haw C, Hawton K, Houston K, Townsend E. Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry. 2001;178:48–54. doi: 10.1192/bjp.178.1.48. [DOI] [PubMed] [Google Scholar]
- Hawton K, Houston K, Haw C, Townsend E, Harris L. Comorbidity of axis I and and II disorders in patients who attempted suicide. Am J Psychiatry. 2003;160:1494–1500. doi: 10.1176/appi.ajp.160.8.1494. [DOI] [PubMed] [Google Scholar]
- Beautrais A, Joyce P, Mulder R. Unmet needs following serious suicide attempt: follow-up of 302 individuals for 30 months. In: Andrews, Henderson, editor. In Unmet Need in Psychiatry. Cambridge: Cambridge University Press; 1999. pp. 245–255. [Google Scholar]
- Nordström P, Samuelsson M, Åsberg M. Survival analysis of suicide risk after attempted suicide. Acta Psychiatr Scand. 1995;91:336–340. doi: 10.1111/j.1600-0447.1995.tb09791.x. [DOI] [PubMed] [Google Scholar]
- Rygnestad T. A prospective 5-year follow-up study of self-poisoned patients. Acta Psychiatr Scand. 1988;77:328–331. doi: 10.1111/j.1600-0447.1988.tb05129.x. [DOI] [PubMed] [Google Scholar]
- Ekeberg O, Ellingsen O, Jacobsen D. Suicide and other causes of death in a five-year follow-up of patients treated foe self-poisoning in Oslo. Acta Psychiatr Scand. 1991;83:432–437. doi: 10.1111/j.1600-0447.1991.tb05570.x. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Subsequent mortality in medically serious suicide attempts: a 5 year follow-up. Aust NZ Psychiatry. 2003;37:595–599. doi: 10.1046/j.1440-1614.2003.01236.x. [DOI] [PubMed] [Google Scholar]
- Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- Ostamo A, Lönnqvist J. Excess mortality of suicide attempters. Soc Psychiatry Psychiatr Epidemiol. 2001;36:29–35. doi: 10.1007/s001270050287. [DOI] [PubMed] [Google Scholar]
- Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537–542. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161:562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- Crawford MJ, Wessely S. Does initial management affect the rate of repetition of deliberate self harm? cohort study. BMJ. 1998;17:985. doi: 10.1136/bmj.317.7164.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Clinical predictors of eventual suicide: a 5- to 10-year prospective study of suicide attempters. J Affect Disord. 1989;17:203–209. doi: 10.1016/0165-0327(89)90001-3. [DOI] [PubMed] [Google Scholar]
- Nimeus A, Träskman-Bendz L, Alsen M. Hopelessness and suicidal behavior. J Affect Disord. 1997;42:137–144. doi: 10.1016/S0165-0327(96)01404-8. [DOI] [PubMed] [Google Scholar]
- Young MA, Fogg LF, Scheftner WA, Fawcett JA. Interactions of risk factors in predicting suicide. Am J Psychiatry. 1994;151:434–435. doi: 10.1176/ajp.151.3.434. [DOI] [PubMed] [Google Scholar]