Abstract
Vaccinations against the encephalitic alphaviruses (western, eastern, and Venezuelan equine encephalitis virus) are of significant interest to biological defense, public health, and agricultural communities alike. Although vaccines licensed for veterinary applications are used in the Western Hemisphere and attenuated or inactivated viruses have been used under Investigational New Drug status to protect at-risk personnel, there are currently no licensed vaccines for use in humans. Here, we will discuss the need for a trivalent vaccine that can protect humans against all three viruses, recent progress to such a vaccine, and a strategy to continue development to Food and Drug Administration licensure.
Introduction
Western (WEEV), eastern (EEEV), and Venezuelan (VEEV) equine encephalitis viruses represent three encephalitic alphaviruses for which safe and effective vaccines are needed. The requirement for these vaccines is, in large part, because of the severe disease caused by each of these viruses and their potential for use as biological weapons, which has resulted in their identification as Category B pathogens by the National Institute of Allergy and Infectious Diseases. Veterinary vaccination programs are currently used to protect equine populations in a number of countries in the Western Hemisphere, but human vaccines are limited to those vaccines that have achieved Investigational New Drug (IND) status and are used only to protect laboratory workers handling the viruses.1 Additional emphasis is needed from the science and technology base through advanced development to develop a Food and Drug Administration (FDA) licensed vaccine against all three of these pathogens.
The alphaviruses are members of the Togaviridae family of enveloped viruses. Alphaviruses use a single-stranded positive-sense RNA genome that encodes four non-structural and five structural proteins.2 These viruses are zoonotic pathogens that are maintained by mosquitoes and birds (WEEV and EEEV) or mammals (VEEV) in an enzootic lifecycle.3 Depending on climate conditions, mosquito species, and/or virus strain, they can also be transmitted to horses and humans by spillover of enzootic transmission or in an equine-amplified epizootic cycle, causing severe encephalitis in some cases.3
The geographic distribution and genomic diversity varies among these three viruses. WEEV can be isolated from birds and mosquitoes, mainly Culex tarsalis, across the western parts of the Americas from as far north as southern Canada and south to Argentina and Brazil.4,5 WEEV is a natural recombinant virus, containing envelope proteins from a Sindbis virus-like ancestor and non-structural and capsid proteins from an EEEV-like ancestor.6 Comparisons of isolates from North and South America reveal several antigenic subtypes and viral lineages,7,8 with variation in virulence in rodent models of disease.9–11
In North America, EEEV circulates between birds and Cx. melanura or other mosquitoes, but transmission to humans or horses can occur through Aedes, Coquillettidia, or Culex mosquito species that feed on both birds and mammals.3 Isolates can be described as North or South American antigenic varieties based on hemagglutinin inhibition assays, and four antigenic subtypes are delineated using neutralization assays.12 North American isolates are also noted as belonging to the Group I lineage and cause the majority of documented human illnesses. South American isolates in Groups IIA, IIB, and III are responsible for equine outbreaks in Central and South America, and recently, they were reclassified as the distinct species Madariaga virus.12,13 Until recently, it was thought that Central and South American EEEV strains were not a major concern in terms of human health. However, recent analyses of EEEV cases in a 2010 Panamanian outbreak may change that view and warrant additional investigation of these isolates.14
VEEV is one of several species in the VEE antigenic complex of alphaviruses. The lifecycle of most of these viruses involves enzootic transmission between rodents and mosquitoes, with outbreaks of epizootic disease being associated with the virus subtype and specific mosquito vectors. It is mainly restricted to Central and South America, and it is the most diverse of the three viruses, with six different subtypes (I–VI) that can be distinguished by serology. Furthermore, there are five different variants within subtype I (AB, C, D, E, and F). The epizootic variants, IAB and IC, are thought to evolve periodically from ID ancestors and cause the majority of epizootic disease in humans and horses.15,16 The ID, IE, and Mucambo virus (formerly VEEV IIIA) strains are also capable of causing febrile disease in humans, but these subtypes and the remaining subtypes are primarily associated with enzootic cycles.3 The diversity of VEEV subtypes creates an additional challenge for vaccine design, which will be discussed further below.
Although WEEV, EEEV, and VEEV are all capable of causing lethal encephalitis in humans and horses, the incidences and courses of disease do vary substantially among them. WEEV is somewhat rare, with fewer than 700 cases reported in the United States since the 1960s and no human infections detected since 1988.17 The rate of asymptomatic versus symptomatic WEEV infection varies widely with age, with children below the age of 1 year old being most susceptible to severe disease and the overall mortality rate being estimated at about 4%.1 Similarly, there are typically only a few cases of EEEV in the United States each year, although many more undetected asymptomatic infections may occur. However, encephalitic cases of EEEV infection have a much higher mortality rate, which is estimated at 30–70%, and survivors often experience severe permanent neurological sequelae.3,18 VEEV seems to have the greatest potential for epizootic disease, although mortality rates are typically only around 1% and mainly involve children.18 Flu-like symptoms are typical of an infection, with many patients recovering in 3–5 days. One of the largest VEEV outbreaks occurred in Columbia in 1995 and affected approximately 75,000 individuals. Among this population, 3,000 people developed neurological signs and symptoms, and the outbreak resulted in about 300 deaths.19 It is important to note that there is substantial evidence that VEEV is also highly infectious through an aerosol route of exposure. This finding is highlighted by over 150 documented cases caused by accidental laboratory exposures in the literature, some of which are presumed to have occurred by the aerosol route.20 This finding has, in part, resulted in an increased emphasis on medical countermeasure development for VEEV, EEEV, and WEEV from a biodefense perspective.
Need for a Trivalent WEEV, EEEV, and VEEV Vaccine
There are currently no FDA-approved vaccines or antiviral medical countermeasures available to protect against or treat infection by WEEV, EEEV, or VEEV. There are two major factors to be considered when discussing the need for a trivalent vaccine: the need from a biodefense perspective and the costs associated with treating severe illness caused these encephalitic alphaviruses. These viruses were developed as agents of biological warfare before the Biological Weapons Convention Treaty.21 These viruses were also pursued for biological warfare applications largely because of the ease of producing high quantities of viruses and their highly infectious nature through aerosol exposure. Furthermore, the cost associated with supportive treatment of endemic cases can range from $21,000 for mild infections up to $3 million for severe encephalitis in the case of WEEV.17 An effective vaccine would greatly limit the threat posed by these viruses by preventing Warfighter fatalities, enhancing the ability of the Warfighter to meet mission objectives, and protecting the civilian population. As a result, the Defense Threat Reduction Agency–Joint Science and Technology Office and Joint Program Executive Office–Medical Countermeasure Systems have formed a translational team to facilitate advancement of candidate vaccines from the technology base to advanced development toward FDA licensure.
Vaccines against encephalitic alphaviruses are also of significant interest to the agricultural community. In the 1960s and 1970s, VEEV outbreaks in Columbia, Central America, Mexico, and the United States warranted vaccination of over 2 million equids with the live vaccine strain TC-83, which was attenuated by 83 passages through cultured guinea pig heart cells. Although TC-83 was quite successful in limiting the spread of the 1971 Texas VEE epizootic, two key issues were noted. In early studies, signs of disease were observed in 5 of 10 horses vaccinated with TC-83, and viremia was observed in 8 of those animals, suggesting that the attenuated virus could be transmitted back to mosquitoes.22,23 This finding also further highlighted a second issue, the potential for reversion back to virulence given that attenuation relies on only two-point mutations.24 In an attempt to mitigate the concern of virulence reversion, a new live-attenuated virus vaccine (V3526) was derived by site-directed mutagenesis of the Trinidad donkey strain of VEEV subtype 1AB. A protein cleavage site (PE2) that had been shown to be involved in virulence was deleted from an infectious complementary DNA (cDNA) clone, and a second mutation was made in the E1 protein.25 Development of V3526 was continued to the point of testing in a horse model of infection and showed promising results in terms of safety and protection.26 A phase I clinical study was initiated and showed promising results in terms of immunogenicity. However, safety remained a concern, because fever and flu-like symptoms were associated with human use of the vaccine.27 An inactivated version of TC-83 (C84) is also available in North America but typically only recommended in high-risk areas. As a result, TC-83 continues to be produced in Colombia and Mexico for use in equids. Vaccination against WEEV and EEEV is currently recommended for horses living in or traveling to North America because of exposure risks and the high mortality associated with these viruses in equine hosts.28 A bivalent preparation is typically used, consisting of formalin-inactivated, adjuvanted whole viruses.
TC-83 is also currently used for laboratory workers and other at-risk personnel under IND status. However, there are substantial issues with both the immunogenicity and safety of this vaccine candidate. Of more than 800 individuals who received the vaccine between 1976 and 1990, nearly 20% did not respond as measured by neutralizing antibody titers.29 Furthermore, over 20% of individuals experienced reactogenicity issues, including fever, muscle aches, and headaches.30 Boosts with C84 are often required for non-responders to TC-83. Formalin-inactivated EEEV and WEEV vaccines have been used under IND status to vaccinate at-risk laboratory workers as well. However, these vaccines require multiple boosts to achieve and maintain detectable neutralizing antibody titers in human recipients and provide incomplete protection in aerosol animal challenge models. With the goal of a trivalent vaccine in mind, it is also important to note that multiple studies have now shown that there is potential for immune interference when these IND vaccines are used in an attempt to protect against all three species; immune interference has been observed when vaccinations are given both sequentially and simultaneously.29,31 Therefore, although the existing IND vaccines are still currently recommended for at-risk laboratory workers, the combination of safety, immunogenicity, and immune interference issues have warranted additional investments in development of an improved trivalent vaccine to fulfill the requirements of the biodefense community.
Recent progress to trivalent WEEV, EEEV, and VEEV vaccines
The research community has continued to pursue safer and more effective vaccines against the encephalitic alphaviruses, with many groups emphasizing VEEV because of its potential for epizootic outbreaks. Efforts have been made to develop next generation vaccines through a number of platforms, including live-attenuated virus chimeras and targeted mutants, viral replicons (VRPs), virus-like particles (VLPs), DNA-based approaches, and an array of different inactivation techniques for whole viruses.32–35 The number of candidate vaccines that have been developed for individual virus species is much larger than the number that has been tested for potential use as trivalent vaccines. Table 1 highlights the progress to a trivalent vaccine against WEEV, EEEV, and VEEV, which has largely focused on inactivated viruses, VRPs, VLPs, and DNA-based vaccines.
Table 1.
Snapshot of current WEVEE vaccines in development
| Vaccine platform | Breadth of protection | Route of challenge | Route of vaccine administration | Animal species |
|---|---|---|---|---|
| DNA vaccine | WEEV, EEEV, and VEEV | Aerosol | Intramuscular* | Cynomolgus macaque |
| VRP | EEEV and VEEV† | Aerosol | Subcutaneous | Cynomolgus macaque |
| VLP | WEEV, EEEV, and VEEV | Aerosol | Intramuscular | Cynomolgus macaque |
| Inactivated virus‡ | WEEV, EEEV, or VEEV | Aerosol | Various | Balb/c mouse |
Current formulation of the DNA vaccine requires electroporation in the administration process. VRP has been shown to protect against EEEV and VEEV but not yet against WEEV Inactivated virus has been assessed via a range of administration routes including intramuscular, subcutaneous, and intranasal.
Various formulations of inactivated virus have been tested in recent years to include different mechanisms of inactivation and routes of administration. These approaches have typically involved a mixture of the three species inactivated by formalin, 1,5-iodonapthyl-azide, or γ-irradiation. The impact of the route of administration has also been investigated, including intramuscular, subcutaneous, and intranasal delivery of the inactivated virus. Immunogenicity and protective efficacy have been shown to vary somewhat as functions of the inactivation strategy and route of administration27,36 (Glass P and others, unpublished data). However, a formulation that elicits an optimal immune response has not been achieved, resulting in decreased emphasis on inactivated candidates.
The VRP platform being pursued is based on an attenuated strain of VEEV (V3014) into which the genes coding for various structural proteins can be inserted.37 In the case of the Western, Eastern, and Venezuelan Equine Encephalitis (WEVEE) vaccine candidate, it involves expression of the alphavirus glycoproteins with deletions in the PE2 furin cleavage site. Protective efficacy of a trivalent WEVEE VRP formulation has been observed in a lethal mouse model for all three viruses. Furthermore, protective efficacy has also been suggested in a cynomolgos macaque model of infection with the WEVEE VRP (Glass P and others, unpublished data). This finding, along with similar results for the VLP and DNA-based vaccines, provides proof of concept that a trivalent alphavirus vaccine may be feasible.
A variety of VLPs has been pursued for vaccination against alphaviruses; however, the most mature VLP has stemmed from initial work with Chikungunya virus. Expression of the virus structural proteins resulted in a VLP that resembled the structure of live alphaviruses.38 This VLP was shown to elicit a robust antibody response and protection against Chikungunya virus.38 These methods are now being applied to WEEV, EEEV, and VEEV, where monovalent preparations were shown to be protective against all three viruses in both mice and non-human primates (NHPs) with no detection of viremia. Trivalent preparations of the three VLPs are currently being evaluated for immunogenicity and protective efficacy in mouse and NHP models of infection.
The DNA-based vaccines consist of plasmids with an insert encoding the E1 and E2 envelope glycoproteins of WEEV, EEEV, or VEEV. The DNA is delivered by intramuscular or intradermal electroporation, which facilitates increased uptake of the DNA by host cells. After they are inside the cells, the viral genes are transcribed and translated by host cell machinery to yield E1 and E2 proteins.34 The DNA vaccines delivered by electroporation elicit a robust immune response to include high levels of virus-neutralizing antibodies in multiple animal species. Protection against aerosol challenge with all three viruses has been observed in mice and NHPs.34 Importantly, there is no reduction in immunogenicity or protective efficacy when the vaccines are given as a trivalent formulation as opposed to monovalent formulations (Dupuy L and others, unpublished data). In terms of vaccines to be used for protection of the Warfighter, the administration of the DNA-based vaccines by electroporation poses a logistical challenge in terms of use for protection of the Warfighter, in that it requires an electrical device for optimal delivery in its present format. However, next generation devices suitable for field deployment are under development and likely to greatly reduce the logistical issues associated with these first generation clinical devices. Nevertheless, the success of the DNA vaccines as a trivalent vaccine suggests that studies to identify simpler delivery platforms may be warranted as well.
Path from experimental vaccines to licensure
As noted in the previous section, multiple vaccines have shown promising efficacy against WEEV, EEEV, and VEEV in established animal models. However, advancing these candidates to licensure will require continued emphasis from both the science and technology base and the advanced development community in the near future. This section will begin to touch on a strategy that may be used to ultimately deliver a safe and effective vaccine against WEEV, EEEV, and VEEV to the Warfighter.
Regarding the protection of Warfighters against the encephalitic alphaviruses, efficacy against an aerosol exposure is the primary goal given the potential biological threat. However, with no cases of aerosol occurring in nature, and a limited number of documented laboratory exposures, approval for an aerosol indication would likely occur through the FDA Animal Rule. That being the case, the development of well-characterized models of aerosol exposure to WEEV, EEEV, and VEEV is paramount to advancing vaccine candidates to licensure. Equine species are natural hosts in terms of the epizootic disease but limited in their use as experimental models of encephalitic alphaviruses because of their size. Therefore, substantial development of both small and large animal models of aerosolized WEEV, EEEV, and VEEV infection has been pursued.
Animal model development.
Mouse models of infection have been pursued extensively for all three viruses and offer the benefits of well-characterized immunological reagents and congenic mutant strains that can help to tease out mechanisms of pathogenesis and immunological protection. Peripheral VEEV infection of mice is lymphotropic, and entrance into the central nervous system (CNS) occurs only after viremia seeds infection of the olfactory neurons.39 Aerosol infections of mice by VEEV have shown a tropism for the olfactory neuroepithelium, resulting in more rapid neuroinvasion relative to a subcutaneous exposure.40,41 VEEV is able to infect a range of neuronal cell types, and lesions are observed in both neural and non-neural tissues. Use of an array of attenuated virus strains and immunodeficient mouse strains has elucidated both viral and host factors that play key roles in VEEV pathogenesis. EEEV infection of mice also results in severe neuroinvasion but is more age-dependent than VEEV. Unlike VEEV, EEEV is not lymphotropic, and its route of CNS invasion through the bloodstream after subcutaneous exposure remains poorly characterized. In contrast, exposure through the aerosol route involves neuroinvasion through the olfactory system much like VEEV.42 Otherwise, many of the general pathological findings seem to be similar to what is often observed in clinical cases. WEEV neuroinvasion and neurovirulence vary widely by strain, and like EEEV, its mechanism of entry into the CNS is not well-understood. Aerosol models of WEEV exposure in mice have also been documented with neuronal lesions but not with the same amount of detail regarding its pathophysiology relative to the other alphaviruses. In all, the mouse models of aerosol exposure of the encephalitic alphaviruses have been characterized rather thoroughly, and many of the pathological findings seem similar to those findings often observed in clinical cases. As a result, they have provided useful tools in the initial assessment and down-selection of vaccine candidates.
Licensure of a trivalent vaccine for WEEV, EEEV, and VEEV by the FDA Animal Rule will likely require a well-characterized large animal model in which pivotal animal studies can be conducted. In this light, the cynomolgus macaque (Macaca fascicularis) would be a logical choice to pursue given (1) the observed pathophysiology, (2) the relation to human disease, and (3) the amount of work in this species described in the literature. Similar to the human condition for VEEV, most infected cynomolgus macaques develop a transient fever and viremia, occasionally with neurological signs, but eventually recover from the infection.43 Although many of the past studies were limited in terms of the technologies that were available to analyze the tissues, the general disease progression is similar to that observed in humans. Additional cynomolgus macaque infections through the aerosol route with more recent clinical isolates will be useful to provide detailed pathophysiological findings and comparisons with past experiments involving subcutaneous exposures.
Relative to VEEV, there have been far fewer studies involving experimental infections of NHPs with EEEV. However, the results of these studies suggest that cynomolgus macaques may also be a suitable model for EEEV. Infection by EEEV was lethal by aerosol challenge with high doses, with 8 of 12 animals developing fever and neurological signs. The animals also succumbed to infection within 5–9 days, which is consistent with the high mortality associated with human disease relative to the other alphaviruses.44 Similarly, there have been a limited number of WEEV infections in the cynomolgus macaque, but they have also suggested use for this NHP species as a model for WEEV. Macaques developed fever within 4–5 days as well as leukocytosis and hyperglycemia, which were accompanied by lesions in the brain, with WEEV antigens being identified in microglial cells and neurons.45 As is typical of WEEV infection in humans, the lethality rate was low, with one of six animals in each of the high- and low-dose groups succumbing to disease.
Infection of the cynomolgus macaque by WEEV, EEEV, or VEEV results in many similar pathological findings relative to human disease,43 but a significant amount of work remains to be completed to thoroughly characterize the infectivity and lethality of the alphaviruses by the aerosol route. This work will need to include detailed analyses of the physiological and immunological responses to the virus. However, the choice of virus strain will also be a critical aspect in additional development of the cynomolgus macaque models of WEEV, EEEV, and VEEV infection.
Strain selection.
In selecting the strains of viruses to incorporate into animal model development, there are a few major criteria that must be considered. Isolation from human clinical cases is a first critical checkpoint for isolates to be considered. WEEV, EEEV, and VEEV can all readily be isolated from their respective vector and reservoir hosts, but not all isolates may be able to cause human disease. Thus, it is important to choose isolates that are known to be capable of causing the disease in humans. Passage history is another key concern for these viruses. Studies with VEEV have shown that removal of selective pressures associated with a two-host lifecycle results in accumulation of single nucleotide polymorphisms (SNPs),46,47 and cell culture passages often result in adaptation for heparin sulfate binding, which can result in artificial attenuation.48 Isolates with low numbers of passages and well-characterized passage histories would be a substantial benefit to the animal models. The use of virus stocks directly propagated from natural isolates versus stocks derived from infectious clones should also be considered. Each strategy offers key advantages, with a natural isolate being a better representation of the quasispecies and an infectious clone providing well-characterized, homogenous challenge material. However, additional discussions with the FDA will be required to decide which strategy is preferable for product licensure.
Relevance to currently circulating strains should also be considered, which would be supported by more extensive sampling and characterization of clinical isolates. VEEV presents an additional concern in that IAB strains were involved in offensive programs in the past, but IC strains are more relevant to recently circulating virus subtypes. The fact that there are multiple subtypes that could be a concern in terms of clinical illness poses a key challenge in terms of appropriate strain selection. That being said, there are multiple isolates for each virus that are quite suitable for inclusion in the development of the cynomolgus macaque model of infection.
Beyond the isolates used in the animal models, additional isolates may be of interest to test the breadth of protection conferred by a vaccine. It is important that a trivalent vaccine protect against the most relevant subtypes and strains of each viral species; thus, it will be essential to show cross-protection against a panel of isolates to determine the breadth of efficacy. EEEV is a fairly conserved species in terms of genomic diversity of strains with known human virulence. Until recently, it was believed that only Group I North American strains were a concern in terms of human disease. However, recent analyses of a 2010 outbreak in Panama have challenged that paradigm.49 Given that these strains caused severe disease in humans, additional studies in animal models may be warranted to determine if and how these strains have evolved to virulence. If these strains prove to be more virulent than other typical Central and South American strains, an assessment of immunological cross-reactivity may be essential to ensure sufficient protection of a licensed vaccine.
WEEV is even more conserved than EEEV, although it is poorly represented in public databases. WEEV has been suggested to be evolving to virulence at a cost of infectivity to mosquito vectors,50 but it is difficult to determine because of the paucity of genomic sequence data available and variability within the animal models. Differential virulence has been observed among WEEV isolates associated with changes in the E2 protein.50 For both WEEV and EEEV, additional genomic sequencing and phylogenetic analyses of clinical and veterinary isolates as well as comparative virulence studies in relevant animal models would provide a solid rationale to define a panel of isolates against which immunological cross-reactivity should be measured.
As noted above, VEEV may present additional challenges because of the large number of subtypes, which may necessitate additional genomic characterization of clinical isolates and analyses of the virulence in defined animal models. The structural proteins, specifically E1 and E2, comprise the antigens that are being included in many of the experimental trivalent WEVEE vaccine constructs. Thus, the genomic variation among VEEV isolates in the E1 and E2 genes could be especially important in considering a panel of strains against which vaccine efficacy could be measured.
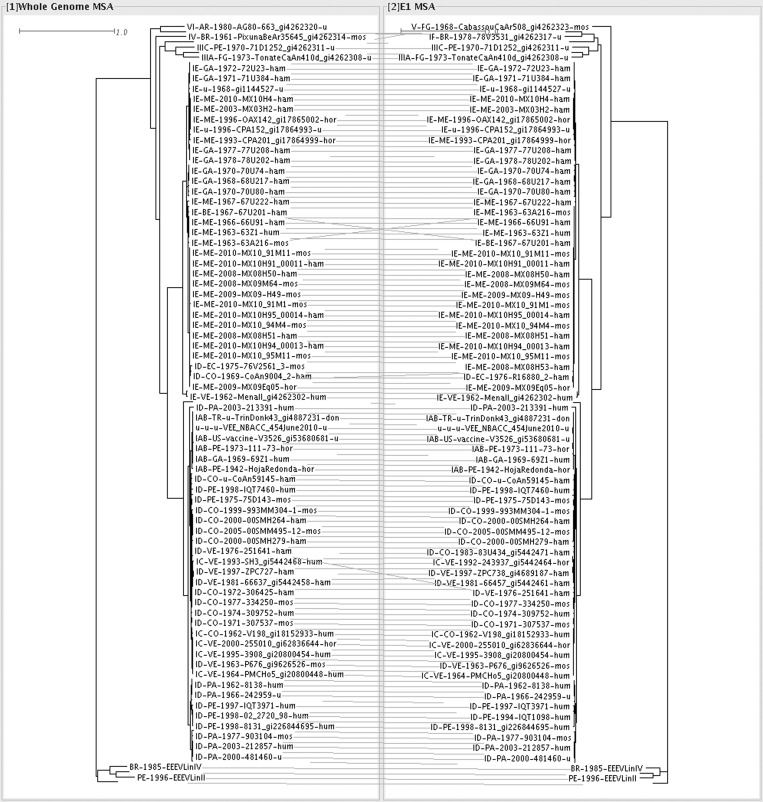
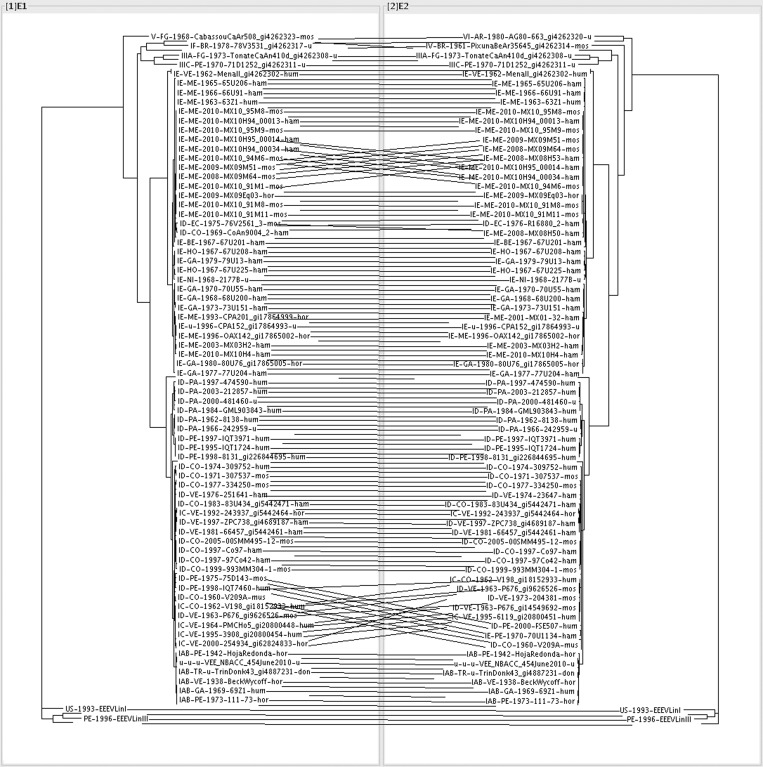
Preliminary analyses have shown that E1 and E2 have lower resolution for strain discrimination than the whole genome, with E2 having better resolution than E1. However, the envelope genes do capture the same higher-level clades in the phylogeny as the full genome. The tanglegram in Figure 1 illustrates that 60% of splits from the whole genome were observed in trees built from just the gene for E1. The observed differences were not in the major branches of the phylogeny but the fine-scale arrangement of strains within clades. Similarly, Figure 2 illustrates the phylogenetic differences between E1 and E2. Figure 2 also shows that major genome groupings are the same and that only the relationship among closely related strains within clades differs between E1 and E2. In particular, the strain relationships differ between E1 and E2 among isolates from a 2008–2010 outbreak of a VEEV IE subtype in Mexico and a subset of IC and ID isolates from Venezuela, Columbia, and Peru (Figure 2). Additional analyses have determined which SNPs have allele variants that are non-randomly associated with given subtypes using χ2 P values using the PPFS package (Hall BG and others, unpublished data).51,52 Values were calculated separately for each subtype versus the others (e.g. type IC versus IAB, ID, IE, etc.). For non-synonymous SNPs, there were 20 and 46 for E1 and E2, respectively, that were non-randomly associated with a subtype. Together, these data suggest that focusing on gene variation in E1 and E2 would identify strains that would be of particular interest for heterologous challenge studies while also displaying the general diversity across major clades for VEEV. A greater understanding of the genomic diversity of these viruses and how that diversity may impact virulence will provide a sound rationale for the selection of a panel of WEEV, EEEV, and VEEV isolates against which immunological cross-reactivity would need to be analyzed.
Figure 1.
Multiple sequence alignment (MSA) was used to generate maximum likelihood tree and tanglegram of whole genome versus E1 gene of VEEV genomes. Maximum likelihood phylogenies were generated from multiple sequence alignment of the genomes. The number of splits shared between different trees was calculated using FastTree and visualized with tanglegrams. The tanglegram was created in Dendroscope. Equivalent branch rotations that did not change the relationships within a tree are performed by an algorithm to minimize the number of crossing lines between trees. The names of the VEEV strains included serotype, country of origin, year of collection, strain name, and the host species from which it was isolated. Countries included Colombia (CO), Venezuela (VE), Ecuador (EC), Peru (PE), the United States (US), Guatemala (GA), Trinidad (TR), Panama (PA), Mexico (ME), Honduras (HO), French Guiana (FG), Belize (BE), Brazil (BR), and unknown (u). Host species included hamster (ham), human (hum), horse (hor), donkey (don), mosquito (mos), and unknown (u).
Figure 2.
Maximum likelihood tree and tanglegram of E1 versus E2 genes of VEEV genomes. The trees and the tanglegram were generated as described in Figure 1. The phylogenetic differences between E1 and E2 show that major genome groupings are the same, and only the relationship among closely related strains within clades differs between the two genes.
Path to FDA licensure.
In seeking a vaccine that will protect against WEEV, EEEV, and VEEV by aerosol exposure, there are several key aspects that will help ensure progress to licensure. It will require well-characterized challenge material with appropriate histories in terms of clinical isolation and limited passaging. Deep sequencing of the working stocks of these strains would provide additional characterization of their quasispecies makeup, but consensus sequences would be required at a minimum.
The animal models of aerosol infection will require additional development to serve as the animal models to be used in pivotal efficacy studies. The lack of aerosol cases in nature poses a challenge, although there are nearly 150 documented cases of VEEV infection caused by accidental laboratory exposure in the literature.20 Thorough comparison of the pathological findings in the cynomolgus macaque with findings from human cases will be critical. However, there may be opportunities to bridge data from aerosol exposures to subcutaneous VEEV exposures as well. Comparisons could be made between subcutaneous exposures in macaques and natural disease in humans and then between subcutaneous and aerosol exposures in macaques to provide the three-way comparison. That being said, the human cases of aerosol exposure, although limited, could be the key data points that will enable the use of cynomolgus macaques in the Animal Rule.
Identification of correlates of protection will be another critical piece of information for a successful WEEV, EEEV, and VEEV vaccine program. It will be essential, given a vaccine candidate, to determine the mechanism by which it confers protection. This determination would enable measurements of the key immunological parameter(s) in clinical trials that are indicative of protective efficacy and shown in pivotal animal studies.53 In that light, validated assays to measure these parameter(s) will also be needed.54
Multiple experimental vaccines are continuing progress to a point at which clinical trials are justifiable. Regarding licensure of a vaccine against aerosol exposures, the phases I and II safety and immunogenicity trials would be conducted in a manner similar to that of products for other infectious diseases. However, a phase III study would not include a field efficacy end point. Instead, phase I/II clinical testing would provide an expanded immunogenicity and safety study to be accompanied by a pivotal animal study. In the case of the trivalent vaccine, the pivotal animal study would likely use an IAB strain of VEEV given its history in offensive programs, relevance to human clinical disease, and that it is the cause of a limited number of aerosol exposures of humans in laboratory accidents. With the goal of a trivalent vaccine in mind, two options could be pursued. The more straightforward option would consist of additional pivotal animal studies showing protective efficacy against a small set of the most relevant strains. Alternatively (and if a correlate of immunity proves to be well-defined for the vaccine in question), material (e.g., serum) from the clinical trials could be used in passive transfer/adoptive transfer experiments in the appropriate animal model and/or in vitro assays to measure immunological cross-reactivity. In all likelihood, it will be some combination of the above. However, continued emphasis on the biology of encephalitic alphaviruses in terms of their genomic diversity, the structural biology of the envelope proteins, and their comparative virulence will provide the rationale needed to inform well-designed studies that will prove the breadth of vaccine efficacy. Additional development of the animal models and assays will enable the eventual licensure of these vaccines. Keeping these issues in mind, a safe and effective vaccine will be delivered to the Warfighter that may also be of use to the public health and agricultural communities.
ACKNOWLEDGMENTS
We thank Dr. Scott Weaver for discussions related to this manuscript. We acknowledge the discussions generated by Symposium #80, “Development of Equine Encephalitis (WEVEE) Vaccines: Epidemiologic, Immunologic, Clinical and Regulatory Considerations,” at the 62nd Annual Meeting of the American Society of Tropical Medicine and Hygiene, which included participation by D.N.W., D.G.H., C.S.S., Scott Weaver, Jorge Boshell, and Erik Henchal. We also thank Dr. Pamela Glass for personal communications regarding her work with trivalent alphavirus vaccines.
Disclaimer: The views and opinions presented here are personal and not to be construed as official positions of the US Government, the Department of Defense, or the affiliated organizations of the authors.
Footnotes
Authors' addresses: Daniel N. Wolfe, Chemical and Biological Technologies Department, Defense Threat Reduction Agency, Fort Belvoir, VA, E-mail: daniel.wolfe@dtra.mil. D. Gray Heppner, TASC, Inc., Lorton, VA, and Chemical and Biological Technologies Department, Defense Threat Reduction Agency, Fort Belvoir, VA, E-mail: donald.heppner@tasc.com. Shea N. Gardner, Computations/Global Security, Lawrence Livermore National Laboratory, Livermore, CA, E-mail: Gardner26@llnl.gov. Crystal Jaing, Physical and Life Sciences Directorate, Lawrence Livermore National Laboratory, Livermore, CA, E-mail: jaing2@llnl.gov. Lesley C. Dupuy and Connie S. Schmaljohn, Virology Division, US Army Medical Research Institute for Infectious Diseases, Fort Detrick, MD, E-mails: lesley.c.dupuy.ctr@mail.mil and connie.s.schmaljohn.civ@mail.mil. Kevin Carlton, Medical Countermeasure Systems, Joint Vaccine Acquisition Program, Fort Detrick, MD, E-mail: kevin.s.carlton.civ@mail.mil.
References
- 1.Paessler S, Weaver SC. Vaccines for Venezuelan equine encephalitis. Vaccine. 2009;27((Suppl 4)):D80–D85. doi: 10.1016/j.vaccine.2009.07.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jose J, Snyder JE, Kuhn RJ. A structural and functional perspective of alphavirus replication and assembly. Future Microbiol. 2009;4:837–856. doi: 10.2217/fmb.09.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zacks MA, Paessler S. Encephalitic alphaviruses. Vet Microbiol. 2010;140:281. doi: 10.1016/j.vetmic.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calisher CH. Medically important arboviruses of the United States and Canada. Clin Microbiol Rev. 1994;7:89–116. doi: 10.1128/cmr.7.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell CJ, Monath TP, Sabattini MS, Daffner JF, Cropp CB, Calisher CH, Darsie RF, Jakob WL. Arbovirus isolates from mosquitoes collected during and after the 1982–1983 epizootic of western equine encephalitis in Argentina. Am J Trop Med Hyg. 1987;36:107–113. doi: 10.4269/ajtmh.1987.36.107. [DOI] [PubMed] [Google Scholar]
- 6.Hahn CS, Lustig S, Strauss EG, Strauss JH. Western equine encephalitis virus is a recombinant virus. Proc Natl Acad Sci USA. 1988;85:5997–6001. doi: 10.1073/pnas.85.16.5997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calisher CH, Karabatsos N, Lazuick JS, Monath TP, Wolff KL. Reevaluation of the western equine encephalitis antigenic complex of alphaviruses (family Togaviridae) as determined by neutralization tests. Am J Trop Med Hyg. 1988;38:447–452. doi: 10.4269/ajtmh.1988.38.447. [DOI] [PubMed] [Google Scholar]
- 8.Weaver SC, Kang W, Shirako Y, Rumenapf T, Strauss EG, Strauss JH. Recombinational history and molecular evolution of western equine encephalomyelitis complex alphaviruses. J Virol. 1997;71:613–623. doi: 10.1128/jvi.71.1.613-623.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bianchi TI, Aviles G, Monath TP, Sabattini MS. Western equine encephalomyelitis: virulence markers and their epidemiological significance. Am J Trop Med Hyg. 1993;49:322–328. doi: 10.4269/ajtmh.1993.49.322. [DOI] [PubMed] [Google Scholar]
- 10.Bianchi TI, Aviles G, Sabattini MS. Biological characteristics of an enzootic subtype of western equine encephalomyelitis virus from Argentina. Acta Virol. 1997;41:13–20. [PubMed] [Google Scholar]
- 11.Nagata LP, Hu WG, Parker M, Chau D, Rayner GA, Schmaltz FL, Wong JP. Infectivity variation and genetic diversity among strains of western equine encephalitis virus. J Gen Virol. 2006;87:2353–2361. doi: 10.1099/vir.0.81815-0. [DOI] [PubMed] [Google Scholar]
- 12.Brault AC, Powers AM, Chavez CL, Lopez RN, Cachon MF, Gutierrez LF, Kang W, Tesh RB, Shope RE, Weaver SC. Genetic and antigenic diversity among eastern equine encephalitis viruses from North, Central and South America. Am J Trop Med Hyg. 1999;61:579–586. doi: 10.4269/ajtmh.1999.61.579. [DOI] [PubMed] [Google Scholar]
- 13.Arrigo NC, Adams AP, Weaver SC. Evolutionary patterns of eastern equine encephalitis virus in North versus South America suggest ecological differences and taxonomic revision. J Virol. 2010;84:1014–1025. doi: 10.1128/JVI.01586-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrera JP, Forrester N, Wang E, Vittor AY, Haddow AD, Lopez-Verges S, Abadia I, Castano E, Sosa N, Baez C, Estripeaut D, Diaz Y, Beltran D, Cisneros J, Cedeno HG, Travassos da Rosa AP, Hernandez H, Martinez-Torres AO, Tesh RB, Weaver SC. Eastern equine encephalitis in Latin America. N Engl J Med. 2013;369:732–744. doi: 10.1056/NEJMoa1212628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brault AC, Powers AM, Holmes EC, Woelk CH, Weaver SC. Positively charged amino acid substitutions in the e2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J Virol. 2002;76:1718–1730. doi: 10.1128/JVI.76.4.1718-1730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weaver SC, Winegar R, Manger ID, Forrester NL. Alphaviruses: population genetics and determinants of emergence. Antiviral Res. 2012;94:242–257. doi: 10.1016/j.antiviral.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention . Fact Sheet Western Equine Encephalitis. 2005. http://www.cdc.gov/ncidod/dvbid/arbor/weefact.htm Available at. Accessed March 6, 2014. [Google Scholar]
- 18.Steele K, Reed DS, Glass PJ, Hart MK, Ludwig GV, Pratt WD, Parker MD, Smith JF. Alphavirus encephalitides. In: Dembek ZF, editor. Medical Aspects of Biological Warfare. Fort Sam Houston, TX: Office of the Surgeon General, Department of the Army and US Army Medical Department Center and School,; 2007. pp. 241–270. [Google Scholar]
- 19.Rivas F, Diaz LA, Cardenas VM, Daza E, Bruzon L, Alcala A, De la Hoz O, Caceres FM, Aristizabal G, Martinez JW, Revelo D, De la Hoz F, Boshell J, Camacho T, Calderon L, Olano A, Villareal LI, Roselli D, Alvarez G, Ludwig G, Tsai T. Epidemic Venezuelan Equine Encephalits in La Guajira, Colombia, 1995. J Infect Dis. 1997;175:828–832. doi: 10.1086/513978. [DOI] [PubMed] [Google Scholar]
- 20.Sewell D. Laboratory-associated infections and biosafety. Clin Microbiol Rev. 1995;8:389–405. doi: 10.1128/cmr.8.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Croddy EC, Hart C, Perez-Armendariz J. Chemical and Biological Warfare. Berlin, Germany: Springer; 2002. pp. 30–31. [Google Scholar]
- 22.Walton TE, Alvarez O, Buckwalter RM, Johnson KM. Experimental infection of horses with enzootic and epizootic strains of Venezuelan equine encephalomyelitis virus. J Infect Dis. 1973;128:271–282. doi: 10.1093/infdis/128.3.271. [DOI] [PubMed] [Google Scholar]
- 23.Walton TE, Alvarez O, Buckwalter RM, Johnson KM. Experimental infection of horses with an attenuated Venezuelan equine encephalomyelitis vaccine (strain TC-83) Infect Immun. 1972;5:750–756. doi: 10.1128/iai.5.5.750-756.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, Johnston RE. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995;212:102–110. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- 25.Spertzel RO, Kahn DE. Safety and efficacy of an attenuated Venezuelan equine encephalomyelitis vaccine for use in Equidae. J Am Vet Med Assoc. 1971;159:731–738. [PubMed] [Google Scholar]
- 26.Fine DL, Roberts BA, Teehee ML, Terpening SJ, Kelly CLH, Raetz JL, Baker DH, Powers AM, Bowen RA. Venezuelan equine encephalitis virus vaccine candidate (V3526) safety, immunogenicity and efficacy in horses. Vaccine. 2007;25:1868–1876. doi: 10.1016/j.vaccine.2006.10.030. [DOI] [PubMed] [Google Scholar]
- 27.Martin SS, Bakken RR, Lind CM, Garcia P, Jenkins E, Glass PJ, Parker MD, Hart MK, Fine DL. Comparison of the immunological responses and efficacy of gamma irradiated V3526 vaccine formulations against subcutaneous and aerosol challenge with venezuelan equine encephalitis virus subtype IAB. Vaccine. 2010;28:1031. doi: 10.1016/j.vaccine.2009.10.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Association of Equine Practitioners . Core Vaccination Guidelines, Eastern/Western Encephalomyelitis. 2014. http://www.aaep.org/-i-165.htm Available at. Accessed March 6, 2014. [Google Scholar]
- 29.Pittman PR, Liu C, Cannon TL, Mangiafico JA, Gibbs PH. Immune interference after sequential alphavirus vaccine vaccinations. Vaccine. 2009;27:4879–4882. doi: 10.1016/j.vaccine.2009.02.090. [DOI] [PubMed] [Google Scholar]
- 30.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996;14:337–343. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- 31.Reisler RB, Gibbs PH, Danner DK, Boudreau EF. Immune interference in the setting of same-day administration of two similar inactivated alphavirus vaccines: eastern equine and western equine encephalitis. Vaccine. 2012;30:7271–7277. doi: 10.1016/j.vaccine.2012.09.049. [DOI] [PubMed] [Google Scholar]
- 32.Paessler S, Weaver SC. Vaccines for Venezuelan equine encephalitis. Vaccine. 2009;27:D80–D85. doi: 10.1016/j.vaccine.2009.07.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guerbois M, Volkova E, Forrester NL, Rossi SL, Frolov I, Weaver SC. IRES-driven expression of the capsid protein of the Venezuelan equine encephalitis virus TC-83 vaccine strain increases its attenuation and safety. PLoS Negl Trop Dis. 2013;7:e2197. doi: 10.1371/journal.pntd.0002197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dupuy LC, Richards MJ, Ellefsen B, Chau L, Luxembourg A, Hannaman D, Livingston BD, Schmaljohn CS. A DNA vaccine for Venezuelan equine encephalitis virus delivered by intramuscular electroporation elicits high levels of neutralizing antibodies in multiple animal models and provides protective immunity to mice and nonhuman primates. Clin Vaccine Immunol. 2011;18:707–716. doi: 10.1128/CVI.00030-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharma A, Gupta P, Glass PJ, Parker MD, Maheshwari RK. Safety and protective efficacy of INA-inactivated Venezuelan equine encephalitis virus: implication in vaccine development. Vaccine. 2011;29:953–959. doi: 10.1016/j.vaccine.2010.11.033. [DOI] [PubMed] [Google Scholar]
- 36.Fine DL, Jenkins E, Martin SS, Glass P, Parker MD, Grimm B. A multisystem approach for development and evaluation of inactivated vaccines for Venezuelan Equine Encephalitis Virus (VEEV) J Virol Methods. 2010;163:424. doi: 10.1016/j.jviromet.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pushko P, Bray M, Ludwig GV, Parker M, Schmaljohn A, Sanchez A, Jahrling PB, Smith JF. Recombinant RNA replicons derived from attenuated Venezuelan equine encephalitis virus protect guinea pigs and mice from Ebola hemorrhagic fever virus. Vaccine. 2000;19:142–153. doi: 10.1016/s0264-410x(00)00113-4. [DOI] [PubMed] [Google Scholar]
- 38.Akahata W, Yang Z, Andersen H, Sun S, Holdaway HA, Kong W, Lewis MG, Higgs S, Rossmann MG, Rao S, Nabel GJ. A VLP vaccine for epidemic Chikungunya virus protects non-human primates against infection. Nat Med. 2010;16:334–338. doi: 10.1038/nm.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aronson JF, Grieder FB, Davis NL, Charles PC, Knott T, Brown K, Johnston RE. A single-site mutant and revertants arising in vivo define early steps in the pathogenesis of Venezuelan equine encephalitis virus. Virology. 2000;270:111–123. doi: 10.1006/viro.2000.0241. [DOI] [PubMed] [Google Scholar]
- 40.Pratt WD, Hart MK, Reed DS, Steele KS. Alphaviruses. In: Swearengen JR, editor. Biodefense: Research Methodology and Animal Models. Boca Raton, FL: Taylor & Francis; 2006. pp. 181–206. [Google Scholar]
- 41.Ryzhikov AB, Ryabchikova EI, Sergeev AN, Tkacheva NV. Spread of Venezuelan equine encephalitis virus in mice olfactory tract. Arch Virol. 1995;140:2243–2254. doi: 10.1007/BF01323243. [DOI] [PubMed] [Google Scholar]
- 42.Vogel P, Kell WM, Frtiz DL, Parker MD, Schoepp RJ. Early events in the pathogenesis of eastern equine encephalitis virus in mice. Am J Pathol. 2005;166:159–171. doi: 10.1016/S0002-9440(10)62241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steele KE, Twenhafel NA. Review paper: pathology of animal models of alphavirus encephalitis. Vet Pathol. 2010;47:790–805. doi: 10.1177/0300985810372508. [DOI] [PubMed] [Google Scholar]
- 44.Reed DS, Lackemeyer MG, Garza NL, Norris S, Gamble S, Sullivan LF, Lind CM, Raymond JL. Severe encephalitis in cynomolgus macaques exposed to aerosolized eastern equine encephalitis virus. J Infect Dis. 2007;196:441–450. doi: 10.1086/519391. [DOI] [PubMed] [Google Scholar]
- 45.Reed DS, Larsen T, Sullivan LJ, Lind CM, Lackemeyer MG, Pratt WD, Parker MD. Aerosol exposure to western equine encephalitis virus causes fever and encephalitis in cynomolgus macaques. J Infect Dis. 2005;192:1173–1182. doi: 10.1086/444397. [DOI] [PubMed] [Google Scholar]
- 46.Coffey LL, Vasilakis N, Brault AC, Powers AM, Tripet F, Weaver SC. Arbovirus evolution in vivo is constrained by host alternation. Proc Natl Acad Sci USA. 2008;105:6970–6975. doi: 10.1073/pnas.0712130105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCurdy K, Joyce J, Hamliton S, Nevins C, Sosna W, Puricelli K, Rayner JO. Differential accumulation of genetic and phenotypic changes in Venezuelan equine encephalitis virus and Japanese encephalitis virus following passage in vitro and in vivo. Virology. 2011;415:20–29. doi: 10.1016/j.virol.2011.03.030. [DOI] [PubMed] [Google Scholar]
- 48.Bernard KA, Klimstra WB, Johnston RE. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapid clearance from blood of mice. Virology. 2000;276:93–103. doi: 10.1006/viro.2000.0546. [DOI] [PubMed] [Google Scholar]
- 49.Carrera JP, Forrester NM, Wang E, Vittor AY, Haddow AD, Lopez-Verges S, Abadia I, Castano E, Sosa N, Baez C, Estripeaut D, Diaz Y, Beltran D, Cisneros J, Cedeno HG, Travassos da Rosa AP, Hernandez H, Martinez-Torres AO, Tesh RB, Weaver SC. Eastern equine encephalitis in Latin America. N Engl J Med. 2013;369:732–744. doi: 10.1056/NEJMoa1212628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mossel EC, Ledermann JP, Phillips AT, Borland EM, Powers AM, Olson KE. Molecular determinants of mouse neurovirulence and mosquito infection for western equine encephalitis virus. PLoS ONE. 2013;8:e60427. doi: 10.1371/journal.pone.0060427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gardner SN, Hall BG. When whole-genome alignments just won't work: kSNP v2 software for alignment-free SNP discovery and phylogenetics of hundreds of microbial genomes. PLoS ONE. 2013;8:e8170. doi: 10.1371/journal.pone.0081760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hall BG. SNP-associations and phenotype predictions from hundreds of microbial genomes without genome alignments. PLoS ONE. 2014;9:e90490. doi: 10.1371/journal.pone.0090490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burns DL. Licensure of vaccines using the Animal Rule. Curr Opin Virol. 2012;2:353–356. doi: 10.1016/j.coviro.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Plotkin SA. Complex correlates of protection after vaccination. Clin Infect Dis. 2013;56:1458–1465. doi: 10.1093/cid/cit048. [DOI] [PubMed] [Google Scholar]