Abstract
Cholera is a disease of poverty that remains prevalent in resource-limited countries. The abrupt emergence of an epidemic frequently takes communities and health systems by surprise. Spread is rapid and initial mortality high: delays in organizing an appropriate response, lack of health worker training, and high patient numbers contribute to high rates of complications and deaths.
Introduction
The epidemic currently affecting the Caribbean prompts us to reflect upon the Peruvian epidemic of 1991–1993, and to share the organizational system developed in Peru during that time. This system adopts a symptomatic approach to patient management, incorporating three key elements: discontinuation of the use of cholera cots, supervised oral rehydration, and focused design of the cholera treatment unit. This strategy facilitates early oral rehydration in severely dehydrated patients. Application of this system in resource-limited settings affected by cholera has the potential to significantly impact the evolution and outcome of ongoing and future cholera epidemics.
Characteristics of cholera infection include rapid dissemination and high mortality rates among affected populations, giving rise to seven pandemics over the past two centuries.1,2 Cholera is transmitted by contaminated food or water, and thus has a propensity to affect disadvantaged populations that lack sanitation facilities and safe water sources.2 General improvements in these services have led to an overall decline in cholera transmission. However, endemic areas and outbreaks still occur in regions where poverty and poor hygiene persist.3 Moreover, the ease and speed with which today's individual carriers are able to reach all corners of the world enables foci of infection with high mortality rates to be rapidly generated.4,5
The decrease in the global burden of morbidity and mortality from cholera is a historical success story, and has largely resulted from improved provision of rapid and efficient rehydration. This is vital during the initial stage of the disease, when sudden severe dehydration can lead to death before the immune system has had time to recognize and react to the infection, and to replace intestinal cells impregnated with the A subunit of the cholera toxin with new cells. The availability of oral rehydration salts (ORS), electrolyte-containing intravenous fluids, higher quality intravenous catheters, nasogastric tubes, and dialysis have all contributed to a reduction in the lethality of the infection.6 Use of antibiotics is also recognized as having an important role in epidemics through reducing the volume of fluid loss in the stools, which permits faster discharge of patients, and by shortening the duration of the shedding of infectious organisms in the stool and thus transmission within the family and wider community.1
The cholera epidemic that took place in Peru in the 1990s is recognized as having had high incidence yet low mortality rates within the current pandemic. There were 604,846 documented cases, with case fatality rates of 0.9%, 0.3%, and 0.8% in 1991, 1992, and 1993 respectively.7 This was consistently lower than the 1.0% rate that is considered internationally acceptable (World Health Organization [WHO], 2010 no. 806) and lower than those observed elsewhere, such as the more recent cholera epidemic in Haiti where case fatality rates averaged 1.2% across 2010–2012.8 In this communication, we present a system for the management of severely dehydrated cholera patients requiring hospitalization during an epidemic. This system is based on lessons learned during the Peruvian epidemic, drawing on the experiences of the Infectious and Tropical Diseases Service in the Hospital Dos de Mayo, Lima (SITE-H2M) in managing these patients. Our proposed system incorporates three key elements.
Discontinuation of the use of cholera cots.
“Cholera cots” are cots with a hole in the center that allows the patient to deposit stools directly into a recipient below without having to get up from the cot. Their use permits ongoing intravenous (IV) fluid administration or commencement of oral rehydration while the patient remains supine. It also allows the quantity of stools produced to be measured, facilitating monitoring of fluid balance and calculation of fluid replacement accordingly.9
In the SITE-H2M, cholera cots were implemented during the intense three year country-wide epidemic, but were abandoned after only 3 weeks because of problems associated with their use. Similar situations arose in different hospitals across Peru. Difficulties encountered that led to the discontinuation of this strategy included:
-
•
Delay in initiation and inadequate administration of oral rehydration: this was found to be the most significant setback resulting from the use of cholera cots. It was attributed to patients' natural desire to sleep in the interval after rapid correction of severe dehydration and consequent failure to commence oral rehydration early, interruption of subsequent drinking by sleep, and a reluctance to drink large volumes, particularly while lying down.
-
•
Challenges maintaining a clean environment: the cot design lead to frequent spillage of stool around the recipient and contamination of the surroundings and the cots themselves. Cleaning a bedpan is quicker and easier for staff than decontamination of a cot and its surroundings
-
•
Insufficient capacity for observation of patients by healthcare workers: in the context of the large number of patients requiring attention during an epidemic, the use of cholera cots meant that busy staff were not always immediately alerted to the passing of stools and were unable to measure losses and calculate individual patients' volume replacement requirements as frequently as this system necessitates. Failure to maintain accurate, concurrent knowledge of fluid balance and ensure prompt fluid administration led to patients who had initially received adequate rehydration re-entering into a clinical state of shock.
Supervised oral rehydration.
Patients who have presented with severe dehydration are relocated to a seated area as early as 2 or 3 hours after admission. Immediate aggressive intravenous rehydration results in a rapid improvement in metabolic acidosis that causes vomiting to cease, and permits early transfer of the patient from their bed to a bench. Here, the intensity of intravenous fluid administration is reduced and the oral rehydration phase is commenced.
Designated healthcare workers prepare ORS and provide each patient with a jug containing one liter of solution. The jug is refilled every hour, and the patient commits to drinking its entire contents for as long as they remain in the unit. Family members are encouraged to sit alongside the patient and to assist with supervision of fluid ingestion. This reduces the burden of healthcare staff, ensuring that patients are under constant observation such that healthcare workers can be immediately alerted to any alteration in their clinical condition while focusing their attention on monitoring unaccompanied patients more closely. Provision of a wall clock helps to ensure that the patients, relatives, and healthcare worker can honor their commitments. In this system, the patient does not return to their bed unless excessive quantities of fluid are lost in their stool exceeding their capacity for ORS ingestion and leading once more to severe dehydration.
This strategy is safe, as it is not possible to fluid overload patients through oral rehydration, and consequently fluid balance monitoring does not need to be as meticulous as during intravenous hydration. Moreover, just one healthcare worker can supervise the oral rehydration of five to 10 patients simultaneously. Antibiotic therapy can be given as soon as oral intake is safe.
Design of the cholera treatment unit (CTU).
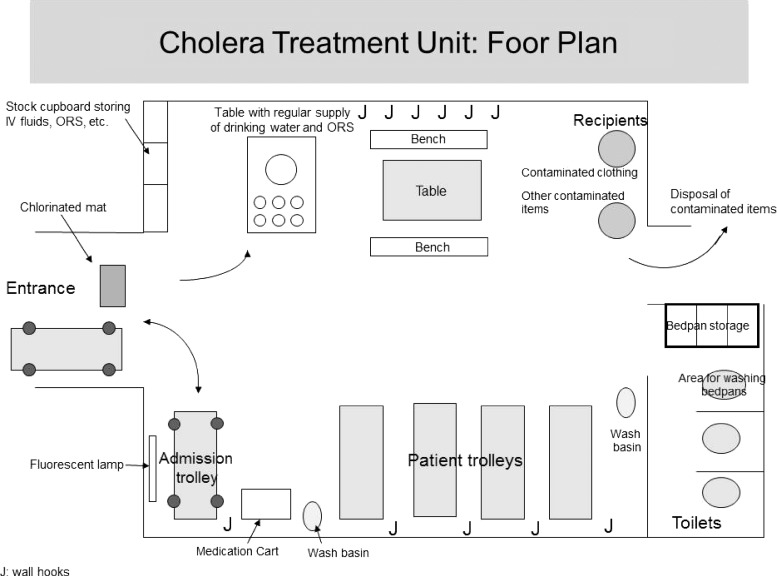
Patients presenting with moderate or severe dehydration require an immediate response and continuous observation, and good medical management can result in rapid recovery and discharge of these patients within 12 hours or less. The CTU is staffed 24 hours a day and functions as a critical care unit. Optimal outcomes are favored by efficient organization and logical layout. The floor plan of the CTU at SITE-H2M is shown in Figure 1. Key features of a carefully planned unit include a location that is easily accessible and a design that enables critically ill patients to be rapidly received and treatment promptly initiated. A stretcher is stored adjacent to the doorway, and patients receive immediate attention on an admissions trolley in a well-lighted area close to the entrance, which facilitates rapid intravenous catheterization. Adjacent to this is an area dedicated to intravenous rehydration, where standard trolleys are used rather than cholera cots, and health personnel provide patients with bedpans as required. Once this phase is completed, patients are transferred to a separate oral rehydration area where they are seated on benches to allow large numbers to be attended. Patients are moved through the unit as their management proceeds. The close proximity of the different areas eases the transition of the patient from lying to sitting, and in cases where further intravenous rehydration is required moving the patient back to the intravenous rehydration area is easily achieved. Equipment such as intravenous fluids, oral rehydration solution, and clean bedpans are stored close to where they are needed. Likewise, washing areas are kept separate from areas for disposal of contaminated items with unidirectional flow of these items to avoid contamination.
Figure 1.
Cholera Treatment Unit: floor plan.
The size of the CTU varies according to the number of patients admitted per day. From experience, a minimum of 6 to 7 trolleys and 2 to 3 toilets or latrines are required per 60 admissions per day. As mentioned previously, during the first 2 hours healthcare staff should provide patients with bedpans as required. Most patients are subsequently able to mobilize independently to the toilets, reducing the burden on staff for assistance with toileting. Relatives may assist the patient during the oral rehydration phase; this can boost ingestion of liquids and also provides a good opportunity to train relatives in the administration of ORS at home. Very few patients require hospitalization in other areas of the hospital, and when this occurs it is usually a result of decompensation of or further complications resulting from pre-existing comorbidities.
Patients are discharged once the following criteria are met: tolerance of oral ingestion of fluids; one or no bowel motions in 2 hours; and a suitable social environment permitting a safe discharge from hospital. The patient is provided with ORS sachets and instructed to consume one glass of solution for every liquid stool passed, until diarrhea ceases. If the frequency or volume of diarrhea increases or vomiting starts, they are asked to return to the hospital for further inpatient management. Rates of return to hospital following discharge are estimated at < 3%.
Discussion
The three key elements of this proposed system are directed toward the same goal: to prioritize early oral rehydration in patients who present with severe dehydration. International guidelines in cholera management recommend initial intravenous rehydration of severely dehydrated patients with 30 mL/kg Ringer's lactate solution (or, if not available, normal saline) as rapidly as possible, followed by 70 mL/kg over 2½ hrs, after which the patient should be assessed and this regimen repeated if necessary. The ORS at 5 mL/kg/hour is recommended as soon as the patient can drink, in addition to IV fluid (WHO, 1993 no. 807). Although these guidelines do mention the importance of early oral hydration, it is not afforded the same emphasis as intravenous fluids in patients with severe dehydration. In the proposed system, oral rehydration is considered as important as intravenous rehydration in the integral management of such patients. It leads to rapid physiological compensation permitting prompt patient discharge, which is of foremost importance in an epidemic setting.
This system takes into consideration factors that have been associated with complications and in-hospital death rates during cholera epidemics.10–12 These factors can be summarized as follows: 1) organization of health services to best respond to high demand (including organization of the CTU); 2) provision of staff training mainly in the administration of large volumes of IV fluids in the immediate rehydration of patients with severe dehydration; 3) adequate maintenance of hydration after initial replacement of the fluid deficit.
The major difficulty encountered in this system is that it requires patients who feel unwell to get out of bed as soon as possible. Such patients may also have a considerable sleep deficit caused by their diarrhea, which can increase their reluctance to sit up and drink. Nevertheless, in the management of cholera, the provision of aggressive oral rehydration is beneficial such that it justifies the patient's effort, and incorporating this as part of a standard protocol makes it easier to implement. This can be compared with current evidence-based surgical practice in which early post-operative mobilization is sought to minimize complications. The use of oral rehydration in a seated patient avoids fluid overload and aspiration pneumonias, and yields a more favorable hydro-electrolyte balance than intravenous rehydration, reducing clinical complications resulting from electrolyte imbalances. It also reduces consumption of intravenous fluids, occupation of hospital beds, and optimizes use of human resources, thus minimizing overall costs.
In a busy setting, the historical focus of cholera management on measurement of stool output and calculation of fluid balance frequently results in overall poor intravenous fluid administration and neglect of oral rehydration. The proposed system applies a symptomatic approach to patient management, using straight forward rehydration protocols rather than complex mathematics to guide fluid administration. This approach is safer, as errors in calculation leading to incorrect and potentially dangerous intravenous fluid administration are avoided. The removal of routine use of fluid balance calculations for the management of the vast majority of patients also reduces the demands on healthcare workers' time. Staff is therefore able to concentrate their efforts on close monitoring of fluid status for those patients who require it, including frail patients and those with cardiovascular and other co-morbidities.
In addition, in an epidemic where patient turnover is high and human resources scarce, the use of cholera cots has created inefficiency in patient care. The use of standard trolleys without holes combined with the structural and organizational changes described lead to significant improvements in efficiency of the unit, such that approximately double the number of patients usually managed using the same human and physical resources can be treated. This can have a significant positive impact during an epidemic.13 Thus, the incorporation of these measures into future guidelines for the management of cholera outbreaks is recommended for consideration.14–16
The lower case fatality rate resulting from the Peruvian than the Haitian epidemic is likely to have been caused by a number of factors. Differences between the health systems in the two countries could have contributed to this difference, as although both settings are resource-poor, Peruvian health services in the 1990s were relatively well organized and stable. In contrast, the Haitian epidemic occurred in the aftermath of a natural disaster that caused significant damage to infrastructure, on a background of weak health, sanitation and water systems, and high rates of malnutrition. Moreover, the hybrid El Tor cholera strain implicit in the Haitian epidemic was found to be particularly virulent8; in such vulnerable circumstances it is all the more important to ensure that services are set up as rapidly and efficiently as possible.
The proposed system offers an improvement in provision of care using standard, readily available equipment and is thus affordable in resource-poor settings. This system was not applied from the onset of the Peruvian epidemic. Rather, it emerged during a process of continuous evaluation by the medical community in Lima during the first year of the epidemic, and was then expanded to the greater part of the country over the following 2 years. Mortality rates observed during this epidemic were low. There is no doubt that cholera outbreaks will continue to occur, especially in settings with limited resources, but if an otherwise healthy patient with cholera arrives at a health service alive, provision of simple measures should always result in their complete recovery. This applies even in challenging settings, such as the ongoing epidemic affecting parts of the Caribbean region or outbreaks in refugee camps. Careful organization of services can result in optimal use of limited resources and, ultimately, good clinical outcomes.
Disclaimers: The views expressed in this manuscript are personal and do not necessarily reflect the official policy or position of Institutions to which we belong.
Footnotes
Financial support: Self-financed.
Authors' addresses: Eduardo Ticona and Jaime Soria, Hospital Nacional Dos De Mayo, Infectious Diseases, Lima, Peru, E-mail: eticonacrg@gmail.com and jaime9504@yahoo.es. Daniela E. Kirwan, St. George?s University, Departments of Infectious Diseases and Medical Microbiology, London, UK, E-mail: dannikirwan@yahoo.com. Robert H. Gilman, Johns Hopkins University, Department of International Health, Baltimore, MD, E-mail: gilmanbob@gmail.com.
References
- 1.Sack DA, Sack RB, Chaignat CL. Getting serious about cholera. N Engl J Med. 2006;355:649–651. doi: 10.1056/NEJMp068144. [DOI] [PubMed] [Google Scholar]
- 2.Seas C, Gotuzzo E. Churchill and Livingstone . Vibrio cholera. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Philadelphia, PA: Elsevier; 2009. pp. 2777–2791. [Google Scholar]
- 3.WHO . Cholera: the prototype “global” disease. In: Hourfar MK, et al., editors. Communicable Diseases 2002: Global Defense against the Infectious Diseases Threat. Geneva: World Health Organization; 2003. pp. 74–75. [Google Scholar]
- 4.Chin, CS, Sorenson J, Harris JB, Robins WP, Charles RC, Jean-Charles RR, Bullard J, Webster DR, Kasarskis A, Peluso P, Paxinos EE, Yamaichi Y, Calderwood SB, Mekalanos JJ, Schadt EE, Waldor MK. The origin of the Haitian cholera outbreakstrain. N Engl J Med. 2011;364:33–42. doi: 10.1056/NEJMoa1012928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eberhart-Phillips J, Besser RE, Tormey MP, Koo D, Feikin D, Araneta MR, Wells J, Kilman L, Rutherford GW, Griffin PM, Baron R, Mascola L. An outbreak of cholera from food served on an international aircraft. Epidemiol Infect. 1996;116:9–13. doi: 10.1017/s0950268800058891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . Oral Rehydration Salts to Reduce Mortality from Cholera. Geneva: World Health Organization; 2010. [Google Scholar]
- 7.Bahamonde Harvez C, Ávila VS. La epidemia de cólera en América Latina: reemergencia y morbimortalidad. Rev Panam Salud Publica. 2013;33:40–46. doi: 10.1590/s1020-49892013000100006. [DOI] [PubMed] [Google Scholar]
- 8.Barzilay EJ, Schaad N, Magloire R, Mung KS, Boncy J, Dahourou GA, Mintz ED, Steenland MW, Vertefeuille JF, Tappero JW. Cholera surveillance during the Haiti epidemic: the first 2 years. N Engl J Med. 2013;368:599–609. doi: 10.1056/NEJMoa1204927. [DOI] [PubMed] [Google Scholar]
- 9.Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet. 2004;363:223–233. doi: 10.1016/s0140-6736(03)15328-7. [DOI] [PubMed] [Google Scholar]
- 10.Guevart E, Noeske J, Solle J, Essomba JM, Edjenguele M, Bita A, Mouangue A, Manga B. Factors contributing to endemic cholera in Douala, Cameroon. Med Trop. 2006;66:283–291. [PubMed] [Google Scholar]
- 11.Piarroux R. Management of a cholera epidemic by a humanitarian organization. Med Trop. 2002;62:361–367. [PubMed] [Google Scholar]
- 12.Gotuzzo E, Cieza J, Estremadoyro L, Seas C. Cholera. Lessons from the epidemic in Peru. Infect Dis Clin North Am. 1994;8:183–205. [PubMed] [Google Scholar]
- 13.Kakar F, Ahmadzai AH, Habib N, Taqdeer A, Hartman AF. A successful response to an outbreak of cholera in Afghanistan. Trop Doct. 2008;38:17–20. doi: 10.1258/td.2006.006336. [DOI] [PubMed] [Google Scholar]
- 14.Bauernfeind A, Croisier A, Fesselet J-F, Herp M, Le Saoût E, Mc Cluskey J, Welmoet Tuynman W. In: Cholera Guidelines. Blok L, Henkens M, Thomas E, editors. Paris, France: Medecins Sans Frontieres; 2004. [Google Scholar]
- 15.Global Task Force on Cholera Control . Cholera Outbreak: Assessing the Outbreak Response and Improving Preparedness. Geneva: World Health Organization; 2010. [Google Scholar]
- 16.WHO . Guidelines for Cholera Control. Geneva: World Health Organization; 1993. [Google Scholar]