Abstract
We measured the effectiveness of a human immunodeficiency virus (HIV) prevention program developed in Kenya and carried out among university students. A total of 182 student volunteers were randomized into an intervention group who received a 32-hour training course as HIV prevention peer educators and a control group who received no training. Repeated measures assessed HIV-related attitudes, intentions, knowledge, and behaviors four times over six months. Data were analyzed by using linear mixed models to compare the rate of change on 13 dependent variables that examined sexual risk behavior. Based on multi-level models, the slope coefficients for four variables showed reliable change in the hoped for direction: abstinence from oral, vaginal, or anal sex in the last two months, condom attitudes, HIV testing, and refusal skill. The intervention demonstrated evidence of non-zero slope coefficients in the hoped for direction on 12 of 13 dependent variables. The intervention reduced sexual risk behavior.
Globally, numerous human immunodeficiency virus (HIV) prevention interventions have targeted youth of differing ethnicity, race, and nationality living in geographically and culturally diverse settings. However, only 18 of 83 evaluated in a recent review of intervention studies were conducted in developing countries.1 Additional and more rigorous studies in developing countries are badly needed, especially in sub-Saharan Africa, where the burden of disease from HIV is the greatest and where the population 15–24 years of age is increasing.2 Prevention programs in developing countries often have added challenges because they frequently function under significant resource constraints and uncertain political environments, making program implementation and rigorous examination of program impact difficult.
These challenges, combined with the costs of doing research, have appropriately fueled the demand for dissemination of evidenced-based programs (DEBIs). The problems in Africa, however, are that these DEBIs frequently were developed in the west and require adaptation to the specific context. Whether these interventions maintain their impact after the required adaptations is uncertain until tested.3,4
Effectiveness trials of indigenously developed HIV prevention programs that use best practices in HIV prevention have the advantage of being contextually appropriate without adaptation. Some of the indigenous programs have already addressed implementation issues that are common in resource-limited environments; issues that frequently pose a challenge to DEBIs trials. However, these indigenously developed HIV prevention programs often lack sound methodologically examination of their impact. Commonly this is caused by lack of capacity and skills necessary to conduct such research or limited funding that is directed exclusively at delivering program.5,6
This report presents results of a longitudinal randomized controlled effectiveness trial of a Kenyan HIV prevention program developed by Kenyans and delivered to Kenyan youth during a time of political turmoil.7 The hypothesis was that the intervention would positively affect sexual risk behaviors.
I Choose Life-Africa (ICL) staff developed a peer educator training intervention for university students, beginning with the University of Nairobi. The curriculum emphasized risk elimination and incorporated a range of risk reduction strategies based on the ABC (abstinence from sexual activity, being faithful to a single partner, and correct and consistent condom use) approach to preventing the sexual transmission of HIV.8
A randomized, controlled, longitudinal trial was conducted among 182 Kenyan University students at Egerton University at the same time that the peer educator intervention was introduced to that institution. Egerton University is located in the Rift Valley, approximately a 40-minute drive from Nakuru, the fourth largest city in Kenya. Students at Egerton University were placed there based on national entrance examinations conducted by the Joint Admissions Board, a national body supervising university admission countrywide. Student preference as to courses of study or location of university played a minimal role in placement, thus ensuring the student body at Egerton University was representative of the national university student population. Recruitment was campus wide, and all first- and second-year students were eligible to participate. Participants received cell phone credit sufficient to send 25 text messages in return for their participation in the survey.
Because of overwhelming interest in participation (training was viewed as advantageous for job placement), students were required to fill out an application. All who filled out the application were invited to an information session describing the study and were informed that if selected for the control group they would have priority entrance to the next training. Randomization occurred at the individual level after obtaining written informed consent and Institutional Review Board approval from the University of Arizona and Egerton University.
Ninety-five students formed the study group and 87 students formed the control group. The 95 students in the intervention received the 32-hour peer education training intervention from ICL staff and became actively involved in working with their peers. Control group participants, as part of the university student body, could have been exposed to ICL peer educators and their material during the follow-up period but did not receive the intensive 32-hour intervention during the study period. The 32-hour intervention was designed for an eight-week delivery, but when political unrest after national elections delayed university opening by 10 weeks, a compressed time frame for delivery and follow-up was necessary. The intervention was presented in four weeks, and the follow-up time frame was reduced to six months.
All study participants were given a paper and pencil survey with measures of sexual attitudes, knowledge, and behavior at pretest, and at two-month intervals for the six-month follow-up period. Responses of persons were linked by using confidential unique identifier numbers.
Data were analyzed by using linear mixed models or generalized linear models to compare the rate of change (slope and intercept) for 13 dependent variables that examined sexual risk behavior. Statistical models were developed for each of the dependent variables to determine whether 1) the intervention had explanatory power on its own; and 2) the intervention added explanatory power to the three independent explanatory (observed) variables (sex, rural upbringing, sexual experience at pretest) in the full model (fit statistics for each model are available on request).
The intervention group was 54% female, 49% reported rural upbringing, 75% reported being sexually experienced, and 5% report being married. The control group was 48% female, 54% reported rural upbringing, 70% reported being sexually experienced, and 4% reported being married. Previous HIV testing was reported by 53% of intervention and 48% of control group participants. Of those who reported being sexually active in the past, 5% of intervention and 5% of control group participants reported use of alcohol or drugs the last time they had sex. Thus, the two groups were similar and reflect the integrity of the randomization process.
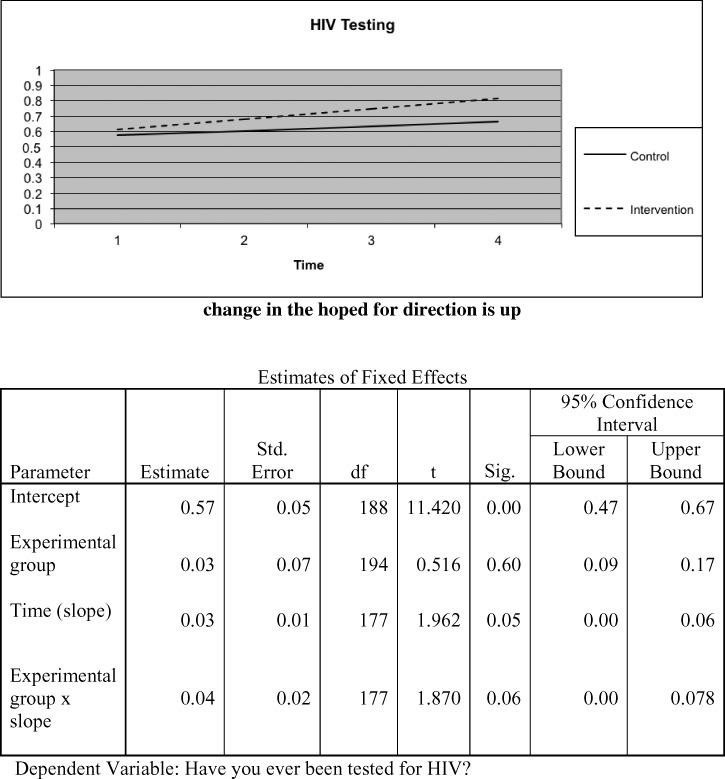
Non-zero slope coefficients in the expected direction were found for 12 of 13 dependent variables. Statistically reliable change was seen for four variables (abstinence from oral, vaginal, or anal sex in the last two months, condom attitudes, HIV testing, and refusal skills) (Figures 1 and 2). Change was identified in the variable; unprotected acts of sex in the last two months but not in the expected direction. The dependent variables beliefs, intentions to use condoms or birth control, intentions to have sex in the future, knowledge, relationship attitudes, risk assessment, stigma, and number of sexual partners in the last two months changed in the expected direction, but not to a level that can be considered statistically reliable with the small sample available. There was no evidence that the intervention influenced students who were abstinent to become sexually active.
Figure 1.
History of previous human immunodeficiency virus (HIV) testing, Kenya. Std. = standard; df = degrees of freedom; Sig. = significance.
Figure 2.
Abstinence from oral, vaginal, or anal sex in the last two months, Kenya. Std. = standard; df = degrees of freedom; Sig. = significance.
Intervention participants subsequently promoted HIV prevention messages to more than 7,800 persons, distributed more than 4,000 condoms, and referred 268 persons for HIV testing on the campus and surrounding community.
This randomized controlled trial demonstrated effectiveness of the intervention in reducing sexual risk behavior in a population in whom most persons were sexually experienced. The changes demonstrated are small, which is the norm, given the resistant nature of the behavior we are attempting to impact. It is probable that an increased sample size would have resulted in demonstration of reliable change on additional indicators for which changes in slope in the desired direction were identified. Change in the variable unprotected acts of sex in the last two months was not in the expected direction. This variable had a Poisson distribution, and one or two persons at each time period appeared to skew the distribution tail.
This study has several potential limitations. Using a delayed treatment group for a control posed a possible selection biases that could reduce differences between the intervention and control group. Reliable and valid tools for measurement are considered essential in measuring behavior change. Psychometric properties of measures used to evaluate interventions, however, are not widely published and no gold standards exist. The pretest itself may have become an unintended intervention. The act of measurement is known to be intrusive and potentially instructive. However, these limitations would tend to minimize potential differences between the intervention and control group. In spite of these limitations, evidence of effect was demonstrated.
In addition, this trial has demonstrated that rigorous studies can be conducted in developing countries during times of political instability, with limited resources, using small samples, a minimal number of trained researchers (one), part time trainers from ICL (two), and inexperienced volunteer research staff.
ACKNOWLEDGMENTS
I thank Mike Mutungi (Executive Director of I Choose Life-Africa), Enid Kaabunga (ICL Monitoring and Evaluation Coordinator), Bernard Barasa and Gladys Mulili (Rift Valley Province ICL staff), the students and administration of Egerton University, and Dr. Lee Sechrest for their outstanding contributions to this project.
Footnotes
Fianncial support: This study was supported in part by funding from the U.S. Agency for International Development via Family Health International to I Choose Life-Africa, which supported the peer education training program at Egerton University, and by a Fulbright Scholar Africa Regional Research Award that supported the author in Kenya.
Author's address: Mary B. Adam, Newborn Community Health Project, AIC Kijabe Hospital, Kijabe, Kenya, E-mail: mary.b.adam@gmail.com.
References
- 1.Kirby D, Obasi A, Laris BA. The effectiveness of sex education and HIV education interventions in schools in developing countries. World Health Organ Tech Rep Ser. 2006;938:103–150. [PubMed] [Google Scholar]
- 2.Eke A, Peersman G, Semaan S, Hylton K, Kiiti N, Sweat M. Acquisition and review of non-U.S.-based HIV risk reduction intervention studies. J Acquir Immune Defic Syndr. 2002;30((Suppl 1)):S51– S55. [PubMed] [Google Scholar]
- 3.Eke AN, Neumann MS, Wilkes AL, Jones PL. Preparing effective behavioral interventions to be used by prevention providers: the role of researchers during HIV Prevention Research Trials. AIDS Educ Prev. 2006;18:44–58. doi: 10.1521/aeap.2006.18.supp.44. [DOI] [PubMed] [Google Scholar]
- 4.McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, Gelaude D, Carey JW. ADAPT Team Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18:59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 5.Kigotho W. Kenyan higher education comes to a halt as post-election violence continues. The Chronicle of Higher Education. 2008. https://chronicle.com/article/Kenyan-Higher-Education-Comes/114399/ Available at.
- 6.Flores SA, Crepaz N. for the HIV Prevention Research Synthesis Team Quality of study methods in individual- and group-level HIV intervention research: critical reporting elements. AIDS Educ Prev. 2004;16:341–352. doi: 10.1521/aeap.16.4.341.40396. [DOI] [PubMed] [Google Scholar]
- 7.Painter TM, Ngalame PM, Lucas B, Lauby JL, Herbst JH. Strategies used by community-based organizations to evaluate their locally developed HIV prevention interventions: lessons learned from the CDC's innovative interventions project. AIDS Educ Prev. 2010;22:387–401. doi: 10.1521/aeap.2010.22.5.387. [DOI] [PubMed] [Google Scholar]
- 8.Stoneburner RL, Low-Beer D. Population-level HIV declines and behavioral risk avoidance in Uganda. Science. 2004;304:714–718. doi: 10.1126/science.1093166. [DOI] [PubMed] [Google Scholar]