Abstract
The lumbrical muscles of the hand originate from the flexor digitorum profundus tendons and insert onto the lateral band of the extensor tendons. Owing to these movable attachments, the function of this muscle is difficult to visualize. To better determine the function of this muscle, we took a novel approach by considering its relative anatomy, biomechanical characteristics, and evolution. With the smallest physiological cross-sectional area in the upper extremity, the lumbrical muscles have weak motor function, which is only 1/10 of the interosseous muscle. Because it is spindle-rich, the lumbrical muscles play an important role in the sensory feedback of the distal interphalangeal, proximal interphalangeal and metacarpalphalangeal joints of the fingers. The first two lumbrical muscles have lower variation in anatomy and higher density of muscle spindles compared to the ulnar two lumbricals. Additionally, the index and long finger lumbrical muscles are innervated by the median nerve, which also innervates the thenar muscles of the thumb. Therefore, it is possible that the first two lumbricals are functionally more important than the two ulnar lumbricals, specifically for precision pinch movements.
Keywords: Intrinsic hand muscles, Lumbrical muscle, Muscle spindles
Introduction
The lumbrical muscles of the hand are intrinsic muscles, meaning that they both originate and insert within the hand. The lumbrical muscles arise from the flexor digitorum profundus (FDP) and insert into the lateral band of the extensor tendon mechanism. Named after the Latin word “lumbricus” meaning earthworm, these muscles are thin and elongated. The lumbricals are unique because although most muscles originate and insert onto bones, the lumbrical muscles both originate and insert onto tendons, giving the lumbricals moveable attachments. This distinctive feature makes determining the function of this muscle very difficult, because the utility of the lumbricals depends upon the activity of the common extensor tendon and the position of the finger joints.
Multiple studies have been conducted to test the function of the lumbrical muscles acting on the hand, mainly for the metacarpalphalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints. (1–4) These studies included electromyography, electrical stimulation studies, as well as biomechanical studies on cadaver hands. Collectively, these studies show that the lumbrical muscles are involved in PIP and DIP joint extension, and may contribute slightly to MCP joint flexion.
Besides humans, the lumbrical muscles can be found in animals including primates and most non-primate mammals. Specifically, these muscles have been studied in various primates, rats, horses, dogs and cats. (5–8) In these species, the lumbrical muscles play an important role in locomotion. (7) For example, chimpanzees move across the ground by walking on the distal surface of the middle phalanx (called knuckle walking). The interosseous and lumbrical muscles provide resistance to flexion of the PIP joint during this motion. (9) In order to better understanding the function of lumbricals in humans, it is critical to consider the evolution and function of these muscles in other animals, particularly regarding the role of the lumbrical muscles in sensory feedback and fine movement coordination.
Despite the uniqueness of these muscles, surgeons have largely ignored the function of the lumbricals in humans, and some have even suggested using the lumbrical as a muscle flap for coverage of defects. (10) Before dismissing this muscle as unimportant, it is necessary to investigate the function of these muscles and their importance for function of the human hand. We took a new perspective on these muscles by reviewing their anatomy, biomechanics, and evolution to investigate the significance of the lumbrical muscles in humans.
Relative Anatomy
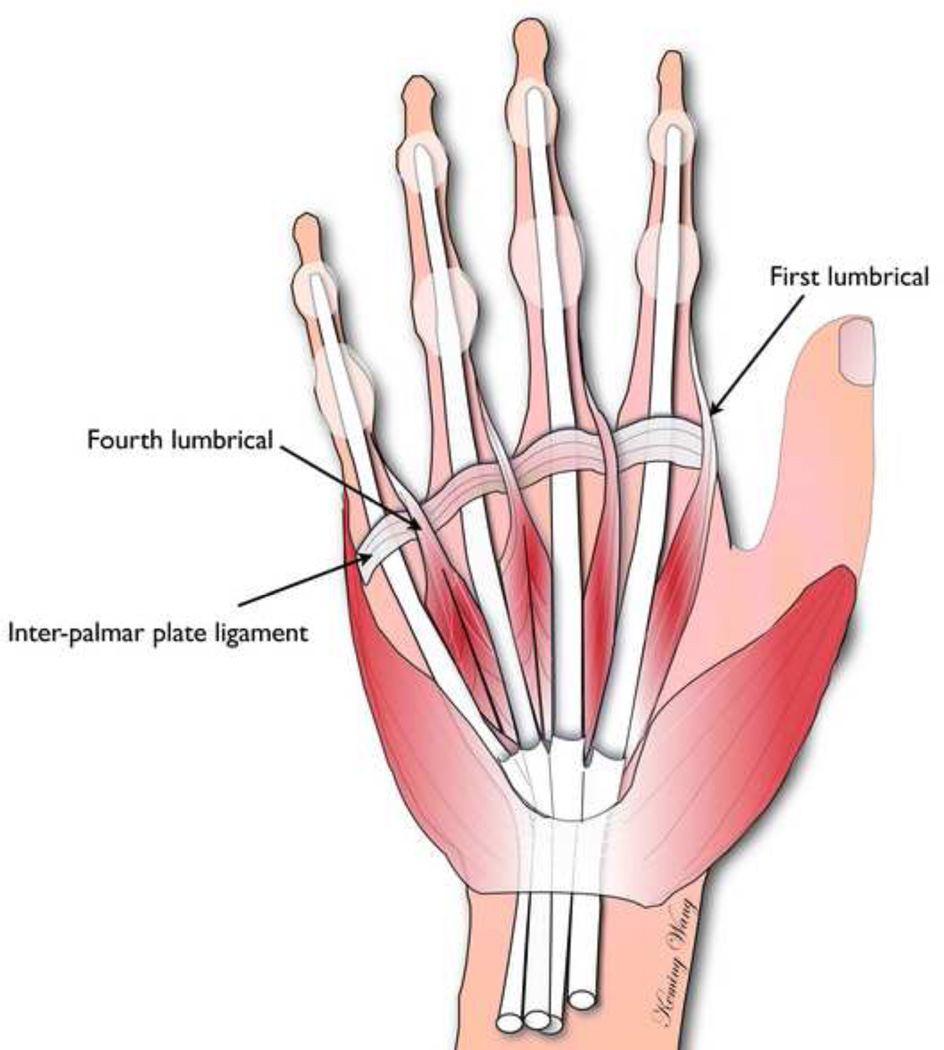
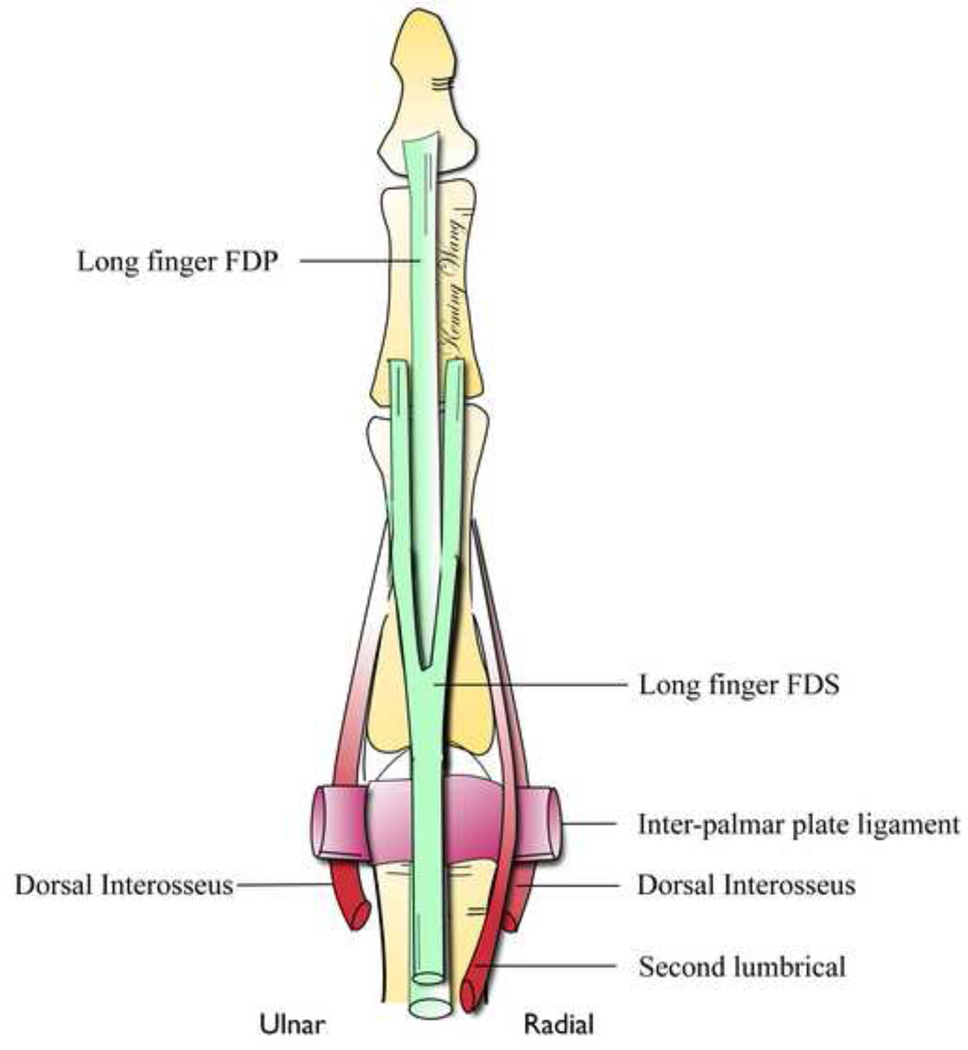
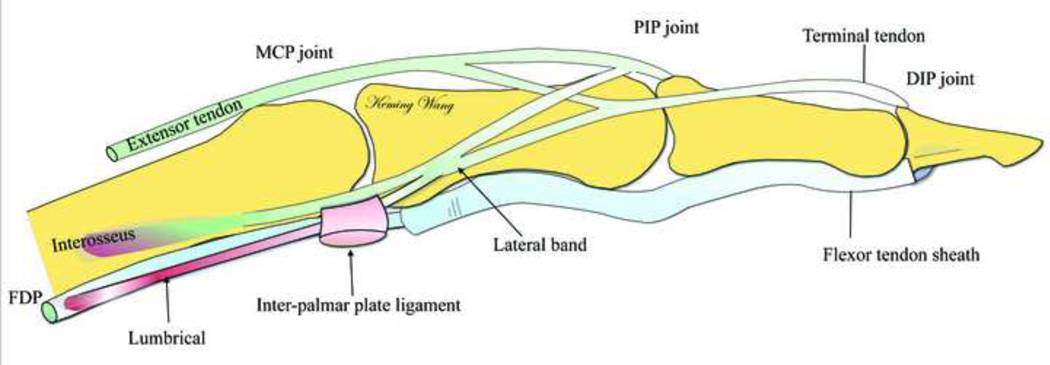
According to standard anatomy textbooks, the index and long finger lumbricals are unipennate muscles originating from the radial side of flexor digitorum profundus (FDP) tendon (Fig. 1). (11,12) The ring and small finger lumbrical muscles arise from bipennate muscle bellies on the adjacent surfaces of the FDP tendons, pass volar to the inter-palmar plate ligament, and distally insert into the radial side of the lateral band of the extensor tendon (Figs. 2, 3). (13) From origin to insertion, the lumbricals pass volar to dorsal (Fig. 4). Similar to the FDP muscles, the nerve supply of the four lumbrical muscles is from two sources. The index and long finger lumbricals are innervated by the median nerve, whereas the ring and small finger lumbricals are innervated by the deep division of the ulnar nerve. The origins and insertions of the lumbrical muscles vary considerably between individuals. The majority of individuals slightly deviate from the textbook anatomy. For example, individuals have been found to have unipennate third and/or fourth lumbricals. Individuals have also been found to have deviations in the origins and insertions of the lumbrical muscles. (14) In a study of 75 cadaveric hands, Mehta and Gardner found that the first and second lumbrical muscles had the most constant anatomy. The first lumbrical adhered to the textbook anatomy in 82.7% of hands, and the second lumbrical adhered to the textbook anatomy in 68% of hands. The third and fourth lumbricals had more variation in their anatomy, as the third lumbrical adhered to the textbook anatomy in only 45.3% of hands and the fourth adhered to the textbook anatomy in 60% of hands. In addition, the fourth lumbrical was the most frequently absent (5.3% of hands). (15)
Figure 1.
Palmar View Showing the Origins of the Lumbricals.
Figure 2.
Palmar View of a Left Cadaver Hand. 2, second lumbrical; 3, third lumbrical; 4, fourth lumbrical. (Adapted with permission of the Journal of Hand Surgery. Eladoumikdachi F, Valkov PL, Thomas J, et al. Anatomy of the Intrinsic hand Muscles Revisited: Part II. Lumbricals. Plast Reconstr Surg. 2002;110:1225–1231.)
Figure 3.
Palmar View of the Long Finger Showing the Anatomy of the Lumbrical and Interosseous Muscles.
Figure 4.
Diagram Demonstrating A Lumbrical Originating from the Flexor Digitorum Profundus Tendon and Inserting into the Lateral Band of Extensor Tendon.
The lumbrical muscles have highly specialized architectural properties. Jacobson et al. found the lumbrical muscles have the smallest physiological cross-sectional area (PCSA) in the upper extremity, which was only 1/10 to 1/20 the PCSA of the FDP muscle. (16) They also reported that the lumbrical muscle fibers could extend 85% to 90% of the muscle length, which indicated that this muscle is designed for long excursions. (16) (Table 1) The small cross-section of the muscle along with the long fiber length has led researchers to believe that in humans these muscles are involved in quick, precision movements of the fingers. (17,18)
Table 1.
Properties of the Lumbricals and Interosseous Muscles of the Human Hand. (16)
| Muscles | Muscle mass (gm) |
Muscle length (mm) |
Fiber length (mm) |
Physical crosssectional area (cm2) |
FL/ML ratio |
|---|---|---|---|---|---|
| L1 | 0.57 ± 0.19 | 64.9 ± 10.0 | 55.4 ± 10.2 | 0.11 ± 0.03 | 0.85 ± 0.03 |
| L2 | 0.39 ± 0.22 | 61.2 ± 17.8 | 55.5 ± 17.7 | 0.08 ± 0.04 | 0.9 ± 0.05 |
| L3 | 0.37 ± 0.16 | 64.3 ± 8.9 | 56.2 ± 10.7 | 0.08 ± 0.04 | 0.87 ± 0.07 |
| L4 | 0.23 ± 0.11 | 53.8 ± 11.5 | 50.1 ± 8.4 | 0.06 ± 0.03 | 0.9 ± 0.05 |
| DI 1 | 4.67 ± 1.17 | 61.9 ± 2.5 | 31.7 ± 2.8 | 1.50 ± 0.4 | 0.51 ± 0.05 |
| DI 2 | 2.65 ± 1.01 | 62.8 ± 8.1 | 25.1 ± 6.3 | 1.34 ± 0.77 | 0.41 ± 0.13 |
| DI 3 | 2.01 ± 0.66 | 54.9 ± 4.6 | 25.8 ± 3.4 | 0.95 ± 0.45 | 0.47 ± 0.07 |
| DI 4 | 1.90 ± 0.62 | 50.1 ± 5.3 | 25.8 ± 3.4 | 0.91 ± 0.38 | 0.52 ± 0.11 |
| PI 2 | 1.56 ± 0.22 | 55.1 ± 5.0 | 25.0 ± 5.0 | 0.75 ± 0.25 | 0.45 ± 0.08 |
| PI 3 | 1.28 ± 0.28 | 48.2 ± 2.9 | 26.0 ± 4.3 | 0.65 ± 0.26 | 0.54 ± 0.08 |
| PI 4 | 1.19 ± 0.33 | 45.3 ± 5.8 | 23.6 ± 2.6 | 0.61 ± 0.23 | 0.52 ± 0.10 |
Biomechanical Studies
A number of biomechanical studies have been carried out to measure the activity of the lumbrical muscle. Backhouse and Catton conducted a study in 1954, in which the authors used needle electrodes to measure action potentials of the second lumbrical muscle. They found that the lumbrical showed activity when the PIP and DIP joints were extended, regardless of the degree of MCP joint flexion. During electrical stimulation of the lumbrical muscle, the PIP and DIP joints extended and the MCP joint flexed. (19) From these results, the authors concluded that the lumbrical muscle was involved in active extension of the PIP and DIP joints, as well as flexion of the MCP joint. In a later study, Ranney and Wells confirmed the findings of this study. They simulated the action of the lumbrical muscle in cadavers, and found that contraction of the muscle caused PIP and DIP joint extension, and MCP joint flexion. (1)
Schreuder and Stam measured the strength of the lumbrical muscles in 12 patients with complete ulnar nerve paralysis. In these patients, it is possible to measure directly the strength of the first and second lumbricals, because the interosseous muscles are innervated by the ulnar nerve and therefore paralyzed. Thus, when the MCP joint is flexed, the lumbricals are the only muscles controlling PIP and DIP joint extension. A dynamometer was used to press against the PIP joint and measure the force required to cause flexion at this joint. Schreuder and Stam found that the ulnar nerve patients lost approximately 90% of intrinsic muscle strength when compared to the opposite hand. (3) This led the authors to conclude that the lumbricals are weak extensors of the PIP joint compared to the interosseous muscles. Similarly, the weakness of the lumbrical muscles has also been proven using biomechanical testing. In a study using computer modeling and biomechanical testing in cadavers, Buford et al. found that the interosseous muscle contributes to about 22% of flexion at the MCP joint, whereas the lumbricals contribute to only 2–3%. (20)
Evolutionary considerations
In order to understand the significance of the lumbrical muscles, it is helpful to consider the evolution of these muscles. One interesting aspect of lumbrical muscle evolution involves the number of muscle spindles in the lumbrical muscles. Muscle spindles are specialized sensory receptors found richly in many human muscles that are involved in precision movements. They provide information to the central nervous system regarding the length and contraction velocity of muscle fibers. The brain uses this information to determine the position of the body part. (21) High spindle density is found in m uscles including the human extraocular muscles, the intrinsic and extrinsic muscles of the human tongue and the closing muscles of the jaw. (22) In addition, muscle spindles play important roles in the tonic fine movements of the tongue and neck. (23) In the tongue, muscle spindles can provide information important to the direction of stretching as well as the position of tongue in three dimensions. (24) In spindle-rich muscle, the latencies of unloading reflexes are shorter than in muscles with few spindles. (25) In the upper extremity, the four lumbricals have the greatest number of spindles with a total of 139 according to Winckler and Foroglou. (26)
Interestingly, the number of spindle fibers in the lumbrical muscles is much greater in mammals that are closely related to humans compared to mammals that are more distantly related. Winkler and Foroglou found that non-primate mammals such as rats, rabbits and hedgehogs had about 15 muscle spindles in their lumbrical muscles. Primates including Callithrix and the Gray Langur had higher levels of spindle fibers (Table 2). In a similar study by Voss, the number of muscle spindles in the lumbricals of chimpanzees was found to be greater than in other primates (Table 2). (27) In both studies, humans had the most spindle fibers with 136 recorded by Voss and 139 recorded by Winckler and Foroglou. Winckler and Foroglou also found that muscle spindles were even more concentrated in the first and second lumbrical muscles of humans, whereas in other mammals, the lumbricals were denser in the second and third fingers (Table 2). (26)
Table 2.
| Subjects | Lumbrical 1 | Lumbrical 2 | Lumbrical 3 | Lumbrical 4 | Total |
|---|---|---|---|---|---|
| Rat | 3 | 3 | 4 | 5 | 15 |
| Weasel | 6 | 4 | 9 | 6 | 25 |
| Cat | 5 | 6 | 12 | 4 | 27 |
| Mongoose lemur | 8 | 10 | 12 | 8 | 38 |
| Callithrix | 12 | 20 | 19 | 13 | 64 |
| Gray Langur | 15 | 22 | 15 | 13 | 65 |
| Chimpanzee | 46 | 31 | 25 | - | 112 |
| Human | 51 | 40 | 23 | 23 | 138 |
In the apes, the anatomy of the lumbrical muscle is very similar to humans, with the lumbrical originating from the FDP and inserting into the extensor expansion. (28) Compared to chimpanzees the lumbrical muscles in humans have become relatively smaller. In a study comparing the anatomy of the intrinsic muscles of Chimpanzees to that of humans, Tuttle found that the second lumbrical was 2.5 percent of the weight of the chimp hand, whereas it was only 1.3 percent of the weight of the human hand. (29) This relationship was true for all four of the lumbrical muscles. This decrease in relative size of the muscles shows a decrease in the strength of the lumbrical muscle from primates to humans.
Implications for the function of the lumbricals
It is evident that the lumbrical muscle has some, albeit limited, motor function. Biomechanical studies have shown that this muscle primarily functions to extend the PIP and DIP joints. However, the interosseous muscle seems to be much more important for this movement. The interosseous muscles have considerably larger cross-sectional areas than the lumbrical muscles. (Table 1) Moreover, the work in ulnar paralysis patients by Schreuder and Stam suggests that the interosseous muscles are much more important for PIP and DIP joint extension. Evidence also suggests that the lumbrical muscle may be involved in flexion at the MCP joint. However, this function of the lumbrical muscle is very limited. Buford et al. found that the lumbrical contributed to only 2% of MCP joint flexion. The small cross-sectional area of the lumbrical (the lowest in the upper extremity) and the limited strength of this muscle suggest that motor function may not be its most important function.
Although the lumbrical is relatively weak, evidence suggests that the sensory function of this muscle may be more important than its motor function. Many authors have speculated on this muscle’s sensory function, given that it originates from a flexor tendon and inserts into an extensor tendon. This anatomy makes the lumbrical muscle a good candidate for monitoring the balance of forces between the flexors and extensors. Leijnse and Kalkker speculated that the lumbricals could play an important role in proprioceptive feedback at the PIP and DIP joints, because small changes in the flexion of the PIP and DIP joints correspond with large lumbrical displacements. In addition, they speculated that isometric contraction of the lumbrical muscle could be helpful to stabilize the DIP and PIP joints while flexing or extending at the MCP joint. (17) In fact, patients that have carpal tunnel syndrome perform poorly on tests measuring precision pinch performance. This may result from compression of the median nerve leading to impairment of first and second lumbrical function. (30)
Physiological characteristics including the PCSA and number of muscle spindles suggest a sensory function. Despite the fact that this muscle has the smallest cross-sectional area in the upper extremity, it has the greatest number of muscle spindles, which are responsible for gathering proprioceptive input. This idea of a proprioceptive organ has been proposed by other authors. Peck et al. conducted a study in 1984 of what they called “parallel muscle combinations.” These were described as pairs of muscles consisting of one small muscle acting across a joint in parallel with a vastly larger muscle. They found that the smaller muscles tended to have higher densities of spindle fibers than the larger muscles. (31) For example, they found that the abductor pollicis brevis had a much higher density of spindle fibers than the abductor pollicis longus. The authors suggested that the small muscles acted as kinesiological monitors of movement of the muscles. Concerning the lumbrical muscle, this would also make sense, because the lumbricals may act as kinesiological monitors for the larger, stronger interosseous muscles.
Evolutionary considerations also support the idea that the lumbricals may have more of a sensory role than a motor function. The decrease in the relative size of the lumbrical muscle between chimpanzees and humans suggests a decrease in strength of this muscle. The increase in the number of spindle fibers in the lumbrical muscles from non-primate mammals to primates to humans also suggests an increase in the proprioceptive ability of the lumbrical muscle. The decrease in size and increase in the number of spindle fibers could be related to the change in use of the forelimbs from primarily locomotion in non-primate mammals towards feeding in some primates, and finally to tool use and precision manipulation of objects in humans.
Specifically, the lumbrical muscle may be important in humans for forming a precision pinch. A precision pinch as described by Marzke is a grip in which a small object is held between the thumb’s distal phalanx and the terminal volar pads of one or more fingers. (32) This type of grip is typically formed using the first three digits i.e. the thumb, index, and long fingers. There are a number of characteristics of the lumbrical muscles that suggest they may be involved in the precision pinch movement. First, the lumbricals originate from the radial side of the FDP and pass on the radial side of the digits. This may be related to the articulation of the fingers with the thumb on the radial side of the hand during precision pinch movements. Second, the first and second lumbricals are innervated by the median nerve, which also innervates the thenar muscles of the thumb. This common innervation could suggest coordination between these muscles during three-digit precision pinch movements. Third, the higher consistency in the anatomy of the first and second lumbricals compared to the third and fourth suggests that lumbricals 1 and 2 may have a more important function. If the lumbricals were involved in precision pinch movements, this would explain the consistency in the anatomy of lumbricals one and two, because these lumbricals would be functionally more important than lumbricals three and four. Fourth, the distribution of spindles fibers among the lumbrical muscles also suggests an involvement in precision pinch movements because in humans spindle fibers are most dense in the first and second lumbricals. This concentration of spindle fibers may exist to better monitor the movement of the index and long fingers during precision pinch movements.
In contrast to humans, n on-primate mammals are incapable of precision pinch movements and have evenly distributed spindle fibers. Moreover, primates such as callithrix (Marmosets) and the Gray Langur are also incapable of precision pinch movements, and have more concentrated spindles in the second and third lumbrical muscles. (Table 2) These primates have very small thumbs and mainly use their hands for climbing and suspensory behavior. The concentration of muscle spindles in the second and third lumbrical muscles may reflect the importance of these digits during locomotion, whereas in humans, the first and second lumbrical muscles have high concentrations of muscle spindles in order to perform precision pinch movements.
The lumbrical muscles have been considered to be involved in MCP joint flexion and IP joint extension. However, this muscle’s small cross-sectional area and measurements of the muscle’s strength in biomechanical studies suggest that this is a relatively weak muscle. This is especially true when the lumbrical is compared to the interosseous muscle, which has a similar function but is considerably stronger. The high number of muscle spindles in the lumbricals suggests that these muscles may have an important role in proprioceptive monitoring of the fingers. Furthermore, anatomical factors and the allocation of spindle fibers among the lumbricals suggests that this muscle is more involved in sensory feedback, which is important for precision pinch movements and precise manipulation of objects.
Clinical relevance
Although the lumbrical is typically ignored by hand surgeons, it does have some clinical relevance. Specifically, the lumbrical muscle may have important implications for certain trauma injuries. For example, patients with replantation for zone III amputations (transmetacarpal amputations) typically have poor functional outcomes. (33) These amputations may have poor outcomes because of damage the lumbrical and interosseous muscles and disruption of blood flow to these structures. (34) Furthermore, for these injuries, the lumbrical and interosseous muscles are usually not repaired by surgeons. This may result in a loss of function, particularly fine motor function because of intrinsic contracture. (35) Therefore, attempts should be made to repair the lumbrical and interosseous muscles for treatment of transmetacarpal amputations.
The lumbrical muscle is also involved in the “lumbrical plus deformity.” This deformity occurs when the FDP ruptures distal to the insertion of the lumbrical muscle. When this occurs, the FDP is no longer attached to its insertion at the distal phalanx, but it is still attached to the lumbrical. Therefore, when the FDP contracts, it pulls on the lumbrical instead of the phalanx. Because the lumbrical muscle inserts on the dorsal side of the finger, the finger extends when the patient tries to flex the digit. (36) This phenomenon may also occur if an overly long tendon graft is used to repair the flexor tendon, resulting in a loose FDP tendon. (18) Management of this deformity involves release of the lumbrical muscle or placement of an appropriate length tendon graft.
The lumbrical muscle is sometimes damaged in crush injuries to the hand. Following these injuries, adhesions may occur between the lumbrical muscle and the interossous muscle. Because the lumbrical passes volar to the inter-palmar plate ligament, whereas the interossous muscle passes dorsal, adhesions distal to the inter-palmar plate ligament limit the proximal movement of the interossous and lumbrical muscles. (37) This deformity causes the patient to have intermetcarpal pain when making a fist. It can typically be treated by release of the involved muscles. The lumbrical muscles have also been shown to be relevant in carpal tunnel syndrome. In a case report of three manual workers, hypertrophic lumbrical muscles were found to cause carpal tunnel syndrome. (38)
The lumbrical has evolved into a highly specialized structure that modulates the tension between the extensor and flexor system during fine pinch that is so identified with human’s adaptability in creating tools to enrich our living environment. It is not simply a dispensable structure that serves no purpose. Rather, it is an intricate sensory organ that orchestrates precision movements, such as the smooth delicate motion of hand surgeons performing microvascular surgery or in repairing flexor tendons within a tight zone 2 sheath. The nondescript worm shape structure of the lumbrical muscle belies a mysteriously elegant structure that toils in obscurity to make our daily activities so much easier.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number K24 AR053120. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Ranney D, Wells R. Lumbrical muscle function as revealed by a new and physiological approach. Anat Rec. 1988;222:110–114. doi: 10.1002/ar.1092220116. [DOI] [PubMed] [Google Scholar]
- 2.Lauer RT, Kilgore KL, Peckham PH, et al. The function of the finger intrinsic muscles in response to electrical stimulation. IEEE Trans Rehabil Eng. 1999;7:19–26. doi: 10.1109/86.750547. [DOI] [PubMed] [Google Scholar]
- 3.Schreuders TA, Stam HJ. Strength measurements of the lumbrical muscles. J Hand Ther. 1996;9:303–305. doi: 10.1016/s0894-1130(96)80034-2. [DOI] [PubMed] [Google Scholar]
- 4.Koh S, Buford WL, Jr, Andersen CR, et al. Intrinsic muscle contribution to the metacarpophalangeal joint flexion moment of the middle, ring, and small fingers. J Hand Surg. 2006;31:1111–1117. doi: 10.1016/j.jhsa.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Sohn A, Kaidoh T, Inoue T. Three-dimensional structure of the synaptic contact of the neuromuscular junction in the rat lumbrical muscle. Arch Histol Cytol. 1999;62:237–247. doi: 10.1679/aohc.62.237. [DOI] [PubMed] [Google Scholar]
- 6.Devanandan MS, Ghosh S, John KT. A quantitative study of muscle spindles and tendon organs in some intrinsic muscles of the hand in the bonnet monkey (Macaca radiata) Anat Rec. 1983;207:263–266. doi: 10.1002/ar.1092070204. [DOI] [PubMed] [Google Scholar]
- 7.Klomkleaw W, Kasashima Y, Fuller GA, et al. Horse lumbrical muscle: possible structural and functional reorganization in regressive muscle. Anat Histol Embryol. 2002;31:85–98. doi: 10.1046/j.1439-0264.2002.00363.x. [DOI] [PubMed] [Google Scholar]
- 8.Banks RW, Emonet-Denand F. Characteristic properties of superficial lumbrical spindles in the cat hind limb, related to their bag1 fibres. J Anat. 1996;189(1):65–71. [PMC free article] [PubMed] [Google Scholar]
- 9.Tuttle RH. Knuckle-walking and the evolution of hominoid hands. Am. J Phys Anthropol. 1967;26:171–206. [Google Scholar]
- 10.Koncilia H, Kuzbari R, Worseg A, et al. The lumbrical muscle flap: anatomic study and clinical application. J Hand Surg Am. 1998;23:111–119. doi: 10.1016/S0363-5023(98)80098-1. [DOI] [PubMed] [Google Scholar]
- 11.Scheunke M, Lamperti ED, Ross LM, et al. Thieme Atlas of Anatomy : General Anatomy and Musculoskeletal System. New York, NY: Thieme; 2006. [Google Scholar]
- 12.Standring S, Gray H. Gray's Anatomy the Anatomical Basis of Clinical Practice. 40th ed. London, UK: Churchill Livingstone/Elsevier; 2008. [Google Scholar]
- 13.Eladoumikdachi F, Valkov PL, Thomas J, et al. Anatomy of the Intrinsic hand Muscles Revisited: Part II. Lumbricals. Plast Reconstr Surg. 2002;110:1225–1231. doi: 10.1097/00006534-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Basu SS, Hazary S. Variations of the lumbrical muscles of the hand. Anat Rec. 1960;136:501–504. doi: 10.1002/ar.1091360409. [DOI] [PubMed] [Google Scholar]
- 15.Mehta HJ, Gardner WU. A study of lumbrical muscles in the human hand. Am J Anat. 1961;109:227–238. doi: 10.1002/aja.1001090302. [DOI] [PubMed] [Google Scholar]
- 16.Jacobson MD, Raab R, Fazeli BM, et al. Architectural design of the human intrinsic hand muscles. J Hand Surg Am. 1992;17:804–809. doi: 10.1016/0363-5023(92)90446-v. [DOI] [PubMed] [Google Scholar]
- 17.Leijnse JN, Kalker JJ. A two-dimensional kinematic model of the lumbrical in the human finger. J Biomech. 1995;28:237–249. doi: 10.1016/0021-9290(94)00070-k. [DOI] [PubMed] [Google Scholar]
- 18.Palti R, Mordechai V. Anatomy and Function of Lumbrical Muscles. Hand Clin. 2012;28:13–17. doi: 10.1016/j.hcl.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Backhouse KM, Catton WT. An experimental study of the functions of the lumbrical muscles in the human hand. J Anat. 1954;88:133–141. [PMC free article] [PubMed] [Google Scholar]
- 20.Buford WL, Jr, Koh S, Andersen CR, et al. Analysis of intrinsic-extrinsic muscle function through interactive 3-dimensional kinematic simulation and cadaver studies. J Hand Surg. 2005;30:1267–1275. doi: 10.1016/j.jhsa.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 21.Kistemaker DA, Van Soest AJK, Wong JD, et al. Control of position and movement is simplified by combined muscle spindle and Golgi tendon organ feedback. J Neurophysiol. 2013;109:1126–1139. doi: 10.1152/jn.00751.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruskell GL. The fine structure of human extraocular muscle spindles and their potential proprioceptive capacity. J Anat. 1989;167:199–214. [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper S, Daniel PM. Muscle Spindles in Man; Their Morphology in the Lumbricals and the Deep Muscles of the Neck. Brain. 1963;86:563–586. doi: 10.1093/brain/86.3.563. [DOI] [PubMed] [Google Scholar]
- 24.Smith A. The control of orofacial movements in speech. Crit Rev Oral Biol Med. 1992;3:233–267. doi: 10.1177/10454411920030030401. [DOI] [PubMed] [Google Scholar]
- 25.Ostry DJ, Gribble PL, Levin MF, et al. Phasic and tonic stretch reflexes in muscles with few muscle spindles: human jaw-opener muscles. Exp Brain Res. 1997;116:299–308. doi: 10.1007/pl00005757. [DOI] [PubMed] [Google Scholar]
- 26.Winckler G, Foroglou C. Comparative study on the neuromuscular spindles of the lumbrical muscles in certain mammals and in man. Arch Anat Histol Embryol. 1965;48:1–17. [PubMed] [Google Scholar]
- 27.Voss H. Untersuchungen uber Zahl, Anordnung und Lange der Muskelspindeln in den Lumbrical-muskeln des Menschen und einiger Tiere. Jahrb Morfph Umikrosk Anat Abt II Zeitschr Mikrosk Anat Forsch. 1937;42:509–524. [Google Scholar]
- 28.Diogo RW. Comparative Anatomy and Phylogeny of Primate Muscles and Human Evolution. New York, NY: CRC press; 2012. Bernard. [Google Scholar]
- 29.Tuttle RH. Quantitative and functional studies on the hands of the Anthropoidea. I. The Hominoidea. J Morphol. 1969;128:309–363. doi: 10.1002/jmor.1051280304. [DOI] [PubMed] [Google Scholar]
- 30.Hsu HY, Kuo LC, Chiu HY, et al. Functional sensibility assessment. Part II: Effects of sensory improvement on precise pinch force modulation after transverse carpal tunnel release. J Orthop Res. 2009;11:1534–1539. doi: 10.1002/jor.20903. [DOI] [PubMed] [Google Scholar]
- 31.Peck D, Buxton DF, Nitz A. A comparison of Spindle Concentrations in Large and Small Muscles Acting in Parrallel Combinations. J Morphol. 1984;180:243–252. doi: 10.1002/jmor.1051800307. [DOI] [PubMed] [Google Scholar]
- 32.Marzke MW. Precision grips, hand morphology, and tools. Am J Phys Anthropol. 1997;102:91–110. doi: 10.1002/(SICI)1096-8644(199701)102:1<91::AID-AJPA8>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 33.Weinzweig N, Sharzer LA, Starker I, et al. Replantation and Revascularization at the Tranmetacarpal Level: Long-term Functional Results. J Hand Surg. 1996;21A:877–883. doi: 10.1016/S0363-5023(96)80208-5. [DOI] [PubMed] [Google Scholar]
- 34.Scheker LR, Chesher SP, Netscher DT, et al. Functional Results of Dynamic Splinting After Transmetacarpal, Wrist, and Distal Forearm Replantation. J Hand Surg. 1995;20:584–590. doi: 10.1016/s0266-7681(05)80115-9. [DOI] [PubMed] [Google Scholar]
- 35.Rui YJ, Shi HF, Mi JY, et al. Surgical Treatment of Stiff Metacarpophalangeal Joint After Hand Injury [Chinese] Zhongguo xiu fu chong jian wai ke za zhi. 2011;25:538–541. [PubMed] [Google Scholar]
- 36.Parkes A. The “Lumbrical Plus” Finger. J Bone Joint Surg. 1971;53:236–239. [PubMed] [Google Scholar]
- 37.Watson KH, Ritland DG, Chung KE. Post-Traumatic Interosseus-Lumbrical Adhesions. J Bone Joint Surgery. 1974;56A:79–84. [PubMed] [Google Scholar]
- 38.Robinson D, Aghasi M, Halperin N. The Treatment of Carpal Tunnel Syndrome Caused by Hypertrophied Lumbrical Muscles. Case Reports. Scand J Plast Reconstr Surg Hand Surg. 1989;23:149–151. doi: 10.3109/02844318909004509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.