Abstract
Background:
Lead is a pollutant with numerous adverse effects on health. Since it can affect blood pressure, peripheral blood vessels, and the heart, the present study aimed to evaluate the relation between occupational exposure to lead and blood pressure.
Materials and Methods:
This cross-sectional study included male individuals working in battery firms in Isfahan. A questionnaire covering demographic characteristics and the history of different diseases and occupational exposure to lead was completed. Each participant's blood pressure was also measured and recorded. After obtaining blood samples and determining lead levels, mean and frequency analyses were performed. In addition, Pearson's correlation test and linear regression were used to assess the relation between blood lead levels (BLLs) and systolic and diastolic blood pressure. All analyses were performed in SPSS.19
Results:
The mean age of the 182 studied workers was 42.85 ± 13.65 years. They had worked in battery firms for a mean period of 23.67 ± 14.72 years. Moreover, the mean value of BLLs among the participants was 7.92 ± 3.44 μg/dL. Correlation between BLL and systolic and diastolic blood pressure was not significant. The effects of lead on systolic and diastolic blood pressure after stepwise regression were B = –0.327 [confidence interval (CI) 95%: –0.877 to 0.223] and B = –0.094 (CI 95%: –0.495 to 0.307), respectively.
Conclusion:
This study revealed that BLLs in battery firm workers to be normal. Additionally, BLLs were not significantly related with either systolic or diastolic blood pressure which might have been the result of normal BLLs.
Keywords: Hypertension, lead, occupational exposure
INTRODUCTION
Lead salts have always existed in the Earth's crust. However, the element itself has rarely been found in human body before industrialization and therefore, its effects were not identified until then.[1] Today, lead is known as a major industrial pollutant,[1] whose levels in the nature can be increased by activities such as production and burning fossil fuels.[2] Although lead-containing gasoline and batteries are considered as most important sources of lead, the element can also be found in a variety of products including lead-containing diesel fuels, paints, ceramics, cosmetics, water pipes, agricultural equipment, hair colors, and airplanes.[3] Consuming lead-contaminated food or water, breathing lead-polluted air, or even skin contact with lead can transmit the element to human body.[4] Individuals in contact with lead in the workplace are also at risk through their contaminated clothes and equipment.[4] The effects of lead contamination may vary according to contact dose and duration, age, career, general health, and lifestyle.[5]
Recent longitudinal studies found harmful effects at levels even lower than 40 μg/dL, that is, neurological impacts of lead occure at a level of 5 μg/dL in children and 18 μg/dL in adults.[6] Some cohort studies found lead levels in workers exposed to lead to be more than 40 μg/dL.[7] Invetigations on the whole population, on the contrary, indicated blood lead concentrations of over 10 μg/dL to be related with increased atherosclorosis, cardiovascular diseases, and mortality.[8,9]
On the basis of above-mentioned facts, lead is regarded as an important pollutant of not only the Earth's surface but also specific workplaces. Although review articles and meta-analyses have shown blood lead levels (BLLs) to increase hypertension,[3,10] some Iranian studies have failed to show such a relation between BLL and systolic blood pressure[11,12] and only one study in the country could successfully establish a weak relation between BLL and diastolic blood pressure.[11] This study also evaluated occupational exposure to lead and its consequent effects on blood pressure among male battery factory workers.
MATERIALS AND METHODS
Study design and sample
This cross-sectional study was conducted in Isfahan during 2011. Overall, 200 male normotensive battery company workers (age: 25-55 years) with chronic skin exposure to lead were included. In order to select participants, a full list of all battery companies in Isfahan (Iran) was collected. Simple random sampling was then used to refer to the companies and enroll workers who consented to participate. Sampling was continued until the desired sample size was reached. Subjects with a history of diabetes mellitus, hypertension, cardiac diseases, cancer, renal disease, or those consuming medicine affecting blood pressure were excluded.
Procedures
First, the objectives of the study were explained to the subjects and written informed consents were obtained. Then, the subjects completed a questionnaire including demographics, socioeconomic and professional data, history of lead exposure (career, duration of employment, previous jobs, and exposure method), history of respiratory diseases, medicine intake, and lifestyle behaviors (smoking, daily physical activity, and diet). Then the physical examination was performed by a physician and using standardized and 0-calibrated instruments. The blood pressure was measured twice in a seated position and recorded the average of two readings for the first and fifth Korotkoff sounds as systolic and diastolic pressures, respectively. Then height was determined barefoot in standing position to the nearest 0.5 cm using a secured metal ruler, and the weight was measured with light clothing and by a calibrated scales. Body mass index (BMI) was calculated as weight divided by squared height (kg/m2). Lifestyle behaviors and anthropometric measurements were done for adjusting the model of effect of lead on blood pressure.
In order to assess BLL, venous blood samples were obtained from all subjects and kept in heparinized lead-free tubes at 4°C. All tests were conducted simultaneously in the morning. A flameless atomic absorption spectrophotometer was used to determine lead levels. The participants were divided into two groups of BLL < 10 μg/dL and BLL ≥ 10 μg/dL.
Statistical analysis
Mean and frequency analyses were first used to evaluate the indices among the whole population. Then, chi-square and student's t-tests were performed to compare the BLLs and other indices between the two groups. The effects of lead on systolic and diastolic blood pressure were assessed by stepwise linear regression and Pearson's correlation test. All analyses were conducted in SPSS19 with a significance level of P < 0.05.
RESULTS
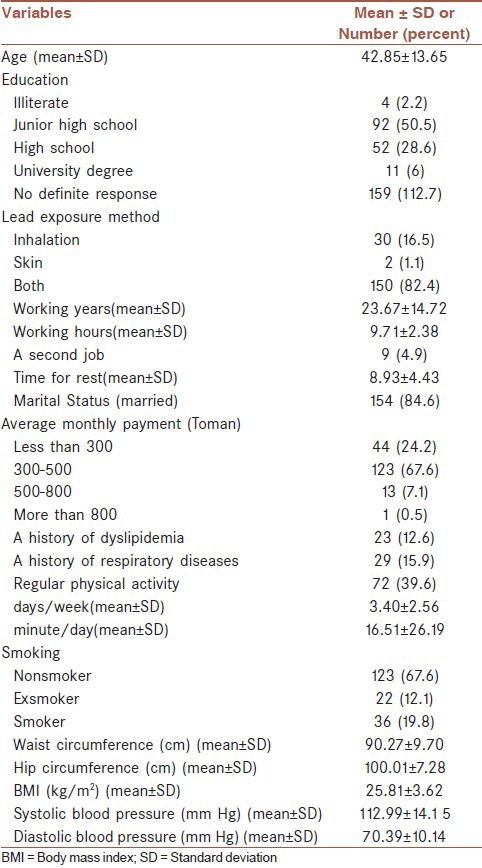
From 200 invited subjects, a total number of 182 battery company workers in Isfahan were evaluated in this study. The mean age of the participants was 42.85 ± 13.65 years and they had worked in battery companies for an average of 23.67 ± 14.72 years. Table 1 shows demographic characteristics, lifestyle, disease history, lead-exposure history, anthropometric measurements, and blood pressure of the studied population. As it is seen, only 6% of the participants held a university degree. Moreover, 82.4% were exposed to lead through both breathing and skin contact. The mean BLL was 7.92 ± 3.44 μg/dL among the subjects.
Table 1.
Demographic characteristics, risk factors, and hypertension of the studied population
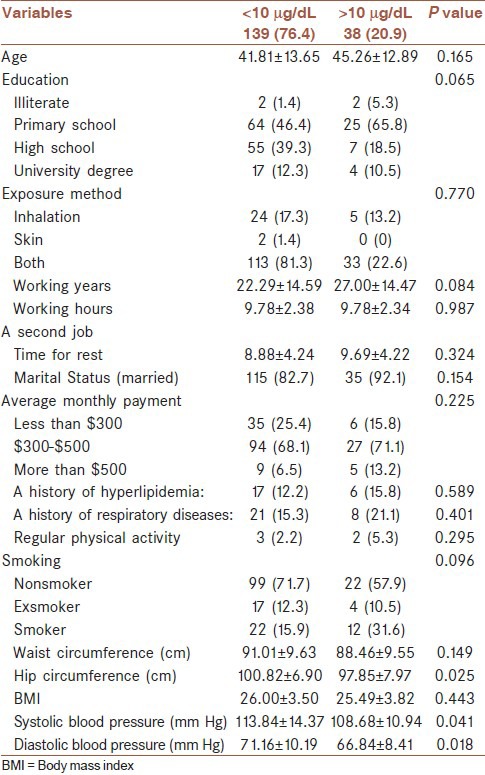
The results of comparisons between groups with BLL < 10 μg/dL and BLL ≥ 10 μg/dL are presented in Table 2. Only hip circumference and systolic blood pressure were significantly higher in those with BLL < 10 μg/dL.
Table 2.
Comparison of different variables in subjects with blood lead levels <10 μg/dL and 10> μg/dL
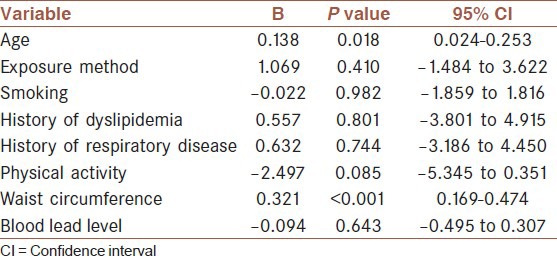
BLL was not found to have any significant effects on systolic or diastolic blood pressure. Correlation coefficients between BLL and systolic and diastolic blood pressure were r = –0.105 (P = 0.165) and r = –0.070 (P = 0.354), respectively. The effects of lead on blood pressure, considering demographics, and lifestyle-related factors, were evaluated by stepwise linear regression [Tables 3 and 4]. In the crude model, the effects of lead on systolic and diastolic blood pressure before stepwise regression were B = –0.422 [95% confidence interval (CI): –1.019 to 0.175] and B = –203 (95% CI: –0.635 to 0.229), respectively. However, after entering age, exposure method, smoking, physical activity, waist circumference, and history of dyslipidemia and respiratory diseases in the regression model, the corresponding values were B = –0.327 (CI 95%: –0.877 to 0.223) and B = –0.094 (CI 95%: –0.495 to 0.307).
Table 3.
The Effect of age, risk factors, and blood lead level on systolic blood pressure
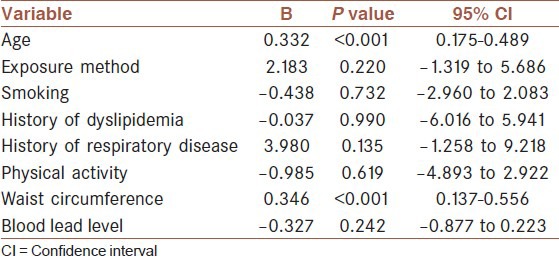
Table 4.
The Effect of age, risk factors, and blood lead level on diastolic blood pressure
DISCUSSION
Despite expectations, the results of the present study on 182 normotensive adult men with a mean lead exposure duration of 23.67 years revealed normal BLLs among battery factory workers. Banihashemrad et al.,[13] evaluated 50 battery factory workers in Mashhad, Iran. They found that although the subjects were in contact with lead for 23.4 ± 19.5 years, their mean BLL was 15 μg/dL. Normal BLLs in our study might have been a result of novel battery usage and recycling methods. While several times of reopening and reuse of the batteries used to put workers in direct contact with lead plates, lead exposure has recently decreased due to the availability of new batteries and the General Safety Regulations for Auto Mechanics.[14] On the contrary, previous studies have shown BLL to be an indicator of air lead levels.[15] Therefore, reductions in BLL following a 2-year implementation of the mentioned regulations could have been caused by reduced lead levels in the air. Although we did not measure air lead pollution in the studied companies, it seems that the regulations have been successful in reducing air lead levels.
Interestingly, a significant relation was not found between BLL and systolic and diastolic blood pressure in the present study. An early study by Pocock et al.,[16] evaluated 7735 middle-aged men in 24 cities in England. They did not find a significant relation between BLL and systolic and diastolic blood pressure even after adjustments for age, alcohol consumption, BMI, and social class. Furthermore, the frequency of hypertension did not increase by augmented BLLs. However, in another study that did on 154 Croatian 19-53 years old showed significant increase in blood pressure that be lead dependent.[17] It is noteworthy that the two last studies evaluated general population.
Several other studies have also assessed individuals in contact with lead and found conflicting results. Fenga et al.,[18] evaluated 27 male battery factory workers and suggested a cumulative lead exposure increase blood pressure significantly in subject with low lead exposure. Another study compared 166 workers exposed to lead with 60 persons in a control group and reported significantly higher diastolic blood pressure among subjects in contact with lead. On the contrary, the two groups did not significantly differ in terms of systolic blood pressure.[19] Schuhmacher et al.,[20] also compared 36 men in occupational exposure to lead with 40 subjects not contacted with lead. They did not find a significant relation between BLL and blood pressure.
Fenga et al.,[18] studied 27 normotensive battery factory workers without a history of mentioned diseases in a cohort study. The studied subjects had a mean BLL of 42.33 ± 15.16 μg/dL. The participants were divided into two groups including those directly working with lead and those indirectly exposed to the element. They suggested the participants working with lead to have higher mean systolic and diastolic blood pressure in comparison with those indirectly exposed to the material. However, Spearman test did not reveal any significant relation between BLL and blood pressure. Like Fenga et al.,[18] we studied normotensive individuals without a history of cardiovascular diseases or diabetes and could not find a significant relation between BLL and blood pressure. However, BLL was more than normal range in their study. Excluding hypertensive persons cannot be responsible for the insignificant relations observed. Kaewboonchoo et al.,[21] studied nonhypertensive bus drivers with normal BLLs and their results shown a significant correlation between BLL with systolic and diastolic blood pressure.
Limited Iranian studies have assessed the blood pressure of battery company workers. For instance, Ghiasvand et al., found the mean BLL levels to be 43.3 μg/dL in 497 male battery workers. However, they failed to establish a significant relationship between BLL and systolic blood pressure. They only detected a weak association between BLL and systolic blood pressure (odds ratio: 1.03; 95% CI: 101-105).[11] In another research on 165 male Iranian battery factory workers, BLL was not significantly related with either systolic or diastolic blood pressure.[12]
Furthermore, considering all hypertension risk factors, such as stress (particularly occupational stress), could have affected the relation between BLL and blood pressure; the results of the present study might also have changed if all risk factors were included.
CONCLUSION
The present revealed normal BLLs among battery factory workers in Isfahan. A significant relation between BLL and systolic or diastolic blood pressure could not be found. Further studies comparing normotensive and hypertensive individuals seem necessary. In addition, a cohort study can better reflect the effects of lead on blood pressure by comparing at-risk individuals with a control group.
LIMITATIONS
Since the study required blood samples from the participants, some subjects did not consent to participate. Moreover, the length of food frequency questionnaire prevented us from asking all questions which might have altered the results. Finally, unavailability of lead levels in different areas of Isfahan eliminated the possibility of evaluating the effects of place of residence.
ACKNOWLEDGMENTS
This research was a Resident's thesis that supported by Vice Chancellor for research, Isfahan University of Medical Sciences (research project number was 389462). Authors would like to acknowledge all battery companies workers who participated in this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Taheri L, Sadeghi M, Sanei H, Rabiei K, Sarrafzadegan N. Effects of occupational exposure to lead on left ventricular echocardiographic variables. ARYA Atherosclerosis Journal. 2012;8:130–135. [PMC free article] [PubMed] [Google Scholar]
- 2.Rossi E. Low level environmental lead exposure-a continuing challenge. Clin Biochem Rev. 2008;29:63–70. [PMC free article] [PubMed] [Google Scholar]
- 3.Navas-Acien A, Guallar E, Silbergeld EK, Rothenberg SJ. Lead exposure and cardiovascular disease-a systematic review. Environ Health Perspect. 2007;115:472–82. doi: 10.1289/ehp.9785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amaya MA, Jolly KW, Pingitore NE., Jr Blood lead in the 21st Century: The sub-microgram challenge. J Blood Med. 2010;1:71–8. doi: 10.2147/JBM.S7765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders T, Liu Y, Buchner V, Tchounwou PB. Neurotoxic effects and biomarkers of lead exposure: A review. Rev Environ Health. 2009;24:15–45. doi: 10.1515/reveh.2009.24.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murata K, Iwata T, Dakeishi M, Karita K. Lead toxicity: Does the critical level of lead resulting in adverse effects differ between adults and children? J Occup Health. 2009;51:1–12. doi: 10.1539/joh.k8003. [DOI] [PubMed] [Google Scholar]
- 7.Menke A, Muntner P, Batuman V, Silbergeld EK, Guallar E. Blood lead below 0.48 micromol/L (10 microg/dL) and mortality among US adults. Circulation. 2006;114:1388–94. doi: 10.1161/CIRCULATIONAHA.106.628321. [DOI] [PubMed] [Google Scholar]
- 8.Navas-Acien A, Selvin E, Sharrett AR, Calderon-Aranda E, Silbergeld E, Guallar E. Lead, cadmium, smoking, and increased risk of peripheral arterial disease. Circulation. 2004;109:3196–201. doi: 10.1161/01.CIR.0000130848.18636.B2. [DOI] [PubMed] [Google Scholar]
- 9.Lustberg M, Silbergeld E. Blood lead levels and mortality. Arch Intern Med. 2002;162:2443–9. doi: 10.1001/archinte.162.21.2443. [DOI] [PubMed] [Google Scholar]
- 10.Patrick L. Lead toxicity, a review of the literature. Part 1: Exposure, evaluation, and treatment. Altern Med Rev. 2006;11:2–22. [PubMed] [Google Scholar]
- 11.Ghiasvand M, Aghakhani K, Salimi A, Kumar R. Ischemic heart disease risk factors in lead exposed workers: Research study. J Occup Med Toxicol. 2013;8:11. doi: 10.1186/1745-6673-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadeghniiat-Haghighi KH, Bahaedini LS, Mehrdad R, Meysami AP, Chavoshi F, Soltani SH. Relationship between blood pressure and lead exposure in battery recycling workers. J Biol Sci. 2011;11:454–8. [Google Scholar]
- 13.Banihashemrad SA, Sanatkhani M, Zareh GH. Prevalence of gingival and oral pigmentations in battery Industry workers in Khorasan province. J Dent Mashhad Univ Med Sci. 2005;29:9–16. [Google Scholar]
- 14.CDC, Third National Report on Human Exposure to Environmental Chemicals, Centers for Disease Control and Prevention, NCEH, Atlanta. 2005. [Publ. No. 05-0570].
- 15.Zeqiri N, Zeqiri S, Skenderaj S. Blood pressure evaluation at the workers exposed to lead. Med Arh. 2012;66:92–3. doi: 10.5455/medarh.2012.66.92-93. [DOI] [PubMed] [Google Scholar]
- 16.Pocock SJ, Shaper AG, Ashby D, Delves HT, Clayton BE. The relationship between blood lead, blood pressure, stroke, and heart attacks in middle-aged British men. Environ Health Perspect. 1988;78:23–30. doi: 10.1289/ehp.887823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Telisman S, Jurasović J, Pizent A, Cvitković P. Blood pressure in relation to biomarkers of lead, cadmium, copper, zinc, and selenium in men without occupational exposure to metals. Environ Res. 2001;87:57–68. doi: 10.1006/enrs.2001.4292. [DOI] [PubMed] [Google Scholar]
- 18.Fenga C, Cacciola A, Martino LB, Calderaro SR, Di Nola C, Verzera A, et al. Relationship of blood lead levels to blood pressure in exhaust battery storage workers. Ind Health. 2006;44:304–9. doi: 10.2486/indhealth.44.304. [DOI] [PubMed] [Google Scholar]
- 19.dos Santos AC, Colacciopo S, Dal Bo CM, dos Santos NA. Occupational exposure to lead, kidney function tests, and blood pressure. Am J Ind Med. 1994;26:635–43. doi: 10.1002/ajim.4700260506. [DOI] [PubMed] [Google Scholar]
- 20.Schuhmacher M, Bosque MA, Domingo JL, Corbella J. Effects of chronic lead and cadmium exposure on blood pressure in occupationally exposed workers. Biol Trace Elem Res. 1994;41:269–78. doi: 10.1007/BF02917428. [DOI] [PubMed] [Google Scholar]
- 21.Kaewboonchoo O, Saleekul S, Powwattana A, Kawai T. Blood lead level and blood pressure of bus drivers in Bangkok, Thailand. Ind Health. 2007;45:590–4. doi: 10.2486/indhealth.45.590. [DOI] [PubMed] [Google Scholar]


