Abstract
Background:
In surgeries of closed calcaneal fractures, the lateral L-shaped incision is usually adopted. Undesirable post-operative healing of the incision is a common complication. In this retrospective study, controllable risk factors of incision complications after closed calcaneal fracture surgery through a lateral L-shaped incision are discussed and the effectiveness of clinical intervention is assessed.
Materials and Methods:
A review of medical records was conducted of 209 patients (239 calcaneal fractures) surgically treated from June 2005 to October 2012. Univariate analyses were performed of seven controllable factors that might influence complications associated with the surgical incision. Binomial multiple logistic regression analysis was performed to determine factors of statistical significance.
Results:
Twenty-one fractures (8.79%) involved surgical incision complications, including 8 (3.35%) cases of wound dehiscence, 7 (2.93%) of flap margin necrosis, 5 (2.09%) of hematoma, and 1 (0.42%) of osteomyelitis. Five factors were statistically significant : The time from injury to surgery, operative duration, post-operative drainage, retraction of skin flap, bone grafting, and patients’ smoking habits. The results of multivariate analyses showed that surgeries performed within 7 days after fracture, operative time > 1.5 h, no drainage after surgery, static skin distraction, and patient smoking were risk factors for calcaneal incision complications. The post-operative duration of antibiotics and bone grafting made no significant difference.
Conclusion:
Complications after calcaneal surgeries may be reduced by postponing the surgery at least 7 days after fracture, shortening the time in surgery, implementing post-operative drainage, retracting skin flaps gently and for as short a time as possible, and prohibiting smoking.
Keywords: calcaneal fractures, calcaneus, incision, open reduction with internal fixation, surgical complication
INTRODUCTION
High-energy calcaneal fractures have become increasingly common in the construction industry and traffic accidents, and patients’ need for early function is paramount.[1] As a result, the number of surgeries for calcaneal fractures has increased significantly,[1] as well as associated surgical complications. The most common and recalcitrant of complications are related to surgical incisions; examples include infection of the incision and necrosis of the skin margin. The incidence rate of post-operative wound complications reported by Folk et al.[2] was 25%. Al-Mudhaffar et al.[3] have reported complication rates of 18.1% infection, 12.1% wound dehiscence, and 3% hematoma. Other reported rates have ranged from 10% to 27%, respectively.[2,4,5,6,7,8]
The high incidence of post-operative wound complications is generally considered due to the anatomical structure of the calcaneus, the poor condition of injured soft-tissues, and the design of surgical incisions. However, our observation is that the outcome varies even when standardized surgical incisions, non-contact technique, and positive anti-infection measures are adopted. Therefore, there might be multiple factors influencing the outcome of calcaneal surgical incisions pertinent to the peri-operative period. Numerous former studies have variously reported that the healing of lateral skin flaps is influenced by the patient's age, cause and type of fracture, surgical wait time, body mass index, reduction of Böhler's angle, quality of the suture, skin distraction method, and timing of the suture removal.[9,10,11,12,13,14] Yet, clinical analyses are required to determine which interventions related to surgery could improve the healing of lateral skin flaps.
In the present study, we reviewed retrospectively and analyzed by logistic regression the data of 239 calcaneal fractures in 209 patients who received surgical treatment at Shanghai First People's Hospital from June 2005 to October 2012, to determine independent factors that may influence the outcome of surgical incisions. The protective or risk function of each factor was assessed, and the effectiveness of clinical intervention was evaluated.
MATERIALS AND METHODS
Cases enrolled were selected based on data in the records of patients who received open reduction with internal fixation of calcaneal fractures in our hospital from June 2005 to October 2012. A total of 209 patients (with 239 calcaneal fractures) were selected (147 men, 62 women; average age 37.6 year). For inclusion in the study, all patients were between the ages of 18 and 70 year, with a closed calcaneal fracture. In all cases a typical L-shaped lateral incision was performed. No patient combined the calcaneal fracture with an ankle fracture on the same side, nor suffered from diabetes or vascular diseases of the lower limbs, nor had obvious soft-tissue infections or skin diseases.
Pre-operative preparation and surgical method
Patients were placed in the lateral position on the uninjured side. A pneumatic tourniquet on the injured limb was maintained at 240 mmHg pressure.
The surgical approach was a lateral L-shaped skin incision, which originated 3-5 cm above the lateral malleolus, extended along the posterior margin of the fibula passing the midpoint of the posterior margin of the Achilles tendon down to the junction of the lateral and plantar skin, and then turned anteriorly reaching 1 cm proximal to the base of the fifth metatarsal bone. The incision was deep to the bone. Full-thickness skin flaps were distracted, and the peroneus was pulled upwards. To separate soft-tissues an electric scalpel was avoided. Either of two methods was used to distract skin flaps. For the static method, three Kirschner wires were drilled into the talus bone and the calcaneal subtalar joint was kept constantly exposed with the bended wires. In the dynamic method, the flaps were distracted manually by other surgeons.
After retraction of the skin flap, the calcaneus was reduced and the smoothness of the subtalar joint and height and width of the calcaneus was restored. For fractures with severe compression, bone defects were filled with autogenous, allograft, or artificial bone and fixed with a calcaneal plate. The incision was closed with a two-layered suture.
Antibiotics were administered routinely from 30 min before surgery to 3 days after surgery for prophylactic purposes, and stopped when the incision was dry without exudation; otherwise administration was prolonged for several days. Usually, sutures were removed 3 weeks after surgery.
Criteria for cases positive for incision complications
A case history was considered to contain positive evidence of surgical incision complications if there was persistent exudation over 2 weeks, or delayed suture removal; hematoma; infection of the incision (i.e., positive bacterial culture); necrosis of the incision skin margin or dehiscence of the incision; deep infection, osteomyelitis, and sinus tract formation; the internal fixator was taken out before healing of the fracture; or there was persistent negative pressure drainage of the wound.
Statistical treatment
The incidence of surgical incision complications was taken as the dependent variable, and possible associated factors as independent variables [Table 1]. According to the relevant literature, there are many factors that may influence the success of the surgical incision. These include the cause of the fracture (and height of the fall, if due to a falling accident), the age, weight, and general condition of the patient, the time between fracture and surgery, time under tourniquet, time in surgery, concomitant diseases or injuries, and post-operative care.[10,11] In the present study with a limited number of cases, logistic regression was conducted to analyze the case quantity requirements of independent variables; sample size should be 10 times the number of variables for each group.[15,16] Factors that may influence each other were excluded. For example, time under tourniquet and surgical time are related, and since the data for time under tourniquet was not as reliable, surgical time was chosen.
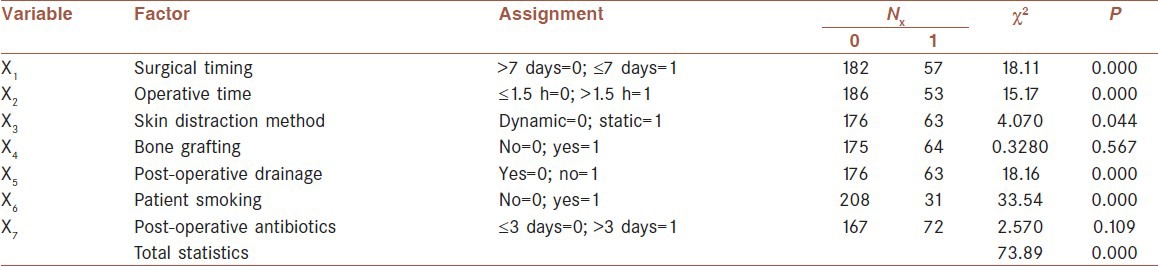
Table 1.
Results of univariate analyses
We excluded factors that were known to have a direct influence on the dependent variable (e.g., infection, diabetes, and vascular diseases). Finally, we choose only factors that could be regulated and were related to surgical steps; uncontrollable factors such as age, gender, weight, height of fall, and type of fracture were not analyzed.
Based on the above principles and previous literature as well as clinical experience, the following factors were selected as independent variables and assigned:
Wait time from fracture to surgery, ≤7 day or >7 day;
Time in surgery, ≤1.5 h or >1.5 h;
Bone grafting, yes or no;
Skin flap distraction method, dynamic or static;
Post-operative drainage, yes or no;
Patients’ smoking, yes or no; and
Antibiotics, applied ≤3 day or >3 day during the post-operative period.
A standardized database was established using SPSS 17.0 Statistical Software (SPSS, Chicago, Illinois). Univariate analyses of the above seven factors were carried out based on the occurrence or not of complications. Factors with statistical significance at P > 0.1 were then excluded from the final logistic regression equation analysis.[15,16]
RESULTS
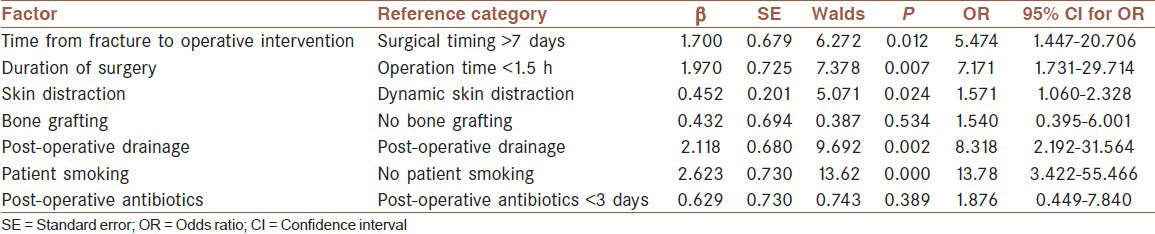
Among the 239 cases of calcaneal fracture reviewed in this study, 21 cases (8.79%) experienced surgical incision complications, of which 8 (3.35%) were wound dehiscence [Figure 1], 5 (2.09%) hematoma, 7 (2.93%) flap margin necrosis, and 1 (0.420%) osteomyelitis. Five factors in the univariate analyses carried statistical significance: the timing and duration of surgery, the skin distraction method, post-operative drainage, and patients’ smoking status [Table 1]. Bone grafting and duration of antibiotics had no statistical relevance. The following regression equation was determined:
Figure 1.

A male patient with many years of smoking history, with wound dehiscence and skin flap necrosis 8 weeks after surgery. Bacteriological culture showed that the infection was caused by methicillin-resistant Staphylococcus aureus
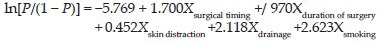
The Hosmer-Lemeshow test for logistic regression indicated that the model fit the data well [χ2 = 10.439, degree of freedom (df) = 7, P = 0.165; Table 2]. The results indicated that the surgical timing, duration of surgery, retraction of skin flap, post-operative drainage, and patients’ smoking were statistically relevant to the incidence of incision complications.
Table 2.
Statistical table of regression analysis
The risk of incision complications for surgeries occurring within 3 days of injury was 5.47 times higher than that of surgeries delayed more than 3 days. Incision complications when time in surgery was longer than 1.5 h were 7.17 times more likely than for surgeries lasting <1.5 h. Static retraction was 1.57 times more likely to result in incision complications than dynamic retraction. Fractures that were given no post-operative drainage were 8.32 times more likely to suffer incision complications than those with post-operative drainage. The risk of incision complications was 13.8 times higher in smoking patients than in those who do not smoke. The application time for antibiotics and whether bone grafting was performed had no statistical bearing on the incidence of complications.
DISCUSSION
The lateral extensile L-shaped incision is widely used in the treatment for calcaneal fractures. It provides adequate exposure and convenience for subtalar articular surface reduction. However, it is associated with a high incidence of incision complications, which if mishandled will not only make patients suffer, but also increase hospitalizations and expenses. Moreover, for some patients with severe infections the internal fixator must be taken out sooner than intended, resulting in failure of the fracture reduction.
Poor blood supply has been considered the reason for problems in lateral skin flap healing. However, studies of calcaneal vascular anatomy show that blood to the lateral heel is mainly supplied from the lateral calcaneal and tarsal arteries, and branches of the lateral malleolar artery. The blood supply of the incision corner is mainly from the lateral calcaneal artery [Figure 2].[17]
Figure 2.
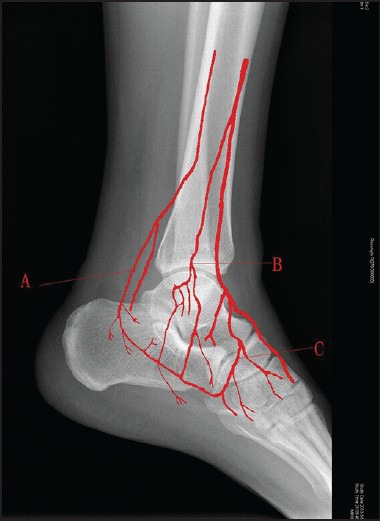
Arteries supplying the L-shaped incision corner. (a) Lateral calcaneal artery. (b) lateral malleolar artery. (c) lateral tarsal artery
In our study, 239 open reduction/internal fixations of closed calcaneal fractures were performed by our senior surgeons through standard extensile L-shaped incision with non-contact technique, and positive anti-infection measures were applied. The rate of wound complications was still very high (8.79%), but slightly lower than the rate reported from other studies (10-27%). Further analyses of incision complications indicate that they are most likely related to intervening measures in the peri-operative period and the particular condition of the patient.[2,6,13,18]
We designed this study to assess these risk factors or protective factors, and to evaluate the effect of clinical intervention. Non-surgical factors such as weight, age, cause of injury, or combinations of these were excluded from the present study because they cannot be regulated or controlled by the surgeon. Rather, the seven factors selected in this study are all under medical control, except for patient smoking. Analyzing through binomial logistic regression the influence of these factors on the incidence of incision complications, we found that the time from injury to surgery, operation time, skin distraction method, performance of post-operative drainage and patient smoking were statistically significant.
Surgical timing
Of the 21 cases of incision complications in this study, the time from fracture to surgery was <7 days in 5 (23.8%). Among orthopedic trauma surgeons the surgical timing of calcaneal fracture is controversial.[1,19,20] Two case groups were reported by Abidi et al.,[11] and the incidence of complications in the earlier-surgery group (4.8 days on average) was 16.6%, while in the delayed-surgery group (9.9 days in average) the incidence rose to 42.5% (P < 0.03). In Al-Mudhaffar et al.'s[3] retrospective, six cases with complications underwent a mean wait time of 4 days (95% confidence interval [CI]: 2-7 days), while 27 cases that were complication-free had a mean wait time of 9 days (95% CI: 7-10).
A current common view is that surgeries should be carried out after the condition of soft-tissues improves. However, complete regression of soft-tissue edema generally requires 3 weeks. If the surgery is postponed for that long, hematoma at the fracture will occur with the formation of fibrous bony callus making separation and reduction of fracture fragments difficult, and will hamper the final success of the surgery.[1]
Emergency open reduction and internal fixation can only be adopted in patients with good calcaneal skin condition without soft-tissue edema. The condition of soft-tissues should be based on a wrinkled skin test, rather than local swelling. This is because outward dislocation due to fracture of the lateral wall of the calcaneus could appear as soft-tissue swelling. If there is tension blister on the skin, the surgery should be conducted after the vesicles are naturally healed.[21]
Duration of surgery
It is usually accepted that the longer the surgical time, the higher the incidence of incision problems. Koski et al.[18] reported a group of cases (126 patients, 148 calcaneal fractures) with an average surgical time of 101 min (range, 40-330 min), in which time in surgery was statistically associated with incision complications (P = 0.04). The average surgical time of cases with complications reported by Al-Mudhaffar et al.[4] was 153 min, which was statistically different from that of the group without complications (114 min).
Application of a tourniquet is standard routine in calcaneus surgery, and longer surgical time means longer hypoxia and ischemia of tissues and more severe damage to local soft-tissue cells due to ischemia reperfusion, which detrimentally influences the healing of the incision. On the other hand, the tourniquet is most often taken away if the surgery lasts more than 1.5 h; hyperemia and swelling of local soft-tissues results and thus high tension when suturing the wound, which is also detrimental to healing. In the present study, we found through regression analysis that the relative risk of incision complications after surgeries of over 1.5 h is 7.29-fold that of surgeries completed within 1.5 h. This indicates that besides ensuring the quality of surgery, shortening the surgical time (i.e., tourniquet time) as much as possible will reduce problems of incision.
Retraction of skin flap
The static method of skin distraction is the most commonly used method clinically. It involves drilling three Kirschner wires into the lateral process of the talus bone, and non-contact skin distraction is effected when the wires are bent. Conversely, the dynamic method is to distract the soft-tissues manually using silk sutures or a bone detacher. Interestingly, the current study results showed that the risk of complication with the static distraction method was 1.59 times higher than when the dynamic was employed. Recently, it was reported that 24 of 109 (22%) patients who underwent static distraction suffered incision complications, while this was true of only 6 of 68 (8%) patients in whom dynamic distraction was used; the incidence of complications with the static method was thus nearly 2.9 times higher than the dynamic.[22] However, which method is safer remains a controversial issue and further prospective studies based on a larger sample are required. Static distraction may incur more incision complications because it is a persistent state. When combined with a longer surgery, this is likely to influence the blood supply of the skin flaps. Particularly in our study, surgeons using the dynamic method were careful to avoid prolonged ischemia of the skin flaps.
Post-operative drainage
Both special anatomical position of the calcaneus and the L-shaped incision are prone to inadequate drainage of the wound, as well as local hematoma and infection. Thus, indwelling drainage is recommended, and this is supported by statistical analysis. In previous studies, the researchers concluded that negative pressure drainage is preferred to prevent wound complications.[23,24,25] With negative pressure drainage, it is easier to discharge congested blood and relieve edema; negative pressure can also promote the expansion of small arteries, mitosis, and the production of a new capillary bed; and negative pressure can reopen capillaries that are occluded around the wound, caused by injuries and infections.[26,27] Pressure bandaging by elastic bandage is also recommended to supplement negative pressure drainage;[28] the flaps are pressed evenly to reduce bleeding and the effect of negative pressure is enhanced by eliminating spaces.
In a multicenter prospective randomized study conducted by Stannard et al.,[24] closed continuous negative pressure drainage was used in treatments for high-risk lower limb fractures including calcaneal fracture. The patients given negative pressure wound therapy experienced significantly fewer incision infections than those given standard post-operative dressings (12.7% and 28.3%, respectively). Therefore, in calcaneal surgeries if symptoms such as wound dehiscence and infections emerge at an early stage after surgery, continuous negative pressure drainage should be adopted as soon as possible to facilitate wound healing.
Smoking
It has been widely reported that smoking has a detrimental effect on the healing of fractures and wounds.[2,13] According to statistical analysis based on the present study, the risk of incision complications is 14-fold higher in smoking patients than in non-smoking patients. Tobacco smoke contains at least three toxic substances: nicotine, tar, and carbon monoxide. These toxins contract blood vessels and reduce blood supply to the extremities, with decrease in the contractility of vessels, blood flow rate, and efficiency of oxygen transportation. Smoking also causes a decline in the body's resistance to infections. These negative effects are reversible.[29] Post-operative complications may be reduced if patients stop smoking for 10 days after surgery.[30,31] We conclude that prohibiting smoking pre- and post-surgery is of great importance in reducing post-surgical complications in calcaneal fracture patients.
Antibiotics
In the present study, according to the regression equation the duration of application of antibiotics played no statistically significant part in the incidence of incision complications. This indicates that application of antibiotics is not helpful in avoiding problems of incisions caused by inadequate pre-operative preparation, improper intra-operative operation, and nonstandard post-operative nursing. Prolonged application of antibiotics will never resolve such problems completely, but can only be used as a remedial measure in cases with incision problems.
Bone grafting
For bone defects under the articular surface of the subtalar joint after reduction, the necessity of bone grafting is still disputed. Grala et al.[32] in their study have reported that bone grafting favored early-stage weight bearing and could reduce risk of later collapse of the articular surface and incidence of nonunion. Bajammal et al.[33] pointed out that bone graft can be used to fill the bone defect to prevent hematoma and reduce the infection rate. However, Rammelt et al.[34] and Longino and Buckley[35] have published data that there is no necessity to implant bone graft for calcaneal fracture. A systematic review from Yang et al.[36] showed that the operative treatment of intraarticular calcaneal fractures with bone grafts could restore Bohler's angle better and the patients could return to full weight bearing earlier. Furthermore, the functional and efficacy outcomes appear to be similar between patients with or without bone grafting, although some literature has reported an association between calcium sulfate and infection rate.[37] There have been no previous studies on the influence of bone grafting on post-operative complications of the incision. In the present study, we found no statistical difference in complications between those who received bone grafting and those who did not. However, clinical experience indicates that with less local space after bone grafting hematoma may be avoided, thus reducing incision problems.
In the present study, we did not address the diversity of fracture types, correction of Böhler's angle, bone grafting materials, or internal fixators, because of the small number of cases and the abnormal distribution of data. On the other hand, it may be that not all relevant factors were investigated in this study. For example, we only recorded the time in surgery, as the time under tourniquet was not available. In addition, the relationship between Böhler's angle and the surgical incision is important and is worth investigating. In addition, as the number of known cases increases, more indices may be accounted for, and a multi-center retrospective study based on larger sample volume will become feasible.
AUTHOR'S CONTRIBUTIONS
Kai Wu carried out the design and coordinated the study, participated in most of the operations and prepared the manuscript. Chuanshun Wang provided assistance in the design of the study, collected all the data. Haoqing Li participated in manuscript preparation.,also reviewed and edited the manuscript. Qiugen Wang provided assistance for the study and revised the paper. All authors have read and approved the content of the manuscript.
CONCLUSION
When the lateral L approach is adopted in treatment of closed calcaneal fractures, aside from basic standards for performing the incision and ensuring proper soft-tissue protection, cautious use of the electric scalpel, and non-contact technique, the results of our study are a reminder that additional controllable factors remain to prevent incision complications. Specifically,
Surgery should be timed to coincide with the wrinkly skin sign, usually occurring more than 7 days after fracture;
The operative procedure (including time under tourniquet) should be made as short and efficient as possible;
The tension and duration of skin flap distraction should be given special attention when static distraction is adopted;
Negative pressure drainage should be routine after surgery;
Patients should be advised not to smoke, both before and after surgery; and
The duration of antibiotic treatment need not be more than 3 days, but can be prolonged if necessary.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Epstein N, Chandran S, Chou L. Current concepts review: Intra-articular fractures of the calcaneus. Foot Ankle Int. 2012;33:79–86. doi: 10.3113/FAI.2012.0079. [DOI] [PubMed] [Google Scholar]
- 2.Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: Analysis of 190 fractures. J Orthop Trauma. 1999;13:369–72. doi: 10.1097/00005131-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Al-Mudhaffar M, Prasad CV, Mofidi A. Wound complications following operative fixation of calcaneal fractures. Injury. 2000;31:461–4. doi: 10.1016/s0020-1383(00)00026-7. [DOI] [PubMed] [Google Scholar]
- 4.Howard JL, Buckley R, McCormack R, Pate G, Leighton R, Petrie D, et al. Complications following management of displaced intra-articular calcaneal fractures: A prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma. 2003;17:241–9. doi: 10.1097/00005131-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Lim EV, Leung JP. Complications of intraarticular calcaneal fractures. Clin Orthop Relat Res. 2001;391:7–16. doi: 10.1097/00003086-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 6.SooHoo NF, Farng E, Krenek L, Zingmond DS. Complication rates following operative treatment of calcaneus fractures. Foot Ankle Surg. 2011;17:233–8. doi: 10.1016/j.fas.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Wiersema B, Brokaw D, Weber T, Psaradellis T, Panero C, Weber C, et al. Complications associated with open calcaneus fractures. Foot Ankle Int. 2011;32:1052–7. doi: 10.3113/FAI.2011.1052. [DOI] [PubMed] [Google Scholar]
- 8.Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res. 1993;290:76–86. [PubMed] [Google Scholar]
- 9.Gupta A, Ghalambor N, Nihal A, Trepman E. The modified Palmer lateral approach for calcaneal fractures: Wound healing and postoperative computed tomographic evaluation of fracture reduction. Foot Ankle Int. 2003;24:744–53. doi: 10.1177/107110070302401003. [DOI] [PubMed] [Google Scholar]
- 10.Shuler FD, Conti SF, Gruen GS, Abidi NA. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures: Does correction of Bohler's angle alter outcomes? Orthop Clin North Am. 2001;32:187–92. doi: 10.1016/s0030-5898(05)70202-9. x. [DOI] [PubMed] [Google Scholar]
- 11.Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int. 1998;19:856–61. doi: 10.1177/107110079801901211. [DOI] [PubMed] [Google Scholar]
- 12.Di Schino M, Bensaïda M, Vandenbussche E, Augereau B, Nich C. Results of open reduction and cortico-cancellous autograft of intra-articular calcaneal fractures according to Palmer. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:135–44. doi: 10.1016/j.rco.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Hao D, Chen C, Wang D, Yin Y. Non-operation related risk factors of wound complications of calcaneal fractures using lateral extensive L-shaped incision. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:30–5. [PubMed] [Google Scholar]
- 14.Gaskill T, Schweitzer K, Nunley J. Comparison of surgical outcomes of intra-articular calcaneal fractures by age. J Bone Joint Surg Am. 2010;92:2884–9. doi: 10.2106/JBJS.J.00089. [DOI] [PubMed] [Google Scholar]
- 15.Long JS. Vol. 7. Texas: Sage; 1997. Regression Models for Categorical and Limited Dependent Variables. [Google Scholar]
- 16.Pampel FC. Vol. 132. Iowa: Sage; 2000. Logistic Regression: A Primer. [Google Scholar]
- 17.Borrelli J, Jr, Lashgari C. Vascularity of the lateral calcaneal flap: A cadaveric injection study. J Orthop Trauma. 1999;13:73–7. doi: 10.1097/00005131-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Koski A, Kuokkanen H, Tukiainen E. Postoperative wound complications after internal fixation of closed calcaneal fractures: A retrospective analysis of 126 consecutive patients with 148 fractures. Scand J Surg. 2005;94:243–5. doi: 10.1177/145749690509400313. [DOI] [PubMed] [Google Scholar]
- 19.Fulkerson EW, Egol KA. Timing issues in fracture management: A review of current concepts. Bull NYU Hosp Jt Dis. 2009;67:58–67. [PubMed] [Google Scholar]
- 20.Dhillon MS, Bali K, Prabhakar S. Controversies in calcaneus fracture management: A systematic review of the literature. Musculoskelet Surg. 2011;95:171–81. doi: 10.1007/s12306-011-0114-y. [DOI] [PubMed] [Google Scholar]
- 21.Strauss EJ, Petrucelli G, Bong M, Koval KJ, Egol KA. Blisters associated with lower-extremity fracture: Results of a prospective treatment protocol. J Orthop Trauma. 2006;20:618–22. doi: 10.1097/01.bot.0000249420.30736.91. [DOI] [PubMed] [Google Scholar]
- 22.Megan BL, Musapatika D, Brokaw D. Complications with open reduction and internal fixation of calcaneal fractures: Static versus dynamic retraction. AAOS Annual Meeting. 2012:490. [Google Scholar]
- 23.Stannard JP, Robinson JT, Anderson ER, McGwin G, Jr, Volgas DA, Alonso JE. Negative pressure wound therapy to treat hematomas and surgical incisions following high-energy trauma. J Trauma. 2006;60:1301–6. doi: 10.1097/01.ta.0000195996.73186.2e. [DOI] [PubMed] [Google Scholar]
- 24.Stannard JP, Volgas DA, McGwin G, 3rd, Stewart RL, Obremskey W, Moore T, et al. Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma. 2012;26:37–42. doi: 10.1097/BOT.0b013e318216b1e5. [DOI] [PubMed] [Google Scholar]
- 25.Timmers MS, Le Cessie S, Banwell P, Jukema GN. The effects of varying degrees of pressure delivered by negative-pressure wound therapy on skin perfusion. Ann Plast Surg. 2005;55:665–71. doi: 10.1097/01.sap.0000187182.90907.3d. [DOI] [PubMed] [Google Scholar]
- 26.Mendonca DA, Papini R, Price PE. Negative-pressure wound therapy: A snapshot of the evidence. Int Wound J. 2006;3:261–71. doi: 10.1111/j.1742-481X.2006.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: A new method for wound control and treatment: Animal studies and basic foundation. Ann Plast Surg. 1997;38:553–62. doi: 10.1097/00000637-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J, Xiao B, Wu Z. Surgical treatment of calcaneal fractures with bioabsorbable screws. Int Orthop. 2011;35:529–33. doi: 10.1007/s00264-010-1183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomsen T, Tønnesen H, Møller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg. 2009;96:451–61. doi: 10.1002/bjs.6591. [DOI] [PubMed] [Google Scholar]
- 30.Thomsen T, Villebro N, Møller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. 2010;7:CD002294. doi: 10.1002/14651858.CD002294.pub3. [DOI] [PubMed] [Google Scholar]
- 31.Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet. 2002;359:114–7. doi: 10.1016/S0140-6736(02)07369-5. [DOI] [PubMed] [Google Scholar]
- 32.Grala P, Machyńska-Bućko Z, Kierzynka G. Surgical treatment of articular calcaneal fractures. Ortop Traumatol Rehabil. 2007;9:89–97. [PubMed] [Google Scholar]
- 33.Bajammal S, Tornetta P, 3rd, Sanders D, Bhandari M. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19:360–4. [PubMed] [Google Scholar]
- 34.Rammelt S, Dürr C, Schneiders W, Zwipp H. Minimally invasive fixation of calcaneal fractures. Oper Orthop Traumatol. 2012;24:383–95. doi: 10.1007/s00064-012-0172-9. [DOI] [PubMed] [Google Scholar]
- 35.Longino D, Buckley RE. Bone graft in the operative treatment of displaced intraarticular calcaneal fractures: Is it helpful? J Orthop Trauma. 2001;15:280–6. doi: 10.1097/00005131-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Yang Y, Zhao H, Zhou J, Yu G. Treatment of displaced intraarticular calcaneal fractures with or without bone grafts: A systematic review of the literature. Indian J Orthop. 2012;46:130–7. doi: 10.4103/0019-5413.93672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bibbo C, Patel DV. The effect of demineralized bone matrix-calcium sulfate with vancomycin on calcaneal fracture healing and infection rates: A prospective study. Foot Ankle Int. 2006;27:487–93. doi: 10.1177/107110070602700702. [DOI] [PubMed] [Google Scholar]


